Abstract
Open fractures of the lower extremity are the most common open long bone injuries, yet their management remains a topic of debate.
This article discusses the basic tenets of management and the subsequent impact on clinical outcome. These include the rationale for initial debridement, antimicrobial cover, addressing the soft-tissue injury and definitive skeletal management.
The classification of injury severity continues to be a useful tool in guiding treatment and predicting outcome and prognosis. The Gustilo-Anderson classification continues to be the mainstay, but the adoption of severity scores such as the Ganga Hospital score may provide additional predictive utility.
Recent literature has challenged the perceived need for rapid debridement within 6 hours and the rationale for prolonged antibiotic therapy in the open fracture. The choice of definitive treatment must be decided against known efficacy and injury severity/type.
Recent data demonstrate better outcomes with internal fixation methods in most open tibial fractures, but external fixation continues to be an appropriate choice in more severe injuries. The incidence of infection and non-union has decreased with new treatment approaches but continues to be a source of significant morbidity and mortality.
Assessment of functional outcome using various measures has been prevalent in the literature, but there is limited consensus regarding the best measures to be used.
Cite this article: EFORT Open Rev 2018;3 DOI: 10.1302/2058-5241.3.170072
Keywords: open fractures, infection, debridement
Epidemiology
Open fractures of the tibia are the most common open long bone fractures, with an annual incidence of 3.4 per 100 000.1,2 The mean age of those who sustain open tibial fractures is 43.3 years, most frequently occurring in young adult males and elderly females.1 High energy trauma is the primary mechanism of injury, with over 50% of cases being attributed to road traffic accidents or falls from a great height.1-3 Noteworthy, the vast majority of proximal and distal tibial fractures present with a significant soft-tissue injury and therefore pose additional complexity when managing the injury.
Classification
Open tibial injuries present with a spectrum of injury severity (Fig. 1). It soon became clear that a classification system is needed to quantify the degree of soft-tissue injury and to guide treatment. The Gustilo-Anderson classification has been the mainstay of open fracture classification since it was first described in 1976.4 Gustilo described three broad categories, I-III, based on the extent of soft-tissue injury and the size of corresponding skin wounds. Type I fractures are defined as clean injuries, with a skin wound < 1 cm and simple fracture pattern. Type II fractures have skin wounds > 1 cm, with minimal soft-tissue injury and no flaps or avulsions. Type III were initially more broadly defined as extensive injuries that were either: multi-fragmented fractures; extensive soft-tissue damage; involving vascular injury or traumatic amputations.4 The type III classification was revised in 1984, due in part to the great variation in predictable outcomes that the broad category presented.5 Gustilo et al proposed types III-A, B and C, stratified according to the degree of need for local coverage and evidence of neurovascular compromise. Type III-C is the most severe of the sub-types, defined as an open fracture with associated vascular injury requiring repair.5 Recommendations for fracture management were described by Gustilo and Anderson in their initial study, according to fracture type.
Fig. 1.
A spectrum of injury severity of open tibial fractures exists.
The Gustilo classification is simple and is widely used by surgeons in assessing the severity of traumatic injuries; however, it has met with some scrutiny. Kim and Leopold described the many limitations of the classification,6 with particular emphasis on the limited inter-observer reliability, with as little as 60% concordance between observers7 and other studies showing only moderate agreement between those using the system.8 In addition, the classification system does not consider the degree of soft-tissue injury and therefore may be limited in its evaluation of long-term tissue viability.6 The classification shows some value as a prognostic indicator and a useful guide towards treatment. Other classification systems may, however, better classify open fractures and their associated soft-tissue injury in severity.
The OTA open fracture classification system, proposed by Agel et al in 2010, considers five categories in assessment of injury severity: skin injury; arterial injury; muscle injury; contamination; and bone loss.9 The descriptive features of each domain are shown in Table 1. This systematic approach focuses on the patho-anatomy of the injury and is believed to be applicable to open fractures of all bones in both adult and paediatric cases.9 Agel et al have conducted early studies into the inter-observer reliability of the new system, demonstrating favourable results over the Gustilo-Anderson system10 and good predictive abilities in guiding treatment.11 The system is an improvement over the standard AO classification of fractures and soft-tissue injury, but more time is needed to assess its efficacy in real-life application.
Table 1.
Parameters of the OTA open fracture classification9
| Parameter | Score | |
|---|---|---|
| Injury to skin | Small injury Large/Immeasurable injury Degloving injury |
1 2 3 |
| Muscular injury | No/Minimal injury Moderate/functional injury Extensive muscle injury |
1 2 3 |
| Arterial injury | No injury Non-ischaemic injury Ischaemia |
1 2 4 |
| Degree of contamination | No/minimal contamination Surface Deep |
1 2 3 |
| Amount of bone loss | No loss Minimal bone loss Significant bone loss |
1 2 3 |
The Ganga Hospital classification12 for severity was developed in an effort to better prognosticate limb salvage in open tibial fractures, overcoming the issues faced by Gustilo-Anderson and other severity scores such as the Mangled Extremity Severity Score (MESS).13 The Ganga Hospital classification scores three contributors of wound severity – skin, soft-tissue and skeletal damage – from 1 to 5. The score then corresponds to recommended treatments and likely outcomes.12 The score is of particular value in the assessment of Gustilo III-B fractures. It has shown greater sensitivity and specificity in predicting amputation over other severity scores.14 A cut-off score of 14 (out of 29) has shown good specificity and sensitivity in predicting salvage in open tibial fractures,15,16 and a score of 17 has shown similar efficacy in predicting amputation.14,16 Breakdowns of the score’s parameters are shown in Table 2.
