Abstract
Purpose
Standardized care via a unified surgeon preference card for pediatric appendectomy can result in significant cost reduction. The purpose of this study was to evaluate the impact of cost and outcome feedback to surgeons on value of care in an environment reluctant to adopt a standardized surgeon preference card.
Methods
Prospective observational study comparing operating room (OR) supply costs and patient outcomes for appendectomy in children with 6-month observation periods both before and after intervention. The intervention was real-time feedback of OR supply cost data to individual surgeons via automated dashboards and monthly reports.
Results
216 children underwent laparoscopic appendectomy for non-perforated appendicitis (110 pre-intervention and 106 post-intervention). Median supply cost significantly decreased after intervention: $884 (IQR $705–$1025) to $388 (IQR $182–$776), p < 0.001. No significant change was detected in median OR duration (47 minutes [IQR 36–63] to 50 minutes [IQR 38–64], p = 0.520) or adverse events (1 [0.9%] to 6 [4.7%], p = 0.062). OR supply costs for individual surgeons significantly decreased during the intervention period for 6 of 8 surgeons (87.5%).
Conclusion
Approaching value measurement with a surgeon-specific (rather than group-wide) approach can reduce OR supply costs while maintaining excellent clinical outcomes.
Keywords: Pediatric appendectomy, Value-based care, Cost reduction
1. INTRODUCTION
Value-based surgical care (outcomes per dollars spent) emphasizes both quality and efficiency in the care of surgical patients. Rising costs, regulatory requirements, and consumer demand are encouraging hospitals and providers to evaluate the value of care provided by measuring costs, tracking outcomes, and providing these data to the public.[1–4] Meanwhile, surgeon preference for differing supplies in the operating room (OR) has been shown to contribute to significant variability in the costs of operations without apparent differences in outcomes.[5–7]
While the importance of measuring costs is widely accepted, relatively few studies have examined the effect of surgeon decision-making on healthcare expenditures.[8] Most surgeons desire to limit costs, yet few have knowledge of hospital costs for each procedure they perform or how their costs compare to that of their colleagues.[8, 9] Recent work suggests that surgeons may choose a lower-cost surgical supply in the OR when presented with costs of potential alternatives.[10–12] The limitation of these studies is that the majority evaluated surgeon behavior after providing aggregated data on a periodic basis [11, 12], while few have measured changes in practice patterns when surgeons were presented real-time, patient-level cost data.[10]
Acquisition of patient-level cost data by surgeons is difficult in most healthcare systems as costs are either not available or aggregated over time or departmentally, rather than provided at the patient-level.[1, 8, 13, 14] We have previously shown that institution of a clinical practice guideline (CPG) for perforated appendicitis resulted in a decrease in variability of care, improvement in clinical outcomes, and decrease in overall cost of care.[14, 15] This CPG did not incorporate any intraoperative changes, such as standardization of OR equipment or incentives for OR cost reduction. Variability in surgical technique and OR supplies for laparoscopic procedures is common.[16–19] Prior publications have reported that standardization of intraoperative device utilization with a unified surgeon preference card resulted in significant cost reduction for pediatric appendectomy.[19, 20] As supplies consist of the greatest proportion of consumable costs in the process of care for pediatric appendectomy[21], they are an important target for potential value improvement. Mandating use of specific OR supplies is not feasible in many surgical practices. The purpose of this study was to evaluate the impact of cost and outcome data feedback to individual surgeons on value of care in an environment reluctant to adopt a standardized surgeon preference card for appendectomy.
2. METHODS
We performed a prospective observational study comparing OR supply costs and patient outcomes for children undergoing appendectomy before and after an intervention to provide surgeons with patient-level, real-time cost data.
2.1 Subjects and setting
The study population consisted of all children treated for non-perforated appendicitis by laparoscopic appendectomy at the Monroe Carell, Jr. Children’s Hospital at Vanderbilt, a 271-bed, freestanding, tertiary referral center affiliated with Vanderbilt University Medical Center in Nashville, TN during a 6-month period before intervention (January 1, 2016 to June 30, 2016) compared to a 6-month period following intervention (October 1, 2016 to March 31, 2017). All children 18 years of age or younger who underwent laparoscopic appendectomy during these time periods were prospectively identified and tracked within Tableau software, a database management software that provides interactive data visualization and analytics.[22] To decrease bias in our two patient cohorts, children were excluded if the laparoscopic case was converted to open or if perforated appendicitis was identified. Electronic medical records were reviewed manually by three reviewers (JRR, NHC, CG) with a fourth reviewer (MLB) involved to address discrepancies. Perforated appendicitis was determined by review of the operative note and defined as fecalith extrusion or a visible hole in the appendix. Children with gangrenous appendicitis were included as non-perforated appendicitis. The institutional review board approved the study with waiver of informed consent.
