Abstract
A poor soft tissue envelope often accompanies periprosthetic tibia fracture around a well-fixed total knee arthroplasty and the tibial stem leaves little room for screw fixation. This article describes the practicability and effectiveness of a novel surgical technique using circular hexapod external fixation, in patients with this clinical scenario. It was applied for fixation of periprosthetic tibia fracture in 2 patients. Contact between the external fixation pins and the prosthesis was avoided. Using a web-based software program, a gradual reduction in all planes was achieved. Adequate fixation, stability, reduction, and quick healing were obtained in the 2 cases, with minimal complications. The patients returned to their activity level a few months after external fixation removal.
Keywords: Periprosthetic fracture, Arthroplasty, Gradual correction, External fixation, Taylor spatial frame, Total knee arthroplasty
Introduction
The incidence of periprosthetic fractures following total knee arthroplasty (TKA) is up to 5.5% and is continuously rising because of an increasing number of knee joint replacements [1]. This results in an increase in revision arthroplasty number and further risk of fracture from periprosthetic bone loss [2]. A series of over 17,000 TKAs reported by the Mayo Clinic Joint Registry published in 1999 indicated that postoperative tibia fractures occurred in 0.4% of the cases after primary TKA [3].
Felix et al classified periprosthetic tibial fractures into 4 types based on the anatomic location and proximity to the prosthesis as well as the status of the prosthetic fixation (Table 1) [4].
Table 1.
Felix classification for periprosthetic tibial fracture.
| Type I | Fracture of the tibial plateau with involvement of the prosthesis-implant interface |
| Type II | Fracture of the meta-diaphyseal transition |
| Type III | Fracture distal to the tibial component |
| Type IV | Fracture of the tibial tuberosity |
| Subtype A | Stable prosthesis |
| Subtype B | Loose prosthesis |
| Subtype C | Intraoperative fracture |
Open reduction and internal fixation (ORIF) is mainly indicated for displaced periprosthetic proximal tibia fractures associated with a well-fixed component. However, plate and screw construct rigidity is limited by the available space between the tibial stem and surrounding bone to pass bicortical screws, which can lead to insufficient fixation and the need for adjunctive fixation [5]. Although proximal tibial locked plating constructs are favored especially in osteopenic bone, these devices have little flexibility for screw placement and trajectory. Multiple incisions also increase the risk of skin necrosis and deep infection [5].
To the best of our knowledge, the use of circular hexapod external fixation (CHEF) to treat periprosthetic tibial fractures has not been reported in the English literature. This method was adopted to overcome the difficulties and complications associated with the more common ORIF treatment.
Surgical technique
After obtaining proper consent and confirmation of the surgical site, the patient undergoes neuraxial or general anesthesia. A fluoroscopy machine is positioned on the contralateral side of the table and used throughout the case to guide external fixation pins positioning. Usual skin disinfection and draping of the limb is performed. The fracture is fixed with CHEF using a 2-ring construct, positioned orthogonal to the desired mechanical axis of both the proximal and distal segments; the proximal ring is fixed using multiple wires and 1 or 2 hydroxyapatite half-pins as dictated by fragment size and bone quality, taking great care to avoid contact with the prosthetic components (Fig. 1). The distal ring is fixed with 3 multiplanar half-pins. The fragments are manually reduced intraoperatively, fixed with 6 telescopic struts, and residual correction (Fig. 2) can be done postoperatively to achieve desired alignment using the CHEF software. Postoperative long bilateral legs standing radiographs are obtained to assess mechanical alignment.
