Abstract
Objective
High salt diet increases blood pressure. Tea garden workers (TGW) of Assam, India have high (60.8%) prevalence of hypertension (HTN), which may be due to consumption of extra salt (salt as side dish) and salted tea at work place and home. The present study evaluated an information, education and communication (IEC) module to reduce salt intake and blood pressure among TGW.
Methods
Two tea gardens (usual care and intervention) were selected at random covering a total population of 13,458. The IEC module consisting of poster display, leaflets, health rally, documentary show, individual and group discussion was introduced in the intervention garden targeting study participants, health care providers, key stake holders, school children and teachers. IEC intervention was continued for one year. Participants from usual care and intervention were followed at three monthly intervals and BP and other information were compared after one year.
Results
A total of 393 study participants (Non intervention: 194; intervention: 199) were included. After one year of follow up, consumption of extra salt was reduced significantly in the intervention participants (66.3 vs. 45.5%, p = 0.000). Intention to treat analysis revealed significant reduction in systolic [−6.4 (−8.6 to −4.2)] and diastolic [−6.9 (−8.1 to −5.7)] blood pressure after one year. Prevalence of HTN was reduced significantly (52.5 vs. 40.0%, p = 0.02) among them.
Conclusions
Our IEC module created awareness about risk of hypertension associated with high salt intake and could reduce dietary salt intake and BP.
Keywords: Blood pressure, Dietary salt, Hypertension, Tea garden worker
1. Introduction
Hypertension (HTN) is the most prevalent non-communicable disease in both developed and developing countries including India.1, 2, 3 It contributes to 7.1 million global deaths and 64.3 million losses of disability-adjusted life years (DALYs).4 About 16% ischemic heart disease, 21% peripheral vascular disease and 24% acute-myocardial-infarction (AMI) cases are attributed to HTN.5 It is a preventable and treatable disease that can be achieved by adopting healthy diet and life styles with or without antihypertensive medications. By controlling blood pressure a significant portion of cardiovascular complications can be minimized.6 It was revealed that population based reduction in diastolic pressure by 2 mm Hg reduces the risk of stroke and transient ischemic attacks by 15% and coronary heart disease by 6%.7
INTERSALT and INTERMAP studies have shown that dietary sodium intake by most adult population in developing world are higher (up to 200 mmol/day) than the amount (≤100 mmol/day) recommended by Joint National Committee-VII.8, 9, 10 Reducing sodium intake from 150 mmol/day to 100 mmol/day or lower (65 mmol/day) can cause a stepwise reduction in BP.10 Such blood pressure reduction following dietary salt restriction is also evidenced in the dietary approaches to stop Hypertension (DASH) study.11 A community based study on reduction of dietary salt intake and blood pressure revealed significant reduction in BP.12
A meta-analysis of thirty-four trials including 3230 participants revealed signification reduction of blood pressure following dietary salt restriction.13 Trials of Hypertension Prevention (TOHP) phases I and II also revealed reduction in blood pressure following dietary salt restriction.14 Recently, WHO had initiated steps toward reducing the global population’s intake of salt about 30% by 2025.15
All these studies have shown consistent reductions in blood pressure but controversy still arises regarding the magnitude of fall in blood pressure in different population groups.16 Therefore, it is difficult to generalize recommendation for dietary salt restriction for reduction of blood pressure in the community.
Tea garden workers (TGW) of Assam migrated from central India (Madhya Pradesh, Andhra Pradesh, Orissa and Jharkhand) to Assam during the pre-independence time to work in tea plantation.17 At present, they are mostly settled in different tea gardens of Assam without massive admixture with indigenous Assamese population. TGW living in different gardens have similar health care facility, ethnicity of population, socio economic status, cultural background, dietary behavior (especially salt intake), lifestyle and custom. Hence, tea garden population between the gardens is well matched.