2.2 Intervention
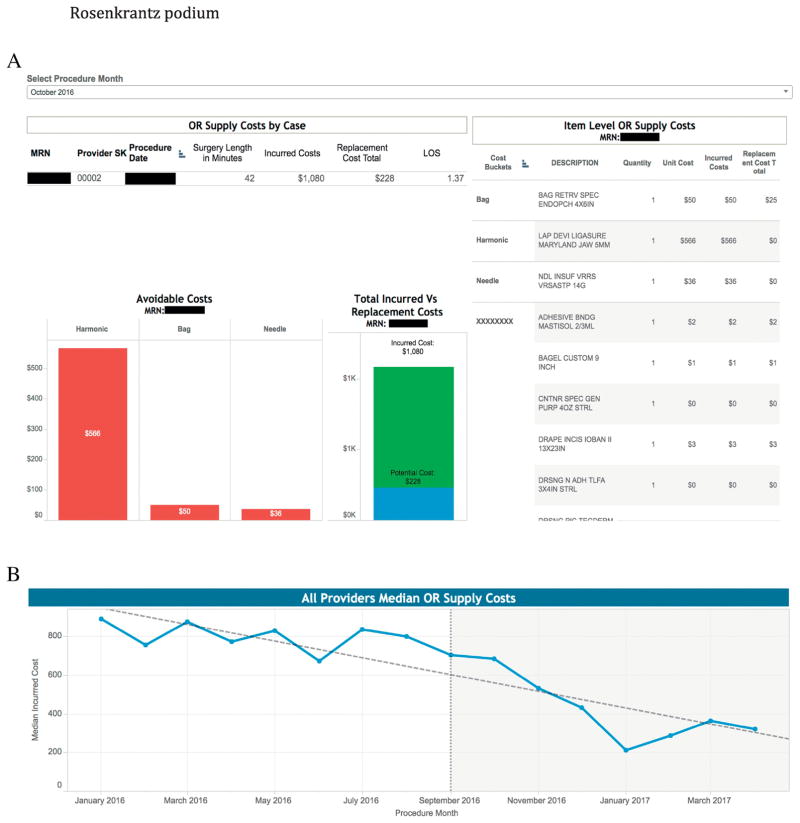
The intervention was real-time feedback of OR supply cost data to individual surgeons via automated dashboards and monthly reports. An automated Tableau dashboard was created, which utilized data extracted from a “point of use (POU)” cost accounting system and database. The POU system was a standard part of the OR charting performed by the OR circulating nurses and accounted for all supplies used during each operation. Variables displayed in the Tableau dashboard (within 48 hours after the operation) included the specific surgeon, procedure duration, hospital length of stay (LOS), and full supply cost data for each operation (Figure 1a). Within Tableau, graphs were created to visualize overall costs for the entire group (Figure 1b) and each surgeon’s average OR supply costs over time.
Figure 1.
Representative views of Tableau dashboard to visualize data for appendectomy cost reduction intervention. (A) Dashboard visualization of OR supply costs for a single case, along with individual supply costs and avoidable costs, representing opportunities for cost reduction. (B) Dashboard visualization showing the reduction in overall median OR supply costs before and after intervention.
Each surgeon’s baseline OR supply use (during the 6-month period before intervention) was compiled to inform opportunities for cost reduction. These cost-reducing opportunities were reviewed in person with each surgeon individually. During intervention, surgeons were shown the Tableau dashboard data at irregular intervals depending on their individual interest level. Monthly reports were also generated from Tableau to show each surgeon’s current average OR supply costs compared to his or her baseline, as well as to the overall group. These reports were emailed, printed, and hand-delivered to all surgeons monthly. Laminated pocket cards were also distributed to all surgeons and OR personnel (circulating nurses and scrub technicians) that listed commonly used supplies with their hospital costs and reviewed the preferred “high value” appendectomy (i.e., non sheathed cannula, hook cautery for mesoappendix, endoloops for appendiceal base, and selective use of the specimen retrieval bag).
