Abstract
The use of larger femoral head size in total hip arthroplasty (THA) has increased during the past decade; 32 mm and 36 mm are the most commonly used femoral head sizes, as reported by several arthroplasty registries.
The use of large femoral heads seems to be a trade-off between increased stability and decreased THA survivorship.
We reviewed the literature, mainly focussing on the past 5 years, identifying benefits and complications associated with the trend of using larger femoral heads in THA.
We found that there is no benefit in hip range of movement or hip function when head sizes > 36 mm are used.
The risk of revision due to dislocation is lower for 36 mm or larger bearings compared with 28 mm or smaller and probably even with 32 mm.
Volumetric wear and frictional torque are increased in bearings bigger than 32 mm compared with 32 mm or smaller in metal-on-cross-linked polyethylene (MoXLPE) THA, but not in ceramic-on-XLPE (CoXLPE).
Long-term THA survivorship is improved for 32 mm MoXLPE bearings compared with both larger and smaller ones.
We recommend a 32 mm femoral head if MoXLPE bearings are used. In hips operated on with larger bearings the use of ceramic heads on XLPE appears to be safer.
Cite this article: EFORT Open Rev 2018;3 DOI: 10.1302/2058-5241.3.170061.
Keywords: head size, large bearing, dislocation, hip arthroplasty, revision
Introduction
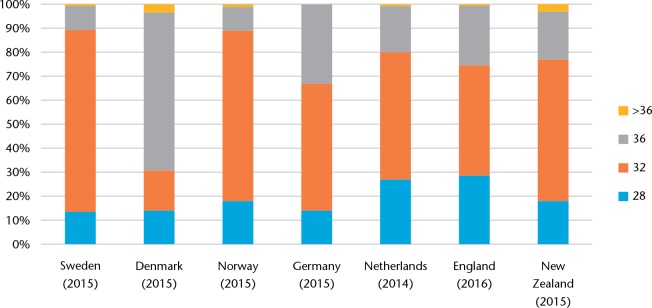
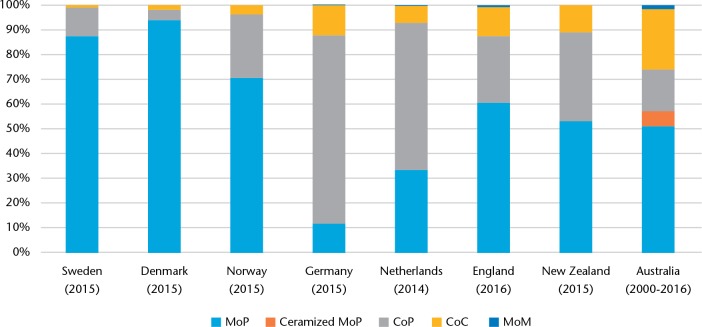
Total hip arthroplasty (THA) currently comprises a variety of head sizes and bearing types. The size of femoral head used in THA gradually increased from 22 mm in the 1960s to 28 mm in the 1990s, and thereafter to 32 mm in the mid-2000s. According to several recent registry reports1-7 the use of 36 mm heads has increased since the mid-2000s. Currently the most common head diameter in THA is 32 mm, as stated by reports from the majority of the registries (Fig. 1).1,3,6,7 Modern wear-resistant sockets such as highly cross-linked polyethylene (XLPE), with or without antioxidants, and ceramics have encouraged the use of so-called ‘larger heads’ comprising a variety of head sizes > 36 mm.8 In this review, the use of 28 mm or greater head diameter in THA with metal-on-XLPE (MoXLPE), ceramic-on-XLPE (CoXLPE) and ceramic-on-ceramic (CoC) bearings is analyzed with respect to range of movement, dislocation, functional outcomes, wear, taper corrosion and groin pain. We excluded hip arthroplasties with metal-on-metal (MoM) bearings due to a limited number of MoMs being used lately (Fig. 2). We also excluded dual mobility acetabular components since this bearing concept is predominantly used in patients with a high risk of dislocation and/or revision situations, has limited long-term follow-up internationally and is still subject to uncertainty regarding polyethylene wear, intraprosthetic dislocation and implant fixation.9-11
Fig. 1.
The current use of different head sizes in various arthroplasty registers across the world1–7
Fig. 2.