As an age-old practice, TGW consume salted tea at home and work site during tea plucking which is provided by garden management. Salted tea at workplace contains about 8–10 gm salt/l and TGW usually consume about 800–1000 ml per day during summer season. Prevalence of hypertension in this community is high (60.8%) and consumption of extra salt (salt as a side dish) during meal was found to be a risk factor for hypertension.18 Prevalence of salt sensitivity phenotype is also high in TGW (manuscript accepted for publication by Natl. Med. J. India).
Community based intervention for dietary salt restriction may modify the habit of high salt consumption and reduce blood pressure. A recent review of behavioral change interventions to reduce population salt intake reveals that population-level behavior change interventions can improve salt-related behaviors and/or reduce salt intake.19 Further, a review of reviews shows positive results in changing health behaviors through community intervention.20 In the present study, we have depicted the effect of information, education and communication (IEC) module on reduction of dietary salt intake and blood pressure in tea garden workers.
2. Materials and methods
2.1. Study area
The present study was carried out during 2012–2014 in two tea gardens selected purposively as intervention where IEC module was introduced and as usual care garden. Both the gardens were run by the same management having equivalent health care facilities and had the distance of about 8 km to avoid contamination.
2.2. Study population and sample size
The total population of the gardens were 13,458 (control garden: 7112, intervention garden: 6346). Sample size for the study was calculated using “Open Epi” software21 and based on assumption of difference of systolic blood pressure 5 mmHg between the groups with standard deviation (SD) 15, 80% power and 5% level of significance. The estimated sample size was 142 in each arm or group. Including 35% (n = 50), loss during follow up a total of 192 participants were targeted in each groups.
2.3. Recruitment of study participants
The present study was approved by Institutional Ethics Committee of Regional Medical Research Centre (Indian Council of Medical Research), Dibrugarh. Tea garden workers (>= 18 years) of both sex was eligible to participate in the study. All the consecutive subjects attending temporary clinic organized at field and garden hospital for free blood pressure check-up and providing informed consent were recruited. Subjects with elevated serum creatinine (male > 1.5 mg% and female > 1.4 mg%), positive urinary protein, subjects with history of acute myocardial infarction, stroke and congestive heart failure, diabetes, dissecting aneurysm, malignancy, hepatic disorder and pregnancy were excluded from the study.
2.4. Instruments and target groups for IEC intervention
The components of the IEC module were counselling (individual and group) and motivational campaign, meetings, posters, small booklet, health rally and audiovisual aids in the form of documentary film. Our module acted based on trans-theoretical model for behavior change, namely, consciousness raising, self-reevaluation, self-liberation, reinforcement, helping relationships and social liberation.22, 23 The module was introduced in the intervention garden targeting five different groups for a period of one year (Table 1).
Table 1.
Different levels of IEC intervention.
| Target population | Focused area of discussion & Methodology applied | Key message | |
|---|---|---|---|
| Level 1 | General Manager, Manager, Assistant Manager and Welfare Officer |
|
Restrict salted tea at work place |
| |||
| |||
| |||
| |||
| Level 2 | Medical officer and staff of the garden hospital |
|
Dietary salt restriction is required for healthy heart |
| |||
| |||
| Level 3 | Key stake holders including union, religious leaders, NGOs, school teachers and other welfare organization |
|
Restrict dietary salt by avoiding salted tea and salt as side dish |
| |||
| |||
| |||
| |||
| Level 4 | Motivational and awareness programme for school children |
|
Restrict dietary salt for yourself and your parents to control blood pressure |
| |||
| |||
| |||
| |||
| Level 5 | Study participants and community by and large |
|
Restrict dietary salt by avoiding salted tea and salt as side dish |
| |||
| |||
| |||
| |||
| |||
2.4.1. Level 1: counselling and motivational campaign for the garden management
The target population was management staff (General-Manager, Manager, Assistant-Manager and Welfare Officer). Garden management supplies salted tea to the workers at work place, which constitute about 6–8 gm/1000 ml of salt in water. During this phase, burden of HTN and loss of garden exchequer in terms of wage loss, productivity and health care cost was discussed. The group was informed about the relation of high salt intake and hypertension and consequences of HTN. Tea garden management was requested to stop supplying salted tea at work place and make an alternative arrangement. The meeting was ended with a take home message “Stop supplying salted tea at work place”.