2.3 Assessment of operative characteristics and clinical outcomes
The main clinical outcomes of interest included adverse events, OR procedure duration (skin incision to skin closure), total OR time, and LOS. Adverse events within 30 days of appendectomy were predefined as superficial or organ-space surgical site infection (SSI), return to OR, postoperative interventional radiology drainage, and readmission. LOS was measured as time from admission order to discharge order. Outcomes were compared using Fisher exact test or Wilcoxon rank sum test as appropriate. Analyses were conducted in R version 3.3.3.[23]
2.4 Analysis of cost data
Finance departmental personnel obtained financial data for the episode of care for each patient from the hospital’s internal cost accounting system. This system, Allscripts Enterprise Performance Systems Inc. (EPSi), provides patient-level hospital costs integrated into a single database and was used in all patients. The data were stored in an Oracle based Enterprise Data Warehouse and extracted using SQL Developer.
All cost data were collected and analyzed at the patient-level. Costs that were extracted included variable and fixed direct and indirect hospital costs (also known as technical costs). Professional costs were not included. Cost comparisons were performed using Wilcoxon rank sum test.
3. RESULTS
3.1 Demographic characteristics
During the study, 216 children underwent laparoscopic appendectomy for non-perforated appendicitis. Of these, 110 were in the 6-month pre-intervention period and 106 were post-intervention. Average age was 11.0 (IQR 8.7–13.6) years. The majority were male (128 children, 59.3%), Caucasian (169 children, 78.2%), and admitted as inpatients (187, 86.6%). Interval appendectomies performed for a resolved perforation were included with 4 patients in the pre-intervention cohort and 1 patient post-intervention. No significant difference was observed between patient demographics before and after the intervention (Table 1).
Table 1.
Demographic and Clinical Characteristics of Children Undergoing Laparoscopic Appendectomy Before and After Intervention
| Before Intervention (n = 110) | After Intervention (n = 106) | P-value | |
|---|---|---|---|
|
| |||
| Age, median years (IQR) | 11.0 (8.3–13.9) | 10.9 (9.1–13.5) | 0.980 |
|
| |||
| Male sex, No. (%) | 70 (63.6) | 58 (54.7) | 0.139 |
|
| |||
| Race, No. (%) | 0.466 | ||
| White | 85 (72.7) | 84 (79.2) | |
| Black | 10 (9.1) | 4 (3.8) | |
| Asian | 1 (0.9) | 1 (0.9) | |
| Native Hawaiian or Pacific Islander | 0 | 1 (0.9) | |
| American Indian | 0 | 1 (0.9) | |
| Unknown | 14 (12.7) | 15 (13.2) | |
|
| |||
| Ethnicity, No. (%) | 0.669 | ||
| Hispanic or Latino | 23 (20.9) | 17 (16.0) | |
| Not Hispanic or Latino | 75 (68.2) | 76 (71.7) | |
| Unknown | 12 (10.9) | 13 (12.3) | |
|
| |||
| Admission type, No (%) | 0.843 | ||
| Inpatient | 96 (87.3) | 91 (85.8) | |
| Outpatient | 14 (12.7) | 15 (14.2) | |
|
| |||
| Insurance status, No. (%) | 0.825 | ||
| Public insurance | 48 (44.0) | 52 (49.1) | |
| Nonpublic insurance | 59 (54.1) | 54 (50.9) | |
| Unknown | 1 (0.9) | 0 | |
|
| |||
| Operating room procedure duration, median minutes (IQR) | 47.0 (36.3–63.0) | 50.0 (38.0–63.8) | 0.520 |
|
| |||
| Total operating room duration, median minutes (IQR) | 83.0 (69.5–102.0) | 86.0 (71.8–102.8) | 0.418 |
|
| |||
| Length of stay, median days (IQR) | 1.1 (0.8–1.5) | 1.2 (0.9–1.6) | 0.023 |
|
| |||
| Any adverse event, No. (%) | 1 (0.9) | 6 (5.7) | 0.062 |
|
| |||
| Mesoappendiceal Ligation, No (%) | < 0.001 | ||
| Stapler | 56 (50.9) | 18 (17.0) | |
| Hook cautery | 19 (17.3) | 65 (61.3) | |
| Hand-held heat source | 35 (31.8) | 23 (21.7) | |
|
| |||
| Appendiceal Ligation, No (%) | < 0.001 | ||
| Stapler | 89 (80.9) | 44 (41.5) | |
| Endoloop | 21 (19.1) | 62 (58.5) | |
|
| |||
| Specimen Retrieval Bag, No (%) | < 0.001 | ||
| Yes | 90 (81.8) | 45 (42.5) | |
| No | 20 (18.2) | 61 (57.5) | |
3.2 Clinical outcomes of children undergoing laparoscopic appendectomy
