Abstract
Objective
To systematically review the symptoms reported by patients with bilateral vestibulopathy (BV) in clinical studies and case reports. This would serve as the first step in establishing a validated patient-reported outcome measures (PROM) for BV.
Methods
A search on symptoms reported by patients with BV was performed in PubMed, and all publications covering these symptoms were included. Exclusion criteria comprised reviews and insufficient details about the frequency of occurrence of symptoms.
Results
1,442 articles were retrieved. 88 studies were included (41 clinical studies, 47 case reports). In consensus, 68 descriptions of symptoms were classified into 6 common and generic symptoms. Frequency of symptoms in clinical studies and case reports were reviewed, respectively; imbalance (91 and 86%), chronic dizziness (58 and 62%), oscillopsia (50 and 70%), and recurrent vertigo (33 and 67%). BV could be accompanied by hearing loss (33 and 43%) and tinnitus (15 and 36%). 15 clinical studies and 10 case reports reported symptoms beyond vestibular and hearing deficits such as limited social activities, depression, concentration, and memory impairment and reduced quality of life in general.
Conclusion
The literature on BV symptomatology mainly focuses on classic symptoms such as imbalance and oscillopsia, while only few report additional symptoms such as cognitive memory impairment and performing dual tasks. In fact, none of the reviewed clinical studies and case reports provided a comprehensive overview of BV symptoms. To develop a validated PROM, qualitative research using semi-structured and unstructured interviews is needed to explore the full spectrum of BV symptoms.
Keywords: bilateral vestibulopathy, symptoms, dizziness, vertigo, imbalance, oscillopsia, bilateral vestibular hypofunction, patient-reported outcome measures
Introduction
Bilateral vestibulopathy (BV) is a heterogeneous chronic condition in which the vestibular function is bilaterally absent or reduced (1). BV can be due to a dysfunction of the vestibular organs, nerves, and/or the brain (1, 2). In 2017, consensus was reached by the Classification Committee of the Bárány Society about the diagnostic criteria of BV (3). Symptoms for diagnosis include unsteadiness when walking or standing, movement-induced blurred vision/oscillopsia during walking or quick head movements, or worsening of unsteadiness on uneven ground and/or darkness (1, 3, 4). However, clinical experience and current literature point to a wider variety of symptoms (5). For example, many patients report a negative impact on physical and social functioning, and compromised cognitive abilities (6–8).
At this moment, questionnaires like the dizziness handicap inventory (DHI) exist to quantify the dizziness symptoms. However, these questionnaires are not specific for vestibular loss (9). Therefore, the objective of this study was to systematically evaluate the nature and frequency of BV symptoms reported in clinical studies and case reports. This would serve as the first step in establishing validated patient-reported outcome measures (PROM) specifically for patients with BV (10). This is a tool to measure patient perceptions of their own functional status and well-being (11).
Methods
Information Source and Search Strategy
A systematic literature search was performed according to the PRISMA statement in the bibliographical database PubMed based on the following keywords: Bilateral[All Fields] AND ((Vestibular[All Fields] AND (Hypofunction[All Fields] OR Failure[All Fields] OR Loss[All Fields])) OR Vestibulopathy[All Fields]) (12). At the beginning, a full search was performed followed by entering some additional restrictions. The outcomes of this selection were first screened by title and then also by abstract. The last selection included a complete reading of the articles found. The selections and full article analysis was performed by the first two authors (Florence Lucieer and Stijn Duijn).
Selection Criteria and Study Selection
A requirement in the basic search was that all articles were written in English. All publications reporting on symptoms of patients with BV were considered, including all types of BV (central, peripheral, or mixed etiology).
Title Screening
Articles were excluded in case of animal studies, if they did not report on BV, if they did not report on symptoms of patients with BV, if no or insufficient details on the frequency of symptoms were available, and in case of systematic reviews, comments, errata, or books.
Abstract Screening
Exclusion criteria were the same as for title screening. In case an abstract was not available, the full article was screened to search for any of the exclusion criteria.
Full-Text Review
In case the full article was not available, the article was excluded. Whenever the inclusion or exclusion criterion of an article included only “unsteadiness” or “oscillopsia,” or “unsteadiness and oscillopsia,” the article was excluded, so few reported symptoms could lead to a bias of interpretation of the frequency of the symptoms.
Data Collection Process and Risk of Bias Assessment
Title selection, abstract selection, full read through selection, and the analysis of the included articles were performed by the first and second author (Florence Lucieer and Stijn Duijn). The list of articles found in the PubMed search was exported to EndNote X8 for Windows and Mac (Clarivate Analytics, Philadelphia). This Endnote library was then used to perform the title, abstract, and full article selection by the two researchers separately. After the title and abstract screening the articles of both researchers were combined and duplicates were removed. After full article selection, articles were combined. Discrepancies between the two authors were discussed and a consensus was reached about selecting the articles for data analysis. A Cohen’s kappa of the full article selection was calculated to evaluate the interrater reliability (13).
The nature and frequency of symptoms and the total number of patients were extracted by the first two authors and compiled using Microsoft Excel. If only percentages were reported, the authors were contacted to get the exact number of patients. The method of symptom collection in the articles was collected to assess risk of bias of the studies. Clinical studies and case reports were analyzed separately.
Qualitative Data Synthesis
The primary outcome measure of this systematic review was a detailed overview regarding nature and frequency of symptoms of BV as reported in clinical studies and case reports. Three authors (Florence Lucieer, Stijn Duijn, and Raymond van de Berg) reviewed the list of descriptions. In consensus, these descriptions were categorized into common symptoms. The frequency of these common symptoms was calculated.