The garden management with the support of all level of participants could stop supplying salted tea at work place. Garden authority first started supplying plain tea with extra salt in separate container with a rider “salt is risky, don’t take in tea”. Gradually they discontinued supplying salt during the course of the study period. Awareness of the people about risk of hypertension associated with high salt consumption helped the management to stop supplying salted tea. The hospital staffs of the intervention garden counseled all the attending patients and their attendants and disseminated our message to restrict high salt consumption. Before intervention, counseling and motivational campaign for the garden management was held at monthly intervals, which were followed by six monthly review meeting.
2.4.2. Level 2: health care providers (Medical-officer and other paramedical staffs of the garden hospital)
Health care provider forms a major motivational force for health related issues in the community. Therefore, motivational meeting among the medical officers and paramedical staffs were held to discuss about the burden and risk factors of HTN among TGW. They were requested to disseminate the message of health risk associated with high salt intake and benefit from dietary salt restriction to the attending participants and the attendants. The session was ended with a key message “Dietary salt restriction is required for healthy heart”. This was conducted at three-monthly intervals.
2.4.3. Level 3: key stake holders
Meeting and group discussion were organised among the key stake holders including Line chowkidars, members of Mother Club, Employee’s Union leaders, School teacher and religious leaders to discuss health hazards of high salt intake and HTN. Special posters displaying healthy and unhealthy foods, documentary show were organized and explained in the forum. The session was ended with a take home message “Restrict dietary salt by avoiding salted tea and salt as side dish”. This was conducted at three-monthly intervals.
2.4.4. Level 4: school children as ambassador for salt restriction programme in the garden
Children can carry message to their home if they are convinced. Lectures and documentary show were organised and posters for healthy diet was displayed in school. Health rally with a slogan “Restrict dietary salt for yourself and your parents to control blood pressure” was organized. This was conducted at three-monthly intervals.
2.4.5. Level 5: IEC for study participants
Recruited study participants were contacted personally and they were counseled to avoid high dietary salt consumption. Various components of our IEC module were introduced to the individual participants or group of participants as applicable and the whole community. Recipes of tea-garden community were discussed and amount of salt present in the recipes were highlighted. High salt consumption and its relation with HTN, complications of hypertension including stroke and heart attack were explained to them. The recommended daily amount of dietary salt advised by scientific bodies likes WHO and JNC-VII were also informed to the participants and the population. “Avoid salted tea, extra salt and packaged food containing high salt”. The IEC activities were targeted to the recruited subjects and the total population by enlarge. The coverage of IEC module was 100% for the recruited participants and about 80% for the remaining population of the intervention garden. Exposure of IEC module was given at least once in three monthly intervals. This was conducted at three-monthly intervals.
2.5. Non intervention (control) garden
Baseline data were collected and appropriate medical advices as per existing medical practices were given to hypertensive participants.
2.6. Collection of data
Baseline information of the participants (control and intervention) including age, type of work, smoking habit, consumption of alcohol, consumption of extra salt, salted tea at work place and home were recorded by personal interview. Blood pressure was checked using electronic blood pressure monitor (Omron, model HEM 907) following standard guidelines. We took three readings at an interval of 5–10 min for each participant and the average of last two readings was used for analysis. Height and weight were recorded by trained person using standard methodologies. Anthropometric rod and platform balance (SECA) were used to measure height and weight respectively. Body mass index (BMI) was calculated as weight in kg divided by height in meter squared.
2.7. Follow up assessment
Participants of each study group (control and intervention) were assessed at three monthly intervals to observe any change in BP of the participants. Final assessment was carried out after one year of follow up (final follow up). Collection of socio-demographic, and clinical information was repeated at final follow up.