The current use of different bearing surfaces in various arthroplasty registers across the world1–8
The benefits and drawbacks of large bearings
The common arguments supporting use of larger femoral heads are primarily the ability to provide a wider impingement-free range of movement and an increase in jumping distance, reducing the risk of dislocation. Moreover, it is argued that big heads are more anatomical since their size is closer to the original size of the native femoral head and this should provide better functional results. On the other hand, there are concerns about the use of big heads in terms of increased wear that might lead to implant loosening, as well as taper corrosion (trunnionosis) and a higher risk of groin pain.
In this paper, we have summarized the evidence behind each of these arguments.
Head size and range of movement of the prosthetic hip
Range of hip movement after THA is determined by patient-specific, surgical and prosthesis-specific factors. Examples are obesity, preoperative hip stiffness, surgical approach, extent of soft-tissue release and repair, implant positioning and implant characteristics. It could be argued that implant design, implant positioning and soft-tissue release set the maximal potential of range of movement that might be limited by soft-tissue repair, impingement, preoperative stiffness, obesity and finally compliance with postoperative rehabilitation. Impingement can occur between the liner and the neck, i.e. implant-to-implant impingement, or between the patient’s own bone and soft tissues, for example between the trochanter major and joint capsule or the trochanter and osteophytes. Head size is only one of the implant characteristics affecting range of movement. It has been demonstrated in finite element analysis and in vitro that increasing head size given a constant neck thickness, i.e. increasing the head-neck ratio, results in a wider impingement-free range of movement.12,13 This effect reaches its limits at head sizes of 38 mm, where range of movement is no longer restricted by implant-to-implant but rather by bone-to-soft tissue/bone impingement,14 which has been confirmed in the following in vivo studies. Intraoperative measurements using CT-based navigation have demonstrated greater range of movement in THA with a 40 mm head compared with a 28 mm head.15 In a study by Matsushita et al,16 postoperative measurements demonstrated a greater range of hip movement in THA with 32 mm compared with 26 mm heads. However, this could not be confirmed in another study where the authors applied intraoperative measurements17 and found that an increase in range of movement was dependent on femoral offset rather than changing from 26 mm to 32 mm head. In a more recent study18 there was no difference in either range of movement or patient-reported outcomes between patients operated on with a 36 mm head and those with head sizes > 36 mm. This is in accordance with a previous in vitro study that demonstrated lack of additional benefits to range of movement when increasing femoral head size > 38 mm.14 Using femoral heads > 36 mm in order to improve range of hip movement is therefore questionable.
Head size and risk of dislocation after THA
The degree of lateral transition of the femoral head centre relative to the centre of the acetabular component required to dislocate defines the jumping distance. With larger head size, the jumping distance increases. However, jumping distance also depends on acetabular component inclination and anteversion and head offset, which is the distance from the centre of the head to the opening plane of the acetabular component.12 The increased jumping distance and hip range of movement associated with bigger femoral heads should theoretically lower the risk of dislocation. In this paragraph, we examine the current evidence associating head size and early (within three years) dislocation after THA. Late dislocations, which are most commonly due to loosening or wear, are discussed later in this manuscript.
Since dislocation after primary THA is rare, it is difficult to study this complication in randomized controlled trials (RCT), as a large number of patients is needed to demonstrate a statistically significant decrease in dislocation rate. We only found one sufficiently powered RCT19 that compared the incidence of dislocation at one year after primary THA between 36 mm and 28 mm MoXLPE bearings, excluding patients with anticipated high risk of dislocation. This study showed a significant difference in the incidence of dislocations (3.6%; 95% confidence interval 0.9 to 6.8) between the groups, favouring the use of 36 mm heads. Registry studies commonly use revision due to dislocation as the main outcome when studying dislocations. In a recent study from the Finnish Arthroplasty Register, hip arthroplasties with a femoral head diameter of 32 mm, 36 mm and > 36 mm were associated with a lower risk of revision due to dislocation compared with 28 mm heads.20 On the other hand, no statistically significant difference was found between 28 mm, 32 mm and 36 mm heads using 28 mm as a reference in another study from the Swedish Hip Arthroplasty Registry.21 A recent study from the Kaiser Permanente Total Joint Registry demonstrated a higher risk of dislocation for bearings < 32 mm compared with 36 mm.22 The most recent study published from the Dutch Arthroplasty Register23 reported a 58% higher risk of revision due to dislocation for THA performed with a 22 mm to 28 mm head compared with 32 mm. The same study showed that THA with 36 mm heads had an even lower risk of revision due to dislocation compared with 32 mm but this difference was statistically significant only in patients operated through the posterolateral surgical approach.