Table 2.
Parameters of Ganga Hospital severity score12
| Parameter | Score | |
|---|---|---|
| Skin losses | No loss Some loss/degloved (+2 to above if over bone) Extensive loss/exposed bone |
1 2 5 |
| Soft tissue injury | No injury Repairable Irreparable Loss of <2 compartments Loss of ⩾2 compartments |
1 2 3 4 5 |
| Bony injury | Fracture, no bone loss Joint involvement Bone losses: < 4cm > 4cm |
1 - 2 3 4 5 |
| Additional risk factors | Age >65 Contamination Chronic illness Systemic injury Other trauma |
+2 for each |
Regardless of classification methods used, the overall consideration for treatment should be guided by the individual clinical picture and established standards.
Principles of management
The fundamental objectives of treatment are to manage the soft-tissue injury, minimize the risk of infection, stabilize and repair the skeletal injury and restore the function of the affected extremity.17-20 The basic principles with reflection on current trends are discussed below.
Standards
Many approaches can be employed in successfully managing the traumatic limb injury. The literature continues to differ in what approaches are favoured. A universal protocol in managing the lower extremity, therefore, does not exist.
In recent years the British Orthopaedic Association (BOA) and British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS) have introduced protocols on how one may approach open traumatic injuries.21 The BOA/BAPRAS guidelines on open injuries of the lower limb use an evidence-based approach in an effort to help standardize the management of traumatic lower extremity injury. The recommendations made are in keeping with modern literature and a step-wise guide is provided to help the surgeon to deal better with the patient. The extent to which these guidelines are employed by trauma centres is yet to be assessed.
Initial assessment and management
Patients presenting with open injury of the lower extremity must first be assessed in accordance with the ATLS system (advanced trauma life support). Most open tibial/ femoral fractures are caused by high impact trauma, so the potential for concomitant life-threatening injury should be ruled out before addressing traumatic limb injury.22 Patients require adequate exposure to complete an examination of all limbs. Assessors should evaluate the neurovascular status of affected limbs. A high index of suspicion should be taken for possible compartment syndromes. If there is significant haemorrhage at a wound site, efforts should be made to control the bleeding with external pressure23 and consideration of more radical approaches if bleeding remains uncontrolled. Vascular damage should be addressed surgically within 3 to 4 hours24 of injury, but may be delayed to 6 hours in warm limbs. The mechanism of injury will help in understanding the exact forces sustained by the patient, which in turn helps in estimating the extent of injury not immediately visible. Furthermore, the extent of environmental contamination should be established.22
Specialist involvement from relevant departments should be sought early in the evaluation of injury. Plans should be formulated early between teams, with clear documentation. Urgent surgery should be considered in heavy contamination.24
Debridement
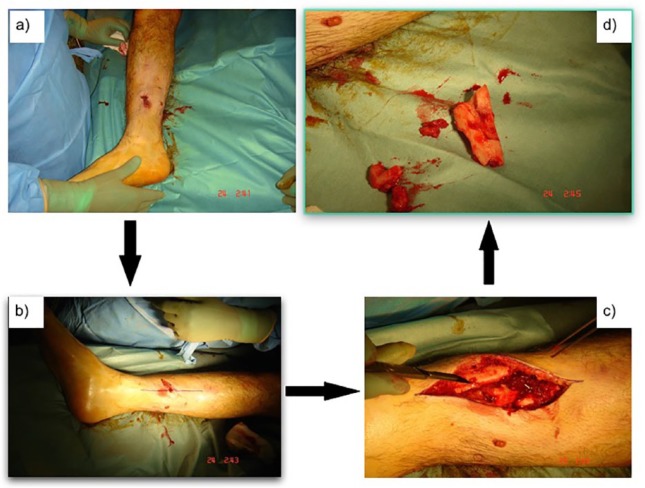
Surgical debridement should be performed in a timely manner following initial presentation. Non-viable tissue should be removed, including necrotic bone fragments and devitalized muscle (Fig. 2). Removal of these tissues is associated with decreased risk of future infection.22,23 Surgical debridement is considered one of the most important procedures for open lower limb fractures.22,23,25 Traditionally, debridement has been performed within 6 hours of presentation. The rationale behind the figure is believed to date back to early studies on micro-organism load following contamination.26 In current literature, the 6-hour wait does not show a clear evidence base. Many studies show insignificant differences in the incidence of infection whether debridement is performed early following presentation or is delayed,22,23,26,27 given that appropriate antibiotic cover is established immediately. Schenker et al27 performed a meta-analysis on the effect of timing on the overall risk of infection in open long bone fractures, finding no difference in the rate of infection of delayed debridement, irrespective of injury severity or anatomical location. The BOA/BAPRAS suggest debridement be carried out within 24 hours of injury21,23,24 on scheduled trauma lists, combining plastic and orthopaedic involvement where possible.
Fig. 2.
The importance of wound debridement: a) grade I open tibial fracture; b) skin incision marked before debridement; c) exposure of the zone of injury; d) removal of devitalized (avascular) bony fragments.
