Abstract
Though eating with others is often a social behavior, relationships between social contexts of eating and nutrient intake have been underexplored. This study evaluates how social aspects of eating – frequencies of eating meals with others, meals prepared at home, and meals outside the home – are associated with nutrient intake. Because diet improvement can reduce complications of diabetes mellitus, we surveyed a multi-ethnic cohort of persons with type 2 diabetes (n=770) about social aspects of diet (based on 24h recalls). Sex-stratified multiple regression analyses adjusted for confounders assessed the relationship between frequency of eating with others and nutrient intake (total energy, energy from fat, energy from carbohydrates, Healthy Eating Index/HEI, Dietary Approaches to Stop Hypertension/DASH score). Although there was slight variation in men’s versus women’s propensity to share meals, after adjustment for confounders, there was no consistently significant association between meals with others and the 5 nutrient intake measures for either men or women. The directions of association between categories of eating with others and diet quality (HEI and DASH scores) – albeit not significant – were different for men (positive) and women (mostly negative), which warrants further investigation. The next analyses estimated nutrient intake associated with meals prepared at home, and meals consumed outside the home. Analyses indicated that greater meal frequency at home was associated with significantly better scores on diet quality indices for men (but not women), while meal frequency outside the home was associated with poorer diet quality and energy intake for women (but not men). Better measurement of social dimensions of eating may inform ways to improve nutrition, especially for persons with diabetes for whom diet improvement can result in better disease outcomes.
Keywords: eating with others, commensality, meal location, social contexts of eating, diet quality, nutrition disparities by sex, diabetes
Introduction
Where we eat, which foods we eat, and with whom we eat are important decisions that shape diet in ways that extend beyond simple fuel for physiological function (Fischler, 2011; Higgs & Thomas, 2015; Rozin, 1996). Though eating with other people is a fundamentally social behavior that appears to transcend population subgroups, the relationships between social contexts of eating and nutrition intake have not been thoroughly explored. Research on food consumption has clearly linked the volume and types of food consumed with cardiometabolic conditions such as obesity, hypertension, cardiovascular disease, and diabetes (Ogden, Carroll, Kit, & Flegal, 2014; Pemberton, et al., 2010). Several decades of research shows the complicated ways that the presence of others while eating, and the characteristics/behaviors of eating partners, can influence the quantity and type of food we eat at meals (Herman, 2015). However, it is less clear whether and how social aspects of the food environment are then associated with one’s overall nutrient intake over longer timescales than the eating occasion.
With this in mind, this study sought to examine how two important but understudied dimensions– where meals are consumed, and the frequency of meals shared with others – might be associated with macronutrient intake as well as overall nutrient intake quality among at-risk patients with a medical reason to maintain a healthy diet. Importantly, we sought to investigate these questions among a sample of Americans with diabetes mellitus (DM). From 1990 to 2008, the incidence and prevalence of DM doubled in the United States, with signs of continuing increases among those with a high school education or less, and among non-Hispanic black and Hispanic subgroups (Geiss, et al., 2014). Recent estimates suggest that elevated blood glucose levels accounted for more than $322 billion in health care expenditures in 2012 (Dall, et al., 2014). Diet improvement can reduce complications of this disease. Thus, a better understanding of how sociability and other aspects of the food environment may shape nutrient intake and diet quality may help identify ways to improve health.
Studies of commensal eating have shown that the presence of other people can increase the volume of food an individual will consume at a given meal, a well-known phenomenon known as social facilitation (Clendenen, Herman, & Polivy, 1994; de Castro, 1994, 2000; Herman, 2015). Increased consumption due to social facilitation may be due to lengthening of mealtime, changes in social norms around eating (Higgs, 2014), modeling behaviors (Cruwys, Bevelander, & Hermans, 2014), social comparison (Polivy & Pliner, 2014), and/or impression management (Vartanian, 2014). This phenomenon appears to vary by gender, though it is not clear whether social facilitation is stronger for men or women. For instance, a food diary study of French students found that the correlation between volume of food consumed and the number of persons present was greater for men than for women, though both were positive and significant (Bellisle, Dalix, & de Castro, 1999). A laboratory study of psychology undergraduate students using a free-eating paradigm found a suppression effect of eating less with same-gender strangers, while within mixed-gender stranger pairs, men consumed a greater volume (Salvy, Jarrin, Paluch, Irfan, & Pliner, 2007). A naturalistic study of college-aged American students found a stronger association among women in a same-sex group situation (Young, Mizzau, Mai, Sirisegaram, & Wilson, 2009). In a diary-based nutrient intake study among obese adult women, Patel and Schlundt (2001) found that there was a stronger association between social eating settings and fat intake than with carbohydrate.
A smaller and distinct body of research that investigates social structure beyond dyadic or small-group scenarios concerns the patterning of food choice in larger social networks. This research has shown that an individual’s food choices over a longer-term timescale can be shaped by specific friends and family members (Conklin, et al., 2014; de la Haye, Robins, Mohr, & Wilson, 2013; M. A. Pachucki, Jacques, & Christakis, 2011; M. C. Pachucki, 2014). However, hyperdyadic network research on food choice – which provides the advantage of accounting for the behaviors of multiple socially-tied contacts – generally does not focus upon the dynamics of the eating occasion. Instead, network research has focused its attentions on documenting similarities and differences in an individual’s food choices with their network contacts, and assessing whether there is evidence that homophily and social influence mechanisms may account for the observed food choices. As a result, whether being socially connected with others who eat in certain ways over longer timescales affects one’s food choice (as network research has done) is a different question than whether eating with others at a given meal may shape nutrient intake (as dyadic and small-group social facilitation research has done).
Food intake is also affected by where meals are consumed. Cross-sectional, nationally-representative nutrition survey data suggest Americans spend less time preparing food at home than in previous decades, decreasing from roughly 98 minutes per day to 35 minutes from 1965 to 2008. In addition, calories consumed outside the home have increased (L. P. Smith, Ng, & Popkin, 2013). The patterns vary by socioeconomic status and ethnicity. In US survey data from 2007–08, low socioeconomic status (SES) individuals were less likely than those of higher SES to prepare foods at home, and black and Hispanic households were less likely than white households to prepare food at home (Virudachalam, Long, Harhay, Polsky, & Feudtner, 2014).
Research on food consumed outside the home has shown that Americans spent 50.1% of their overall food dollars on food away from home in 2014, up from 43% in 1990, and more than twice the percentage of expenditures (23.8%) in 1948 ((ERS), 2016). Individuals tend to underestimate fat, energy, and sodium intake in foods that come from commercially-prepared settings; such foods tend to be more calorically dense and of larger portion size (Story, Kaphingst, Robinson-O’Brien, & Glanz, 2008). Evidence suggests that the trend towards more meals eaten outside the home extends beyond the US, with similar findings from cohorts in Europe (Myhre, Loken, Wandel, & Andersen, 2014; Orfanos, et al., 2007), and Australia (Burns, Jackson, Gibbons, & Stoney, 2002).
There is also considerable variation in how and why people eat out of the home and in the home, and what these behaviors mean to different people. For instance, eating out may be for reasons of convenience, celebrating a special occasion, or for sociability – yet eating out for women is increasingly for purposes of sociability (Paddock, Warde, & Whillans, 2017). Women also eat less frequently outside the home than men (Kant & Graubard, 2004; Lund, Kjaernes, & Holm, 2017), and spend proportionately less than men, whether married, divorced, or never married (Kroshus, 2008). Although there were no statistically significant gender differences in HEI or energy intake in a study of 2003–04 NHAHES meals consumed away from home, each additional meal consumed away from home was associated with a 2.1-point reduction in HEI score for women, and a 1.9-point reduction in HEI score for men (Mancino, Todd, & Lin, 2009).
Examination of this research prompts several observations. First, a rigorous nutrient intake protocol has not been used to examine whether propensity to eat meals with others is associated with overall diet quality, nor whether this association varies between men and women in a large sample. Put another way, a great deal of laboratory and small-group research on social facilitation has shown evidence of a social correlation wherein an increase in the number of meal partners tends to be positively associated with food or nutrient intake when measured at the occasion of a meal. However, it is not clear that there is a longer-term effect of this social correlation wherein it translates to adverse nutrient intake over a greater span of time than a meal. There has also been relatively little research to compare the relative contributions to nutrient intake of meals prepared at home versus meals consumed outside the home in the context of the same study, nor how this nutrient intake may vary for men and women. Knowing more about how these aspects of eating are socially patterned may provide important information to improve the likelihood of success in modifying eating behaviors.
Prior research on social facilitation leads us to hypothesize that individuals who report a greater frequency of meals with others will also report greater energy intake (H1), though it is likely that this pattern is not linear. Social facilitation at the timescale of the meal occasion has been found to occur with as few as one eating partner and follows a power-law distribution (de Castro & Brewer, 1992). This comports with limited network research – notably, based on average prior-month food consumption – that suggests that those with poorer overall diet quality (often associated with greater caloric intake) also have a greater network size (M. A. Pachucki, et al., 2011).