Results
Search Process
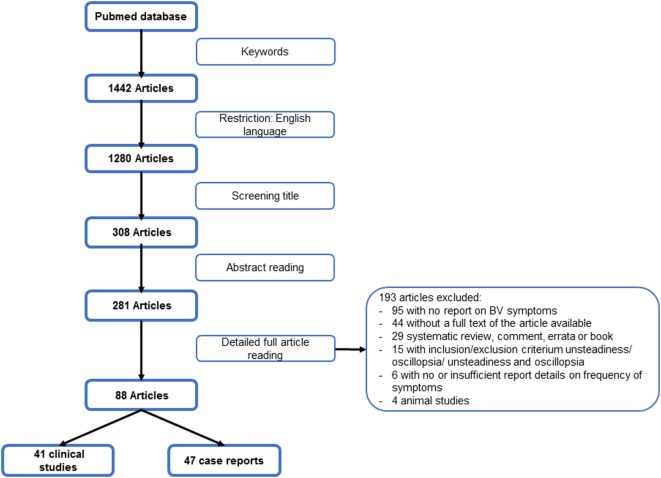
The search was conducted in the bibliographical database PubMed on October 25, 2017. The initial search resulted in 1,442 publications. For a schematic overview of the search strategy, see Figure 1. A high level of interrater reliability was reached on the full article selection with a Cohen’s kappa of 0.98. Finally, 1,385 unique patients from 41 clinical studies and 86 patients from 47 case reports were included (2, 5, 14–99). The characteristics of these articles can be found in Tables A1 and A2 in Supplementary Material.
Figure 1.
Flowchart search strategy.
Demographic Data of the Articles
Twenty-two of the clinical studies were European, 12 North-American, 4 Asian, 3 Australian, and 1 South-American, dated between 1984 and 2017. Twenty-one case reports were European, 13 North-American, 11 Asian, 1 Australian, and 1 South-American, originated from 1985 until 2017.
Classification of Symptoms
Sixty-eight descriptions of BV symptoms were retrieved. In consensus, these descriptions were classified into six universal symptoms: imbalance (including worsening in darkness or on uneven grounds), chronic dizziness, oscillopsia, recurrent vertigo, hearing loss, and tinnitus. Data from these six universal symptom classes can be found in Table A3 in Supplementary Material.
Clinical Studies
Symptoms found in clinical studies are presented in Table 1. Two times, two publications were merged in the results because of reporting duplicate data (24, 74, 97, 98). Imbalance was the most frequent symptom (91.4%). Fifteen clinical studies reported additional symptoms, for example, socio-economic impacts, depression, cognitive impairment, and increased risk of falling (5, 16, 27, 32, 43, 45, 54, 60, 63, 75, 76, 81–83, 90).
Table 1.
Nature and frequency of most common symptoms reported by patients with bilateral vestibulopathy in clinical studies.
| Symptom | n/t | Reported (%) |
|---|---|---|
| Imbalance Worse in darkness On uneven ground |
1,025/1,121 110/115 12/12 |
91.4% 95.7% 100% |
| Chronic dizziness | 86/149 | 57.7% |
| Oscillopsia | 559/1,116 | 50.1% |
| Recurrent vertigo | 267/808 | 33.0% |
| Hearing loss | 256/787 | 32.5% |
| Tinnitus | 59/398 | 14.8% |
n, number of patients reporting the symptom; t, total number of patients in subset.
Case Reports
Symptoms found in case studies are presented in Table 2. Imbalance was the major symptom (86.1%). Ten case reports reported additional symptoms like sleep disturbances, unable to perform daily chores, and appearing to be depressed (18, 28, 30, 62, 67, 68, 70, 89, 91, 94). For a complete overview of additional symptoms in clinical studies and case reports, see Table 3.
Table 2.
Nature and frequency of most common symptoms reported by patients with bilateral vestibulopathy in case reports.
| Symptom | n/t | Reported (%) |
|---|---|---|
| Imbalance Worse in darkness On uneven ground |
62/72 28/42 7/13 |
86.1% 66.7% 53.8% |
| Chronic dizziness | 21/34 | 61.8% |
| Oscillopsia | 40/57 | 70.2% |
| Recurrent vertigo | 36/54 | 66.7% |
| Hearing loss | 30/70 | 42.9% |
| Tinnitus | 10/28 | 35.7% |
n, number of patients reporting the symptom; t, total number of patients in subset.
Table 3.
Additional symptoms in bilateral vestibulopathy reported in articles.
| Additional symptoms | |
|---|---|
| Clinical studies |
|
| Case reports |
|
Discussion
After a structural review until October 2017, 41 clinical studies and 47 case reports were reviewed to determine the nature and frequency of symptoms experienced by patients with BV. No study was identified that created an inventory of patient-reported outcomes. Almost all patients suffered from imbalance, chronic dizziness, and oscillopsia, next to other inner ear problems like hearing loss and tinnitus. The high rate of imbalance and oscillopsia comply with the recent diagnostic criteria for BV (3). However, additional symptoms were rarely mentioned.
Hearing loss and tinnitus most likely shared the same etiology as BV or resulted from aging, rather than from vestibular dysfunction. A typical example for this is aminoglycoside toxicity is a well-known cause of sensorineural hearing loss and vestibular dysfunction (2, 97, 100). In addition, the average patient with BV in the literature was 60–62 years old and the prevalence of hearing loss in the United States is 25.1 and 42.7% for the age groups 55–64 and 65–84, respectively (101). The same conclusion could be drawn for recurrent vertigo. Vertigo is most likely an expression of the shared etiology, but is not the result of BV since an absent or reduced vestibular function is most likely not the cause of attacks of vertigo (2, 4).