Before the intervention, one child had an adverse event compared to 6 children after the intervention, although this change was not statistically significant (p = 0.062). The most frequent adverse events were superficial SSIs with 5 in the post-intervention cohort and none before intervention. The remaining adverse event was a post-operative small bowel obstruction requiring reoperation. No significant change was detected in median OR procedure duration before (47 [IQR 36–63] minutes) compared to after the intervention (50 [IQR 38–64] minutes, p = 0.520) or total OR duration (83 [IQR 70–102] before versus 86 [IQR 72–103] after, p = 0.418). LOS before the intervention was slightly shorter than length of stay after (1.1 [IQR 0.8–1.5] days versus 1.2 [IQR 0.9–1.6] days, p = 0.023).
3.3 Cost outcomes of children undergoing laparoscopic appendectomy
OR supply costs for laparoscopic appendectomy represented 20.9% of total hospital costs before the intervention (Table 2). There was a significant reduction in OR supply costs following the intervention ($884 [IQR $705–$1025] pre-intervention to $388 [IQR $182–$776] post-intervention, p < 0.001), representing a 56% reduction. Following the intervention, OR supply costs represented 9.8% of total hospital costs. The costs of OR services, anesthesia, and post-anesthetic care unit stay also declined following intervention. The reduction in supply costs, however, was the greatest in magnitude (Table 2). There was a significant reduction (p <0.001) in overall hospital costs after intervention from $4225 (IQR $3864–$4989) to $3949 (IQR $3462–$5006), attributable to the significant reduction in variable costs. There was no change in fixed costs.
Table 2.
Categorized Hospital Cost Data for Patients Before and After Intervention
| Cost Before Intervention, Median Dollars (IQR) | Cost After Intervention, Median Dollars (IQR) | P-value | |
|---|---|---|---|
| All Technical (Hospital) Costs | $4225 ($3864–$4980) | $3949 ($3462–$5006) | <0.001 |
| Variable Direct | $2700 ($2381–$2969) | $2364 ($1939–$2796) | <0.001 |
| Variable Indirect | $244 ($213–$309) | $216 ($186–$283) | 0.002 |
| Fixed Direct | $224 ($156–$287) | $189 ($156–$287) | 0.229 |
| Fixed Indirect | $1137 ($997–$1479) | $1178 ($985–$1479) | 0.496 |
| OR services | $1053 ($1053–$1304) | $938 ($938–$1163) | <0.001 |
| Nursing care/room and board | $932 ($802–$1106) | $994 ($213–$1704) | 0.113 |
| Supply | $884 ($705–$1025) | $388 ($182–$776) | <0.001 |
| ER services | $437 ($437–$437) | $469 ($469–$469) | <0.001 |
| Post-anesthesia care unit | $405 ($357–$453) | $337 ($292–$397) | <0.001 |
| Pharmacy | $162 ($99–$282) | $226 ($124–$368) | 0.329 |
| Anesthesia Services | $128 ($128–$153) | $141 ($141–$169) | 0.021 |
| Radiology | $77 ($0–$77) | $77 ($0–$78) | 0.145 |
| Pathology | $37 ($37–$37) | $38 ($38–$38) | <0.001 |
| Diagnostic laboratory | $18 ($0–$29) | $13 ($0–$35) | 0.151 |
| Therapeutic/diagnostic services | $0 ($0–$48) | $47 ($0–$51) | 0.115 |
3.4 Effect of the intervention on specific device utilization
Stapler use, both for mesoappendiceal control and appendiceal base ligation, significantly decreased (p <0.001) following the intervention (Table 1). Staplers were the most frequently used method of mesoappendiceal control before intervention (50.9%); however, monopolar electrosurgical energy with a reusable hook was the most common method to divide the mesoappendix after the intervention (61.3%). Use of the stapler during appendiceal base ligation decreased by almost 50% after the intervention as well. The endoloop was the most common method of base ligation after the intervention (58.5%). The use of specimen retrieval bags significantly declined following intervention (81.8% prior versus 42.5% post-intervention, p <0.001). In most cases in which a specimen retrieval bag was not utilized, another skin protective mechanism was used instead (i.e., appendix removed through the trocar or sterile surgical glove). However, in 34.6% (28 of 81 cases) the appendix was removed directly through the incision.