A second hypothesis (H2) is that, after adjusting for the above expectation of increased energy intake and socio-demographic confounders, meals with others will remain associated with nutrient intake and diet quality. It is unclear from prior research whether this association will be stronger among men or women, though the association between meals with others and calories from fat is likely to be greater than the association between meals with others and calories from carbohydrate.
Finally, nationally-representative studies on meals prepared at home and eating outside the home prompt a third hypothesis that, generally speaking, eating more meals prepared at home will be associated with healthier nutrient intake, while eating more meals outside the home will be associated with poorer nutrient intake (H3). However, given clearly gendered divisions of labor in food preparation in the home, and research that shows that meanings of eating outside the home differ for men and women, we predict there to be differences in the magnitude of these associations. Diet quality is especially important among adults with Type 2 diabetes, and understanding how to promote a healthy diet is of special importance for this population. Thus, the current study is conducted with a sample of adults diagnosed with this chronic condition.
Material and Methods
The study was conducted among participants in the Diabetes Study of Northern California (DISTANCE). The DISTANCE cohort consists of an ethnically-stratified group of members from the Kaiser Permanente Northern California (KPNC) managed health care organization with diabetes (n=20,188) who were randomly selected in 2005 from the Kaiser Permanente Diabetes registry. The main purpose of this parent study was to understand social disparities in health. Participants provided information about their health status, behaviors, and socio-demographic background in an extensive survey (Moffet, et al., 2009). This study has yielded many insights, including links between cardiometabolic risk and neighborhood deprivation (Laraia, et al., 2012; Stoddard, et al., 2013), racial and ethnic differences in the link between obesity and healthful food environments (Jones-Smith, et al., 2013), and associations between socioeconomic status position and hypoglycemia risk (Berkowitz, et al., 2014).
In 2011, an ancillary study was conducted among a subset of DISTANCE respondents; the emphasis of this new study was understanding how nutrition and the food environment were associated with participant health. Eligibility criteria included current KPNC membership, being an English speaker and living in a Metropolitan Statistical Area. Invitation letters were sent to 1,500 eligible subjects during 2011 and 2012 to gauge their interest in taking part. A total of 770 participants then completed the study via telephone survey for a response rate of 56.6%, after accounting for eligibility and people who were unable to be contacted (Research, 2008). All study protocols were approved by [Redacted for Review] Institutional Review Board Human Subjects Committees.
In addition to a written survey, participants also completed two interviewer assisted 24-hour dietary recalls (one weekday, one weekend) over the phone using the Nutrition Data System for Research software developed at the University of Minnesota Nutrition Coordinating Center (NCC) (Feskanich, Sielaff, Chong, & Buzzard, 1989; Sievert, Schakel, & Buzzard, 1989). Information on the nutrient content of food items was then transformed into estimates of nutrient intake using a food item database maintained by NCC and aggregated into average single-day estimates of nutrient intake using the both days of intake data. There is considerable discussion about best methods for assessing nutrient intake (for instance, 24-hour recall, food diaries, food frequency questionnaires, doubly-labeled water) and much progress in assessing validity and reliability of these methods (Willett, 2013). While no approach is perfect (Dhurandhar, et al., 2015; Shim, Oh, & Kim, 2014), given the ancillary study sample size and the choice to administer it via telephone survey, a validated 24-hour dietary recall approach was assessed to be the most appropriate (F. E. Thompson, et al., 2015).
Outcome measures
The outcomes of interest included nutrient intake measures derived from the dietary recall and included estimates of percentage of daily energy intake from fat, percentage of daily energy intake from carbohydrate and total energy (kilocalories). These particular measures are especially relevant to a population of persons with diabetes because energy and nutrient management of carbohydrate and fat are key parts of a type 2 diabetes control strategy. The main diet quality measures were derived from reported food intake and were the Healthy Eating Index-2010 (HEI) score and the Dietary Approaches to Stop Hypertension (DASH) score.
The HEI was developed by the US Department of Agriculture to measure compliance with national nutrition guidelines, and monitor change in American diets (Kennedy, Ohls, Carlson, & Fleming, 1995). The HEI-2010 has 12 components, including 9 adequacy components (whole fruit, total fruit, whole grains, dairy, total protein foods, seafood & plant proteins, greens & beans, total vegetables, fatty acids) and 3 moderation components (refined grains, sodium, empty calories). The HEI-2010 conforms to the most recent Dietary Guidelines for Americans and is assessed on a 100-point scale (Guenther, et al., 2013).
The DASH (Dietary Approaches to Stop Hypertension) diet, assessed on a 40-point scale, was developed as part of an intervention to reduce blood pressure. Higher scores reflect high intake of fruits and vegetables, moderate intake of low-fat dairy, low intake of animal protein, and high intake of plant-based proteins (Appel, et al., 1997).
Exposures
Three eating behaviors related to eating were examined as social exposures relevant to the dietary outcomes:
Meals with others was indicated by a summary measure that assessed the frequency with which an individual reported eating a meal with one of seven types of social relations. Participants were asked, “Over the course of the last seven days, how many times have you shared a meal with the following people?” and separate questions queried frequency of meals consumed with others (open response) with family members, spouse/partner, co-worker, friend, sibling, neighbor, or other type of meal partner. As our interest was in the volume of eating at a table with different persons who were socially connected to a participant, we summed these frequencies to provide a rough estimate of the number of meals with others per week. It should be noted that because we treated individuals, rather than meals, as the unit of analysis, it is possible that if a given participant reported 4 meals consumed with neighbors and 8 meals consumed with friends, that both friends and neighbors could have been both present at some proportion of those meals. Thus, while this measure overestimates the absolute number of meals consumed with others as opposed to by oneself, it provides an individual-level measure of the extent of meal-based sociability.
Meals prepared at home, assessed the extent to which an individual consumed food prepared by someone in their home. Participants were asked, “How many meals per week do you eat that have been prepared at home (meaning food that has put together and cooked yourself (or by someone else in the household) and has not been pre-prepared/take out/fast food)?” Separate questions were asked for breakfast, lunch, and dinner, (each between 0–7 times per week), and responses were summed to estimate the number of meals prepared at home per week.
Meals eaten out, measured the response to the question “In an average [select: week or month], how many times do you eat [select: breakfast/lunch/supper] from a restaurant or cafeteria?” After gathering information for frequencies of each type of meal eaten out per week or month, responses were summed to estimate the number of meals eaten out per month. We determined this periodicity to be more appropriate than the weekly measure of meals prepared at home.
Confounding variables
Since eating behaviors vary by demographic and socioeconomic attributes, we adjusted for possible confounders of the relationship between social food behaviors and nutrient intake. Demographic measures included age (continuous), biological sex (binary; participants did not report on gender identity), and race (categorical: Caucasian, African American, Latino, Asian, Other). Socioeconomic attributes included income (a 13-level categorical variable transformed to a continuous measure using the median of each category), education (did not complete high school, high school graduate/GED/trade school, Associate degree, College graduate, Postgraduate), and subjective social status (a visual instrument asking participants to rank themselves on one of 10 rungs of a ladder according to their perception of their relative socioeconomic status) (Adler, E, G, & J, 2000). Finally, two control variables were included: total calories (kcal) and household size, the first because mealtime sociability is often associated with an increased volume of food consumption. A continuous measure of members in the household was included to accompany household income because the relationships between outcomes (nutrient intake) and exposures (social food behaviors) may be confounded by household size.
Analysis strategy
After tabulating patient characteristics, we calculated bivariate associations between eating behavior measures and the three main exposures using appropriate non-parametric tests of association. A series of multiple linear regressions were specified to estimate the relationship between each macronutrient or diet index (outcome) with the frequency of meals with others (exposure). Due to a non-linear distribution of meals with others, the continuous covariate was transformed to a categorical variable (0 weekly meals with others, 1–6, 7–13, 14–20, >21). The modal category was >21 meals with others/week (n=186 persons, 24.2%); this subset of participants ate nearly all meals with at least one other person. In addition, in this population with diabetes, individuals may have a greater number of small meal occasions per day as part of disease management.
A second series of regressions estimated the relationship between each macronutrient or diet index (outcome) with the frequencies of meals prepared at home or eaten outside the home (exposures). Due to a similar non-linear distribution of exposures, we transformed continuous meals at home to a categorical variable (0 meals weekly, 1–3, 14–20, >21); monthly meals outside the home was transformed slightly differently due to lower monthly frequency (0 meals, 1–4 meals, 4–11 meals, >11 meals). The largest group of participants (n=254 persons, 33%) consumed more than 11 meals/week outside the home, and the modal category of meals prepared at home was 14–20 meals/week at home (n=252 persons, 32.7%). Further information on the participant distribution across meal location categories is reported in Figures 2–3 in the Supplemental Data.