Only 15 clinical studies and 10 case reports reported additional symptoms. The existence of these symptoms is supported by other literature that suggested that patients with BV could also suffer from cognitive deficits (7, 8), autonomic (102–104) and psychological symptoms (6, 105, 106), tiredness (6), visually induced dizziness (7, 107, 108), and impaired quality of life (6, 90, 106). Unfortunately, these symptoms could not reliably be quantified since they were not often mentioned in clinical studies and case reports. At this moment, it is uncertain why these symptoms were reported so infrequently. It could be hypothesized that these symptoms did have a low occurrence, that they were not part of routine history taking, or that patients were not aware of the link between their vestibular deficit and these types of symptoms (4). Therefore, structured patient interviews with open-ended questions should be conducted in which patients with BV are specifically asked to describe all of their symptoms and thereby evaluate in which words they describe their own symptoms, to determine the nature and frequency of all symptoms related to BV. This is necessary to develop PROM for BV (10).
At this moment, vestibular specific PROM exist like the DHI (109) and the vestibular disorders activities of daily living scale (VADL) (110). The DHI evaluates different aspects of vestibular complaints (function, physical, and emotional) and the VADL assesses the independency in activities of daily living. However, both questionnaires only focus on balance and do not assess the classic BV symptoms like oscillopsia, recurrent vertigo, hearing loss, and tinnitus. Therefore, there is also a need for PROM for BV specifically.
Several limitations of this systematic review were identified. Almost all articles gathered data differently and many of them were of retrospective nature. It was uncertain whether all publications used an open interview and whether all symptoms were explicitly mentioned or not. In addition, it was not possible to determine whether symptoms were mentioned but denied, or not even mentioned at all. Moreover, patients can describe the same complaint (e.g., dizziness and vertigo) differently. As a result, the same complaints could be categorized into different universal symptoms (4, 111). In addition, different articles used various diagnostic criteria for BV, resulting in a heterogeneous patient population, which made direct comparison of the patient population between articles difficult. Furthermore, it is known that BV is often misdiagnosed and missed (4, 90). This implies that even the percentages mentioned in literature do not reflect the real prevalence of the symptoms. Finally, only three clinical studies and one case report measured quality of life (e.g., DHI and HADS), therefore, outcomes could not be pooled for analysis (27, 30, 41, 42).
In this review, clinical studies and case reports provided complimentary information. Clinical studies were better in quantifying the established symptoms and case reports were better in giving an overview of the array of symptoms.
In the future, a qualitative research model would be of added value. This would allow getting a clear overview of all symptoms patients with BV experience, including additional symptoms.
Conclusion
Current literature on BV symptomatology mainly focuses on classic symptoms such as imbalance and oscillopsia, while only a few report additional symptoms such as cognitive memory impairment and dual tasking. In fact, none of the reviewed clinical studies and case reports provided a comprehensive overview of BV symptoms. To develop validated PROM, a qualitative research using semi-structured and unstructured interviews is needed to explore the full spectrum of BV symptoms.
Author Contributions
All authors contributed extensively to the work presented in this paper. FL and SD conducted the analysis and wrote the manuscript. RB supervised the writing and edited the manuscript. HK supervised the writing and reviewed the manuscript. VR, AF, NG, and JP reviewed the manuscript.
Conflict of Interest Statement
The first author was supported through funding of MedEl. The remaining coauthors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The reviewer DS and handling Editor declared their shared affiliation.
Supplementary Material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fneur.2018.00352/full#supplementary-material.
References
- 1.Hain TC, Cherchi M, Yacovino DA. Bilateral vestibular loss. Semin Neurol (2013) 33(3):195–203. 10.1055/s-0033-1354597 [DOI] [PubMed] [Google Scholar]
- 2.Lucieer F, Vonk P, Guinand N, Stokroos R, Kingma H, van de Berg R. Bilateral vestibular hypofunction: insights in etiologies, clinical subtypes, and diagnostics. Front Neurol (2016) 7:26. 10.3389/fneur.2016.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strupp M, Kim JS, Murofushi T, Straumann D, Jen JC, Rosengren SM, et al. Bilateral vestibulopathy: diagnostic criteria consensus document of the classification committee of the Barany Society. J Vestib Res (2017) 27(4):177–89. 10.3233/VES-170619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van de Berg R, van Tilburg M, Kingma H. Bilateral vestibular hypofunction: challenges in establishing the diagnosis in adults. ORL J Otorhinolaryngol Relat Spec (2015) 77(4):197–218. 10.1159/000433549 [DOI] [PubMed] [Google Scholar]