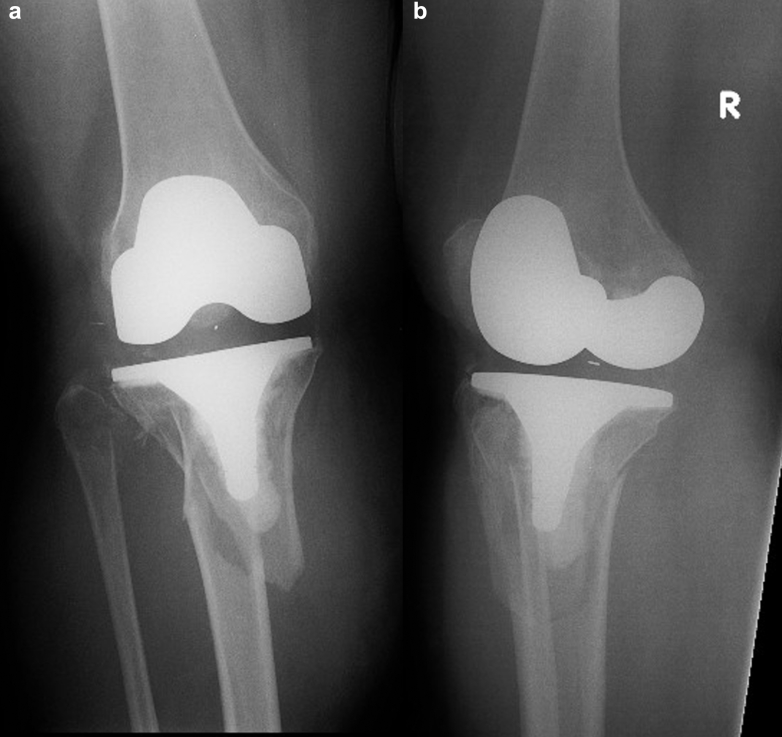
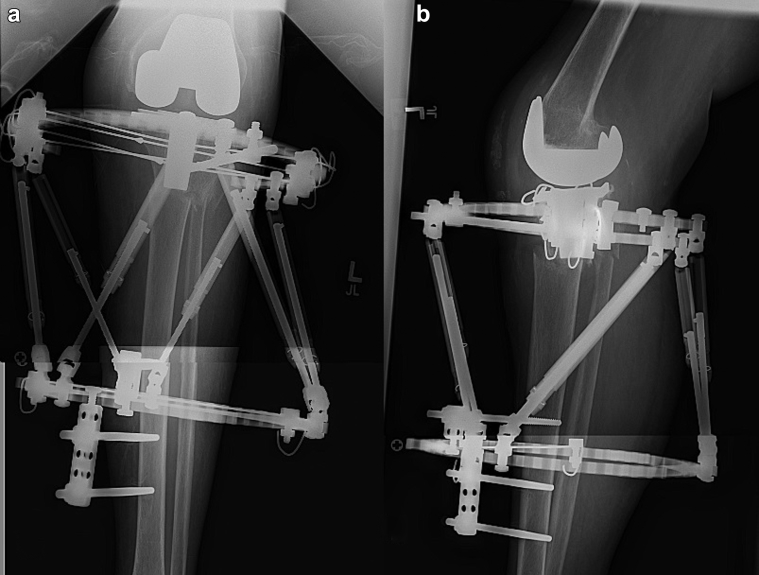
Figure 1.
Intra-operative antero-posterior (a) view of the proximal tibia showing clearance between the 6 mm half-pin and the prosthesis. Lateral view (b) showing clearance of the Ilizarov wire.
Figure 2.
Anterior posterior (a), lateral (b) radiographic views and clinical picture (c) of the knee after surgery. If imperfect reduction is obtained during surgery, gradual correction can be achieved through the web-based program.
Range of motion exercises of the knee are started from the first postoperative day. The patient is allowed progressive weight bearing as tolerated. Deep venous thrombosis prophylaxis is ordered for 4 weeks after surgery. The fixator is removed when full radiological consolidation is observed.
Case 1
A 48-year-old female with past medical history of seronegative rheumatoid arthritis and osteoporosis sustained a right periprosthetic Felix type 2A tibial fracture following a road accident as a pedestrian (Fig. 3). She had undergone a right TKA 3.5 years earlier. She denied any history of knee pain prior to the accident and there was no radiological sign of aseptic loosening of the tibia component. Because of her poor bone quality as well as the small size of the proximal fragment, it was judged that an ORIF would yield poor fixation. CHEF was elected as a method of choice to obtain rigid fixation and provide accurate reduction.
Figure 3.
Case 1: Anterior posterior (a) and tentative lateral (b) radiographic views of the fracture on the day of injury.
The fixator was removed after 13 weeks and there were no pin tract infections during treatment. At follow-up 18 months after injury, the patient was mobilizing independently, with a knee range of motion of 0°-120° and has resumed her prefracture level of activity (Fig. 4). The latest radiographs show good fracture healing with 5° of “procurvatum” in comparison to the left normal side (Fig. 5).