Finally, data from the Australian Orthopaedic Association National Joint Replacement Registry (hereinafter referred to as the Australian Registry) showed a declining cumulative incidence of dislocation at one year from 2.0% down to 0.1% as the head size increases from 28 mm or smaller to 40 mm or bigger in CoC bearings.8 Based on the findings of the above-mentioned studies with short- to medium-term follow-up, increasing femoral head diameter up to 32 mm or 36 mm, especially when a posterior approach is used, seems to be associated with a decreased risk of dislocation compared with bearing sizes of 28 mm or smaller. However, one should keep in mind that these studies do not cover the long-term effect of head size on THA stability.
Late dislocations are considered to occur secondary to bearing wear and can therefore not be examined irrespective of the bearing surface. In a recently published study24 from the Australian Registry, late dislocation after primary THA performed with 28 mm, 32 mm and 36 mm MoXLPE, CoXLPE and CoC bearings was investigated. The study found an increased cumulative percentage revision (CPR) due to dislocation for 36 mm MoXLPE compared with 36 mm CoXLPE and CoC THA at nine-year follow-up. For 28 mm and 32 mm head sizes, there was no difference in CPR due to dislocation between the different bearing surfaces. The authors concluded that 36 mm MoXLPE THA had a higher risk of revision due to late dislocation than CoXLPE and CoC. Moreover, they suggested this difference was due to the effect of the 36 mm metal head on taper corrosion rather than the effect of the 36 mm head on XPLE wear.24 These results suggest some caution if 36 mm heads are used in MoXLPE THA, as its long-term survival could be compromised by late dislocation despite the initial short- to medium-term stabilizing benefits of 36 mm heads.
Head size and functional results
The native femoral head diameter averages approximately 48 mm in female patients and 55 mm in male patients.25 It is argued that restoring the native femoral head size is beneficial from an anatomical point of view and will therefore achieve better functional results.26,27 Such big heads are, however, possible only in MoM THA or hip resurfacing, because both in hard-on-soft bearings and in CoC THA the head size is limited by the minimum thickness of the ceramic and XLPE liners.27 We found only one study supporting this hypothesis; the authors reported significantly better activities of daily living (ADL) function in patients with 32 mm heads compared with those with 26 mm heads.16 However, clinical studies have not been able to demonstrate a statistically significant increase in hip function in terms of various patient-reported outcomes,28,29 clinical outcome scores18 and gait function30,31 in bearings > 32 mm or 36 mm. It is therefore suggested that there are no functional benefits in using femoral heads > 36 mm.
Head size and wear
There are two main concerns when it comes to big femoral heads and the longevity of THA: bearing wear and taper corrosion. Bearing wear and head size cannot be examined irrespective of the bearing surface as different materials have different bearing friction properties. Fractures of thin liners and bearing wear pose threats to THA survivorship. Although there is an agreement about the minimum safe thickness of XLPE liners at 5 mm to 6 mm,27 in ceramic inserts the minimum thickness is debated between 6 mm and as thin as 3.5 mm depending on the type of ceramic material and design.32,33 The thickness of the metal back is also important as thick metal backs combined with large heads reduce the liner thickness while thin metal backs on the other hand can be deformed on impaction, compromising the seating and locking mechanism of the liner especially in the more sensitive ceramic bearings.