2.8. Statistical analysis
We used Statistical Package for Social Science (SPSS) version 17.0. (SPSS for windows, version 12.0.1.2001 SPSS Inc, Chicago, USA) for all analysis.24 General linear model (univariate) was used to carry out intention to treat and per protocol analysis. For intention to treat analysis, we assigned cluster specific mean blood pressure values of participants who completed final follow up (n = 346) to those (n = 47) with missing blood pressure values at final follow up.25, 26 We also carried out per protocol analysis, after excluding lost to follow up participants at final follow up. We presented mean difference of blood pressure (SBP & DBP) between the intervention and control group after adjusting for age, sex and base line values of SBP and DBP. For all analysis, p values <0.05 was regarded as significant.
3. Results
3.1. Changes in dietary salt intake, blood pressure and prevalence of hypertension
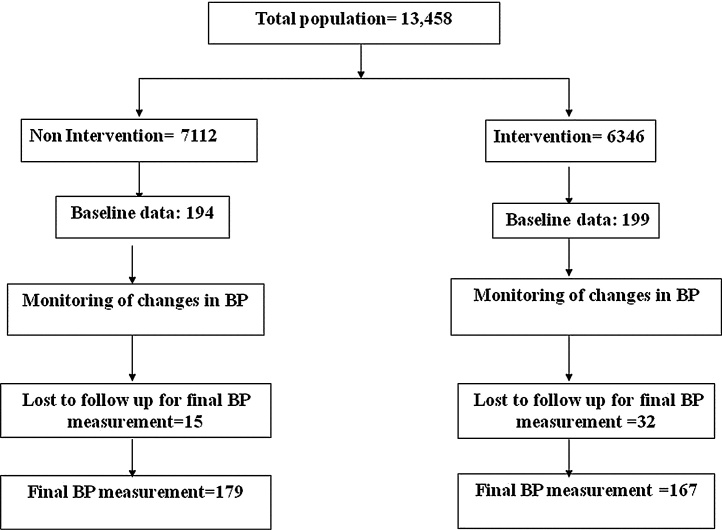
Our study included 393 (control: 194 and intervention: 199) subjects from the two gardens (Fig. 1). Out of them, 47 (15 control, 32 intervention) subjects were lost to follow up and blood pressure readings could not be recorded. Base line mean blood pressure levels of participants with missing versus non missing blood pressure values at final follow up did not show any significant differences (P > 0.05).
Fig. 1.
Represents the flow chart of study design.
Table 2 represents the distribution of socio-demographic variables among the subjects. After one year of follow up, the practice of consuming extra salt during meal had been reduced significantly in the intervention participants (66.3 vs. 45.5%, p = 0.000). Both systolic (139.2 ± 18.8 vs. 134.7 ± 20.9, p = 0.055) and diastolic (81.3 ± 9.5 vs. 78.6 ± 11.01, p = 0.025) blood pressures were higher among participants consuming extra salt.
Table 2.
Baseline socio-demographic and clinical variables in non- intervention vs. intervention TGW subjects.
| Variables | Non Intervention (N = 194) | Intervention (N = 199) | p values |
|---|---|---|---|
| Male, N (%) | 109 (56.2) | 97 (48.7) | 0.084 |
| Age, years (mean ± SD) | 40.4 ± 15.5 | 44.5 ± 14.4 | 0.06 |
| Educational status N (%) | |||
| Illiterate | 113 (58.2) | 108 (54.3) | 0.139 |
| Primary | 64 (33.3) | 82 (41.2) | |
| Higher secondary and above | 17 (8.7) | 9 (4.5) | |
| Monthly income (Rs) | |||
| Up to 2000 | 74 (38.1) | 105 (52.8) | 0.009 |
| 2000 to 3000 | 30 (15.5) | 15 (7.5) | |
| 3000 | 15 (7.8) | 19 (9.5) | |
| Not applicable | 75 (38.7) | 60 (30.2) | |
| Physical activity, N (%) | |||
| Light | 27 (13.9) | 42 (21.1) | 0.000 |
| Moderate | 144 (74.2) | 71 (35.7) | |
| Heavy | 23 (11.9) | 86 (43.2) | |
| Dietary salt as a side dish, N (%) | 140 (72.2) | 132 (66.3) | 0.126 |
| Tobacco consumption, N (%) | 130 (67.0) | 143 (71.9) | 0.175 |
| Alcohol consumption, N (%) | 107 (55.2) | 127 (63.8) | 0.05 |
| Smoking, N (%) | 13 (6.7) | 17 (8.5) | 0.031 |
| BMI, (mean ± SD) | 19.2 ± 2.5 | 18.1 ± 2.4 | 0.572 |
| SBP, mmHg (mean ± SD) | 141.6 ± 19.5 | 140.4± 26.9 | 0.711 |
| DBP, mmHg (mean ± SD) | 84.2 ± 12.0 | 84.8 ± 14.5 | 0.674 |
| Hypertension, N (%) | 114 (58.8) | 105 (52.8) | 0.264 |
Prevalence of hypertension was also found to be reduced significantly (52.5 vs. 40.0%). However, there was no significant changes of these parameters among non intervention participants.