There is no consensus on the type of irrigation solution, nor on the delivery method and pressure.28 There is limited evidence on the value of additives over normal saline in reducing infection.28-31 The FLOW (Fluid Lavage of Open Wounds) trial30 is a recent comprehensive study looking into the impact of different irrigation solutions and pressure on re-operation rates in the open wound due to infection or healing issues. In comparing saline against castile soap solution, saline was superior in preventing the rate of re-operation with statistically significant results.30 In addition the trial showed insignificant differences in re-operation rates when comparing irrigation pressures,30 dispelling many myths regarding its importance in irrigation. A few other studies have argued for other irrigation solutions, including a recent Cochrane database review comparing saline against distilled water. However, this review found no difference in infection rates between water irrigation or isotonic saline.32
Antibiotics
BAPRAS guidelines21 and other authors,33-35 regarding antimicrobial cover, suggest commencement of broad-spectrum antibiotics within 3 hours of injury, which should continue until first debridement. Antibiotics should continue to be administered until primary closure of the wound, or for 72 hours, whichever is sooner.21,24,36 A recent meta-analysis of comparative studies on antibiotic protocols demonstrated insignificant differences in the incidence of septic complication with prolonged therapy (> 72 hours) or short-course (< 72 hours). This was seen irrespective of the fracture severity and sub-group analysis. Comparative results were achieved when comparing even shorter courses (24-48 hours) to prolonged therapy.37
Choice of antibiotic should be decided against local anti-microbial protocol and established guidelines. Intravenous co-amoxiclav (or cephalosporin) and Gentamicin may supply adequate gram-positive and gram-negative cover.
Soft-tissue injury
Gustilo type III-B and C injuries often present with extensive soft-tissue damage. A delay in wound coverage is associated with increased rate of infection and surgical failure.38 BOA/BAPRAS guidance recommended wound cover be established within 72 hours of injury and not delayed beyond seven days.23,24 The choice of coverage is dependent on location and size of defect and overall extent of soft-tissue damage.38
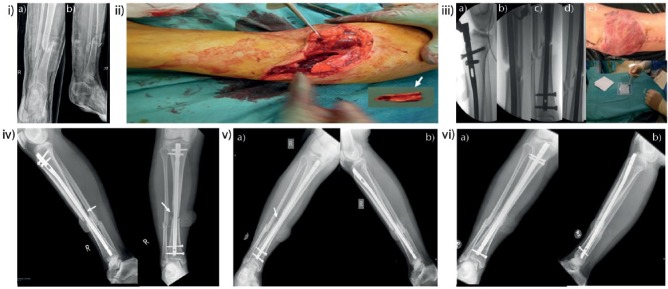
The ‘fix and flap’ approach aims for soft-tissue coverage and definitive fixation within the theatre setting39 (Fig. 3). This approach is considered optimal in managing lower extremity injuries, limiting the complications associated with delayed repair. This is not always possible with complex injuries.
Fig. 3.
i. a, b) Anteroposterior and lateral radiographs of a right tibial open grade III-B fracture in a 24-year-old female following a road traffic accident. ii. Intra-operative photograph demonstrating the extent of soft-tissue damage. The arrow indicates a piece of bone that had no soft tissue attachment (non-viable) which required removal. iii. a, b, c, d) Intra-operative fluoroscopic images illustrating stabilization of the tibia with reamed IM nailing after irrigation and debridement. The wound was covered at the same theatre setting with a latissimus dorsi flap. At the end of flap reconstruction, a BMP-2 growth factor was implanted to attempt to promote fracture healing. iv. Radiographs of the right tibia four weeks after reconstruction. The arrow demonstrates the area of bone loss. v. a, b) Anteroposterior and lateral radiographs at six-month follow-up demonstrating some healing activity at the area of the previous bone loss (arrow). The patient had previously undergone, at four months, removal of the proximal locking screws for dynamization. vi. a, b) Radiographs at 12-month follow-up demonstrating union of the fracture. The patient underwent, nine months previously, exchange nailing to attempt further stimulation of the healing response.
Negative pressure wound therapy has been described as a feasible adjunct in managing Gustilo III-B tibial fractures.40-42 Its use after debridement may allow for flap repair beyond 72 hours without an increase in infection rate, and may reduce the flap necrosis rate.43 However, further study into negative pressure wound therapy is needed.
Fasciocutaneous flaps are the treatment of choice for covering significant defects. The choice of a local or ‘free’ flap is dependent on the location of the defect and potential compromise of local vascular supply. Free flaps are preferable in covering large defects with extensive local soft-tissue damage. They are less prone to vascular compromise secondary to local limb trauma when compared with local flaps.38 A free muscle flap and skin graft may be considered if a fasciocutaneous flap is not deemed adequate to cover significant soft-tissue loss. The outcomes of fasciocutaneous and muscle flaps have been shown to be comparable in managing lower extremity injury.44
Stabilization and skeletal injury
In managing the skeletal injury, the surgeon must consider the challenges in achieving adequate stabilization and the complications associated with inadequate mechanical stability. The method by which surgical fixation is achieved in open tibial fractures has been subject to ongoing debate. The BOA/BAPRAS standards recommend provisional stabilization before definitive fixation, unless this can be achieved at primary debridement. In such cases spanning external fixation is recommended.23,24
The use of external fixators in definitive management is no longer a mainstay in management. A meta-analysis comparing the management of open tibial fractures showed no difference in the rate of nonunion and infection with external fixation when compared with internal fixation methods. However, there were statistically significant differences in the rates of malunion and need for further surgery,45,46 favouring the use of internal fixation as definitive treatment. The popularity of the use of external fixators stemmed from their ease of use and limited soft-tissue interference.38
External fixation, via fine-wire fixators and a circular frame, may continue to be an option in fractures with significant bone loss38 and to support soft-tissue reconstruction, particularly where reconstruction involves weight-bearing areas or is near mobile joints.47 Its efficacy is demonstrated in military studies of severe injuries. Wire or pin placement is key to adequate use of an external fixation device. There is a noted risk of tract pin infection,23 which may complicate injuries. Similarly, however, internal fixation options pose the risk of infection at the site of the prosthesis,48 potentially affecting fracture healing. Particular care must be taken with regards to pin placement and spacing, especially if there is to be planned reconstructive surgery.49 The FIXIT study,50 a prospective randomized trial, aims to assess the outcome of severe, high impact, open injuries of the tibia when managed by external or internal fixation devices. The study looks to cover some of the gaps in the literature relating to the most severe open tibial injuries, with the scientific community waiting to see the final outcomes to be published.