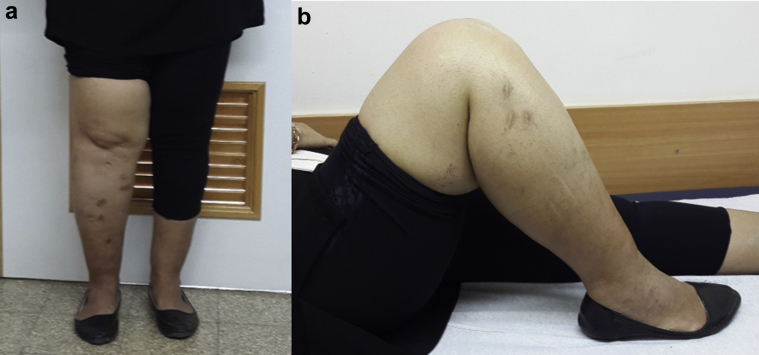
Figure 4.
Case 1: Front (a) and lateral (b) clinical pictures of the knee at 18 months after surgery.
Figure 5.
Case 1: Anterior posterior (a) and lateral (b) radiographic views of the fracture at 18 months after surgery.
Case 2
A 78-year-old woman with past medical history of post-traumatic left knee osteoarthritis and patellectomy sustained a left closed periprosthetic proximal tibia and fibula fracture around a well-fixed TKA implant from a fall from her height (Fig. 6). Her soft tissue envelope as well as poor bone stock did not make her a good candidate for ORIF (Fig. 7). She was treated with CHEF and gradual reduction of the fracture (Fig. 8). Intentional “recurvatum” was built in the correction to allow locking of the knee in full extension, for a functional position as she had a flexed femoral component. This is explained by a previous supracondylar femoral fracture healed in flexion, as noted by the medial meta-diaphyseal callus overlying the cortical border (Fig. 9). Weight bearing as tolerated was allowed while she was in the frame. The external fixator was removed 5 months later after radiologic confirmation of complete fracture healing. Within 2 weeks she progressed to full weight bearing. At 10-week follow-up, she had obtained a stable range of motion from 0° to 90°. At 7-month follow-up, she was ambulating with a walker and a drop lock hinged knee brace for her long-standing quadriceps insufficiency. One instance of superficial pin tract infection was noted 1 week prior to frame removal and was treated with a course of oral doxycycline and wire removal.
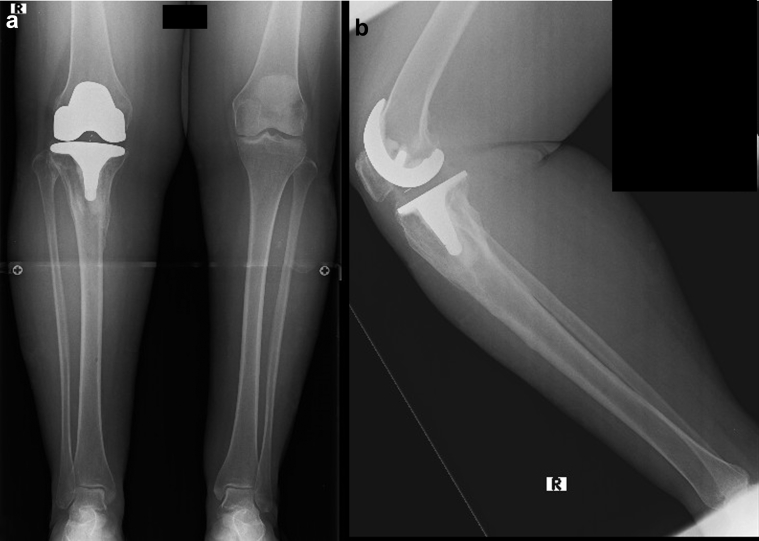
Figure 6.
Case 2: Anterior posterior (a) and lateral (b) radiographic views of the fracture on the day of injury.
Figure 7.
Case 2: Extension (a) and flexion (b) clinical pictures of the knee during treatment, depicting poor soft tissue envelope around the fracture site.
Figure 8.
Case 2: Anterior posterior (a) and lateral (b) views after surgery.