- 5.Miffon M, Guyot JP. Difficulties faced by patients suffering from total bilateral vestibular loss. ORL J Otorhinolaryngol Relat Spec (2015) 77(4):241–7. 10.1159/000433553 [DOI] [PubMed] [Google Scholar]
- 6.Guinand N, Boselie F, Guyot JP, Kingma H. Quality of life of patients with bilateral vestibulopathy. Ann Otol Rhinol Laryngol (2012) 121(7):471–7. 10.1177/000348941212100708 [DOI] [PubMed] [Google Scholar]
- 7.Hanes DA, McCollum G. Cognitive-vestibular interactions: a review of patient difficulties and possible mechanisms. J Vestib Res (2006) 16(3):75–91. [PubMed] [Google Scholar]
- 8.McCall AA, Yates BJ. Compensation following bilateral vestibular damage. Front Neurol (2011) 2:88. 10.3389/fneur.2011.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gofrit SG, Mayler Y, Eliashar R, Bdolah-Abram T, Ilan O, Gross M. The association between vestibular physical examination, vertigo questionnaires, and the electronystagmography in patients with vestibular symptoms. Ann Otol Rhinol Laryngol (2017) 126(4):315–21. 10.1177/0003489417691298 [DOI] [PubMed] [Google Scholar]
- 10.Rothrock NE, Kaiser KA, Cella D. Developing a valid patient-reported outcome measure. Clin Pharmacol Ther (2011) 90(5):737–42. 10.1038/clpt.2011.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dawson J, Doll H, Fitzpatrick R, Jenkinson C, Carr AJ. The routine use of patient reported outcome measures in healthcare settings. BMJ (2010) 340:c186. 10.1136/bmj.c186 [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg (2010) 8(5):336–41. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 13.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) (2012) 22(3):276–82. 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Acierno MD, Trobe JD, Shepard NT, Cornblath WT, Disher MJ. Two types of oscillopsia in a patient with idiopathic vestibulopathy. J Neuroophthalmol (1997) 17(2):92–4. [PubMed] [Google Scholar]
- 15.Agrup C, Keir G, Thompson EJ, Bronstein AM. Systemic autoantibodies against discrete inner ear compartments in bilateral vestibular loss. Neurology (2005) 65(1):167. 10.1212/01.wnl.0000167609.12890.da [DOI] [PubMed] [Google Scholar]
- 16.Ahmed RM, Hannigan IP, MacDougall HG, Chan RC, Halmagyi GM. Gentamicin ototoxicity: a 23-year selected case series of 103 patients. Med J Aust (2012) 196(11):701–4. 10.5694/mja11.10850 [DOI] [PubMed] [Google Scholar]
- 17.Albernaz PL, Cusin FS. The video head impulse test in a case of suspected bilateral loss of vestibular function. Int Arch Otorhinolaryngol (2016) 20(1):84–6. 10.1055/s-0034-1395999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aran Yoo BS, Kattah JC. Superficial siderosis syndrome with progressive hearing loss and bilateral vestibular failure, 51 years after a neurosurgical procedure: diagnostic value of combined MRI and video head impulse test. J Neurol (2017) 264(2):391–3. 10.1007/s00415-016-8358-y [DOI] [PubMed] [Google Scholar]
- 19.Baloh RW, Enrietto J, Jacobson KM, Lin A. Age-related changes in vestibular function: a longitudinal study. Ann N Y Acad Sci (2001) 942:210–9. 10.1111/j.1749-6632.2001.tb03747.x [DOI] [PubMed] [Google Scholar]
- 20.Baloh RW, Honrubia V, Yee RD, Hess K. Changes in the human vestibulo-ocular reflex after loss of peripheral sensitivity. Ann Neurol (1984) 16(2):222–8. 10.1002/ana.410160209 [DOI] [PubMed] [Google Scholar]
- 21.Baloh RW, Jacobson K, Fife T. Familial vestibulopathy: a new dominantly inherited syndrome. Neurology (1994) 44(1):20–5. 10.1212/WNL.44.1.20 [DOI] [PubMed] [Google Scholar]
- 22.Baloh RW, Jacobson K, Honrubia V. Idiopathic bilateral vestibulopathy. Neurology (1989) 39(2 Pt 1):272–5. 10.1212/WNL.39.2.272 [DOI] [PubMed] [Google Scholar]
- 23.Baxter M, Agrawal Y. Vestibular dysfunction in Turner syndrome: a case report. Otol Neurotol (2014) 35(2):294–6. 10.1097/MAO.0b013e31829e16df [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brandt T, Schautzer F, Hamilton DA, Bruning R, Markowitsch HJ, Kalla R, et al. Vestibular loss causes hippocampal atrophy and impaired spatial memory in humans. Brain (2005) 128(Pt 11):2732–41. 10.1093/brain/awh617 [DOI] [PubMed] [Google Scholar]
- 25.Brantberg K, Lofqvist L. Preserved vestibular evoked myogenic potentials (VEMP) in some patients with walking-induced oscillopsia due to bilateral vestibulopathy. J Vestib Res (2007) 17(1):33–8. [PubMed] [Google Scholar]
- 26.Bringoux L, Schmerber S, Nougier V, Dumas G, Barraud PA, Raphel C. Perception of slow pitch and roll body tilts in bilateral labyrinthine-defective subjects. Neuropsychologia (2002) 40(4):367–72. 10.1016/S0028-3932(01)00103-8 [DOI] [PubMed] [Google Scholar]
- 27.Brown KE, Whitney SL, Wrisley DM, Furman JM. Physical therapy outcomes for persons with bilateral vestibular loss. Laryngoscope (2001) 111(10):1812–7. 10.1097/00005537-200110000-00027 [DOI] [PubMed] [Google Scholar]