Plating is another method of internal fixation to consider in open fractures of the lower extremity. It poses a risk of infection45 and may compromise periosteal blood supply.38 However, there is reported use of plating in modern management of open tibial fractures as an adjunct to assist intramedullary (IM) nailing. Provisional plating, the temporary use of a dynamic compression plate to stabilize a fracture before nailing, may provide added stability when reaming and inserting a nail.51 The reduced need for large clamps may be of use in surgery, particularly in times of limited surgical assistance. Additionally, this approach may allow greater cortical contact41 and consequently improve the rate of successful union. Limited studies have not shown an increased risk of infection or other complications.52
Definitive repair of the skeletal injury is best achieved with an IM nail, providing the greatest mechanical stability of available surgical methods.25,38 The choice of whether to use reamed or unreamed interlocking nails continues to provoke debate.53 It has been suggested that reaming allows for the insertion of larger diameter nails and increases stability.38,54,55 This may be achieved, however, at the cost of damaging endosteal blood supply and diminishing cortical wall thickness.56,57 Unreamed nailing shows comparable outcomes to reamed nails in terms of infection rates,38,45,56 risk of nonunion and rates of re-operation.45 The conclusions were affirmed by a Cochrane database review,58 demonstrating insignificant differences in complication rates of reamed and unreamed nailing. These findings are consistent with modern studies comparing the two methods. The choice of approach may be considered in relation to the type of injury – reamed nailing shows early union rates in Gustilo type III fractures58 – or may be a matter of surgeon choice. The choice of definitive fixation should be considered on a case-by-case basis, with consideration to be given to the associated soft-tissue or vascular injury.
Complications and outcomes
As expected with any open injury, open fractures of the lower extremity can be subject to ongoing complications. The incidence of complications varies according to treatment approach, injury severity and individual patient factors. Individual studies have shown variable results in clinical outcomes with different methods59-63 and this is due, in part, to the often limited sample sizes that are available at any given study period. An example of the variability among studies can be seen in Table 3, looking at the incidence of adverse complications in Gustilo type III fractures managed with an IM nail, in studies conducted in recent times. The added issues of classification also adversely affect the evaluation of outcome. The Gustilo type III-B subgroup presents great challenges in this area; there is great variability in the possible degree of soft-tissue involvement and therefore severity.
Table 3.
Recent studies on the clinical outcomes of Gustilo type III tibial shaft fractures
| Study | n | IM nail | Union time (weeks) | Infection (n (%)) | Malunion (n (%)) | Re-operation |
|---|---|---|---|---|---|---|
| Naique 200648 | 26 | Reamed | 29 | 3 (12) | 0 (0) | - |
| Tielinen 200749 | 19 | Unreamed | 35 | 0 (0) | - | 9 (19%) |
| Inan 200751 | 29 | Unreamed | 21 | 3 (10) | 5 (17) | 24.1% |
| Rohde 200752 | 20 | Unreamed | - | 10 (10) | 8 (40) | 0.15 |
| Mohseni 201150 | 25 | Unreamed | 6 | 4 (16) | 0 (0) | - |
Overall, limitations that exist in small studies are adequately addressed with recently published systematic reviews and meta-analyses,64-66 which allow a more robust evaluation of other data available on this subject.
Infection
Infection is a big factor for adverse outcomes in the open fracture of the lower extremity. Standards on anti-microbial cover and management of soft-tissue injury have helped to reduce the incidence of infection and consequent complications. However, the risk remains significant. The limb may be complicated by infection from initial inoculation at injury, but may also suffer from iatrogenic infection caused by the surgical approach and choice of implant.
Injuries complicated by infection are more likely to require further operative management67 and complications with bony union. The injury should be assessed for superficial infections, of the wound and superficial tissues, and deep infections, of the soft tissues and osteomyelitis.
Data on the impact of surgical approach on the incidence of infection have shown some variability. Recent meta-analyses have shown the incidence of infection to be significantly reduced in Gustilo type III injuries managed with IM nailing when compared with external fixation.65,66 However, another meta-analysis showed insignificant differences in the rate of infection with both internal and external fixation.64
Nonunion
Nonunion is a known, detrimental, complication of fracture healing. Its impact on functional outcome transcends expected physical limitations. Sufferers may go on to develop psychological problems as a result of chronic intractable pain and subsequent misuse of opiate analgesics and alcohol.68 A study69 assessing the functional outcome six and 12 months after long bone fracture found poorer health outcomes in malunion/nonunions, due primarily to the physical sequelae of disease and a greater level of unemployment.69 Although the retrospective analysis did not show differences in mental health status, chronic disease and pain are known risk factors in the development of mental illness such as depression.70,71
Santolini et al68 analysed the risk factors from nonunion and found open fractures to be the second most significant risk factor in poor bony union, based on levels of evidence in the available literature. The risk was higher in fractures of the tibial shaft due to its poor anterior soft-tissue coverage and vascularization. Tibial shaft fracture with any degree of vascular compromise shows a three times greater risk of nonunion compared with fractures with no vascular involvement.72
Other factors affecting union include the type of management: external fixation carries higher risk of adverse outcomes than IM nailing,65 including nonunion and infection rates. The two noted outcomes have a known relationship: infection contributes to development of necrotic bone and fixation failure, making bony union more difficult.73 It should be noted, however, that severe fractures at initial presentation require external fixation devices, owing to the increased risk of complications.