We used multivariable linear regression analyses to estimate the association between measures of nutrient intake (energy, % of energy from fat, % of energy from carbohydrate, HEI-2010, DASH) and frequency of meals with others while adjusting for socio-demographic confounders. In analyses for total energy, we used a natural log transformation due to a non-normal distribution of the outcome. Observations with missing measurements were removed from the analysis rather than imputing missing covariate data (complete case analysis).
We estimated robust standard errors in all regression analyses to correct for model misspecification due to heteroskedasticity. Analyses were performed using Stata version 15 (StataCorp, 2017).
Findings from research on biological sex and gender differences in commensal eating prompted us to examine associations between nutrient intake and diet quality with the social food behaviors separately for males and females. Prior research on social facilitation suggests that there may be some effect modification by sex, but it is not clear whether the effects will be stronger for males or females. Interaction terms between meals with others and sex in adjusted regression models for diet quality (HEI and DASH scores) outcomes were significant, while those for the other outcomes were not. Taken together, these diagnostic tests lent support to the decision to stratify analyses by sex.
Results
Sample characteristics
Participants had a mean age of 63.3 years with slightly more women (52.9%) than men, and, because of the race-stratified sampling, had relatively balanced proportions of Caucasian, African American, Latino, and Asian participants (Table 1). The age of this cohort reflects the purpose of the ancillary study, to study the nutritional landscape of persons with type 2 diabetes, which has the highest prevalence among individuals ages 45 to 64 (Prevention, 2017). The majority of participants (64%) were married, and the sample had an average household income of approximately $67,200 per year; the modal category of educational attainment among participants (42%) was a high school degree. Participants perceived themselves to be slightly above the midpoint of the subjective socioeconomic status distribution and the average household size was 2.67 persons, including the respondent. In terms of social food behaviors, participants reported an average of 13 meals with others per week. In a typical week, slightly more than half of meals were prepared at home, while in a typical month roughly a tenth of meals were consumed outside the home. There were some missing data on income (n=102, 13.2%) and subjective social status (n=54, 7.0%), with a smaller amount missing on race (n=22, 2.9%), education (n=9, 1.2%), household size (n=4, 0.5%), and total energy, energy from fat, energy from carbohydrates, and DASH score (n=8, 1.0%). Men and women were significantly different in terms of nutrient intake, diet quality, and meals eaten outside the home each month, as well as race, marital status, income, and educational attainment.
Table 1.
Sociodemographic characteristics, social food behaviors, nutrient intake
| Characteristics | Total | Male | Female | p-val for diff | |||
|---|---|---|---|---|---|---|---|
| n= | Cat % / Mean (SD) | n= | Cat % / Mean (SD) | n= | Cat % / Mean (SD) | ||
| Age (mean, SD) | 770 | 63.3 (9.9) | 363 | 63.4 (9.8) | 407 | 63.2 (10.1) | 0.93 |
| Sex (%) | - | - | - | ||||
| Male | 363 | 47.1% | |||||
| Female | 407 | 52.9% | |||||
| Race (%) | 0.001 | ||||||
| Caucasian | 166 | 21.6% | 98 | 27.0% | 68 | 16.7% | |
| African American | 177 | 23.0% | 70 | 19.3% | 107 | 26.3% | |
| Latino | 137 | 17.8% | 53 | 14.6% | 84 | 20.6% | |
| Asian | 164 | 21.3% | 85 | 23.4% | 79 | 19.4% | |
| Other | 104 | 13.5% | 44 | 12.1% | 60 | 14.7% | |
| NA (not available) | 22 | 2.9% | 13 | 3.6% | 9 | 2.2% | |
| Marital status (%) | <0.001 | ||||||
| Married | 489 | 63.9% | 280 | 77.8% | 209 | 51.6% | |
| Divorced | 75 | 9.8% | 22 | 6.1% | 53 | 13.1% | |
| Widowed | 95 | 12.4% | 19 | 5.3% | 76 | 18.8% | |
| Single | 106 | 13.9% | 39 | 10.8% | 67 | 16.5% | |
| Income, household (mean, SD) | 668 | $67,219 ($36,975) | 318 | $75,456 ($37528) | 350 | $59,736 ($34866) | <0.001 |
| Household size (mean, SD) | 766 | 2.67 (1.6) | 361 | 2.61 (1.57) | 405 | 2.74 (1.61) | 0.16 |
| Education (%) | <0.001 | ||||||
| No HS diploma | 80 | 10.4% | 38 | 10.5% | 42 | 10.3% | |
| HS diploma/GED/trade school | 325 | 42.2% | 131 | 36.1% | 194 | 47.7% | |
| Associate degree | 99 | 12.9% | 37 | 10.2% | 62 | 15.2% | |
| College degree | 163 | 21.2% | 87 | 24.0% | 76 | 18.7% | |
| Post-graduate degree | 94 | 12.2% | 66 | 18.2% | 28 | 6.9% | |
| NA (not available) | 9 | 1.2% | 4 | 1.1% | 5 | 1.2% | |
| Subjective SES ladder (mean, SD) | 716 | 6.4 (1.8) | 340 | 6.5 (1.7) | 376 | 6.3 (1.8) | 0.16 |
| Meals with others, per week (mean, SD) | 770 | 13.1 (11.5) | 363 | 13.6 (11.2) | 407 | 12.6 (11.8) | 0.12 |
| Meals prepared at home, per week (mean, SD) | 770 | 12.2 (8.0) | 363 | 11.9 (7.8) | 407 | 12.4 (8.2) | 0.40 |
| Meals eaten out, per month (mean, SD) | 770 | 10.2 (11.9) | 363 | 12.8 (13.4) | 407 | 8.0 (9.9) | <0.001 |
| Nutrients and energy (mean, SD) | |||||||
| Total energy (kCal) | 762 | 1.63 (0.6) | 358 | 1.79 (0.6) | 404 | 1.50 (0.5) | <0.001 |
| Energy from fat (%) | 762 | 35.9 (7.6) | 358 | 36.3 (7.8) | 404 | 35.5 (7.4) | 0.15 |
| Energy from carbohydrate (%) | 762 | 45.1 (9.1) | 358 | 43.9 (9.9) | 404 | 46.1 (8.1) | <0.001 |
| Overall diet indices (mean, SD) | |||||||
| Healthy Eating Index (HEI-2010) score | 770 | 65.7 (14.5) | 363 | 63.9 (14.6) | 407 | 67.3 (14.3) | 0.001 |
| DASH diet adherence | 762 | 23.7 (5.09) | 358 | 23.0 (5.4) | 404 | 24.3 (4.7) | 0.001 |
The distribution of meals with others (not reported in Table 1) was 36% with family members; 30% with spouse/partners; 14.5% with friends; 11.1% with co-workers; 7.1% with siblings; and 1.4% with neighbors. This roughly comports with research by Sobal and Nelson (2003), who suggest that among adults, commensal meals are more often shared with partner/spouse and family/children than others (co-workers, others). Other research, albeit among younger cohorts, shows that individuals tend to eat frequently with family and friends (e.g., de Castro, 1994; Herman, Roth, & Polivy, 2003).
Bivariate association between social food behaviors, nutrient outcomes, and sample characteristics
Eating more meals with others (our first social food behavior) was significantly associated with greater intake of total energy and better diet quality, according to one of our indices (HEI-2010), but not energy from fat or carbohydrate, nor DASH diet score (Table 2). This provides preliminary support for the first hypothesis about energy intake; when we further stratified by sex, this positive correlation between frequency of meals with others and energyintake appeared to be largely driven among women (ρ =0.17, p<0.001), while there was no significant association for men (ρ = 0.03, p=0.58).
Table 2.
