Abstract
Background
Peripheral arterial disease (PAD) is an underdiagnosed illness often affecting the elderly population. Ankle brachial index (ABI) is a good diagnostic tool for PAD in outpatient practice, but remains underused.
Materials and methods
Patients were recruited from an outpatient medical camp in rural India, and assessed for symptoms and pre-existing risk factors. Measured ABI ≤ 0.9 was considered abnormal and considered PAD.
Results
Out of 100 patients recruited, PAD was diagnosed in 57 patients. Associated risk factors were like age >55 years (67%), hypertension (66%), smoking (69%) and diabetes mellitus (35%) were common.
Conclusion
PAD is a very common and underdiagnosed illness in rural India. A simple tool like ABI can help diagnosis in underserved areas.
Keywords: Peripheral arterial disease, Ankle brachial index, Screening
1. Introduction
Peripheral Arterial Disease (PAD) is a major cause of morbidity and mortality predominantly affecting the elderly population.1 PAD is largely undetected due to its silent progression which warrants pre-symptomatic screening.2 Screening for PAD is based on the definition of ankle brachial index (ABI) ≤ 0.90 (American College of Cardiology/American Heart Association (ACC/AHA) 2005 guidelines).3 ABI is a symptom independent, simple, cost effective reliable screening tool for PAD in primary care but remains underused.4 For diagnosis of PAD, ABI of less than 0.9 is 95% sensitive and close to 100% specific.1, 3 In a rural population with limited access to health care, PAD remains understudied. In this study we wanted to measure the disease burden and risk factors of PAD in a rural part of Gujarat, India.
2. Materials and methods
This study was carried out in a tribal belt of Gujarat with poor access to healthcare facilities. At an outpatient medical camp, patients were screened for study participation. All men and women between 18 and 80 years of age were considered, excluding patients with prior history of amputation of any limb. After screening patients, patients were randomly recruited using pre-randomized sealed envelopes. After informed consent, a thorough history and physical examination were obtained. Resting brachial and ankle blood pressures were measured in supine position on both extremities, 5 min apart and the mean pressure recorded and ABI was calculated. All measurements were carried out with a mercury sphygmomanometer and handheld pulse Doppler using a standard technique. Patients with ABI ≤ 0.9 were considered to have PAD.
2.1. Statistical analysis
Continuous variables were expressed as mean ± SD and compared using Student’s t-test. Categorical variables were expressed as numbers (percentage) and compared with a χ2 or Fisher exact test as appropriate. Level of significance was set at 5% for the analysis. Adjusted odds ratios (OR) for potential risk factors were calculated using multivariable logistic regressions, using univariable regressions to choose variables. All statistical analysis was done in Stata® v13.1 (StataCorp LP, College Station, TX).
3. Results
Due to resource constraints, the study was limited to 100 patients. Mean age was 59.3 ± 11 years and 36% were females. Smokers comprised 69% of the sampled population, 66% of subjects were hypertensive, and 35% were diabetic. There was no statistically significant difference between sexes in terms of demographics.
Mean ABI for all subjects was 0.87 ± 0.12. A cut-off value of ABI ≤ 0.9 was used, resulting in 57 patients being diagnosed with PAD. Patients with PAD were more frequently females (46% vs 23%, p = 0.02), hypertensive (77% vs 51%, p = 0.007) and diabetic (53% vs 12%, p < 0.01). All patients with a history of known coronary artery disease (CAD, 30 patients) were found to have PAD. Smokers were commonly found to have PAD (84% vs 48%, p < 0.01). These observations are described in Table 1.
Table 1.
Risks associated with PAD.
| Parameter | Overall (n = 100) | PAD (n = 57) | No PAD (n = 43) | p-value |
|---|---|---|---|---|
| Female | 36 (36) | 26 (46) | 10 (23) | 0.02 |
| HTN | 66 (66) | 44 (77) | 22 (51) | 0.007 |
| DM | 35 (35) | 30 (53) | 5 (12) | <0.001 |
| CAD | 30 (30) | 30 (53) | 0 | <0.001 |
| Smoking | 69 (69) | 48 (84) | 21 (48) | <0.001 |
| Hyperlipidemia | 3 (3) | 3 (5) | 0 (0) | 0.26 |
| Family history | 3 (3) | 2 (4) | 1 (2) | 1 |
| Age | 59.3 ± 11 | 61.9 ± 8.7 | 55.8 ± 12.9 | 0.006 |
| BMI | 22.2 ± 1.8 | 22.9 ± 1.9 | 21.2 ± 1.4 | <0.001 |
Binary outcomes are expressed as n (%).