In addition, it is important to counsel patients on reducing their own risk factors by trying to stop smoking, maintaining better glycaemic control if diabetic and limiting alcohol intake.
Regional pain syndrome
Complex regional pain syndrome may develop in individuals following surgery, particularly following complex fractures.74 The incidence in open tibial fractures is less often noted, but some studies estimate an incidence of 30%. The causes of regional pain syndrome are not entirely clear, but evidence supports a hypothesis of an exaggerated inflammatory response to trauma and nervous hypersentization.74 Definitive treatment is yet to be identified. Patients may experience intense debilitating pain, oedema, blood flow changes in the skin, allodynia and burning sensations.
Amputation
Primary amputation may be considered in cases of uncontrollable haemorrhage, prolonged crush injury, an avascular limb or segmental bone/muscle loss. The decision is not taken lightly and should be discussed with other experienced surgeons.21,75-77 Severity scores may provide a measured value in predicting the need for amputation.13,14
Secondary amputation may also be a viable surgical option in an injury that is complicated by ongoing problems, e.g. deep infection. Amputation is an absolute indicator of poor outcome,21 but may be necessary in preventing further deterioration or indeed maintaining quality of life. Long-term functional outcome may not be significantly affected in the amputee when compared with that which would have occurred in a salvaged injury.21
Functional outcome
Functional outcome is assessed with self-reported patient questionnaires or scores. Many assessment tools have been described in the literature, including the Short Form 36 (SF-36), EQ-5D and specific scores assessing limb and joint function, e.g. Iowa Ankle and Knee scores. There is not known to be a universal tool in the scoring of lower extremity injury. The literature has therefore showed varied use of scoring systems, making accurate comparison difficult.
Lower extremity scores have been proposed in the assessment of the lower limb. The Lower Extremity Functional Scale (LEFS) shows good reliability and prognostic correlation.78 It has been shown to be comparable with SF-36 in assessing open injuries of the lower limb.79 There are limited data, however, on its clinical use in the open fracture of the lower extremity.
Others have used the Enneking Functional score,80 a scoring system traditionally used for functional assessment after resection of musculoskeletal tumours. Its use in lower limb trauma was demonstrated by Khan et al,81 affirming some validity in its use beyond tumours. This score is one of those recommended by BAPRAS,21 particularly following reconstructive surgery. The score is expressed as a percentage of the unaffected contralateral limb. A small study by Filobos et al82 showed good functional outcome of lower limb trauma (52% Gustilo type III-B) using the Enneking score in a specialist centre.
A meta-analysis comparing the functional outcomes using various quality-of-life measures shows statistically significant differences in the incidence of pain and mobility following Gustilo type III tibial shaft fractures compared with the general population.66 Those particular outcomes were based on EQ-5D data, but additional analysis showed significant ankle problems in the injured group using the Iowa score.66
Summary of recommendations
The basic rationale and methods of managing open fractures of the lower extremity remain largely the same. Recent bodies of data have challenged past notions on the importance of the 6-hour wait for debridement and prolonged antibiotic treatment. The open fracture should be assessed as a matter of urgency following presentation, with the commencement of antibiotics within 3 hours, and transfer to theatre for debridement within 24 hours. Antibiotic management should not exceed 72 hours unless there is an indicated need, such as the development of spreading sepsis. Mechanical stabilization may be initially achieved with external fixation if definitive management with an IM nail cannot be achieved at the time of debridement. The ultimate choice of fixation device is dependent on the severity of the injury. Appropriate vascular and plastic surgical involvement should be sought early as indicated by injury severity. Adequate soft-tissue cover and vascularity to the injury site are important to limit complications and promote bone healing.
Even with the current trends in treatment, adverse consequences of infection, nonunion and poor functional outcome continue to plague open injuries of the lower extremity, albeit to a lesser degree. Careful management of the injury and a holistic approach to the patient may better reduce the risk of adverse complications, with particular care to address patient co-morbidities and counselling.