Bivariate associations between social food behaviors, nutrient outcomes, and sample characteristics
| (1) Meals with others/wk (freq) | (2) Meals prepared at home/wk (freq) | (3) Meals eaten outside the home/month (freq) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n= | Med | IQR | corr. | p-val | n= | Med | IQR | corr. | p-val | n= | Med | IQR | corr. | p-val | |
|
|
|
|
|||||||||||||
| Outcomes | |||||||||||||||
| Macronutrients | |||||||||||||||
| Total energy (kCal) | 762 | - | - | 0.11 | 0.003*** | 762 | - | - | −0.08 | 0.03** | 762 | - | - | 0.24 | <0.001*** |
| Energy from fat (%) | 762 | - | - | 0.01 | 0.85 | 762 | - | - | −0.15 | <0.001*** | 762 | - | - | 0.20 | <0.001*** |
| Energy from carbohydrate (%) | 762 | - | - | 0.02 | 0.60 | 762 | - | - | 0.08 | 0.02** | 762 | - | - | −0.19 | <0.001*** |
| Nutrition indices | |||||||||||||||
| Healthy Eating Index (HEI-2010) score | 770 | - | - | 0.07 | 0.05** | 770 | - | - | 0.22 | <0.001*** | 770 | - | - | −0.13 | <0.001*** |
| DASH diet score | 762 | - | - | 0.04 | 0.25 | 762 | - | - | 0.18 | <0.001*** | 762 | - | - | −0.18 | <0.001*** |
| Confounders | |||||||||||||||
| Age | 770 | - | - | -0.06 | 0.09 | 770 | - | - | 0.05 | 0.19 | 770 | - | - | −0.24 | <0.001*** |
| Sex | 0.12 | 0.40 | <0.001*** | ||||||||||||
| Male | 363 | 13 | 17 | - | 363 | 13 | 13 | - | 363 | 8.3 | 16.4 | - | |||
| Female | 407 | 10 | 16 | - | 407 | 15 | 15 | - | 407 | 4.4 | 10.0 | - | |||
| Race | 0.01*** | 0.65 | 0.03** | ||||||||||||
| Caucasian | 166 | 14 | 15 | - | 166 | 15 | 14 | - | 166 | 8.0 | 12.7 | - | |||
| African American | 177 | 7 | 16 | - | 177 | 14 | 14 | - | 177 | 4.4 | 10.0 | - | |||
| Latino | 137 | 11 | 18 | - | 137 | 14 | 18 | - | 137 | 7.4 | 14.7 | - | |||
| Asian | 164 | 14 | 17 | - | 164 | 14.5 | 14 | - | 164 | 5.2 | 12.1 | - | |||
| Other | 104 | 13 | 15 | - | 104 | 13 | 13.5 | - | 104 | 5.0 | 13.5 | - | |||
| NA | 22 | 9 | 15 | - | 22 | 16 | 11.0 | 22 | 5.7 | 21.8 | - | ||||
| Marital status | <0.001*** | 16 | <0.001*** | <0.001*** | |||||||||||
| Married | 489 | 15 | 14 | - | 489 | 15 | 14 | - | 489 | 7.0 | 14.1 | - | |||
| Divorced | 75 | 4 | 10 | - | 75 | 7 | 19 | - | 75 | 4.4 | 11.7 | - | |||
| Widowed | 95 | 3 | 9 | - | 95 | 18 | 14 | - | 95 | 3.0 | 7.7 | - | |||
| Single | 106 | 4.5 | 10 | - | 106 | 12 | 13 | - | 106 | 8.2 | 15.1 | - | |||
| Income, household (mean, SD) | 668 | - | - | 0.23 | <0.001*** | 668 | - | - | −0.004 | 0.93 | 668 | - | - | 0.32 | <0.001*** |
| Household size (mean, SD) | 766 | - | - | 0.29 | <0.001*** | 766 | - | - | 0.10 | 0.005*** | 766 | - | - | −0.03 | 0.40 |
| Education | 0.82 | 0.18 | 0.006*** | ||||||||||||
| No HS diploma | 80 | 12.5 | 17.5 | - | 80 | 15.5 | 14 | - | 80 | 4.0 | 12.0 | - | |||
| HS diploma/GED/trade school | 325 | 11 | 18 | - | 325 | 14 | 17 | - | 325 | 6.0 | 12.1 | - | |||
| Associate degree | 99 | 11 | 18 | - | 99 | 15 | 13 | - | 99 | 5.0 | 10.0 | - | |||
| College degree | 163 | 11 | 14 | - | 163 | 14 | 14 | - | 163 | 7.4 | 14.7 | - | |||
| Post-graduate degree | 94 | 12 | 15 | - | 94 | 15 | 13 | - | 94 | 8.5 | 17.9 | - | |||
| NA | 9 | 16 | 18 | 9 | 9 | 14 | - | 9 | 7.0 | 4.0 | - | ||||
| Subjective Social Status (mean, SD) | 740 | - | - | −0.03 | 0.37 | 740 | - | - | −0.05 | 0.14 | 740 | - | - | 0.09 | 0.02** |
P <0.05,
P <0.01
Note: social food behaviors are not normally distributed; therefore, appropriate non-parametric tests of association were used to obtain p-values binary (wilcoxon mann-whitney U); continuous (pearson correlation); continuous ordinal (spearman correlation); categorical (kruskal-wallis test)
Note on abbreviations: general equivalency diploma (GED); inter-quartile range (IQR); kCal (kilocalories); Median (Med); not available (NA); standard deviation (SD)
Because investigation of these social aspects of eating behaviors is somewhat less common in studies of nutrient intake, we also report on associations between exposures and confounders to examine socioeconomic and demographic variation. The frequency of meals with others did not significantly vary by age, sex, education, or subjective social status. Differences in race/ethnicity, marital status, income, and household size, however, were significantly associated with meals with others. Greater household size, higher income, and being married were associated with more meals with others. Caucasian and Asian respondents reported the most weekly meals with others, while African American respondents reported the fewest meals with others.
Participant consumption of meals prepared at home (second social food behavior) was positively associated with higher HEI-2010 score, DASH score, and energy from carbohydrate, and negatively associated with total energy and energy from fat. The crude associations between meals prepared at home and age, sex, race, income, education or subjective social status were not statistically significant. Differences in marital status and household size were both significantly associated with frequency of meals prepared at home.
Eating more meals outside the home (third social food behavior) was associated with significantly higher consumption of total energy and energy from fat, significantly lower energy from carbohydrate, and lower diet quality on both indices, and significant differences in all demographic and socioeconomic variables except household size.
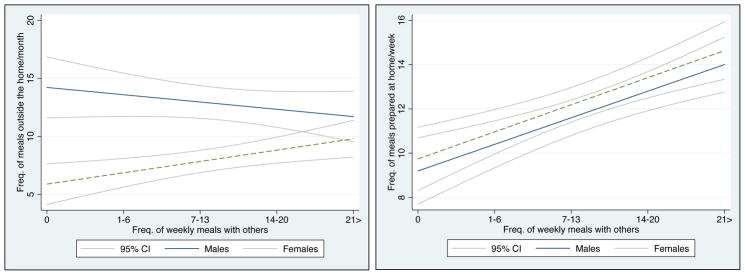
Although our primary goal is ultimately to assess how each of the social exposures are related to nutrient intake, it is useful to examine the relationship between these exposures. As a linear fit plot illustrates (Figure 1a), women who report eating more meals with others each week tend to eat more meals outside the home; in contrast, men who eat more meals with others tend to eat fewer meals outside the home. For men, the Pearson correlation between meals with others and eating out is ρ = −0.07, and for women is ρ = 0.12. Separately, there is a positive relationship between eating meals at home and eating meals with others for both men and women (Figure 1b). For men, the Pearson correlation between meals with others and eating out is ρ = 0.20, and for women is ρ = 0.18. These associations suggest that men and women may vary in terms of the extent of sociability they engage in with others when eating outside the home.
Figure 1.
(a) Bivariate linear association of meals out, by meals consumed with others. (b) Linear association of meals at home, by meals consumed with others.
Association between nutrient intake and meals with others
After adjusting for socioeconomic and demographic factors we found no clear or consistent evidence that meals with others was significantly associated with nutrient intake for men or women. However, among women, eating most of one’s meals with others (in the category of “>21 meals per week”) was marginally associated with poorer diet quality on the HEI-2010 measure relative to women who ate no meals with others (Table 3). A broader (albeit nonsignificant) trend observed between meals with others and both HEI and DASH diet quality outcomes is that men have a largely positive linear gradient between frequency of meals with others and diet quality, suggesting that men’s diet quality may benefit from meals with others. Women, on the other hand, demonstrate a nonlinear gradient, wherein relative to those who report no meals with others each week, women reporting 7–13 meals with others/week have the smallest magnitude of association with diet quality scores. This pattern is striking because the gradient-like trends – though only suggestive – are in completely opposite directions for men (positive) and women (negative). It is worth noting that those who eat all meals alone may be an unusual group and possibly socially isolated. Though according to a 2006–08 study by the US Bureau of Labor Statistics American Time Use Survey, in one-person households, 71% of meals were consumed alone, while in multi-person households, 27% of meals were alone (Hamrick, Andrews, Guthrie, Hopkins, & McClelland, 2011). In addition, as Yates and Warde (2017) recently pointed out in a study of social contexts of eating alone in British households, due to a rise in single-person households during the last half-century in Britain, nearly 30% of meals – and especially breakfasts and lunches – were eaten by oneself. Because of this uncertainty, an alternate set of analyses that specified a different reference category (1–6 meals per week instead of 0) showed similarly little association between meals with others and nutrient intake (analyses available from corresponding author).
Table 3.