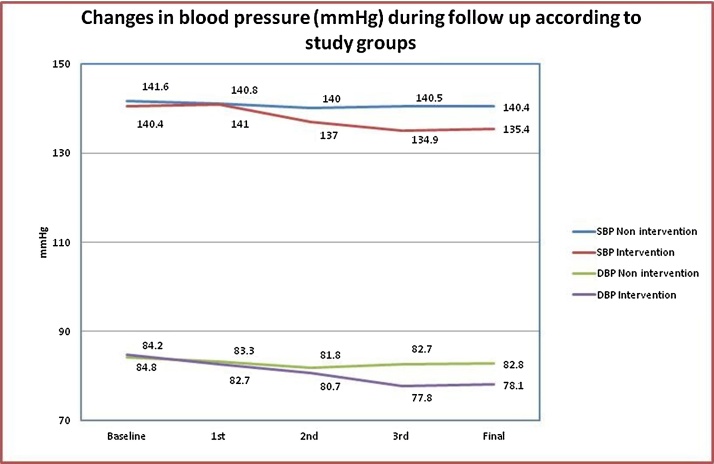
The intervention participants revealed gradual decline of blood pressure measured at three monthly intervals during one year follow up. The non intervention participants showed only moderate change of these parameters (Fig. 2).
Fig. 2.
Represents distribution of blood pressure (SBP & DBP) during follow up.
In intention to treat analysis, blood pressure at 95% confidence interval and adjusted for age and sex showed significant reduction of systolic [−6.4 (−8.6 to −4.2)] and diastolic [−6.9 (−8.1 to −5.7)] blood pressure (Table 3).
Table 3.
Change (95% confidence interval) in blood pressure.
| Clinical parameters | Non intervention | Intervention | p value |
|---|---|---|---|
| Intention to treat analysis | |||
| SBP, mmHg at final follow upa | 141.1 (138.9–143.3) | 134.6 (132.5–136.8) | 0.000 |
| DBP, mmHg at final follow upa | 83.3 (82.1–84.5) | 77.6 (76.4–78.8) | 0.000 |
| Difference in SBP, mmHg (Final follow up – Baseline value)a | −1.1 (−2.2 to 2.2) | −6.4 (−8.6 to −4.2) | 0.000 |
| Difference in DBP, mmHg (Final follow up – Baseline value)a | −1.0 (−2.3 to 0.2) | −6.9 (−8.1 to −5.7) | 0.000 |
| Per protocol analysis | |||
| SBP, mmHg at final follow upa | 141.9 (139.6–144.3) | 133.6 (131.1–136.0) | 0.000 |
| DBP, mmHg at final follow upa | 83.6 (82.3–84.9) | 77.2 (75.8–78.6) | 0.000 |
| Difference in SBP, mmHg (Final follow up – Baseline value)a | 0.2 (−2.2 to 2.6) | −8.2 (−10.6 to −5.7) | 0.000 |
| Difference in DBP, mmHg (Final follow up – Baseline value)a | −1.2 (−2.5 to 0.1) | −7.6 (−8.1 to −6.2) | 0.000 |
Adjusted for age, sex and baseline blood pressure, smoking, physical activity and alcohol consumption.