Footnotes
ICMJE Conflict of interest statement: P. Giannoudis declares grant/s from Stryker; consultancy for Zimmer Biomet; payment for lectures from Medtronic, activities outside the submitted work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15-year review. Injury 2012;43:891-7. [DOI] [PubMed] [Google Scholar]
- 2. Larsen P, Elsoe R, Hansen SH, et al. Incidence and epidemiology of tibial shaft fractures. Injury 2015;46:746-50. [DOI] [PubMed] [Google Scholar]
- 3. Jenkins PJ, Keating JF, Simpson AH. Fractures of the tibial shaft. Surgery 2010;28:489-93. [Google Scholar]
- 4. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg [Am] 1976;58-A:453-8. [PubMed] [Google Scholar]
- 5. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984;24:742-6. [DOI] [PubMed] [Google Scholar]
- 6. Kim PH, Leopold SS. In brief: Gustilo-Anderson classification. [corrected]. Clin Orthop Relat Res 2012;470:3270-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brumback RJ, Jones AL. Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons. J Bone Joint Surg [Am] 1994;76-A:1162-6. [DOI] [PubMed] [Google Scholar]
- 8. Horn BD, Rettig ME. Interobserver reliability in the Gustilo and Anderson classification of open fractures. J Orthop Trauma 1993;7:357-60. [DOI] [PubMed] [Google Scholar]
- 9. Orthopaedic Trauma Association: Open Fracture Study Group. A new classification scheme for open fractures. J Orthop Trauma 2010;24:457-64. [DOI] [PubMed] [Google Scholar]
- 10. Agel J, Evans AR, Marsh JL, et al. The OTA open fracture classification: a study of reliability and agreement. J Orthop Trauma 2013;27:379-84. [DOI] [PubMed] [Google Scholar]
- 11. Agel J, Rockwood T, Barber R, Marsh JL. Potential predictive ability of the orthopaedic trauma association open fracture classification. J Orthop Trauma 2014;28:300-6. [DOI] [PubMed] [Google Scholar]
- 12. Rajasekaran S. Ganga hospital open injury severity score - A score to prognosticate limb salvage and outcome measures in Type IIIb open tibial fractures. Indian J Orthop 2005;39:4-13. [Google Scholar]
- 13. Johansen K, Daines M, Howey T, Helfet D, Hansen ST. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma 1990;30:568-72; discussion 572-3. [DOI] [PubMed] [Google Scholar]
- 14. Venkatadass K, Grandhi TSP, Rajasekaran S. Use of Ganga Hospital Open Injury Severity Scoring for determination of salvage versus amputation in open type IIIB injuries of lower limbs in children-An analysis of 52 type IIIB open fractures. Injury 2017;48:2509-14. [DOI] [PubMed] [Google Scholar]
- 15. Madhuchandra P, Rafi M, Devadoss S, Devadoss A. Predictability of salvage and outcome of Gustilo and Anderson type-IIIA and type-IIIB open tibial fractures using Ganga Hospital Scoring system. Injury 2015;46:282-7. [DOI] [PubMed] [Google Scholar]
- 16. Rajasekaran S, Sabapathy SR, Dheenadhayalan J, et al. Ganga hospital open injury score in management of open injuries. Eur J Trauma Emerg Surg 2015;41:3-15. [DOI] [PubMed] [Google Scholar]
- 17. Okike K, Bhattacharyya T. Trends in the management of open fractures. A critical analysis. J Bone Joint Surg [Am] 2006;88-A:2739-48. [DOI] [PubMed] [Google Scholar]
- 18. Zalavras CG, Patzakis MJ. Open fractures: evaluation and management. J Am Acad Orthop Surg 2003;11:212-9. [DOI] [PubMed] [Google Scholar]
- 19. Pape H-C, Webb LX. History of open wound and fracture treatment. J Orthop Trauma 2008;22(suppl):S133-4. [DOI] [PubMed] [Google Scholar]
- 20. Chen AT, Vallier HA. Noncontiguous and open fractures of the lower extremity: Epidemiology, complications, and unplanned procedures. Injury 2016;47:742-7. [DOI] [PubMed] [Google Scholar]
- 21. Nanchahal J, Nayagam S, Khan U, et al. Standards for the management of open fractures of the lower limb. London: British Association of Plastic, Reconstructive and Aesthetic Surgeons; 2009. [Google Scholar]
- 22. Halawi MJ, Morwood MP. Acute management of open fractures: an evidence-based review. Orthopedics 2015;38:e1025-33. [DOI] [PubMed] [Google Scholar]
- 23. Ali AM, Noyes D, Cogswell LK. Management of open fractures of the lower limb. Br J Hosp Med (Lond) 2013;74:577-80. [DOI] [PubMed] [Google Scholar]
- 24. British Orthopaedic Association and British Association of Plastic, Reconstructive and Aesthetic Surgeons. Standard for trauma – 2009. BOAST 4: the management of severe open lower limb fractures. www.boa.ac.uk/publications/boa-standards-trauma-boasts (date last accessed 17 March 2018).