- 28.Calder JH, Jacobson GP. Acquired bilateral peripheral vestibular system impairment: rehabilitative options and potential outcomes. J Am Acad Audiol (2000) 11(9):514–21. [PubMed] [Google Scholar]
- 29.Castellucci A, Piras G, Brandolini C, Modugno GC, Ferri GG. Waldenstrom’s macroglobulinemia presenting with bilateral vestibular loss: a case report. Braz J Otorhinolaryngol (2015) 81(5):571–5. 10.1016/j.bjorl.2015.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen PY, Hsieh WL, Wei SH, Kao CL. Interactive wiimote gaze stabilization exercise training system for patients with vestibular hypofunction. J Neuroeng Rehabil (2012) 9:77. 10.1186/1743-0003-9-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi SY, Kee HJ, Park JH, Kim HJ, Kim JS. Combined peripheral and central vestibulopathy. J Vestib Res (2014) 24(5–6):443–51. 10.3233/VES-140524 [DOI] [PubMed] [Google Scholar]
- 32.Choi SY, Kim HJ, Kim JS. Chasing dizzy chimera: diagnosis of combined peripheral and central vestibulopathy. J Neurol Sci (2016) 371:69–78. 10.1016/j.jns.2016.09.063 [DOI] [PubMed] [Google Scholar]
- 33.Constantinescu L, Schneider D, Claussen C. Vestibular evoked potentials in two patients with bilateral vestibular loss. Int Tinnitus J (1996) 2:45–57. [PubMed] [Google Scholar]
- 34.de Waele C, Shen Q, Magnani C, Curthoys IS. A novel saccadic strategy revealed by suppression head impulse testing of patients with bilateral vestibular loss. Front Neurol (2017) 8:419. 10.3389/fneur.2017.00419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deroualle D, Toupet M, van Nechel C, Duquesne U, Hautefort C, Lopez C. Anchoring the self to the body in bilateral vestibular failure. PLoS One (2017) 12(1):e0170488. 10.1371/journal.pone.0170488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Durrant JD, Furman JM. Long-latency rotational evoked potentials in subjects with and without bilateral vestibular loss. Electroencephalogr Clin Neurophysiol (1988) 71(4):251–6. 10.1016/0168-5597(88)90024-X [DOI] [PubMed] [Google Scholar]
- 37.Finn S, Dietzek M, Karvouniari P, Klingner CM, Neumann R, Guntinas-Lichius O, et al. Bilateral vestibulopathy with positive Tullio phenomenon. Laryngoscope (2017) 128(5):1223–5. 10.1002/lary.26690 [DOI] [PubMed] [Google Scholar]
- 38.Fujimoto C, Iwasaki S, Matsuzaki M, Murofushi T. Lesion site in idiopathic bilateral vestibulopathy: a galvanic vestibular-evoked myogenic potential study. Acta Otolaryngol (2005) 125(4):430–2. 10.1080/00016480410024668 [DOI] [PubMed] [Google Scholar]
- 39.Fujimoto C, Murofushi T, Chihara Y, Suzuki M, Yamasoba T, Iwasaki S. Novel subtype of idiopathic bilateral vestibulopathy: bilateral absence of vestibular evoked myogenic potentials in the presence of normal caloric responses. J Neurol (2009) 256(9):1488–92. 10.1007/s00415-009-5147-x [DOI] [PubMed] [Google Scholar]
- 40.Fujimoto C, Murofushi T, Sugasawa K, Chihara Y, Ushio M, Yamasoba T, et al. Bilateral vestibulopathy with dissociated deficits in the superior and inferior vestibular systems. Ann Otol Rhinol Laryngol (2012) 121(6):383–8. 10.1177/000348941212100604 [DOI] [PubMed] [Google Scholar]
- 41.Ghulyan-Bedikian V, Paolino M, Paolino F. Short-term retention effect of rehabilitation using head position-based electrotactile feedback to the tongue: influence of vestibular loss and old-age. Gait Posture (2013) 38(4):777–83. 10.1016/j.gaitpost.2013.03.018 [DOI] [PubMed] [Google Scholar]
- 42.Gill-Body KM, Beninato M, Krebs DE. Relationship among balance impairments, functional performance, and disability in people with peripheral vestibular hypofunction. Phys Ther (2000) 80(8):748–58. [PubMed] [Google Scholar]
- 43.Gillespie MB, Minor LB. Prognosis in bilateral vestibular hypofunction. Laryngoscope (1999) 109(1):35–41. 10.1097/00005537-199901000-00008 [DOI] [PubMed] [Google Scholar]
- 44.Grunfeld EA, Morland AB, Bronstein AM, Gresty MA. Adaptation to oscillopsia: a psychophysical and questionnaire investigation. Brain (2000) 123(Pt 2):277–90. 10.1093/brain/123.2.277 [DOI] [PubMed] [Google Scholar]
- 45.Herdman SJ, Blatt P, Schubert MC, Tusa RJ. Falls in patients with vestibular deficits. Am J Otol (2000) 21(6):847–51. [PubMed] [Google Scholar]
- 46.Hertel S, Schwaninger M, Helmchen C. Combined toxicity of penicillin and aspirin therapy may elicit bilateral vestibulopathy. Clin Neurol Neurosurg (2013) 115(7):1114–6. 10.1016/j.clineuro.2012.08.033 [DOI] [PubMed] [Google Scholar]
- 47.Hirvonen TP, Aalto H. Recovery of bilateral vestibular loss in Cogan’s syndrome – a case report. Otol Neurotol (2013) 34(9):1736–8. 10.1097/MAO.0b013e3182953154 [DOI] [PubMed] [Google Scholar]
- 48.Honrubia V, Marco J, Andrews J, Minser K, Yee RD, Baloh RW. Vestibulo-ocular reflexes in peripheral labyrinthine lesions: III. Bilateral dysfunction. Am J Otolaryngol (1985) 6(5):342–52. 10.1016/S0196-0709(85)80011-9 [DOI] [PubMed] [Google Scholar]