It is well known that bearing particles (metal, polyethylene, ceramic) can cause a foreign body reaction, triggering an osteolytic process that eventually leads to implant loosening. Furthermore, with increasing wear, the head moves eccentrically in the liner, resulting in impingement and potentially instability and late dislocation. In vitro studies have indicated that bearing wear in XLPE and vitamin E-diffused XLPE is independent of head size up to 46 mm.34,35 A more recent study36 showed an increased frictional torque in MoXLPE bearings for head sizes 36 mm and 40 mm compared with 28 mm and 32 mm. In the same study, there was no difference in frictional torque related to head size when a CoXLPE bearing was used. Finally, vitamin E-diffused XLPE, combined with both metal and ceramic 32 mm heads, showed a higher fictional torque compared with XLPE.37 In long-term clinical studies no differences have been demonstrated in linear wear between 26 mm, 28 mm, 32 mm and 36 mm to 40 mm heads when MoXLPE bearings are used.38,39 However, there was significantly more volumetric wear in 36–40 mm heads compared with smaller sizes.39 These findings comply with both the increased frictional torque36 and the decreased survival due to late dislocation for 36 mm MoXLPE bearings compared with CoC and CoXLPE bearings.24 Moreover, a 13-year report on THA survival from the Australian Registry shows that THA with both bigger and smaller than 32 mm MoXLPE bearings have a greater risk of revision compared with 32 mm.8 Whilst < 32 mm bearings were revised more frequently due to dislocation, > 32 mm bearings were revised more frequently due to aseptic loosening or fracture,8 complications that can be associated with wear. The same report demonstrated a higher 13-year survival rate for 36 mm or bigger CoC bearings compared with 32 mm or smaller. As in MoXLPE bearings, the main reason for revision in CoC bearings < 32 mm was dislocation, whilst in bearings > 32 mm aseptic loosening and fractures were predominant. There is a concern for liner fracture in larger CoC bearings, as the use of > 32 mm heads, especially in small patients, could push the thickness of the ceramic liner and its metal back to its lowest limits; however, so far there is not enough evidence as head size has not been identified as a risk factor for ceramic liner fracture.40 Thus, from a wear perspective, the use of 32 mm heads in MoXLPE THA seems to pose a smaller threat to THA longevity than bigger sizes. Ceramic heads seem to have a safer profile when combined with XLPE liners when femoral head sizes > 32 mm are used compared with metal heads.
Head size and taper corrosion
Fretting and corrosion, also known as ‘trunnionosis’, at the head-neck junction of modular metal heads has gained a lot of attention in recent years. Although more common in MoM,41,43 it has also been reported in MoXLPE THA.42,44,45 This phenomenon has been correlated to groin pain, adverse local tissue reaction (ALTR), THA instability secondary to erosion of joint capsule and abductor musculature26,42 and femoral head-neck dissociation.46 An association between large heads, especially combined with small taper dimensions, and trunnionosis has been reported as the result of increased torque along the taper interface during activity.47-49 However, this theory has been questioned by a study comparing different head sizes (22 mm to 44 mm) and taper designs in MoXLPE hips, concluding that head size does not influence either fretting or corrosion.50 In patients with large-headed MoM hips, however, increasing head size has been shown to be an independent risk factor for revision due to ALTR.51 This difference between MoXLPE and MoM hips may be explained by the fact that head sizes are on average markedly larger in MoM THA than in MoXLPE THA, and it has also been speculated that the higher frictional torque associated with large diameter MoM bearings is transmitted along the taper junction and would thus be a contributing factor to wear and corrosion at this interface.47 Irrespective of the bearing type, this complication seems to be associated with specific small taper designs, such as short and rough compared with smooth and long tapers, a difference in head and trunnion alloys and length of implantation.50,52,53 To sum up, association between head size and trunnionosis is being debated in the published literature and there seems to be a lack of consensus currently, especially in MoXLPE THAs.
Head size and groin pain
Groin pain following THA can be a symptom suggestive of many complications. Infection, implant loosening and ALTRs might present as groin pain. Illiopsoas impingement has been reported as a possible cause of persistent groin pain after THA.26,54 Although mainly associated with oversized or malpositioned (retroverted) acetabular components,54-56 it has also been reported in patients with larger heads in MoM THA. So far, there are only case reports of iliopsoas impingement in THA with well-positioned components in three female patients who had received heads larger than their native femoral head.57 The pain resolved after release of the tendon and downsizing of the bearing. Illiopsoas impingement has also been reported in one case with MoP 36 mm THA where the prosthetic head was smaller than the native femoral head and the pain resolved after arthroscopic tendon release.58 The suggested pathophysiological mechanism connecting large heads to iliopsoas impingement includes overstuffing of the anterior capsule, protrusion of the large prosthetic head anteriorly and medially in relation to the native femoral head and scarring between the anterior capsule and the tendon.57,59 Thus, there might be an association between iliopsoas impingement and THA with head sizes that are considered big in relation to the native femoral head size. This association and potential cause-effect relation warrants further investigation.