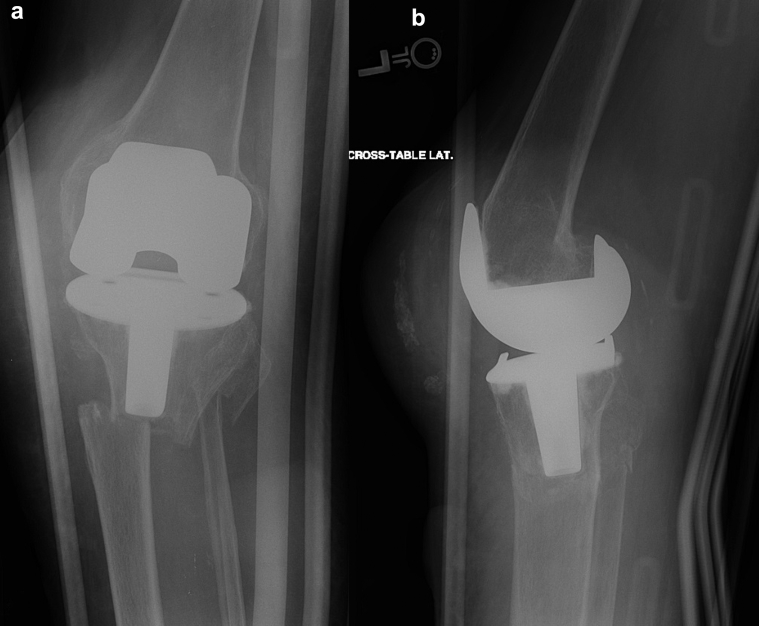
Figure 9.
Case 2: Anterior posterior (a) and lateral (b) views after gradual correction and fixator removal. The proximal tibia was intentionally left in recurvatum (b) to accommodate the flexed femoral component and obtain full extension of the knee.
Discussion
There is no clear treatment protocol for the management of displaced periprosthetic tibial fractures. Operative reduction and stabilization is indicated for displaced periprosthetic proximal tibia fractures associated with a well-fixed component for all types of Felix classification. However, obtaining adequate fixation during ORIF with a plate and screws of a periprosthetic proximal tibia fracture can be a challenge. Ruchholtz et al concluded that, with respect to periprosthetic fractures around the knee, compromised bone quality has been observed which may be due to patient age. Achievement of stable fixation and successful rehabilitation can be difficult, contributing to the incidence of greater delayed union and nonunion. The risk of soft tissue complications, including deep infection, is much higher in the tibia than in the distal femur [6].
Plate and screw constructs are limited by the available bone around the tibial stem proximally to pass bicortical screws. Modern locked plating constructs have even less flexibility in screw placement than older nonlocking designs. The inability to pass multiple screws across the proximal fragment leading to insufficient fixation may call for adjunctive fixation with unicortical locked screws, cables, secondary posterior-medial plates, or some combination thereof, all of which further compromise the blood supply of the bone. Since this scenario is common, the surgeon may be left with marginal fixation in the proximal fragment afforded by a lateral plate and screw construct. Dual plating of these fractures is often required to obtain adequate fracture stability. A medial plate usually adds sufficient stability even when a limited number of proximal fixation points are obtained [5]. However, maintaining adequate skin bridges between the medial and lateral incisions used for ORIF and any anterior incision pre-existing from the knee arthroplasty is fraught with possible danger. The medial incision must be placed sufficiently posterior to minimize the risk of skin necrosis while still allowing adequate exposure for posterior-medial plating [7].
For displaced subtype A fractures, most authors use locked plates because of the inability to obtain proximal bicortical fixation [1], [5], [6], [8], [9]. In a systematic review by Ebraheim et al [10] of periprosthetic tibia fracture after TKA, a database search yielded 13 reports that fit their inclusion criteria. Only 15 of 154 fractures were type 2, and all subclass A were treated with locking plates.
However, there are reports of significant complication rates in using the locked plates. Platzer et al [2] found reduction or fixation failures in 8 of 38 (21%) patients managed with locking plates. Reoperation in 3 patients was also necessary. Ebraheim et al found that 37% of 27 patients with periprosthetic femur fractures adjacent to their TKA treated with locking plate ORIF experienced complications: failure of fixation in 7, delayed union in 2, and nonunion in 1 [11].