- 49.Hughes GB, Kinney SE, Hamid MA, Barna BP, Calabrese LH. Autoimmune vestibular dysfunction: preliminary report. Laryngoscope (1985) 95(8):893–7. 10.1288/00005537-198508000-00001 [DOI] [PubMed] [Google Scholar]
- 50.Ishiyama G, Ishiyama A, Kerber K, Baloh RW. Gentamicin ototoxicity: clinical features and the effect on the human vestibulo-ocular reflex. Acta Otolaryngol (2006) 126(10):1057–61. 10.1080/00016480600606673 [DOI] [PubMed] [Google Scholar]
- 51.Jahn K, Arbusow V, Zingler VC, Strupp M, Kretzschmar HA, Brandt T. Bilateral vestibular failure as an early sign in Creutzfeldt-Jakob disease. Ann N Y Acad Sci (2009) 1164:390–3. 10.1111/j.1749-6632.2008.03741.x [DOI] [PubMed] [Google Scholar]
- 52.Jandl NM, Sprenger A, Wojak JF, Gottlich M, Munte TF, Kramer UM, et al. Dissociable cerebellar activity during spatial navigation and visual memory in bilateral vestibular failure. Neuroscience (2015) 305:257–67. 10.1016/j.neuroscience.2015.07.089 [DOI] [PubMed] [Google Scholar]
- 53.Jansen NL, Feuerecker R, Becker-Bense S, Zwergal A, Wulff M, Xiong G, et al. Assessment of cerebral dopamine D 2/3 formula-receptors in patients with bilateral vestibular failure. J Vestib Res (2014) 24(5–6):403–13. 10.3233/VES-140526 [DOI] [PubMed] [Google Scholar]
- 54.Janssen M, Stokroos R, Aarts J, van Lummel R, Kingma H. Salient and placebo vibrotactile feedback are equally effective in reducing sway in bilateral vestibular loss patients. Gait Posture (2010) 31(2):213–7. 10.1016/j.gaitpost.2009.10.008 [DOI] [PubMed] [Google Scholar]
- 55.Jung I, Choi SY, Kim HJ, Kim JS. Delayed vestibulopathy after heat exposure. J Neurol (2017) 264(1):49–53. 10.1007/s00415-016-8322-x [DOI] [PubMed] [Google Scholar]
- 56.Kagoya R, Iwasaki S, Chihara Y, Ushio M, Tsuji S, Murofushi T, et al. Cephalic tetanus presenting as acute vertigo with bilateral vestibulopathy. Acta Otolaryngol (2011) 131(3):334–6. 10.3109/00016489.2010.526144 [DOI] [PubMed] [Google Scholar]
- 57.Kang KW, Lee C, Kim SH, Cho HH, Lee SH. Bilateral vestibulopathy documented by video head impulse tests in superficial siderosis. Otol Neurotol (2015) 36(10):1683–6. 10.1097/MAO.0000000000000865 [DOI] [PubMed] [Google Scholar]
- 58.Kapoula Z, Gaertner C, Yang Q, Denise P, Toupet M. Vergence and standing balance in subjects with idiopathic bilateral loss of vestibular function. PLoS One (2013) 8(6):e66652. 10.1371/journal.pone.0066652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim S, Oh YM, Koo JW, Kim JS. Bilateral vestibulopathy: clinical characteristics and diagnostic criteria. Otol Neurotol (2011) 32(5):812–7. 10.1097/MAO.0b013e31821a3b7d [DOI] [PubMed] [Google Scholar]
- 60.Lekhel H, Popov K, Bronstein A, Gresty M. Postural responses to vibration of neck muscles in patients with uni- and bilateral vestibular loss. Gait Posture (1998) 7(3):228–36. 10.1016/S0966-6362(98)00012-5 [DOI] [PubMed] [Google Scholar]
- 61.Lempert T, Gianna CC, Gresty MA, Bronstein AM. Effect of otolith dysfunction. Impairment of visual acuity during linear head motion in labyrinthine defective subjects. Brain (1997) 120(Pt 6):1005–13. 10.1093/brain/120.6.1005 [DOI] [PubMed] [Google Scholar]
- 62.MacDougall HG, Moore ST, Black RA, Jolly N, Curthoys IS. On-road assessment of driving performance in bilateral vestibular-deficient patients. Ann N Y Acad Sci (2009) 1164:413–8. 10.1111/j.1749-6632.2008.03733.x [DOI] [PubMed] [Google Scholar]
- 63.Martin T, Moussay S, Bulla I, Bulla J, Toupet M, Etard O, et al. Exploration of circadian rhythms in patients with bilateral vestibular loss. PLoS One (2016) 11(6):e0155067. 10.1371/journal.pone.0155067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matsuzaki M, Murofushi T. Vestibular evoked myogenic potentials in patients with idiopathic bilateral vestibulopathy. Report of three cases. ORL J Otorhinolaryngol Relat Spec (2001) 63(6):349–52. 10.1159/000055772 [DOI] [PubMed] [Google Scholar]
- 65.Minor LB. Gentamicin-induced bilateral vestibular hypofunction. JAMA (1998) 279(7):541–4. 10.1001/jama.279.7.541 [DOI] [PubMed] [Google Scholar]
- 66.Moon M, Chang SO, Kim MB. Diverse clinical and laboratory manifestations of bilateral vestibulopathy. Laryngoscope (2017) 127(1):E42–9. 10.1002/lary.25946 [DOI] [PubMed] [Google Scholar]
- 67.Nuti D, Passero S, Di Girolamo S. Bilateral vestibular loss in vertebrobasilar dolichoectasia. J Vestib Res (1996) 6(2):85–91. 10.1016/0957-4271(95)02010-1 [DOI] [PubMed] [Google Scholar]
- 68.Pollak L, Milo R, Kossych V, Rabey MJ, Shapira E. Bilateral vestibular failure as a unique presenting sign in carcinomatous meningitis: case report. J Neurol Neurosurg Psychiatry (2001) 70(5):704–5. 10.1136/jnnp.70.5.704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rinne T, Bronstein AM, Rudge P, Gresty MA, Luxon LM. Bilateral loss of vestibular function: clinical findings in 53 patients. J Neurol (1998) 245(6–7):314–21. 10.1007/s004150050225 [DOI] [PubMed] [Google Scholar]
- 70.Robinson BS, Cook JL, Richburg CM, Price SE. Use of an electrotactile vestibular substitution system to facilitate balance and gait of an individual with gentamicin-induced bilateral vestibular hypofunction and bilateral transtibial amputation. J Neurol Phys Ther (2009) 33(3):150–9. 10.1097/NPT.0b013e3181a79373 [DOI] [PubMed] [Google Scholar]