- 25. Griffin M, Malahias M, Khan W, Hindocha S. Update on the management of open lower limb fractures. Open Orthop J 2012;6:571-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Werner CML, Pierpont Y, Pollak AN. The urgency of surgical débridement in the management of open fractures. J Am Acad Orthop Surg 2008;16:369-75. [DOI] [PubMed] [Google Scholar]
- 27. Schenker ML, Yannascoli S, Baldwin KD, Ahn J, Mehta S. Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review. J Bone Joint Surg [Am] 2012;94-A:1057-64. [DOI] [PubMed] [Google Scholar]
- 28. Barnes S, Spencer M, Graham D, Johnson HB. Surgical wound irrigation: a call for evidence-based standardization of practice. Am J Infect Control 2014;42:525-9. [DOI] [PubMed] [Google Scholar]
- 29. Crowley DJ, Kanakaris NK, Giannoudis PV. Irrigation of the wounds in open fractures. J Bone Joint Surg [Br] 2007;89:580-5. [DOI] [PubMed] [Google Scholar]
- 30. Bhandari M, Jeray KJ, Petrisor BA, et al. ; FLOW Investigators. A trial of wound irrigation in the initial management of open fracture wounds. N Engl J Med 2015;373:2629-41. [DOI] [PubMed] [Google Scholar]
- 31. Anglen JO. Comparison of soap and antibiotic solutions for irrigation of lower-limb open fracture wounds. A prospective, randomized study. J Bone Joint Surg [Am] 2005;87-A:1415-22. [DOI] [PubMed] [Google Scholar]
- 32. Fernandez R, Griffiths R. Water for wound cleansing. Cochrane Database Syst Rev 2012;2:CD003861. [DOI] [PubMed] [Google Scholar]
- 33. Lack WD, Karunakar MA, Angerame MR, et al. Type III open tibia fractures: immediate antibiotic prophylaxis minimizes infection. J Orthop Trauma 2015;29:1-6. [DOI] [PubMed] [Google Scholar]
- 34. Holtom PD. Antibiotic prophylaxis: current recommendations. J Am Acad Orthop Surg 2006;14(suppl):S98-S100. [DOI] [PubMed] [Google Scholar]
- 35. Saveli CC, Belknap RW, Morgan SJ, Price CS. The role of prophylactic antibiotics in open fractures in an era of community-acquired methicillin-resistant Staphylococcus aureus. Orthopedics 2011;34:611-6. [DOI] [PubMed] [Google Scholar]
- 36. Lenarz CJ, Watson JT, Moed BR, et al. Timing of wound closure in open fractures based on cultures obtained after debridement. J Bone Joint Surg [Am] 2010;92-A:1921-6. [DOI] [PubMed] [Google Scholar]
- 37. Messner J, Papakostidis C, Giannoudis PV, Kanakaris NK. Duration of administration of antibiotic agents for open fractures: meta-analysis of the existing evidence. Surg Infect (Larchmt) 2017;18:854-67. [DOI] [PubMed] [Google Scholar]
- 38. Melvin JS, Dombroski DG, Torbert JT, et al. Open tibial shaft fractures: II. Definitive management and limb salvage. J Am Acad Orthop Surg 2010;18:108-17. [DOI] [PubMed] [Google Scholar]
- 39. Gopal S, Majumder S, Batchelor AG, et al. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg [Br] 2000;82-B:959-66. [DOI] [PubMed] [Google Scholar]
- 40. Schlatterer DR, Hirschfeld AG, Webb LX. Negative pressure wound therapy in grade IIIB tibial fractures: fewer infections and fewer flap procedures? Clin Orthop Relat Res 2015;473:1802-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lachica RD. Evidence-based medicine: management of acute lower extremity trauma. Plast Reconstr Surg 2017;139:287e-301e. [DOI] [PubMed] [Google Scholar]
- 42. Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg [Br] 2006;88-B:281-9. [DOI] [PubMed] [Google Scholar]
- 43. Foote CJ, Guyatt GH, Vignesh KN, et al. Which surgical treatment for open tibial shaft fractures results in the fewest reoperations? a network meta-analysis. Clin Orthop Relat Res 2015;473:2179-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Parikh PM, Hall MM, Attinger CE, Masden DL, Steinberg JS. External fixation: indications in lower extremity reconstruction and limb salvage. Plast Reconstr Surg 2009;123:160e-1e. [DOI] [PubMed] [Google Scholar]
- 45. Gristina AG, Costerton JW. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J Bone Joint Surg [Am] 1985;67-A:264-73. [PubMed] [Google Scholar]
- 46. Giotakis N, Narayan B. Stability with unilateral external fixation in the tibia. Strateg Trauma Limb Reconstr 2007;2:13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Herscovici D, Jr, Sanders RW, Scaduto JM, Infante A, DiPasquale T. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries. J Orthop Trauma 2003;17:683-8. [DOI] [PubMed] [Google Scholar]
- 48. Pollak AN, McCarthy ML, Burgess AR; The Lower Extremity Assessment Project (LEAP) Study Group. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. J Bone Joint Surg [Am] 2000;82-A:1681-91. [PubMed] [Google Scholar]
- 49. Bhattacharyya T, Mehta P, Smith M, Pomahac B. Routine use of wound vacuum-assisted closure does not allow coverage delay for open tibia fractures. Plast Reconstr Surg. 2008;121:1263-6. [DOI] [PubMed] [Google Scholar]
- 50. OʼToole RV, Gary JL, Reider L, et al. ; METRC. A prospective randomized trial to assess fixation strategies for severe open tibia fractures: modern ring external fixators versus internal fixation (FIXIT Study). J Orthop Trauma 2017;31(suppl):S10-7. [DOI] [PubMed] [Google Scholar]
- 51. Dunbar RP, Nork SE, Barei DP, Mills WJ. Provisional plating of Type III open tibia fractures prior to intramedullary nailing. J Orthop Trauma 2005;19:412-4. [DOI] [PubMed] [Google Scholar]
- 52. Ludwig M, Hymes RA, Schulman J, Pitta M, Ramsey L. Intramedullary nailing of open tibial fractures: provisional plate fixation. Orthopedics 2016;39:e931-6. [DOI] [PubMed] [Google Scholar]