In order to avoid the complications related to the treatment modalities mentioned above, another option is the use of CHEF [12]. The system works on the foundation of the theory of projected geometry and the mechanical basis of the Stewart-Gough platform. The fixator allows simultaneous correction of multiplanar deformities. Six deformity parameters may be corrected gradually and simultaneously—both angulation and translation in the coronal, sagittal, and axial planes. The minimally invasive nature of circular fixation, using wires and half-pins to achieve stable fixation in even narrow segments of bone, makes this method particularly suited to the treatment of difficult fracture configurations and those with overlying soft tissue problems [13], [14]. The ability to gradually correct the deformity allows the surgeon to apply fixation percutaneously and avoid opening the fracture site. Acute closed reduction is performed in the operating room and any residual deformity and displacement is corrected with a gradual correction using the CHEF over the next several days.
Only 2 case reports have been described in the literature, successfully using an external fixator to treat periprosthetic fractures following total knee replacement. However, they relate to fractures around the femoral component, using the Ilizarov circular external fixator, fixing the fracture with wires only. In one case, in an attempt to stay away from the total knee components and minimize the possibility of seeding the prosthesis, no implants were placed directly into the distal femoral fracture fragments themselves. The frame was constructed to span the knee joint, held in full extension [15]. In the other case report, the frame was placed entirely above the knee, thus allowing a full range of knee movement during the healing process. The distal pins were placed slightly proximal to the femoral prosthesis [16].
The most worrisome complication in the presented technique is pin-track infection which could lead to deep infection. To protect against this, we have adopted the technique of wire or half-pins insertion around an internal implant, as described by many authors when using external and internal fixation [3], [6], [17], [18], [19], [20], [21], [22], [23]. We are meticulous about avoiding any contact between the external fixator pins and the internal implant. In the series of 13 tibias lengthened over an intramedullary nail by Bilen et al, none of their patients developed an intramedullary infection related to the Schanz screws. These authors were also careful to ensure that there was no contact between the nail and the external fixation pins [11]. In a study by Guo et al, 51 tibia lengthening procedures over an intramedullary nail were performed, using the Ilizarov external fixator. No deep intramedullary infection occurred in any tibia [18]. In another study, Motallebi Zadeh et al included 143 patients who underwent bilateral tibia lengthening over an intramedullary nail. No deep infection occurred in any patient; however, superficial skin pin tract infection was seen in 65 (45.7%) individuals, all of whom responded to oral antibiotics [21]. In the study by Kim et al [19], none of the 5 patients with post-traumatic mal-union and axial frame deformity, who underwent lengthening of the femurs over an existing intramedullary nail, suffered from deep infection.
Finally, it is important to mention that experience with circular external fixation, fracture care, and deformity correction is necessary to employ this technique. Both cases presented in this article were treated by surgeons whose practice is focused primarily on deformity correction using both internal and external fixation.
Summary
Circular external fixation and gradual correction of a periprosthetic fracture around a well-fixed tibia component is an important option in patients with poor bone stock and compromised soft tissue envelope. Avoiding contact between wires and the implant is critically important to reduce the risk of deep infection. This technique should preferably be used by a surgeon comfortable with the principles of deformity correction with CHEF.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2017.03.001.
Appendix A. Supplementary data
References
- 1.Kim K.I., Egol K.A., Hozack W.J., Parvizi J. Periprosthetic fractures after total knee arthroplasties. Clin Orthop Relat Res. 2006;446:167. doi: 10.1097/01.blo.0000214417.29335.19. [DOI] [PubMed] [Google Scholar]