- 71.Ruehl RM, Guerkov R. Amiodarone-induced gait unsteadiness is revealed to be bilateral vestibulopathy. Eur J Neurol (2017) 24(2):e7–8. 10.1111/ene.13203 [DOI] [PubMed] [Google Scholar]
- 72.Rust H, Peters N, Allum JHJ, Wagner B, Honegger F, Baumann T. VEMPs in a patient with cerebellar ataxia, neuropathy and vestibular areflexia (CANVAS). J Neurol Sci (2017) 378:9–11. 10.1016/j.jns.2017.04.029 [DOI] [PubMed] [Google Scholar]
- 73.Sargent EW, Goebel JA, Hanson JM, Beck DL. Idiopathic bilateral vestibular loss. Otolaryngol Head Neck Surg (1997) 116(2):157–62. 10.1016/S0194-5998(97)70318-8 [DOI] [PubMed] [Google Scholar]
- 74.Schautzer F, Hamilton D, Kalla R, Strupp M, Brandt T. Spatial memory deficits in patients with chronic bilateral vestibular failure. Ann N Y Acad Sci (2003) 1004:316–24. 10.1196/annals.1303.029 [DOI] [PubMed] [Google Scholar]
- 75.Schlick C, Schniepp R, Loidl V, Wuehr M, Hesselbarth K, Jahn K. Falls and fear of falling in vertigo and balance disorders: a controlled cross-sectional study. J Vestib Res (2016) 25(5–6):241–51. 10.3233/VES-150564 [DOI] [PubMed] [Google Scholar]
- 76.Schniepp R, Schlick C, Schenkel F, Pradhan C, Jahn K, Brandt T, et al. Clinical and neurophysiological risk factors for falls in patients with bilateral vestibulopathy. J Neurol (2017) 264(2):277–83. 10.1007/s00415-016-8342-6 [DOI] [PubMed] [Google Scholar]
- 77.Schuler O, Strupp M, Arbusow V, Brandt T. A case of possible autoimmune bilateral vestibulopathy treated with steroids. J Neurol Neurosurg Psychiatry (2003) 74(6):825. 10.1136/jnnp.74.6.825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Smith JH, Stovall KC, Coons S, Fife TD. Bilateral vestibular hypofunction in neurosarcoidosis: a case report. Ear Nose Throat J (2011) 90(1):E1–3. [DOI] [PubMed] [Google Scholar]
- 79.Spiegel R, Kalla R, Classen J, Bardins S, Anciaes da Silva F, Farahmand P, et al. Aminopyridine treatment in a patient with bilateral vestibular failure and cryptogenic downbeat nystagmus. J Neuroophthalmol (2012) 32(2):190. 10.1097/WNO.0b013e31824f397f [DOI] [PubMed] [Google Scholar]
- 80.Strupp M, Jahn K, Brandt T. Another adverse effect of aspirin: bilateral vestibulopathy. J Neurol Neurosurg Psychiatry (2003) 74(5):691. 10.1136/jnnp.74.5.691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Suarez H, Sotta G, San Roman C, Arocena S, Ferreira E, Geisinger D, et al. Postural response characterization in elderly patients with bilateral vestibular hypofunction. Acta Otolaryngol (2013) 133(4):361–7. 10.3109/00016489.2012.739731 [DOI] [PubMed] [Google Scholar]
- 82.Swanenburg J, Zurbrugg A, Straumann D, Hegemann SCA, Palla A, de Bruin ED. A pilot study investigating the association between chronic bilateral vestibulopathy and components of a clinical functional assessment tool. Physiother Theory Pract (2017) 33(6):454–61. 10.1080/09593985.2017.1323362 [DOI] [PubMed] [Google Scholar]
- 83.Szmulewicz DJ, Waterston JA, Halmagyi GM, Mossman S, Chancellor AM, McLean CA, et al. Sensory neuropathy as part of the cerebellar ataxia neuropathy vestibular areflexia syndrome. Neurology (2011) 76(22):1903–10. 10.1212/WNL.0b013e31821d746e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tang L, Schubert M, Marlowe A, Weinreich H. Bilateral hearing and vestibular loss in a patient with untreated chronic myeloid leukemia. JAMA Otolaryngol Head Neck Surg (2017) 143(7):736–7. 10.1001/jamaoto.2017.0283 [DOI] [PubMed] [Google Scholar]
- 85.Tuo KS, Cheng YY, Kao CL. Vestibular rehabilitation in a patient with whiplash-associated disorders. J Chin Med Assoc (2006) 69(12):591–5. 10.1016/S1726-4901(09)70336-3 [DOI] [PubMed] [Google Scholar]
- 86.van de Berg R, Guinand N, Guyot JP, Kingma H, Stokroos RJ. The modified ampullar approach for vestibular implant surgery: feasibility and its first application in a human with a long-term vestibular loss. Front Neurol (2012) 3:18. 10.3389/fneur.2012.00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.van Kerckhoven G, Mert A, De Ru JA. Treatment of vertigo and postural instability using visual illusions. J Laryngol Otol (2014) 128(11):1005–7. 10.1017/S0022215114002254 [DOI] [PubMed] [Google Scholar]
- 88.van Leeuwen RB, Smits BW, Rodenburg RJ, van Engelen BG. Bilateral vestibulopathy aggravates balance and gait disturbances in sensory ataxic neuropathy, dysarthria, and ophthalmoparesis: a case report. J Clin Neuromuscul Dis (2016) 18(1):34–6. 10.1097/CND.0000000000000126 [DOI] [PubMed] [Google Scholar]
- 89.van Leeuwen RB, van Kooten B, de Cock AF. Bilateral vestibular hypofunction and Lyme disease: a causal link? Acta Neurol Belg (2017) 117(1):367–8. 10.1007/s13760-016-0658-6 [DOI] [PubMed] [Google Scholar]