3.5 Surgeon-specific cost outcomes
The same 8 surgeons performed laparoscopic appendectomies before and after the intervention (Table 3). Volume ranged from 12–43 cases per surgeon with an average of 27 (IQR 21–32) cases per surgeon. OR supply costs for individual surgeons significantly decreased during the intervention period for 6 of the 8 surgeons (75.0%). OR supply costs increased for 1 surgeon ($789 [IQR $498–$1022] pre-intervention to $1006 [$916–$1097] post-intervention, p = 0.039) and was unchanged for one surgeon. OR time was unchanged for 7 of the 8 surgeons (87.5%), but increased for the surgeon with the lowest study period case volume (Table 3).
Table 3.
Per surgeon or resident supply cost and operating time for laparoscopic appendectomy for non-perforated appendicitis before and after intervention. PGY = Post Graduate Year
| OR Supply Cost, median dollars (IQR) | OR Time, median minutes (IQR) | |||||
|---|---|---|---|---|---|---|
| Surgeon* | Baseline | Intervention | P-value | Baseline | Intervention | P-value |
| A (n=43) | $876 ($746–$1063) | $470 ($394–$702) | <0.001 | 57 (40–76) | 62 (54–77) | 0.223 |
| B (n=39) | $789 ($498–$1022) | $1006 ($916–$1097) | 0.039 | 31 (26–42) | 36 (30–44) | 0.257 |
| C (n=29) | $878 ($857–$989) | $196 ($166–$213) | <0.001 | 60 (53–67) | 61 (51–69) | 0.913 |
| D (n=27) | $783 ($754–$884) | $755 ($477–$839) | 0.195 | 58 (47–74) | 58 (49–67) | 0.843 |
| E (n=26) | $676 ($668–$808) | $248 ($209–$276) | <0.001 | 64 (45–79) | 58 (44–72) | 0.697 |
| F (n=21) | $581 ($317–$726) | $190 ($155–$250) | <0.001 | 41 (38–45) | 36 (31–43) | 0.155 |
| G (n=19) | $842 ($756–$1002) | $443 ($208–$499) | <0.001 | 37 (31–40) | 38 (33–47) | 0.595 |
| H (n=12) | $915 ($387–$759) | $612 ($387–$759) | 0.009 | 34 (33–44) | 55 (48–60) | 0.045 |
| Resident Level* | Baseline | Intervention | P-value | Baseline | Intervention | P-value |
| Intern (n=50) | $794 ($716–$878) | $682 ($419–$916) | 0.146 | 56 (50–69) | 56 (44–66) | 0.701 |
| PGY 3/4 (n=90) | $808 ($672–$1002) | $428 ($219–$727) | <0.001 | 50 (37–73) | 56 (42–65) | 0.702 |
| Junior Fellow (n=32) | $888 ($781–$1002) | $872 ($428–$959) | 0.416 | 46 (32–51) | 58 (35–64) | 0.126 |
| Senior Fellow (n=43) | $737 ($622–$881) | $250 ($185–$392) | <0.001 | 42 (34–45) | 40 (32–47) | 0.920 |
Total number of cases per surgeon or resident level in both time periods
All included procedures involved a resident or fellow assistant, with the majority of the cases (41.7%) assisted by a PGY-3 or -4 resident surgeon. OR supply costs were significantly reduced in cases assisted by a PGY-3, PGY-4, or senior pediatric surgery fellow (p <0.001); however, there was no change in costs in those with an intern or junior pediatric surgery fellow (Table 3).