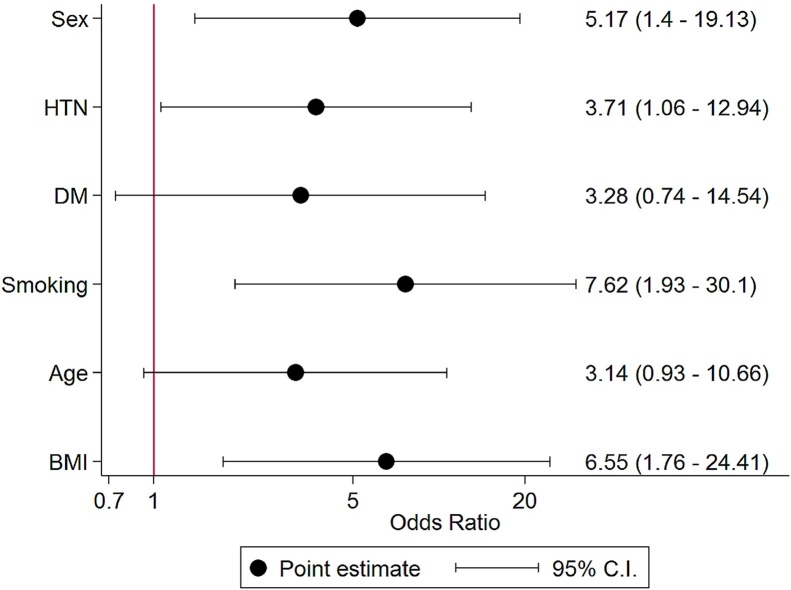
Female sex, hypertension, diabetes mellitus and smoking were found to be predictors of PAD in univariable analysis. Multivariable analysis showed smoking to be the strongest independent predictor of PAD (OR 7.62, 95% CI: 1.93–30.1, p = 0.004). On multivariable analysis age did not show a correlation to prevalence of PAD (OR 3.14, 95% CI 0.93–10.66, p = 0.066). Odds ratios and confidence intervals obtained on multivariable analysis are plotted graphically in Fig. 1.
Fig. 1.
Adjusted Odds Ratios from Multivariable Analysis.
4. Discussion
PAD is a disease of peripheral arteries of lower extremities.1 After CAD and stroke, PAD is third leading cause of cardiovascular morbidity.5 The pathology of PAD is predominantly due to atherosclerotic narrowing of arteries. While prevalence of PAD from developed countries has been studied, but data are lacking from underdeveloped nations. There are very few published accounts of peripheral artery disease in rural India.
Since PAD is primarily asymptomatic, diagnosis in a limited healthcare setting is difficult. ABI is a cheap and simple diagnostic test to screen for peripheral artery disease in the community. It is defined as the ratio of highest systolic pressure at the ankle to that of the brachial artery.6 It has a high sensitivity and specificity, which combined with low costs, make ABI an excellent screening test of choice in populations at risk.2, 3 Well-known risk factors for PAD include smoking, diabetes, hypertension, dyslipidemia, obesity and cardiovascular disease.7 In our study, we found a very high proportion of smokers (69%), hypertensive patients (66%) and diabetics (35%). On multivariable analysis, female sex, hypertension, and smoking were identified as predictors for PAD. Smoking showed a strong associated with PAD (adjusted OR 6.75, p < 0.01). Most diabetics in our study were also smokers. Since smoking is a known predictor of PAD, we could not investigate the association of diabetes with PAD.