- 2.Platzer P., Schuster R., Aldrian S. Management and outcome of periprosthetic fractures after total knee arthroplasty. J Trauma. 2010;68:1464. doi: 10.1097/TA.0b013e3181d53f81. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein M., Fragomen A.T., Sabharwal S., Barclay J., Rozbruch S.R. Does integrated fixation provide benefit in the reconstruction of posttraumatic tibial bone defects? Clin Orthop Relat Res. 2015;473(10):3143. doi: 10.1007/s11999-015-4326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felix N.A., Stuart M.J., Hanssen A.D. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997:113. [PubMed] [Google Scholar]
- 5.Ricci W.M. Periprosthetic fractures. In: Court-Brown C.M., Heckman J.D., McQueen M.M., Ricci W.M., editors. 8th ed. Vol. 1. Wolters Kluwer Health; 2014. p. 681. (Rockwood and Green's fractures in adults). [Google Scholar]
- 6.Rozbruch S.R., Kleinman D., Fragomen A.T., Ilizarov S. Limb lengthening and then insertion of an intramedullary nail: a case-matched comparison. Clin Orthop Relat Res. 2008;466:2923. doi: 10.1007/s11999-008-0509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebraheim N.A., Liu J., Hashmi S.Z. High complication rate in locking plate fixation of lower periprosthetic distal femur fractures in patients with total knee arthroplasties. J Arthroplasty. 2012;27:809. doi: 10.1016/j.arth.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Sala F., Elbatrawy Y., Thabet A.M., Zayed M., Capitani D. Taylor spatial frame fixation in patients with multiple traumatic injuries: study of 57 long-bone fractures. J Orthop Trauma. 2013;27:442. doi: 10.1097/BOT.0b013e31827cda11. [DOI] [PubMed] [Google Scholar]
- 9.Taylor J. Six-axis deformity analysis and correction. In: Paley D., editor. Principles of deformity correction. Springer; Berlin; New York: 2002. p. 411. [Google Scholar]
- 10.Ebraheim N.A., Ray J.R., Wandtke M.E. Systematic review of periprosthetic tibia fracture after total knee arthroplasties. World J Orthop. 2015;6:649. doi: 10.5312/wjo.v6.i8.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bilen F.E., Kocaoglu M., Eralp L., Balci H.I. Fixator-assisted nailing and consecutive lengthening over an intramedullary nail for the correction of tibial deformity. J Bone Joint Surg Br. 2010;92:146. doi: 10.1302/0301-620X.92B1.22637. [DOI] [PubMed] [Google Scholar]
- 12.Simpson A.H., Cole A.S., Kenwright J. Leg lengthening over an intramedullary nail. J Bone Joint Surg Br. 1999;81:1041. doi: 10.1302/0301-620x.81b6.9359. [DOI] [PubMed] [Google Scholar]
- 13.Henderson D.J., Barron E., Hadland Y., Sharma H.K. Functional outcomes after tibial shaft fractures treated using the Taylor spatial frame. J Orthop Trauma. 2015;29:e54. doi: 10.1097/BOT.0000000000000192. [DOI] [PubMed] [Google Scholar]
- 14.Ruchholtz S., Tomas J., Gebhard F., Larsen M.S. Periprosthetic fractures around the knee—the best way of treatment. Eur Orthop Traumatol. 2013;4:93. doi: 10.1007/s12570-012-0130-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarmah S.S., Patel S., Reading G. Periprosthetic fractures around total knee arthroplasty. Ann R Coll Surg Engl. 2012;94:302. doi: 10.1308/10.1308/003588412X13171221592537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hurson C., Synnott K., McCormack D. Above-knee Ilizarov external fixation for early periprosthetic supracondylar femoral fracture—a case report. Knee. 2005;12:145. doi: 10.1016/j.knee.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Berry D.J. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30:183. doi: 10.1016/s0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 18.Guo Q., Zhang T., Zheng Y. Tibial lengthening over an intramedullary nail in patients with short stature or leg-length discrepancy: a comparative study. Int Orthop. 2012;36:179. doi: 10.1007/s00264-011-1246-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim H.J., Fragomen A.T., Reinhardt K., Hutson J.J., Jr., Rozbruch S.R. Lengthening of the femur over an existing intramedullary nail. J Orthop Trauma. 2011;25:681. doi: 10.1097/BOT.0b013e3181f92d6e. [DOI] [PubMed] [Google Scholar]
- 20.Mahboubian S., Seah M., Fragomen A.T., Rozbruch S.R. Femoral lengthening with lengthening over a nail has fewer complications than intramedullary skeletal kinetic distraction. Clin Orthop Relat Res. 2012;470:1221. doi: 10.1007/s11999-011-2204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Motallebi Zadeh N., Mortazavi S.H., Khaki S. Bilateral tibial lengthening over the nail: our experience of 143 cases. Arch Orthop Trauma Surg. 2014;134:1219. doi: 10.1007/s00402-014-2069-6. [DOI] [PubMed] [Google Scholar]
- 22.Paley D., Herzenberg J.E., Paremain G., Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Simon R.G., Brinker M.R. Use of Ilizarov external fixation for a periprosthetic supracondylar femur fracture. J Arthroplasty. 1999;14:118. doi: 10.1016/s0883-5403(99)90214-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.