4. DISCUSSION
Our study shows that a purely optional and non-standardized approach to intraoperative cost reduction through real-time cost feedback to surgeons is both safe and effective at reducing OR supply costs for pediatric laparoscopic appendectomy. Laparoscopic appendectomy is one of the most common surgical interventions in children, and OR supply costs are a significant portion of the costs of care in these patients.[21] Thus, reduction of OR costs could significantly reduce overall costs and improve value. While prior studies have focused on standardization of supply use at the group level, this is the first study to show a reduction in OR supply costs for pediatric appendectomy by influencing surgeon decision-making with real-time patient-level cost data and emphasizing an approach tailored for each surgeon.
Avansino et al. reported a 20% average reduction in OR supply cost without a change in clinical outcomes through implementation of a standardized surgeon preference card for pediatric laparoscopic appendectomy.[20] Skarda et al. found a 64% reduction in OR supply cost for pediatric laparoscopic appendectomy with standardization to a single preference card, also with no change in clinical outcomes.[19] Our intervention using a non-unified approach with real-time cost feedback resulted in a 56% reduction in OR costs.
The primary changes in supply use following the intervention included an increase in the use of monopolar energy with a reusable hook to divide the mesoappendix and endoloops to control the appendiceal base rather than stapling devices. Use of specimen retrieval bags also decreased. In addition to these modifications in operative technique, surgeons were more cognizant of what disposable supplies were brought into the OR, discouraged opening supplies before approval, and reviewed the POU supply list at case conclusion to ensure accuracy.
While there was no direct incentive, monetary or otherwise, for the surgeons to participate in cost reduction decision-making, the competitive personalities of surgeons allowed for personal encouragement and subsequent acceptance of the intervention by most. By showing surgeons their OR supply cost data compared to the group’s average and their own baseline data, several surgeons became much more focused on cost reduction than the study leaders envisioned. Prior studies have used monetary incentives to influence surgeon intraoperative decision-making on supply utilization[12]. It is reasonable to assume that if financial incentives were in place to encourage surgeon-led cost reduction, the magnitude of cost reduction in this project would likely have been greater. These incentives would also likely encourage other cost reduction efforts in other patient populations.
Although the majority of surgeons chose to make lower cost supply decision-making choices in the OR, one surgeon within the group had an increase in cost following the intervention. This finding supports the notion that without a focus on cost reduction the natural tendency will be cost increases over time (costs will not remain flat), as the supply costs do increase over time. While standardization of OR supplies has been shown to decrease costs, it does require agreement by surgeons to adopt a single technique.[19] Even with attempted standardization through a unified surgeon preference card, some surgeons will have minimal to no change in supply use or costs.[20] The primary barrier to achieving a unified surgical approach is surgeon bias for or comfort with a particular surgical technique, with concern that a deviation in that method may result in compromising safety or time.[20] Our study and others have demonstrated no significant change in operative time or clinical outcomes with a significant change in the operative technique for the majority of surgeons performing laparoscopic appendectomies. Rather than standardizing operative technique, we aimed to identify if surgeon preferences change when they are provided with cost data and comparisons, and if so, how. Understanding why some surgeons enthusiastically embrace cost reduction efforts and others do not (all within the same organization with the same incentives) is an area of interest that will be explored in the future.
There is limited evidence regarding the association of device utilization with outcomes in laparoscopic appendectomy.[24] Although not significant, there was a trend toward an increase in SSI following the change in OR supply utilization and operative techniques. While the cause of this rise in SSI rate is unknown and could be secondary to chance, we have identified several possible contributing factors. Of the children who developed a SSI, 4 of the 5 (80%) appendices were removed without the aid of a specimen retrieval bag. While 2 of the cases noted extraction of the appendix through the trocar, 2 of the appendices were removed directly through the skin incision without protection. The rate of SSI with use of a specimen retrieval bag was 0.7%. However, if no bag was used, the rate was 4.9%. Surgeons have reported concern that eliminating the use of a specimen retrieval bag during laparoscopic appendectomy may increase rates of SSIs, although this has not been demonstrated in prior studies.[19] All of the cases resulting in a postoperative SSI were performed with the use of an endoloop for the appendiceal base. Prior studies have shown no difference in rates of SSIs with the use of endoloops compared to staplers for laparoscopic appendectomy in children.[19, 25]
Our study also suggests that the surgical assistant, in these cases being a resident or fellow trainee, can have an impact on operative supply costs. While our data does not provide evidence on why this association occurs, we hypothesize that the operative technique chosen by the operating surgeon may vary depending on the assistant. As the majority of non-perforated laparoscopic appendectomies in our teaching institution are performed by the trainees with guidance from the operating surgeon, the trainee could have impact on the method based upon his or her skill level, comfortability, or preference for a particular technique. We also found a reduction in costs for other areas of care, such as anesthesia and post-anesthesia care, following the intervention. While we are unaware of any specific practice changes, factors outside of our initiative could have driven these reductions in costs. Further studies should aim to investigate these findings.