Table 3 also reveals mean change in blood pressure based on per protocol analysis. There was significant reduction of mean systolic (−8.2 in intervention vs. 0.2 mmHg in non-intervention participants, p = 0.000) and diastolic pressure (−7.6 in intervention vs. −1.2 mmHg non-intervention participants, p = 0.000). All analysis was adjusted for age, sex and baseline blood pressure, smoking, physical activity and alcohol consumption.
4. Discussion
Our intervention module targeted two issues, supply of salted tea at work place by the garden management and consumption of high salt in different forms (salt as a side dish and salted tea during meal) by the TGW. Management were counseled to stop supply of salted tea at work place by highlighting the adverse effect associated with high salt consumption. Tea garden workers were informed about the harmful effect of extra salt in diet and salted tea and convinced to avoid these unhealthy dietary practices. As a part of our intervention, tea garden management stopped supplying salted tea at workplace with full support from the community and union leaders, mother club members, village head and the community as a whole. Such initiative of the garden management can be regarded as a “paternalistic nudge” or Libertarian paternalism as it can be legitimized for implementation of salt restriction program for the paramount interest of the people while respecting freedom of choice to accept or not to accept. The workers also had the freedom to use salt at work place which was supplied separately (not mixed with tea as done traditionally) but with a precautionary rider “Salt is risky, don’t take in tea”.
Present study reveals that dietary salt restriction through IEC module is possible in the context of TWG. Earlier study revealed association of extra salt with HTN in TGW.18 Reduction of dietary sodium consumption reduces blood pressure and result in decrease vascular risk associated with HTN.27 Our study has revealed that dietary salt restriction was associated with reduction of systolic and diastolic BP and prevalence of HTN (52.5 vs. 40.0%, p = 0.02). Compliance to salt restriction was evidenced by habitual change in dietary intake.
Meta-analysis of different controlled trials revealed reduction of SBP and DBP to an extent of 5.4 and 6.5 mmHg respectively following restriction of sodium intake to 100 mmol/24 h.28 Decreased dietary sodium consumption was associated with reduction of DBP with a decreased risk of vascular complications.29, 30
The salt-genetics hypothesis states that excessive salt intake in susceptible individuals may lead to development of HTN.31 However, the linear relation between sodium intake and BP is inconsistent.29, 30, 31, 32 Inconsistency between BP and dietary salt consumption may be ascribed to inadequacy of linear model due to geographical, environmental and population heterogeneity and complex interplay of gene-environment interaction.28, 29, 30, 31, 32 Our study was done in an ethnically homogenous population that revealed linear downward trend of reduction of blood pressure with reduction of salt consumption.
Although, life style modification and alteration of habit are economically attractive yet very difficult to implement at community level. Moderate salt restriction result in a leftward shift of the blood pressure distribution in the community and therefore it results in a considerable reduction of cardiovascular morbidity and mortality.33 The present study showed positive impact on three major behaviours of the study participants: The garden management could stop providing salted tea at the work place which contributed a substantial reduction in daily salt consumption by the study participants. Habit of taking extra salt during meal and salted tea had been reduced significantly. Tea garden workers are economically poor and they have limited access to costlier package food items that contains high amount of salt. Therefore, behavioral modifications carried out by the present study with significant reduction of BP has significant translational values. Application of this intervention module to all the TGW (about 5 million contributing 16% of total population) may reduce a significant burden of HTN.
Our study had some limitations. We have not checked 24 h urinary sodium to correlate reduction in dietary intake of salt by the study participants. Our study was conducted in community settings without hampering day-to-day activities of the study participants. Some amount of contamination by sharing health promotional message between intervention and non intervention garden cannot be ignored. Perhaps for this reason a negligible amount of fall in BP had been observed in the nonintervention garden also. Further, our module may not be applicable to the general population who don’t use extra salt and salted tea. In spite of these, reduction of blood pressure through modification of high risk behavior (high dietary salt intake) has practical implications for TGW and needs to be promoted. Larger studies in this direction will validate our study.