Conclusions
The most commonly used bearing sizes in primary THA are 32 mm and 36 mm. The optimal bearing size should combine the highest possible stability and best hip function with the lowest possible wear in an attempt to increase THA longevity. Keeping in mind that the longevity also depends on patients’ lifestyle, surgical technique and implant design, we tried in our review to identify the femoral head size that best meets the above-mentioned requirements. We examined the current evidence on associations between head size and hip range of movement, dislocation, hip function, bearing wear, taper corrosion and groin pain due to iliopsoas impingement. In summary, we found that:
- hip range of movement increases with larger bearing sizes up to 36 mm to 38 mm;
- 36 mm or larger femoral heads provide THA with greater stability compared with 28 mm or smaller, and probably even with 32 mm;
- hip function and patient-reported outcomes do not improve in THA with heads > 32 mm to 36 mm;
- bearings > 32 mm have increased volumetric wear and frictional torque compared with 32 mm or smaller in MoXLPE THA but not in CoXLPE;
- long-term THA survival is better for 32 mm MoXLPE bearings compared with both bigger and smaller bearings;
- possible cause-effect relation between large femoral heads and taper corrosion is controversial;
- the effect of head size on the incidence of groin pain due to iliopsoas impingement after THA needs further investigation.
Based on current evidence we recommend the use of the 32 mm head size when a MoXLPE THA is being used, especially in young patients where THA longevity is of great importance. If bigger head sizes are desired, then ceramic heads up to 36 mm to 38 mm on XLPE or possibly ceramic inserts should be considered. Whereas novel technologies will probably allow the use of thinner liners accommodating 36 mm or larger heads within the average population, > 32 mm heads should not be used at the expense of acetabular bone preservation as there are patients and pathologies where bone stock preservation for future surgery is more important than striving for a larger head. Femoral heads > 38 mm should probably not be used routinely since they do not seem to provide any additional benefits and it is still not clear whether they are associated with trunnionosis and groin pain.
Most registry studies use 28 mm heads as a baseline when studying the association between dislocation and head size. Since 28 mm heads are rarely used nowadays, future studies should use 32 mm as a reference. Further studies are needed to evaluate the long-term effect of bigger head sizes on wear of thin polyethylene components and taper corrosion, the presence of any association between large femoral heads and groin pain, and to elucidate the role of 36 mm heads when used in ceramic articulations.
Footnotes
ICMJE Conflict of interest statement: M. Mohaddes declares grants from ZimmerBiomet; Travel/accommodation/meeting expenses from Link, ZimmerBiomet and Stryker, activities outside the submitted work. A. Eskelinen declares grants from DePuy; lecture fees from DePuy; research funding from ZimmerBiomet, activities outside the submitted work. O. Rolfson declares lecture fees from Link and ZimmerBiomet, activities outside the submitted work.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. No authors listed. Swedish Hip Arthroplasty Register. Annual report; 2015. https://registercentrum.blob.core.windows.net/shpr/r/Annual-Report-2015-H19dFINOW.pdf (date last accessed 16 January 2018).
- 2. No authors listed. Danish Hip Arthroplasty Register. Annual report 2016. http://danskhoftealloplastikregister.dk/wp-content/uploads/2015/11/DHR-%C3%A5rsrapport-2016.pdf (date last accessed 16 January 2018).
- 3. No authors listed. The Norwegian Arthroplasty Register. Annuar Report 2016. http://nrlweb.ihelse.net/eng/Rapporter/Report2016_english.pdf (date last accessed 16 January 2018).
- 4. No authors listed. LROI Report 2014. Arthroplasty in the Picture. Annual Report of the Dutch Arthroplasty Register (Landelijke Registratie Orthopedische Implantaten); 2014. https://www.lroi.nl/downloads/9/Report%20LROI%202014%20English.pdf (date last accessed 16 January 2018).
- 5. No authors listed. Endoprothesenregister Deutschland (EPRD). Jahresbericht 2015. https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/EPRD-Jahresbericht_2015_FINAL_Web.pdf (date last accessed 16 January 2018).
- 6. No authors listed. National Joint Registry: 14th Annual Report, National Joint Registry for England, Wales and Northern Ireland, 2017. http://www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2014th%20Annual%20Report%202017.pdf (date last accessed 16 January 2018).