Several limitations of the study exist. The study was performed at a single institution and changes in surgeon OR decision-making may vary at other sites. There may have been inadequate power to demonstrate a difference in clinical outcomes, such as SSIs. OR supply cost is only a portion of the costs of care in a child undergoing laparoscopic appendectomy, and this intervention did not incorporate other changes to the continuum of care. Room and board was found to be a large proportion of hospital costs for this procedure. Therefore, a potential further area for cost reduction of appendectomy at our institution is reduction of LOS as demonstrated by others previously.[26]
5. CONCLUSIONS
Approaching value measurement with a surgeon-specific, rather than a group-wide standardization approach, is an alternative to reduce OR supply costs and maintain excellent outcomes. Providing real-time cost data to surgeons changes behavior significantly even without obvious incentives.
Acknowledgments
FUNDING
JR Robinson receives salary and tuition support by the T15 LM007450 training grant from the NIH National Library of Medicine.
Footnotes
LEVEL OF EVIDENCE: Level II
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–81. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 2.Smoldt RK, Cortese DA. Pay-for-performance or pay for value? Mayo Clin Proc. 2007;82(2):210–3. doi: 10.4065/82.2.210. [DOI] [PubMed] [Google Scholar]
- 3.Cosgrove T. Value-based health care is inevitable and that’s good. Harvard Business Review. 2013 [Google Scholar]
- 4.Burwell SM. Setting value-based payment goals--hhs efforts to improve u.S. Health care. N Engl J Med. 2015;372(10):897–9. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 5.Brauer DG, Hawkins WG, Strasberg SM, Brunt LM, Jaques DP, Mercurio NR, et al. Cost variation in a laparoscopic cholecystectomy and the association with outcomes across a single health system: Implications for standardization and improved resource utilization. HPB: the official journal of the International Hepato Pancreato Biliary Association. 2015;17(12):1113–8. doi: 10.1111/hpb.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zygourakis CC, Valencia V, Boscardin C, Nayak RU, Moriates C, Gonzales R, et al. Predictors of variation in neurosurgical supply costs and outcomes across 4904 surgeries at a single institution. World Neurosurg. 2016;96:177–83. doi: 10.1016/j.wneu.2016.08.121. [DOI] [PubMed] [Google Scholar]
- 7.Adkins HH, Hardacker TJ, Ceppa EP. Examining variation in cost based on surgeon choices for elective laparoscopic cholecystectomy. Surgical endoscopy. 2016;30(7):2679–84. doi: 10.1007/s00464-015-4553-7. [DOI] [PubMed] [Google Scholar]
- 8.Jackson CR, Eavey RD, Francis DO. Surgeon awareness of operating room supply costs. The Annals of otology, rhinology, and laryngology. 2016;125(5):369–77. doi: 10.1177/0003489415614864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okike K, O’Toole RV, Pollak AN, Bishop JA, McAndrew CM, Mehta S, et al. Survey finds few orthopedic surgeons know the costs of the devices they implant. Health Aff (Millwood) 2014;33(1):103–9. doi: 10.1377/hlthaff.2013.0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tabib CH, Bahler CD, Hardacker TJ, Ball KM, Sundaram CP. Reducing operating room costs through real-time cost information feedback: A pilot study. Journal of endourology. 2015;29(8):963–8. doi: 10.1089/end.2014.0858. [DOI] [PubMed] [Google Scholar]