- 53. Bhandari M, Guyatt G, Walter SD, et al. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. J Bone Joint Surg [Am] 2008;90-A:2567-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Anglen JO, Blue JM. A comparison of reamed and unreamed nailing of the tibia. J Trauma 1995;39:351-5. [DOI] [PubMed] [Google Scholar]
- 55. Shao Y, Zou H, Chen S, Shan J. Meta-analysis of reamed versus unreamed intramedullary nailing for open tibial fractures. J Orthop Surg 2014;9:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bong MR, Kummer FJ, Koval KJ, Egol KA. Intramedullary nailing of the lower extremity: biomechanics and biology. J Am Acad Orthop Surg 2007;15:97-106. [DOI] [PubMed] [Google Scholar]
- 57. Hofmann A, Dietz S-O, Pairon P, Rommens PM. The role of intramedullary nailing in treatment of open fractures. Eur J Trauma Emerg Surg 2015;41:39-47. [DOI] [PubMed] [Google Scholar]
- 58. Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev 2012;1:CD008241. [DOI] [PubMed] [Google Scholar]
- 59. Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg [Br] 2006;88:351-7. [DOI] [PubMed] [Google Scholar]
- 60. Tielinen L, Lindahl JE, Tukiainen EJ. Acute unreamed intramedullary nailing and soft tissue reconstruction with muscle flaps for the treatment of severe open tibial shaft fractures. Injury 2007;38:906-12. [DOI] [PubMed] [Google Scholar]
- 61. Mohseni MA, Soleimanpour J, Mohammadpour H, Shahsavari A. AO tubular external fixation vs. unreamed intramedullary nailing in open grade IIIA-IIIB tibial shaft fractures: a single-center randomized clinical trial. Pak J Biol Sci 2011;14:490-5. [DOI] [PubMed] [Google Scholar]
- 62. Inan M, Halici M, Ayan I, Tuncel M, Karaoglu S. Treatment of type IIIA open fractures of tibial shaft with Ilizarov external fixator versus unreamed tibial nailing. Arch Orthop Trauma Surg 2007;127:617-23. [DOI] [PubMed] [Google Scholar]
- 63. Rohde C, Greives MR, Cetrulo C, et al. Gustilo grade IIIB tibial fractures requiring microvascular free flaps: external fixation versus intramedullary rod fixation. Ann Plast Surg 2007;59:14-7. [DOI] [PubMed] [Google Scholar]
- 64. Fang X, Jiang L, Wang Y, Zhao L. Treatment of Gustilo grade III tibial fractures with unreamed intramedullary nailing versus external fixator: a meta-analysis. Med Sci Monit 2012;18:RA49-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Giovannini F, de Palma L, Panfighi A, Marinelli M. Intramedullary nailing versus external fixation in Gustilo type III open tibial shaft fractures: a meta-analysis of randomised controlled trials. Strateg Trauma Limb Reconstr 2016;11:1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Dickson DR, Moulder E, Hadland Y, Giannoudis PV, Sharma HK. Grade 3 open tibial shaft fractures treated with a circular frame, functional outcome and systematic review of literature. Injury 2015;46:751-8. [DOI] [PubMed] [Google Scholar]
- 67. Zelle BA, Boni G. Safe surgical technique: intramedullary nail fixation of tibial shaft fractures. Patient Saf Surg 2015;9:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Santolini E, West R, Giannoudis PV. Risk factors for long bone fracture non-union: a stratification approach based on the level of the existing scientific evidence. Injury 2015;46(suppl 8):S8-S19. [DOI] [PubMed] [Google Scholar]
- 69. Tay W-H, de Steiger R, Richardson M, Gruen R, Balogh ZJ. Health outcomes of delayed union and nonunion of femoral and tibial shaft fractures. Injury 2014;45:1653-8. [DOI] [PubMed] [Google Scholar]
- 70. Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain 1997;13:116-37. [DOI] [PubMed] [Google Scholar]
- 71. Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis 2005;2:A14. [PMC free article] [PubMed] [Google Scholar]
- 72. Dickson K, Katzman S, Delgado E, Contreras D. Delayed unions and nonunions of open tibial fractures. Correlation with arteriography results. Clin Orthop Relat Res 1994;(302):189-93. [PubMed] [Google Scholar]
- 73. Calori GM, Albisetti W, Agus A, Iori S, Tagliabue L. Risk factors contributing to fracture non-unions. Injury 2007;38(suppl 2):S11-8. [DOI] [PubMed] [Google Scholar]
- 74. Goh EL, Chidambaram S, Ma D. Complex regional pain syndrome: a recent update. Burns Trauma 2017;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Webb LX, Bosse MJ, Castillo RC, et al. Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Joint Surg [Am] 2007;89-A:923-8. [DOI] [PubMed] [Google Scholar]
- 76. Bosse MJ, McCarthy ML, Jones AL, et al. The insensate foot following severe lower extremity trauma: An indication for amputation? J Bone Joint Surg [Am] 2005;87-A:2601-8. [DOI] [PubMed] [Google Scholar]
- 77. Cannada LK, Melton DH, Deren ME, Hayda RA, Harvey EJ. Dealing with catastrophic outcomes and amputations in the mangled limb. J Orthop Trauma 2015;29(suppl 12):S39-S42. [DOI] [PubMed] [Google Scholar]
- 78. Binkley JM, Stratford PW, Lott SA, Riddle DL; North American Orthopaedic Rehabilitation Research Network. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther 1999;79:371-83. [PubMed] [Google Scholar]
- 79. Pan S-L, Liang H-W, Hou W-H, Yeh T-S. Responsiveness of SF-36 and Lower Extremity Functional Scale for assessing outcomes in traumatic injuries of lower extremities. Injury 2014;45:1759-63. [DOI] [PubMed] [Google Scholar]
- 80. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;(286):241-6. [PubMed] [Google Scholar]
- 81. Khan U, Smitham P, Pearse M, Nanchahal J. Management of severe open ankle injuries. Plast Reconstr Surg 2007;119:578-89. [DOI] [PubMed] [Google Scholar]
- 82. Filobbos G, Salim F, Khan U. Is the injury severity score relevant in complex lower limb trauma? Ann R Coll Surg Engl 2013;95:1–3. [Google Scholar]