Association between nutrient intake and meals eaten with others, stratified by sex
| Males | (a) Energy from fat (%) | (b) Energy from carb (%) | (c) Total energy (kCal, nat. log) | (d) HEI-2010 score | (e) DASH adherence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | |
| Meals with others/week (ref=0 meals) | |||||||||||||||
| 1–6 meals | 3.49 | (1.71) | 0.04** | −1.93 | (2.19) | 0.38 | 0.06 | (0.07) | 0.43 | −0.90 | (2.67) | 0.74 | −0.84 | (1.04) | 0.42 |
| 7–13 meals | 0.52 | (1.75) | 0.77 | −1.55 | (2.08) | 0.46 | 0.03 | (0.08) | 0.71 | 0.77 | (2.50) | 0.76 | −0.40 | (1.10) | 0.72 |
| 14–20 meals | 0.03 | (1.74) | 0.99 | −0.91 | (2.04) | 0.66 | 0.15 | (0.08) | 0.06 | 2.78 | (2.60) | 0.29 | 0.04 | (1.09) | 0.97 |
| > 21 meals | −0.55 | (1.72) | 0.75 | 2.35 | (2.09) | 0.26 | 0.06 | (0.07) | 0.38 | 2.86 | (2.47) | 0.25 | 0.89 | (1.01) | 0.38 |
| N= | 296 | 296 | 296 | 296 | 296 | ||||||||||
| Prob>F | 0.003 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||
| R2 | 0.15 | 0.15 | 0.18 | 0.10 | 0.14 | ||||||||||
| Females | (a) Energy from fat (%) | (b) Energy from carb (%) | (c) Total energy (kCal, nat. log) | (d) HEI-2010 score | (e) DASH adherence | ||||||||||
| Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | |
|
| |||||||||||||||
| Meals with others/week (ref=0 meals) | |||||||||||||||
| 1–6 meals | 1.99 | (1.43) | 0.17 | −1.81 | (1.59) | 0.26 | 0.06 | (0.08) | 0.48 | −3.60 | (2.50) | 0.15 | −1.13 | (0.89) | 0.21 |
| 7–13 meals | 1.60 | (1.43) | 0.26 | −1.56 | (1.57) | 0.32 | 0.02 | (0.08) | 0.80 | −1.20 | (2.33) | 0.61 | −1.08 | (0.99) | 0.27 |
| 14–20 meals | 1.87 | (1.52) | 0.22 | −1.12 | (1.78) | 0.53 | 0.08 | (0.08) | 0.36 | −2.44 | (2.40) | 0.31 | −1.41 | (1.01) | 0.16 |
| > 21 meals | 2.11 | (1.41) | 0.14 | −0.88 | (1.55) | 0.57 | 0.15 | (0.08) | 0.07 | −4.62 | (2.35) | 0.05** | −1.86 | (0.97) | 0.06 |
| N= | 323 | 323 | 323 | 323 | 323 | ||||||||||
| Prob>F | 0.01 | 0.06 | <0.001 | <0.001 | <0.001 | ||||||||||
| R2 | 0.13 | 0.07 | 0.15 | 0.12 | 0.16 | ||||||||||
P<0.05,
P<0.01
Note: Table reports estimates from 10 separate linear regression models for nutrient intake. Models adjust for respondent age, race, education, subjective social status, income, household size, marital status. All models except model (c) also adjust for energy intake (kcals).
Abbreviations: kCal = kilocalories, Coeff = unadjusted coefficient, Rob. SE = robust standard error
Association between nutrient intake and meal locations
Stratified adjusted linear regression models found that the proportion of meals consumed in the home was associated with a stepwise improvement in diet among men. Compared to men who ate no meals prepared at home, having 14–20 meals at home (at least 2 daily) was associated with three percent less energy from fat, a 6.8 point greater HEI score and 3 points greater on the DASH score, while those in the category of consuming more than 21 meals at home (at least 3 daily) had 4.5% less energy from fat, a 9-point greater HEI score and 3.5 points greater DASH score. Diet quality among men was not significantly associated with monthly meals consumed outside the home. Alternate analyses with an alternate reference category (1–13 weekly meals at home, and 1–4 monthly meals outside the home) had results similar to the original model specification of “no meals prepared at home” and “no outside meals” as reference categories (analyses available from corresponding author).
Similar to men, the number of meals consumed at home by women (relative to a reference category of 0 meals at home) was associated with lower intake of energy from fat but only at the highest level of meals prepared at home (>21 meals week). However, meals prepared at home did not appear to be associated with energy from carbohydrates, total calories, or either diet quality measure (Table 4). Women who most frequently ate outside the home (more than 11 times per month) consumed significantly more energy from fat (2.9% more), more total calories (nearly 34% more), and had a nearly 9-point lower HEI score and almost 4-point lower DASH score relative to women who ate no meals out.
Table 4.
Association between meal location and overall diet quality, stratified by sex
| Males | (a) Energy from fat (%) | (b) Energy from carb (%) | (c) Total energy (kCal, nat. log) | (d) HEI-2010 score | (e) DASH adherence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | |
| Meals prepared at home, weekly (ref=0) | |||||||||||||||
| 1–13 meals | −1.10 | (1.31) | 0.40 | −0.38 | (1.52) | 0.80 | −0.02 | (0.06) | 0.70 | 4.06 | (2.28) | 0.08 | 0.92 | (0.91) | 0.32 |
| 14–20 meals | −3.19 | (1.32) | 0.02** | 1.68 | (1.51) | 0.27 | −0.020 | (0.05) | 0.71 | 6.78 | (2.14) | 0.002*** | 3.06 | (0.93) | 0.001*** |
| > 21 meals | −4.48 | (1.56) | 0.005*** | 2.13 | (1.90) | 0.26 | −0.13 | (0.07) | 0.07 | 9.04 | (2.63) | 0.001*** | 3.52 | (1.11) | 0.002*** |
| Meals outside the home, monthly (ref=0) | |||||||||||||||
| 1–4 meals | 1.03 | (1.94) | 0.60 | −3.62 | (2.38) | 0.13 | 0.04 | (0.09) | 0.68 | 1.40 | (3.15) | 0.66 | 0.09 | (1.46) | 0.95 |
| 4–11 meals | 2.63 | (1.72) | 0.13 | −3.06 | (2.34) | 0.19 | 0.05 | (0.08) | 0.52 | 0.28 | (2.74) | 0.92 | 0.22 | (1.26) | 0.86 |
| > 11 meals | 3.26 | (1.83) | 0.08 | −4.47 | (2.38) | 0.06 | 0.05 | (0.08) | 0.51 | 0.59 | (2.89) | 0.84 | 0.32 | (1.30) | 0.81 |
| N= | 296 | 296 | 296 | 296 | 296 | ||||||||||
| Prob>F | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||
| R2 | 0.20 | 0.16 | 0.18 | 0.15 | 0.18 | ||||||||||
| Females | (a) Energy from fat (%) | (b) Energy from carb (%) | (c) Total energy (kCal, nat. log) | (d) HEI-2010 score | (e) DASH adherence | ||||||||||
| Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | Coeff. | Rob. SE | P | |
|
| |||||||||||||||
| Meals prepared at home, weekly (ref=0) | |||||||||||||||
| 1–13 meals | −0.53 | (1.23) | 0.67 | 0.47 | (1.42) | 0.74 | −0.13 | (0.06) | 0.02** | −0.45 | (2.27) | 0.84 | −0.74 | (0.80) | 0.35 |
| 14–20 meals | −0.01 | (1.14) | 0.99 | −1.02 | (1.24) | 0.42 | −0.04 | (0.05) | 0.43 | −0.23 | (2.08) | 0.91 | 0.04 | (0.76) | 0.96 |
| > 21 meals | −2.99 | (1.26) | 0.02** | 2.59 | (1.35) | 0.06 | −0.10 | (0.06) | 0.11 | 2.68 | (2.41) | 0.27 | 0.29 | (0.84) | 0.73 |
| Meals outside the home, monthly (ref=0) | |||||||||||||||
| 1–4 meals | 0.55 | (1.32) | 0.68 | −1.20 | (1.45) | 0.41 | 0.22 | (0.07) | 0.003*** | −3.71 | (2.57) | 0.15 | −2.35 | (0.86) | 0.006*** |
| 4–11 meals | 0.93 | (1.28) | 0.47 | −1.33 | (1.43) | 0.35 | 0.18 | (0.07) | 0.009*** | −2.51 | (2.71) | 0.36 | −1.70 | (0.87) | 0.053 |
| > 11 meals | 2.85 | (1.34) | 0.03** | −2.99 | (1.53) | 0.052 | 0.34 | (0.07) | <0.001*** | −8.59 | (2.83) | 0.003*** | −3.82 | (0.91) | <0.001*** |
| N= | 323 | 323 | 323 | 323 | 323 | ||||||||||
| Prob>F | <0.001 | 0.001 | <0.001 | <0.001 | <0.001 | ||||||||||
| R2 | 0.16 | 0.11 | 0.22 | 0.16 | 0.22 | ||||||||||
P<0.05,
P<0.01
Note: Table reports 10 separate linear regression models for nutrient intake. Models adjust for respondent age, race, education, subjective social status, income, household size, marital status. All models except model (c) also adjust for energy intake (kcals).