What is already known on this subject?
Dietary sodium intake by most adult population in developing world is higher than the recommended, which is a potent cause of hypertension. Reducing sodium intake can cause a stepwise reduction in blood pressure.
Tea garden workers also possess the habit of consuming high dietary salt and found to be associated with high risk of hypertension. Tea garden management believed that heavy sweating of workers during tea plucking in the sun causes salt loss and to keep the vigor they need salt supplementation. Hence, these workers were given salted-tea freely to drink. This habit continued across the tea gardens of Assam for ages. Further, they have a habit of taking extra salt along with every meal.
What does this study add?
Community based intervention to change the aged old practice and life style is difficult. We tried a multilevel community based intervention module to reduce consumption of dietary salt through counseling IEC activities involving various levels of people in the study tea garden. Our study revealed significant reduction of dietary salt intake, blood pressure and prevalence of hypertension among the tea garden workers. The study has translational values as application of this intervention module to all the tea gardens of Assam may reduce the burden of HTN.
Funding
We sincerely acknowledge Indian Council of Medical Research, New Delhi for funding of this study.
Declaration of interest
We declare that there are no known conflicts of interest associated with this publication and there has been no financial interest for this work that could have influenced the outcome of the study.
Acknowledgments
We acknowledge technical support and critical evaluation by the members of different Scientific Review Committee. We acknowledge the persistent help of Munmi Rajkhowa for IEC activities and other project staffs during field and laboratory works. Medical Officer and other staffs of tea garden hospital, and garden management officials deserve special thanks for their logistic support. Finally, we deeply acknowledge all the enrolled participants of the study.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.ihj.2017.08.008.
Contributor Information
Prasanta K. Borah, Email: prasant47@yahoo.com.
Hem C. Kalita, Email: kalita_hc@rediffmail.com.
Suman K. Paine, Email: painesuman01@gmail.com.
Purnananda Khaund, Email: purnananda.khaund@amalgamated.in.
Chandra Bhattacharjee, Email: chandrabhattacharya111@gmail.com.
Dilip Hazarika, Email: hazarikad@rediffmail.com.
Meenakshi Sharma, Email: smeenakshi@hotmail.com.
Jagadish Mahanta, Email: jmahanta@gmail.com.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anchala R., Kannuri N.K., Pant H. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forouzanfar M.H., Liu P., Roth G.A. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA. 2017;317(2):165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 4.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–78. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 5.Subramanian H., Soudarssanane M.B., Jayalakshmy R. Non-pharmacological interventions in hypertension: a community-based cross-over randomized controlled trial. Indian J Commun Med. 2011;36(July (3)):191. doi: 10.4103/0970-0218.86519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.King D.E., Mainous A.G., Geesey M.E. Turning back the clock: adopting a healthy lifestyle in middle age. Am J Med. 2007;120:598–603. doi: 10.1016/j.amjmed.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Cook N.R., Cohen J., Hebert P.R., Taylor J.O., Hennekens C.H. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709. [PubMed] [Google Scholar]
- 8.Assessment of burden of non-communicable diseases in India. Final report of Project WR/SE IND RPC 001 RB 02. SE/02/419575. New Delhi: Indian Council of Medical Research; 2004, http://www.whoindia.org/LinkFiles/AssessmentofburdenofNCDHypertensionAssessmentofBurdenofNCDs.pdf (27 August, 2009, accessed 10 July, 2014).