- 7. No authors listed. The New Zealand Joint Registry; 17th yearn report: January 1999. to December 2015. https://nzoa.org.nz/system/files/NZJR%2017%20year%20Report.pdf (date last accessed 16 January 2018).
- 8. No authors listed. Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2017 Annual Report; Adelaide: AOA, 2017. https://aoanjrr.sahmri.com/documents/10180/397736/Hip%2C%20Knee%20%26%20Shoulder%20Arthroplasty (date last accessed 16 January 2018). [Google Scholar]
- 9. Grazioli A, Ek ET, Rüdiger HA. Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop 2012;36:2411-2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Caton JH, Prudhon JL, Ferreira A, Aslanian T, Verdier R. A comparative and retrospective study of three hundred and twenty primary Charnley type hip replacements with a minimum follow up of ten years to assess whether a dual mobility cup has a decreased dislocation risk. Int Orthop 2014;38:1125-1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mohaddes M, Cnudde P, Rolfson O, Wall A, Kärrholm J. Use of dual-mobility cup in revision hip arthroplasty reduces the risk for further dislocation: analysis of seven hundred and ninety one first-time revisions performed due to dislocation, reported to the Swedish Hip Arthroplasty Register. Int Orthop 2017;41:583-588. [DOI] [PubMed] [Google Scholar]
- 12. Sariali E, Lazennec JY, Khiami F, Catonné Y. Mathematical evaluation of jumping distance in total hip arthroplasty: influence of abduction angle, femoral head offset, and head diameter. Acta Orthop 2009;80:277-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Crowninshield RD, Maloney WJ, Wentz DH, Humphrey SM, Blanchard CR. Biomechanics of large femoral heads: what they do and don’t do. Clin Orthop Relat Res 2004;429:102-107. [PubMed] [Google Scholar]
- 14. Burroughs BR, Hallstrom B, Golladay GJ, Hoeffel D, Harris WH. Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes. J Arthroplasty 2005;20:11-19. [DOI] [PubMed] [Google Scholar]
- 15. Tsuda K, Haraguchi K, Koyanagi J, et al. A forty millimetre head significantly improves range of motion compared with a twenty eight millimetre head in total hip arthroplasty using a computed tomography-based navigation system. Int Orthop 2016;40:2031-2039. [DOI] [PubMed] [Google Scholar]
- 16. Matsushita I, Morita Y, Ito Y, Gejo R, Kimura T. Activities of daily living after total hip arthroplasty. Is a 32-mm femoral head superior to a 26-mm head for improving daily activities? Int Orthop 2011;35:25-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jinno T, Koga D, Asou Y, et al. Intraoperative evaluation of the effects of femoral component offset and head size on joint stability in total hip arthroplasty. J Orthop Surg (Hong Kong) 2017;25:2309499016684298. [DOI] [PubMed] [Google Scholar]
- 18. Delay C, Putman S, Dereudre G, et al. Is there any range-of-motion advantage to using bearings larger than 36mm in primary hip arthroplasty: A case-control study comparing 36-mm and large-diameter heads. Orthop Traumatol Surg Res 2016;102:735-740. [DOI] [PubMed] [Google Scholar]
- 19. Howie DW, Holubowycz OT, Middleton R, Large Articulation Study Group. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg [Am] 2012;94-A:1095-1102. [DOI] [PubMed] [Google Scholar]
- 20. Kostensalo I, Junnila M, Virolainen P, et al. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop 2013;84:342-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hailer NP, Weiss RJ, Stark A, Kärrholm J. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop 2012;83:442-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cafri G, Paxton EW, Love R, Bini SA, Kurtz SM. Is There a Difference in Revision Risk Between Metal and Ceramic Heads on Highly Crosslinked Polyethylene Liners? Clin Orthop Relat Res 2017;475:1349-1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zijlstra WP, De Hartog B, Van Steenbergen LN, Scheurs BW, Nelissen RGHH. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop 2017;88:395-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shah SM, Walter WL, Tai SM, Lorimer MF, de Steiger RN. Late Dislocations After Total Hip Arthroplasty: Is the Bearing a Factor? J Arthroplasty 2017;32:2852-2856. [DOI] [PubMed] [Google Scholar]