Abbreviations: kCal = kilocalories, Coeff = unadjusted coefficient, Rob. SE = robust standard error.
Discussion
It is already known that where meals are consumed and the extent to which one eats meals with others may affect food choice. In this study, we sought to go further and measure whether these important social aspects of eating were also then associated with nutrient intake using a validated diet recall protocol in a multiethnic sample of Americans with diabetes. Our first hypothesis was that the frequency of meals with others would be positively associated with caloric intake, and a second hypothesis was that meals with others would also be associated with diet quality. Indeed, increased caloric intake was associated with a greater frequency of meals with others in unadjusted bivariate analyses, but after stratifying by sex, this correlation was only significant for women. However, contrary to expectations, after adjusting for confounders neither men’s nor women’s frequency of meals with others was significantly associated with their nutrient intake.
Given that effects of social facilitation have been consistently found to predict increased energy intake in humans, this null finding was surprising. Several factors may explain the disconnect between this finding with the bulk of research on social facilitation. For one, the focus of the majority of commensality research has been the occasion of the meal; this study expands the scope of study beyond the single meal occasion to a retrospective report on a set of meals consumed with others during an average week. It is plausible that short-term social facilitation effects observed at a given mealtime vary considerably meal-to-meal, and are thus obscured in measures of nutrient intake observed over longer spans of time.
Given the relatively large sample size of this population study, we were able to adjust for a variety of possible confounders in the relationship between meals with others and nutrient intake. This benefit of including more information about an individual’s social context is not always a possibility in smaller studies, and may also help to explain how some of the modest bivariate association between an individual’s meals with others with measures of nutrient intake (energy and diet quality) becomes further attenuated when including additional confounders. It is also worth noting that the average age of respondents in this study, 63, was considerably older than the majority of research on social facilitation, which tends to skew younger and involve college-age samples. In a sensitivity analysis, we tested whether age moderated the association between meals with others and nutrient intake; there was no evidence for this. Still, this points to the fact that research on social facilitation has not yet systematically established how this phenomenon may vary over the life course.
There are other suggestive trends that warrant further investigation. Although it was not significant, the magnitude of association across men’s categories of meals with others suggests a positive gradient with diet quality (in terms of both HEI and DASH scores). Among women, on the other hand, there were signs of a negative and nonlinear gradient between diet quality and eating meals with others. A separate component of the second hypothesis was that, following Patel & Schlundt (2001), the association between meals with others and calories from fat was likely to be greater than the association between meals with others and calories from carbohydrate. Given that there was no evidence of a significant association between meals with others and calories from fat or carbohydrate, there is not support for this proposition. However, despite a lack of significance, the direction and magnitude of these associations were largely consistent in that there tended to be a positive association between meals with others and calories from fat, and a negative association between meals with others and calories from carbohydrate. Additional study in other population samples could further explore if men and women derive different nutritional benefits from eating with others over timescales beyond the meal occasion.
An additional set of analyses sought to test a third hypothesis of a positive relationship between meals prepared at home and nutrient intake, coupled with a negative relationship between meals outside the home and intake. An important strength of these analyses was that separate measures of meals prepared at home and meals consumed outside the home enabled us to adjust for one while holding levels of the other constant. There was partial support for this hypothesis; we indeed found that nutrient intake varied according to the number of meals prepared at home as well as outside the home, but these associations varied significantly by sex. Specifically, for men, eating more meals prepared at home was significantly and monotonically associated with a better diet as measured by lower fat intake and meaningfully higher scores on both HEI-2010 and DASH diet quality scores, while eating meals away from home was not associated with dietary indicators. Conversely, for women, eating meals prepared at home did not appear to be associated with diet quality but eating meals away from home was associated with a lower quality diet, especially when eating out often. These analyses suggest that meals prepared at home may be protective for male diet quality, whereas, women’s diet quality may be more vulnerable to meals consumed outside the home with no commensurate benefit for cooking at home.
Our findings with respect to men and women are complementary but not consistent with each other, and different mechanisms may explain differential returns to nutrient intake by sex. Given prior research showing negative ramifications to diet from excessive food consumed outside the home, it was surprising that only the diet quality of women was negatively associated with meals out and that only the diet quality of men was positively associated with meals prepared at home. Mechanisms that might explain the outcome span a gendered division of labor; whether meals consumed outside the home were taken in company or alone; possible differences in family member schedules; and intentionality of the food preparer, among others. This study is better positioned to document these differences than to explain them. For instance, research on sex and gender differences in the household division of labor suggests that although men’s share of time spent cooking has more than doubled during the last 50 years, a significant gender gap remains (Flagg, Sen, Kilgore, & Locher, 2014; L. P. Smith, et al., 2013). This gender gap is also present in the present analytic sample. A separate survey question asked participants where they obtain ideas for cooking, to which 92% of the sample (n=710) responded. Of those who responded with the answer, “I don’t cook” (16%, n=114), 82% were men (n=93) and 18% were women (n=21). Given this is an older-skewing population of individuals with diabetes, the increase in men’s diet quality associated with more meals at home suggests that their diet quality is likely benefiting disproportionately from someone cooking for them.
Whether meals consumed outside the home were taken in company or alone is important information that future research could help to clarify in terms of the observed sex difference in nutrient intake by meal location. Analysis of the crude association between meal location and frequency of eating suggests that women who report more meals with others also eat out more, whereas there is an inverse association for men. Although we cannot assess the reasons why study participants reported eating food outside the home, if as Paddock, Warde, Whillans (2017) suggest, women tend to eat outside the home more for reasons of sociability, and because women may be more likely to eat out in groups than men, then social facilitation may help to explain why women have poorer diet quality (HEI-2010) scores. This explanation does not, however, address why men’s HEI-2010 score would demonstrate a significant positive gradient with meals prepared at home, while women’s HEI-2010 score would show no significant association or trend. Further research on the interaction of eating out, meal preparation in the home, and the attributes of meal partners with whom individuals eat meals may help to illuminate these processes.
There are limitations to what can be inferred from this study. The measure of commensal eating we used was designed to probe participants’ recall of meals consumed with others during the prior week with specific types of social relations. There was adequate variation in the frequency of meals with others by sex to test hypotheses about nutrient intake. The findings of positive bivariate associations of meals with others with energy intake volume comport with findings of a wide range of laboratory-based and free-living commensality studies. However, due to the imprecision of the measurement, we cannot distinguish whether a participant who reported a meal consumed with a spouse and also a meal consumed with a neighbor was, in fact, referring to the same meal. Thus, while the measure indicates the relative extent of commensality within the sample of respondents, a respondent’s answer likely overestimates the absolute number of meals consumed with others per week.
Although the study sample was comprised of adults with diabetes, the overall diet quality of participants who contributed to this study was similar, and slightly better than that of the overall American population. The average participant HEI-2010 score (μ=65.7) was higher than recently available nationally-representative diet data based on HEI-2005 data (μ40–59 years=57.0, μ60+ years=63.8, using NHANES 1999–2002 data)(Ervin, 2011). This somewhat better diet than the average American may be due to the fact that participants in this sample received considerable health education about diet. Average participant accordance with the DASH diet (μ=23.7) was also slightly higher than recently available nationally-representative diet data (μ=20.7, using NHANES 2001–2002 data) (Monsivais, Rehm, & Drewnowski, 2013), but still relatively low (the upper limit of the scale is 40). However, given that these nationally-representative data are more than 15 years old, comparisons should be interpreted with caution.
Knowing more information about attributes of an individual’s eating partners may benefit future population-scale research in terms of assessing how an individual’s multiple eating partners reinforce healthy or unhealthy eating habits. For instance, given that individuals with lower socioeconomic status tend to have unhealthier diet, and given propensities for individuals to build social networks with those who are similar to them (Marsden, 1987; J. A. Smith, McPherson, & Smith-Lovin, 2014), it may be that social networks reinforce unhealthy eating more so among low-SES individuals, and networks reinforce healthy eating more among high-SES individuals. Although some research shows that individuals with more education tend to have a greater diversity of social ties (Marsden, 1987), the propensity for individuals to mate with those of similar education may be, in fact, greater for those who are more educated (Skopek, Schulz, & Blossfeld, 2010). Thus, there may be greater reinforcement of eating behaviors – healthy or unhealthy – within high-SES individuals’ social networks. As J. A. Smith, et al. (2014) relay, however, there is variation among multiple forms of similarity within one’s network contacts; educational homophily tends to be weaker than race or religious homophily, and so these multiple traits of network contacts could be accounted for and tested in models estimating network effects on nutrient intake.