- 11.Guzman MJ, Gitelis ME, Linn JG, Ujiki MB, Waskerwitz M, Umanskiy K, et al. A model of cost reduction and standardization: Improved cost savings while maintaining the quality of care. Diseases of the colon and rectum. 2015;58(11):1104–7. doi: 10.1097/DCR.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 12.Zygourakis CC, Valencia V, Moriates C, Boscardin CK, Catschegn S, Rajkomar A, et al. Association between surgeon scorecard use and operating room costs. JAMA Surg. 2017;152(3):284–91. doi: 10.1001/jamasurg.2016.4674. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan RS, Porter ME. The big idea: How to solve the cost crisis in health care. Harvard Business Review. 2011 Sep; [PubMed] [Google Scholar]
- 14.Robinson JR, Avritscher EBC, Gay JC, Willis ZI, Putnam LR, Anglemyer A, et al. Measuring the value of a clinical practice guideline for children with perforated appendicitis. Ann Surg. 2017;266(1):195–200. doi: 10.1097/SLA.0000000000001946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willis ZI, Duggan EM, Bucher BT, Pietsch JB, Milovancev M, Wharton W, et al. Effect of a clinical practice guideline for pediatric complicated appendicitis. JAMA Surg. 2016:e160194. doi: 10.1001/jamasurg.2016.0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen JW, Polk HC., Jr A study of added costs of laparoscopic cholecystectomy based on surgery preference cards. Am Surg. 2002;68(5):474–6. [PubMed] [Google Scholar]
- 17.Mahomed AA, McLean V. Cost analysis of minimally invasive surgery in a pediatric setting. Journal of laparoendoscopic & advanced surgical techniques Part A. 2007;17(3):375–9. doi: 10.1089/lap.2006.0077. [DOI] [PubMed] [Google Scholar]
- 18.Chu T, Chandhoke RA, Smith PC, Schwaitzberg SD. The impact of surgeon choice on the cost of performing laparoscopic appendectomy. Surgical endoscopy. 2011;25(4):1187–91. doi: 10.1007/s00464-010-1342-1. [DOI] [PubMed] [Google Scholar]
- 19.Skarda DE, Rollins M, Andrews S, McFadden M, Barnhart D, Meyers R, et al. One hospital, one appendectomy: The cost effectiveness of a standardized doctor’s preference card. Journal of pediatric surgery. 2015;50(6):919–22. doi: 10.1016/j.jpedsurg.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Avansino JR, Goldin AB, Risley R, Waldhausen JH, Sawin RS. Standardization of operative equipment reduces cost. Journal of pediatric surgery. 2013;48(9):1843–9. doi: 10.1016/j.jpedsurg.2012.11.045. [DOI] [PubMed] [Google Scholar]
- 21.Yu YR, Abbas PI, Smith CM, Carberry KE, Ren H, Patel B, et al. Time-driven activity-based costing to identify opportunities for cost reduction in pediatric appendectomy. Journal of pediatric surgery. 2016;51(12):1962–6. doi: 10.1016/j.jpedsurg.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 22.Tableau. [accessed October 15, 2017]; https://www.tableau.com/2017.
- 23.R core team. R: A language and environment for statistical computing. R foundation for statistical computing; vienna, austria: 2015. http://www.r-project.org/ [Google Scholar]
- 24.Langer M, Safavi A, Skarsgard ED. Management of the base of the appendix in pediatric laparoscopic appendectomy: Clip, ligate, or staple? Surg Technol Int. 2013;23:81–3. [PubMed] [Google Scholar]
- 25.Miyano G, Urao M, Lane G, Kato Y, Okazaki T, Yamataka A. Appendiceal stump closure in children with complicated appendicitis: A prospective analysis of endoloops versus endostaples. Asian journal of endoscopic surgery. 2011;4(3):116–9. doi: 10.1111/j.1758-5910.2011.00091.x. [DOI] [PubMed] [Google Scholar]
- 26.Skarda DE, Schall K, Rollins M, Andrews S, Olson J, Greene T, et al. Response-based therapy for ruptured appendicitis reduces resource utilization. Journal of pediatric surgery. 2014;49(12):1726–9. doi: 10.1016/j.jpedsurg.2014.09.012. [DOI] [PubMed] [Google Scholar]