- 25. Young EY, Gebhart J, Cooperman D, Ahn NU. Are the left and right proximal femurs symmetric? Clin Orthop Relat Res 2013;471:1593-1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cooper HJ, Della Valle CJ. Large diameter femoral heads: is bigger always better? Bone Joint J 2014;96-B(suppl A):23-26. [DOI] [PubMed] [Google Scholar]
- 27. Girard J. Femoral head diameter considerations for primary total hip arthroplasty. Orthop Traumatol Surg Res 2015;101(suppl):S25-S29. [DOI] [PubMed] [Google Scholar]
- 28. Hanna SA, Sewell MD, Sri-Ram K, et al. The effect of femoral head size on functional outcome in primary total hip arthroplasty: a single-blinded randomised controlled trial. Hip Int 2012;22:592-597. [DOI] [PubMed] [Google Scholar]
- 29. Allen CL, Hooper GJ, Frampton CM. Do larger femoral heads improve the functional outcome in total hip arthroplasty? J Arthroplasty 2014;29:401-404. [DOI] [PubMed] [Google Scholar]
- 30. Jensen C, Penny JØ, Nielsen DB, Overgaard S, Holsgaard-Larsen A. Quantifying gait quality in patients with large-head and conventional total hip arthroplasty–a prospective cohort study. J Arthroplasty 2015;30:2343-8.e1. [DOI] [PubMed] [Google Scholar]
- 31. Zagra L, Anasetti F, Bianchi L, Licari V, Giacometti Ceroni R. No difference in gait recovery after THA with different head diameters: a prospective randomized study. Clin Orthop Relat Res 2013;471:3830-3837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Masson B. Comments on: “Femoral head diameter considerations for primary total hip arthroplasty” by J. Girard published in Orthop Trauma Surg Res 2015;101:S25-9. Orthop Traumatol Surg Res 2015;101:265. [DOI] [PubMed] [Google Scholar]
- 33. Girard J. Response to the letter by B. Masson. Orthop Traumatol Surg Res 2015;101:267-268. [DOI] [PubMed] [Google Scholar]
- 34. Oral E, Muratoglu OK. Vitamin E diffused, highly crosslinked UHMWPE: a review. Int Orthop 2011;35:215-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Muratoglu OK, Bragdon CR, O’Connor D, et al. Larger diameter femoral heads used in conjunction with a highly cross-linked ultra-high molecular weight polyethylene: a new concept. J Arthroplasty 2001;16(suppl 1):24-30. [DOI] [PubMed] [Google Scholar]
- 36. Meneghini RM, Lovro LR, Wallace JM, Ziemba-Davis M. Large Metal Heads and Vitamin E Polyethylene Increase Frictional Torque in Total Hip Arthroplasty. J Arthroplasty 2016;31:710-714. [DOI] [PubMed] [Google Scholar]
- 37. Meneghini RM, Lovro LR, Wallace JM, Ziemba-Davis M. Large Metal Heads and Vitamin E Polyethylene Increase Frictional Torque in Total Hip Arthroplasty. J Arthroplasty 2016;31:710-714. [DOI] [PubMed] [Google Scholar]
- 38. Hagio K, Saito M, Okawa T, et al. Polyethylene wear associated with 26- and 32-mm heads in total hip arthroplasty: a multicenter, prospective study. J Arthroplasty 2016;31:2805-2809. [DOI] [PubMed] [Google Scholar]
- 39. Lachiewicz PF, Soileau ES, Martell JM. Wear and Osteolysis of Highly Crosslinked Polyethylene at 10 to 14 Years: The Effect of Femoral Head Size. Clin Orthop Relat Res 2016;474:365-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Traina F, De Fine M, Di Martino A, Faldini C. Fracture of ceramic bearing surfaces following total hip replacement: a systematic review. BioMed Res Int 2013;2013:157247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lanting BA, Teeter MG, Howard JL, MacDonald SJ, Van Citters DW. Metal-on-metal compared with metal-on-polyethylene: the effect on trunnion corrosion in total hip arthroplasty. J Arthroplasty 2017;32:2574-2579. [DOI] [PubMed] [Google Scholar]