No causal inferences can be made due to the cross-sectional design of this study. Future research that integrates measurement of commensality with a longitudinal design would be beneficial to evaluate how different aspects of mealtime sociability change over time, as well as how these changes may shape diet quality, food choices, and other cardiometabolic risk factors. Given the lack of prior research on commensality and nutrient intake, our aims were to evaluate multiple associations between sociability propensity and different types of nutrient intake including several common nutrient measures (% energy from fat, % energy from carbohydrate, and total energy) and indices of diet quality (HEI, DASH scores). We chose not to adjust regression estimates for multiple hypothesis tests because of the known tradeoff of Bonferroni (or other similar corrections) between Type 1 and Type 2 errors (Gelman, Hill, & Yajima, 2012). While we do discuss common trends, we remain conservative and do not give special emphasis to discussion of associations above conventional levels of significance (p>0.05). Given the robust and productive debate across epidemiological and social scientific fields about the “multiple comparison problem”, “p-hacking”, and errors of “Type S”(sign) and “Type M”(magnitude) in observational data (Gelman, et al., 2012; Goeman & Solari, 2014; J. R. Thompson, 1998), this is a design decision that future work may address through study pre-registration, statistical approaches such as Bayesian or multi-level modeling, and testing hypotheses in an experimental framework.
Finally, individuals who were missing complete covariate information were omitted from analyses. Scrutiny of those who were omitted suggest that omitted men consumed less energy from fat and carbohydrate, and had fewer meals with others. Women who were omitted also consumed less energy from fat and carbohydrate, as well as had lower total energy intake. Speculatively, if men who are omitted tend to have fewer meals with others than those included in the analyses, it could be that the true association between meals with others and diet quality might be more positively biased. If this analysis under-represents those women who eat out less, the true association between women who report fewer meals out and their diet quality may have a positive bias as well, although the other categories of eating out suggest that the magnitude would still be negative. This said, neither men nor women had significant differences in overall diet (HEI, DASH) between those who were included and omitted.
In conclusion, we found, surprisingly, that there was no significant association between the frequency of eating meals with others and nutrient intake for either men or women after adjusting for a wide range of known confounders, though there were some suggestive differences in this association by sex that warrant further study. Eating more meals outside the home or eating meals prepared at home may have different ramifications for diet quality depending upon the sex of the eater. Findings indicate that men’s diet quality may benefit from consuming more meals prepared at home (net of meals eaten outside the home), and that women’s diet quality may be adversely harmed by meals outside the home (net of meals prepared at home). Future research should continue to evaluate the mechanisms that contribute to the association between these social aspects of eating environments and diet quality. In future population research on this topic, it may be especially worthwhile to incorporate additional information about eating partners (as network research endeavors to do), as well as information on meal occasions (as small-group research on social facilitation has traditionally done). This type of synthetic approach to evaluating such mechanisms may offer useful means for targeted recommendations to bolster health-promoting eating behaviors and inhibiting risk-promoting behaviors among persons with type 2 diabetes and in the general population as well.
Acknowledgments
Dr. Pachucki would like to thank Anne Thorndike, Seth Berkowitz, Sridharan Raghavan, Doug Levy, and James Meigs for comments on an early presentation of this manuscript; and Anthony Paik, David Cort, and Youngjoon Bae for conversations and feedback that improved the manuscript. The authors have no conflicts of interest to declare.
Funding: This study was supported by the NIH National Institute of Diabetes and Digestion and Kidney study “Neighborhood Effects on Weight Change and Diabetes Risk Factors (PI Barbara Laraia, R01 DK080744). The DISTANCE study group was further supported by NIDDK (R01 DK065664) and (P30 DK092924-06). Salary support for development of the social food behaviors module of the survey was provided during Dr. Pachucki’s fellowship with the Robert Wood Johnson Foundation Health & Society Scholars Program at UCSF & UC Berkeley.
References
- (ERS), E. R. S. Food Expenditures. Economic Research Service, U.S. Department of Agriculture (USDA); 2016. Food away from home as a share of food expenditures. [Google Scholar]
- Adler N, EE, GC, JI Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy white women. Health Psychology. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- Bellisle F, Dalix A, de Castro JM. Eating patterns in French subjects studied by the “weekly food diary” method. Appetite. 1999;32:46–52. doi: 10.1006/appe.1998.0195. [DOI] [PubMed] [Google Scholar]
- Berkowitz SA, Karter AJ, Lyles CR, Liu JY, Schillinger D, Adler NE, Moffet HH, Sarkar U. Low Socioeconomic Status is Associated with Increased Risk for Hypoglycemia in Diabetes Patients: the Diabetes Study of Northern California (DISTANCE) Journal of health care for the poor and underserved. 2014;25:478. doi: 10.1353/hpu.2014.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns C, Jackson M, Gibbons C, Stoney RM. Foods prepared outside the home: association with selected nutrients and body mass index in adult Australians. Public Health Nutr. 2002;5:441–448. doi: 10.1079/phn2001316. [DOI] [PubMed] [Google Scholar]
- Clendenen VI, Herman CP, Polivy J. Social facilitation of eating among friends and strangers. Appetite. 1994;23:1–13. doi: 10.1006/appe.1994.1030. [DOI] [PubMed] [Google Scholar]
- Conklin AI, Forouhi NG, Surtees P, Khaw KT, Wareham NJ, Monsivais P. Social relationships and healthful dietary behaviour: Evidence from over-50s in the EPIC cohort, UK. Soc Sci Med. 2014;100:167–175. doi: 10.1016/j.socscimed.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruwys T, Bevelander KE, Hermans RC. Social modeling of eating: A review of when and why social influence affects food intake and choice. Appetite. 2014 doi: 10.1016/j.appet.2014.08.035. [DOI] [PubMed] [Google Scholar]
- Dall TM, Yang W, Halder P, Pang B, Massoudi M, Wintfeld N, Semilla AP, Franz J, Hogan PF. The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care. 2014;37:3172–3179. doi: 10.2337/dc14-1036. [DOI] [PubMed] [Google Scholar]
- de Castro JM. Family and friends produce greater social facilitation of food intake than other companions. Physiol Behav. 1994;56:445–445. doi: 10.1016/0031-9384(94)90286-0. [DOI] [PubMed] [Google Scholar]
- de Castro JM. Eating behavior: lessons from the real world of humans. Nutrition. 2000;16:800–813. doi: 10.1016/s0899-9007(00)00414-7. [DOI] [PubMed] [Google Scholar]
- de Castro JM, Brewer EM. The amount eaten in meals by humans is a power function of the number of people present. Physiol Behav. 1992;51:121–125. doi: 10.1016/0031-9384(92)90212-k. [DOI] [PubMed] [Google Scholar]
- de la Haye K, Robins G, Mohr P, Wilson C. Adolescents’ Intake of Junk Food: Processes and Mechanisms Driving Consumption Similarities Among Friends. Journal of Research on Adolescence. 2013;23:524–536. [Google Scholar]
- Dhurandhar NV, Schoeller D, Brown AW, Heymsfield SV, Thomas D, Sorensen TIA, Speakman JR, Jeansonne M, Allison DB, Working EBM. Energy balance measurement: when something is not better than nothing. Int J Obes (Lond) 2015;39:1109–1113. doi: 10.1038/ijo.2014.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ervin RB. Healthy Eating Index--2005 total and component scores for adults aged 20 and over: National Health and Nutrition Examination Survey, 2003–2004. Natl Health Stat Report. 2011:1–9. [PubMed] [Google Scholar]
- Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed. 1989;30:47–57. doi: 10.1016/0169-2607(89)90122-3. [DOI] [PubMed] [Google Scholar]
- Fischler C. Commensality, society and culture. Social Science Information. 2011;50:528–548. [Google Scholar]
- Flagg LA, Sen B, Kilgore M, Locher JL. The influence of gender, age, education and household size on meal preparation and food shopping responsibilities. Public Health Nutr. 2014;17:2061–2070. doi: 10.1017/S1368980013002267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, Albright AL, Gregg EW. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312:1218–1226. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- Gelman A, Hill J, Yajima M. Why We (Usually) Don’t Have to Worry About Multiple Comparisons. Journal of Research on Educational Effectiveness. 2012;5:189–211. [Google Scholar]