Solanki et al. have studied PAD in diabetics an urban India. Among 110 diabetics included, 46% had symptomatic PAD and 35% had low ABI.8 Premalatha et al. conducted a larger study in urban South India. 1262 eligible subjects above the age of 20 participated. Oral glucose tolerance test was used to classify subjects into normal, impaired glucose tolerance and diabetic. Prevalence of PAD in normal, impaired and diabetics is 2.7%, 2.9% and 6.3% respectively with overall being 3.2%. They found age over 50 years was a significant risk factor but observed no association with smoking.9 However ABI was measured in only 50% of subjects. This, in addition to the fact that this study was conducted in an urban area may explain the reports of low prevalence of PAD in the study. Sarangi et al. studied the correlation between PAD and CAD using ABI in an inpatient setting in India. All patients were above the age of 45 years. Out of 182 patients only 32 (18%) had PAD, of which 15 patients had CAD.10 Khurana et al. showed prevalence of PAD based on ABI in Punjab, India. Out of 200 diabetics with age >45 years, 33% had abnormal ABI ≤ 0.9. Nag et al. in 2012 have published a study showing the association of chronic venous ulcer and peripheral arterial disease. They compared the ABI and color Doppler study for PAD and found a strong correlation between them.11
5. Limitations
The cross sectional nature of this study was not designed to evaluate the accuracy of diagnostic methods of PAD. Sample size was relatively small and would not represent an accurate estimation of PAD prevalence. More studies with larger sample sizes are necessary. Recruiting patients from a medical camp possibly contributed to the high prevalence of PAD and its risk factors. We could not use gold standard color Doppler studies for diagnosing PAD due to lack of resources.
6. Conclusion
The prevalence of PAD in the Indian population is understudied. Defining the population at risk and using ABI as an early screening tool would help in prompt treatment and prevent further complications. ABI is a simple and low-cost tool to aid screening for disease.
Conflict of interest
None.
Funding source
None.
Acknowledgement
None.
References
- 1.Criqui M.H., Denenberg J.O., Langer R.D., Fronek A. The epidemiology of peripheral arterial disease: importance of identifying the population at risk. Vasc Med. 1997;2:221–226. doi: 10.1177/1358863X9700200310. [DOI] [PubMed] [Google Scholar]
- 2.Hiatt W.R., Hoag S., Hamman R.F. Effect of diagnostic criteria on the prevalence of peripheral arterial disease. The San Luis Valley Diabetes Study. Circulation. 1995;91:1472–1479. doi: 10.1161/01.cir.91.5.1472. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch A.T., Haskal Z.J., Hertzer N.R. ACC/AHA Guidelines for the Management of Patients with Peripheral Arterial Disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Associations for Vascular Surgery/Society for Vascular Surgery, Society. J Vasc Interv Radiol. 2006;17:1383–1397. doi: 10.1097/01.RVI.0000240426.53079.46. [quiz 1398] [DOI] [PubMed] [Google Scholar]
- 4.Newman A.B., Siscovick D.S., Manolio T.A. Ankle-arm index as a marker of atherosclerosis in the cardiovascular health study. Circulation. 1993;88:837–845. doi: 10.1161/01.cir.88.3.837. [DOI] [PubMed] [Google Scholar]
- 5.Fowkes F.G.R., Rudan D., Rudan I. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet (London, England) 2013;382:1329–1340. doi: 10.1016/S0140-6736(13)61249-0. [DOI] [PubMed] [Google Scholar]
- 6.Aboyans V., Criqui M.H., Abraham P. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012;126:2890–2909. doi: 10.1161/CIR.0b013e318276fbcb. [DOI] [PubMed] [Google Scholar]
- 7.Criqui M.H., Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015;116:1509–1526. doi: 10.1161/CIRCRESAHA.116.303849. [DOI] [PubMed] [Google Scholar]
- 8.Solanki J.D., Makwana A.H., Mehta H.B., Gokhale P.A., Shah C.J. A study of prevalence and association of risk factors for diabetic vasculopathy in an urban area of Gujarat. J Fam Med Prim Care. 2013;2:360–364. doi: 10.4103/2249-4863.123906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Premalatha G., Shanthirani S., Deepa R., Markovitz J., Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: the Chennai Urban Population Study. Diabetes Care. 2000;23:1295–1300. doi: 10.2337/diacare.23.9.1295. [DOI] [PubMed] [Google Scholar]
- 10.Sarangi S., Srikant B., Rao D.V., Joshi L., Usha G. Correlation between peripheral arterial disease and coronary artery disease using ankle brachial index–a study in Indian population. Indian Heart J. 2012;64:2–6. doi: 10.1016/S0019-4832(12)60002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nag F., De A., Hazra A., Chatterjee G., Ghosh A., Surana T. Chronic venous ulceration of leg associated with peripheral arterial disease: an underappreciated entity in developing country. Int Wound J. 2014;11:546–549. doi: 10.1111/iwj.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]