- 90.Ward BK, Agrawal Y, Hoffman HJ, Carey JP, Della Santina CC. Prevalence and impact of bilateral vestibular hypofunction: results from the 2008 US National Health Interview Survey. JAMA Otolaryngol Head Neck Surg (2013) 139(8):803–10. 10.1001/jamaoto.2013.3913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wenzel A, Ward BK, Schubert MC, Kheradmand A, Zee DS, Mantokoudis G, et al. Patients with vestibular loss, Tullio phenomenon, and pressure-induced nystagmus: vestibular atelectasis? Otol Neurotol (2014) 35(5):866–72. 10.1097/MAO.0000000000000366 [DOI] [PubMed] [Google Scholar]
- 92.Wester JL, Ishiyama A, Ishiyama G. Recurrent vestibular migraine vertigo attacks associated with the development of profound bilateral vestibulopathy: a case series. Otol Neurotol (2017) 38(8):1145–8. 10.1097/MAO.0000000000001486 [DOI] [PubMed] [Google Scholar]
- 93.Wiest G, Demer JL, Tian J, Crane BT, Baloh RW. Vestibular function in severe bilateral vestibulopathy. J Neurol Neurosurg Psychiatry (2001) 71(1):53–7. 10.1136/jnnp.71.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wong RS, Abdul Kadir SY. An unusual case of bilateral vestibulopathy, chronic subjective dizziness and spondyloarthropathy. Gen Hosp Psychiatry (2015) 37(4):372.e3–4. 10.1016/j.genhosppsych.2015.03.011 [DOI] [PubMed] [Google Scholar]
- 95.Yetiser S. Bilateral cochleovestibulopathy due to internal auditory canal metastasis in a patient with stomach cancer. J Int Adv Otol (2016) 12(3):353–5. 10.5152/iao.2016.2762 [DOI] [PubMed] [Google Scholar]
- 96.Yukawa K, Hagiwara A, Ogawa Y, Nishiyama N, Shimizu S, Kawaguchi S, et al. Bilateral progressive hearing loss and vestibular dysfunction with inner ear antibodies. Auris Nasus Larynx (2010) 37(2):223–8. 10.1016/j.anl.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 97.Zingler VC, Cnyrim C, Jahn K, Weintz E, Fernbacher J, Frenzel C, et al. Causative factors and epidemiology of bilateral vestibulopathy in 255 patients. Ann Neurol (2007) 61(6):524–32. 10.1002/ana.21105 [DOI] [PubMed] [Google Scholar]
- 98.Zingler VC, Weintz E, Jahn K, Huppert D, Cnyrim C, Brandt T, et al. Causative factors, epidemiology, and follow-up of bilateral vestibulopathy. Ann N Y Acad Sci (2009) 1164:505–8. 10.1111/j.1749-6632.2009.03765.x [DOI] [PubMed] [Google Scholar]
- 99.Zingler VC, Weintz E, Jahn K, Mike A, Huppert D, Rettinger N, et al. Follow-up of vestibular function in bilateral vestibulopathy. J Neurol Neurosurg Psychiatry (2008) 79(3):284–8. 10.1136/jnnp.2007.122952 [DOI] [PubMed] [Google Scholar]
- 100.Rybak LP, Whitworth CA. Ototoxicity: therapeutic opportunities. Drug Discov Today (2005) 10(19):1313–21. 10.1016/S1359-6446(05)03552-X [DOI] [PubMed] [Google Scholar]
- 101.Cruickshanks KJ, Tweed TS, Wiley TL, Klein BE, Klein R, Chappell R, et al. The 5-year incidence and progression of hearing loss: the epidemiology of hearing loss study. Arch Otolaryngol Head Neck Surg (2003) 129(10):1041–6. 10.1001/archotol.129.10.1041 [DOI] [PubMed] [Google Scholar]
- 102.Balaban CD. Projections from the parabrachial nucleus to the vestibular nuclei: potential substrates for autonomic and limbic influences on vestibular responses. Brain Res (2004) 996(1):126–37. 10.1016/j.brainres.2003.10.026 [DOI] [PubMed] [Google Scholar]
- 103.Highstein SM, Holstein GR. The anatomical and physiological framework for vestibular prostheses. Anat Rec (Hoboken) (2012) 295(11):2000–9. 10.1002/ar.22582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Holstein GR, Friedrich VL, Jr, Kang T, Kukielka E, Martinelli GP. Direct projections from the caudal vestibular nuclei to the ventrolateral medulla in the rat. Neuroscience (2011) 175:104–17. 10.1016/j.neuroscience.2010.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grill E, Strupp M, Muller M, Jahn K. Health services utilization of patients with vertigo in primary care: a retrospective cohort study. J Neurol (2014) 261(8):1492–8. 10.1007/s00415-014-7367-y [DOI] [PubMed] [Google Scholar]
- 106.Sun DQ, Ward BK, Semenov YR, Carey JP, Della Santina CC. Bilateral vestibular deficiency: quality of life and economic implications. JAMA Otolaryngol Head Neck Surg (2014) 140(6):527–34. 10.1001/jamaoto.2014.490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cutfield NJ, Scott G, Waldman AD, Sharp DJ, Bronstein AM. Visual and proprioceptive interaction in patients with bilateral vestibular loss. Neuroimage Clin (2014) 4:274–82. 10.1016/j.nicl.2013.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Guerraz M, Yardley L, Bertholon P, Pollak L, Rudge P, Gresty MA, et al. Visual vertigo: symptom assessment, spatial orientation and postural control. Brain (2001) 124(Pt 8):1646–56. 10.1093/brain/124.8.1646 [DOI] [PubMed] [Google Scholar]
- 109.Jacobson GP, Newman CW. The development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg (1990) 116(4):424–7. 10.1001/archotol.1990.01870040046011 [DOI] [PubMed] [Google Scholar]
- 110.Cohen HS, Kimball KT. Development of the vestibular disorders activities of daily living scale. Arch Otolaryngol Head Neck Surg (2000) 126(7):881–7. 10.1001/archotol.126.7.881 [DOI] [PubMed] [Google Scholar]
- 111.Newman-Toker DE, Edlow JA. TiTrATE: a novel, evidence-based approach to diagnosing acute dizziness and vertigo. Neurol Clin (2015) 33(3):577–99, viii. 10.1016/j.ncl.2015.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.