- 42. Cooper HJ, Della Valle CJ, Berger RA, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg [Am] 2012;94-A:1655-1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fricka KB, Ho H, Peace WJ, Engh CA., Jr. Metal-on-metal local tissue reaction is associated with corrosion of the head taper junction. J Arthroplasty 2012;27(suppl):26-31.e1. [DOI] [PubMed] [Google Scholar]
- 44. Witt F, Bosker BH, Bishop NE, et al. The relation between titanium taper corrosion and cobalt-chromium bearing wear in large-head metal-on-metal total hip prostheses: a retrieval study. J Bone Joint Surg [Am] 2014;96:e157, 1-9. [DOI] [PubMed] [Google Scholar]
- 45. Whitehouse MR, Endo M, Zachara S, et al. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J 2015;97-B:1024-1030. [DOI] [PubMed] [Google Scholar]
- 46. Matsen Ko L, Chen AF, Deirmengian GK, Hozack WJ, Sharkey PF. Catastrophic Femoral Head-Stem Trunnion Dissociation Secondary to Corrosion. J Bone Joint Surg [Am] 2016;98:1400-1404. [DOI] [PubMed] [Google Scholar]
- 47. Dyrkacz RM, Brandt JM, Ojo OA, Turgeon TR, Wyss UP. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J Arthroplasty 2013;28:1036-1040. [DOI] [PubMed] [Google Scholar]
- 48. Carli A, Politis A, Zukor D, Huk O, Antoniou J. Clinically significant corrosion at the head-neck taper interface in total hip arthroplasty: a systematic review and case series. Hip Int 2015;25:7-14. [DOI] [PubMed] [Google Scholar]
- 49. DelBalso C Teeter MG Tan SC Howard JL Lanting BA. Trunnionosis: Does Head Size Affect Fretting and Corrosion in Total Hip Arthroplasty? J Arthroplasty 2016;31:2332-2336. [DOI] [PubMed] [Google Scholar]
- 50. Triantafyllopoulos GK, Elpers ME, Burket JC, et al. Otto Aufranc Award: large heads do not increase damage at the head-neck taper of metal-on-polyethylene total hip arthroplasties. Clin Orthop Relat Res 2016;474:330-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Reito A, Elo P, Puolakka T, Pajamäki J, Eskelinen A. Femoral diameter and stem type are independent risk factors for ARMD in the large-headed ASR THR group. BMC Musculoskelet Disord 2015;16:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Brock TM, Sidaginamale R, Rushton S, et al. Shorter, rough trunnion surfaces are associated with higher taper wear rates than longer, smooth trunnion surfaces in a contemporary large head metal-on-metal total hip arthroplasty system. J Orthop Res 2015;33:1868-1874. [DOI] [PubMed] [Google Scholar]
- 53. Hothi HS, Eskelinen AP, Berber R, et al. Factors Associated With Trunnionosis in the Metal-on-Metal Pinnacle Hip. J Arthroplasty 2017;32:286-290. [DOI] [PubMed] [Google Scholar]
- 54. Henderson RA, Lachiewicz PF. Groin pain after replacement of the hip: aetiology, evaluation and treatment. J Bone Joint Surg [Br] 2012;94-B:145-151. [DOI] [PubMed] [Google Scholar]
- 55. Odri GA, Padiolleau GB, Gouin FT. Oversized cups as a major risk factor of postoperative pain after total hip arthroplasty. J Arthroplasty 2014;29:753-756. [DOI] [PubMed] [Google Scholar]
- 56. Park KK, Tsai TY, Dimitriou D, Kwon YM. Three-dimensional in vivo difference between native acetabular version and acetabular component version influences iliopsoas impingement after total hip arthroplasty. Int Orthop 2016;40:1807-1812. [DOI] [PubMed] [Google Scholar]
- 57. Browne JA, Polga DJ, Sierra RJ, Trousdale RT, Cabanela ME. Case report: failure of larger-diameter metal-on-metal total hip arthroplasty resulting from anterior iliopsoas impingement. J Arthroplasty 2011;26:978.e5-978e8. [DOI] [PubMed] [Google Scholar]
- 58. Baumgarten KM, McKenzie MJ. Case reports: iliopsoas tendon impingement after total hip arthroplasty with use of a large-diameter femoral head. A case report. JBJS Case Connect 2012;2:1-5. [DOI] [PubMed] [Google Scholar]
- 59. Cobb JP, Davda K, Ahmad A, et al. Why large-head metal-on-metal hip replacements are painful: the anatomical basis of psoas impingement on the femoral head-neck junction. J Bone Joint Surg [Br] 2011;93-B:881-885. [DOI] [PubMed] [Google Scholar]