- Goeman JJ, Solari A. Multiple hypothesis testing in genomics. Statistics in Medicine. 2014;33:1946–1978. doi: 10.1002/sim.6082. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, Kahle LL, Krebs-Smith SM. Update of the healthy eating index: HEI-2010. J Acad Nutr Diet. 2013;113:569–580. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamrick KS, Andrews M, Guthrie J, Hopkins D, McClelland K. How much time do Americans spend on food. US Department of Agriculture, Economic Research Service; 2011. [Google Scholar]
- Herman CP. The social facilitation of eating. A review. Appetite. 2015;86:61–73. doi: 10.1016/j.appet.2014.09.016. [DOI] [PubMed] [Google Scholar]
- Herman CP, Roth DA, Polivy J. Effects of the presence of others on food intake: A normative interpretation. Psychological Bulletin. 2003;129:873–886. doi: 10.1037/0033-2909.129.6.873. [DOI] [PubMed] [Google Scholar]
- Higgs S. Social norms and their influence on eating behaviours. Appetite. 2014 doi: 10.1016/j.appet.2014.10.021. [DOI] [PubMed] [Google Scholar]
- Higgs S, Thomas J. Social influences on eating. Current Opinion in Behavioral Sciences 2015 [Google Scholar]
- Jones-Smith JC, Karter AJ, Warton EM, Kelly M, Kersten E, Moffet HH, Adler N, Schillinger D, Laraia BA. Obesity and the food environment: income and ethnicity differences among people with diabetes: the Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36:2697–2705. doi: 10.2337/dc12-2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant AK, Graubard BI. Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med. 2004;38:243–249. doi: 10.1016/j.ypmed.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Kennedy ET, Ohls J, Carlson S, Fleming K. The healthy eating index: design and applications. J Am Diet Assoc. 1995;95:1103–1108. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- Kroshus E. Gender, Marital Status, and Commercially Prepared Food Expenditure. J Nutr Educ Behav. 2008;40:355–360. doi: 10.1016/j.jneb.2008.05.012. [DOI] [PubMed] [Google Scholar]
- Laraia BA, Karter AJ, Warton EM, Schillinger D, Moffet HH, Adler N. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE) Soc Sci Med. 2012;74:1082–1090. doi: 10.1016/j.socscimed.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund TB, Kjaernes U, Holm L. Eating out in four Nordic countries: National patterns and social stratification. Appetite. 2017;119:23–33. doi: 10.1016/j.appet.2017.06.017. [DOI] [PubMed] [Google Scholar]
- Mancino L, Todd J, Lin BH. Separating what we eat from where: Measuring the effect of food away from home on diet quality. Food Policy. 2009;34:557–562. [Google Scholar]
- Marsden PV. Core Discussion Networks of Americans. American Sociological Review. 1987;52:122–131. [Google Scholar]
- Moffet HH, Adler N, Schillinger D, Ahmed AT, Laraia B, Selby JV, Neugebauer R, Liu JY, Parker MM, Warton M, Karter AJ. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)--objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol. 2009;38:38–47. doi: 10.1093/ije/dyn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monsivais P, Rehm CD, Drewnowski A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern Med. 2013;173:1922–1924. doi: 10.1001/jamainternmed.2013.9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myhre JB, Loken EB, Wandel M, Andersen LF. Eating location is associated with the nutritional quality of the diet in Norwegian adults. Public Health Nutr. 2014;17:915–923. doi: 10.1017/S1368980013000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orfanos P, Naska A, Trichopoulos D, Slimani N, Ferrari P, van Bakel M, Deharveng G, Overvad K, Tjonneland A, Halkjaer J, Santucci de Magistris M, Tumino R, Pala V, Sacerdote C, Masala G, Skeie G, Engeset D, Lund E, Jakszyn P, Barricarte A, Chirlaque MD, Martinez-Garcia C, Amiano P, Quiros JR, Bingham S, Welch A, Spencer EA, Key TJ, Rohrmann S, Linseisen J, Ray J, Boeing H, Peeters PH, Bueno-de-Mesquita HB, Ocke M, Johansson I, Johansson G, Berglund G, Manjer J, Boutron-Ruault MC, Touvier M, Clavel-Chapelon F, Trichopoulou A. Eating out of home and its correlates in 10 European countries. The European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2007;10:1515–1525. doi: 10.1017/S1368980007000171. [DOI] [PubMed] [Google Scholar]
- Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101:2170–2177. doi: 10.2105/AJPH.2011.300282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachucki MC. Alimentation et réseau social: une étude sur «le goût par nécessité» en contexte social. Sociologie et sociétés. 2014;46:229–252. doi: 10.7202/1027149ar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paddock J, Warde A, Whillans J. The changing meaning of eating out in three English cities 1995–2015. Appetite. 2017;119:5–13. doi: 10.1016/j.appet.2017.01.030. [DOI] [PubMed] [Google Scholar]
- Patel KA, Schlundt DG. Impact of moods and social context on eating behavior. Appetite. 2001;36:111–118. doi: 10.1006/appe.2000.0385. [DOI] [PubMed] [Google Scholar]
- Pemberton VL, McCrindle BW, Barkin S, Daniels SR, Barlow SE, Binns HJ, Cohen MS, Economos C, Faith MS, Gidding SS, Goldberg CS, Kavey RE, Longmuir P, Rocchini AP, Van Horn L, Kaltman JR. Report of the National Heart, Lung, and Blood Institute’s Working Group on obesity and other cardiovascular risk factors in congenital heart disease. Circulation. 2010;121:1153–1159. doi: 10.1161/CIRCULATIONAHA.109.921544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polivy J, Pliner P. “She got more than me”. Social comparison and the social context of eating. Appetite. 2014 doi: 10.1016/j.appet.2014.08.007. [DOI] [PubMed] [Google Scholar]
- Prevention, C. f. D. C. a. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2017. [Google Scholar]
- Research, T. A. A. f. P. O. Standard definitions: Final disposition of case codes and outcome rates for surveys. Lenexa, Kansas: The American Association for Public Opinion Research; 2008. [Google Scholar]
- Rozin P. Food choice, acceptance and consumption. Springer; 1996. The socio-cultural context of eating and food choice; pp. 83–104. [Google Scholar]
- Salvy SJ, Jarrin D, Paluch R, Irfan N, Pliner P. Effects of social influence on eating in couples, friends and strangers. Appetite. 2007;49:92–99. doi: 10.1016/j.appet.2006.12.004. [DOI] [PubMed] [Google Scholar]
- Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:e2014009. doi: 10.4178/epih/e2014009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sievert YA, Schakel SF, Buzzard IM. Maintenance of a nutrient database for clinical trials. Control Clin Trials. 1989;10:416–425. doi: 10.1016/0197-2456(89)90006-8. [DOI] [PubMed] [Google Scholar]
- Skopek J, Schulz F, Blossfeld HP. Who contacts whom? Educational homophily in online mate selection. European Sociological Review. 2010;27:180–195. [Google Scholar]
- Smith JA, McPherson M, Smith-Lovin L. Social Distance in the United States: Sex, Race, Religion, Age, and Education Homophily among Confidants, 1985 to 2004. American Sociological Review. 2014;79:432–456. [Google Scholar]
- Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutr J. 2013;12:45. doi: 10.1186/1475-2891-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobal J, Nelson MK. Commensal eating patterns: a community study. Appetite. 2003;41:181–190. doi: 10.1016/s0195-6663(03)00078-3. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LP; 2017. [Google Scholar]
- Stoddard PJ, Laraia BA, Warton EM, Moffet HH, Adler NE, Schillinger D, Karter AJ. Neighborhood deprivation and change in BMI among adults with type 2 diabetes: the Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36:1200–1208. doi: 10.2337/dc11-1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Thompson FE, Kirkpatrick SI, Subar AF, Reedy J, Schap TE, Wilson MM, Krebs-Smith SM. The National Cancer Institute’s Dietary Assessment Primer: A Resource for Diet Research. J Acad Nutr Diet. 2015;115:1986–1995. doi: 10.1016/j.jand.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JR. Invited commentary: Re: “Multiple comparisons and related issues in the interpretation of epidemiologic data”. American Journal of Epidemiology. 1998;147:801–806. doi: 10.1093/oxfordjournals.aje.a009530. [DOI] [PubMed] [Google Scholar]
- Vartanian LR. Impression management and food intake. Current directions in research. Appetite. 2014 doi: 10.1016/j.appet.2014.08.021. [DOI] [PubMed] [Google Scholar]
- Virudachalam S, Long JA, Harhay MO, Polsky DE, Feudtner C. Prevalence and patterns of cooking dinner at home in the USA: National Health and Nutrition Examination Survey (NHANES) 2007–2008. Public Health Nutr. 2014;17:1022–1030. doi: 10.1017/S1368980013002589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett W. Nutritional epidemiology. 3. Oxford ; New York: Oxford University Press; 2013. [Google Scholar]
- Yates L, Warde A. Eating together and eating alone: meal arrangements in British households. British Journal of Sociology. 2017;68:97–118. doi: 10.1111/1468-4446.12231. [DOI] [PubMed] [Google Scholar]
- Young ME, Mizzau M, Mai NT, Sirisegaram A, Wilson M. Food for thought. What you eat depends on your sex and eating companions. Appetite. 2009;53:268–271. doi: 10.1016/j.appet.2009.07.021. [DOI] [PubMed] [Google Scholar]