- 9.Pietinen P., Uusitalo U., Nissinen A. INTERSALT: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988;297(6644):319–328. doi: 10.1136/bmj.297.6644.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chobanian A.V., Bakris G.L., Black H.R. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 11.Appel Lawrence J., Brands Michael W., Daniels Stephen R., Karanja Njeri, Elmer Patricia J., Sacks Frank M. Dietary approaches to prevent and treat hypertension. A Scientific Statement from the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 12.Forte J.G., Miguel J.M., Miguel M.J., de Pádua F., Rose G. Salt and blood pressure: a community trial. J Hum Hypertens. 1989;3:179–184. [PubMed] [Google Scholar]
- 13.He F.J., Li J., Macgregor G.A. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. doi: 10.1136/bmj.f1325. [DOI] [PubMed] [Google Scholar]
- 14.Susan Hedayati S., Elsayed Essam F., Reilly Robert F. Non-pharmacological aspects of blood pressure management: what are the data? Kidney Int. 2011;79:1061–1070. doi: 10.1038/ki.2011.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO Media Centre . 2016. Salt Reduction.www.who.int/mediacentre/factsheets/fs393/en/ [Google Scholar]
- 16.Jones Daniel W. Dietary sodium and blood pressure. Hypertension. 2004;43:932–935. doi: 10.1161/01.HYP.0000126610.89002.c6. [DOI] [PubMed] [Google Scholar]
- 17.Griffith P. Weiden & Nicolson; London: 1997. The History of Indian Tea Industry. [Google Scholar]
- 18.Hazarika N.C., Biswas D., Narain K., Kalita H.C., Mahanta J. Hypertension and its risk factors in tea garden workers of Assam. Natl Med J India. 2001;15:63–68. [PubMed] [Google Scholar]
- 19.Trieu K., McMahon E., Santos J.A. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. 2017;14:17. doi: 10.1186/s12966-017-0467-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jepson Ruth G., Harris Fiona M., Platt Stephen, Tannahill Carol. The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health. 2010;10:538. doi: 10.1186/1471-2458-10-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sullivan K.M., Dean A., Soe M.M. On academics: OpenEpi. a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124:471–474. doi: 10.1177/003335490912400320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prochaska James O., Di Clemente Carlo C., Norcross John C. In search of how people change applications to addictive behaviours. Am Psychol. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 23.Abraham C., Michie S. A taxonomy of behaviour change techniques used in interventions. Health Psychol. 2008;27(3):379–387. doi: 10.1037/0278-6133.27.3.379. 0278-6133/08/$12.00. [DOI] [PubMed] [Google Scholar]
- 24.Inc SP. SPSS statistics for Windows version 17 0. Chicago. Released; 2008.
- 25.Taljaard M., Donner A., Klar N. Imputation strategies for missing continuous outcomes in cluster randomized trials. Biometr J. 2008;50:329–345. doi: 10.1002/bimj.200710423. [DOI] [PubMed] [Google Scholar]
- 26.Jafar T.H., Islam M., Hatcher J. Community based lifestyle intervention for blood pressure reduction in children and young adults in developing country: cluster randomized controlled trial. BMJ. 2010;340:c2641. doi: 10.1136/bmj.c2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aburto N.J., Ziolkovska A., Hooper L., Elliott P., Cappuccio F.P., Meerpohl J.J. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. doi: 10.1136/bmj.f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 29.Alderman M.H. Reducing dietary sodium: the case for caution. JAMA. 2010;303:448–449. doi: 10.1001/jama.2010.69. [DOI] [PubMed] [Google Scholar]
- 30.Staessen J.A., Lijnen P., Thijs L., Fagard R. Salt and blood pressure in community-based intervention trials. Am J Clin Nutr. 1997;65:661S–670S. doi: 10.1093/ajcn/65.2.661S. [DOI] [PubMed] [Google Scholar]
- 31.Kunes J., Kadlecova M., Zicha J. Genes and Cardiovascular Function. Springer; US: 2011. Gene-environment interactions their role in hypertension development; pp. 177–184. [Google Scholar]
- 32.Kolata G.I. New York Times; 2013. No Benefit Seen in Sharp Limits on Salt in Diet; p. 15. May 14. [Google Scholar]
- 33.Ha S.K. Dietary salt intake and hypertension. Electrol Blood Press. 2014;12:7–18. doi: 10.5049/EBP.2014.12.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.