Abstract
Recurrent patellar dislocation is a disabling condition, which can lead to articular cartilage injuries, osteochondral fractures, recurrent instability, pain, decreased activity and patellofemoral osteoarthritis. Trochlear dysplasia represents an important component of patellar dislocation.
Imaging provides an objective basis for the morphological abnormalities and thus allows determination of the surgical strategy according to the concept of ‘à la carte’ surgery.
The main surgical techniques of trochleoplasty are the sulcus deepening trochleoplasty, the ‘Bereiter’ trochleoplasty and the recession trochleoplasty.
At mid-term, all techniques have shown a postoperative improvement in clinical scores, with a low rate of recurrence of dislocation and a possible return to sport. But these techniques do not halt the progression of patellofemoral arthritis.
Cite this article: EFORT Open Rev 2018;3 DOI: 10.1302/2058-5241.3.170058
Keywords: patellar instability, crossing sign, supra-trochlear spur, deepening trochleoplasty, Bereiter trochleoplasty, recession trochleoplasty, patellofemoral osteoarthritis
Introduction
Recurrent patellar instability is a disabling condition that can lead to articular cartilage injuries, osteochondral fractures, pain, decreased activity and patellofemoral osteoarthritis (OA). The average annual incidence of primary patellar dislocation has been reported to be 5.8 cases per 100 000, and the rate is higher for younger and more active populations.1,2 Patellar dislocation is a multifactorial problem, which depends on limb alignment, the osseous structure of the patella and trochlea, and the integrity of the static and dynamic soft-tissue constraints. Trochlear dysplasia represents an important component of patella instability that has been recognized for many years. Dejour et al3 found that 96% of patients with a history of a true patellar dislocation had evidence of trochlear dysplasia. High-grade trochlear dysplasia is characterized by the combination of a flat and/or prominent trochlea proud of the anterior femoral cortex, which offers inadequate tracking during flexion and leads to patellar subluxation. Other static or dynamic abnormalities are usually combined with trochlear dysplasia, such as genu recurvatum, patella alta, increased Q angle and bone torsional abnormalities. Trochleoplasty is indicated mainly for high-grade trochlear dysplasia. In the majority of these cases, trochleoplasty is performed in association with other procedures (such as anterior tibial tubercle [ATT] transfer or medial patella-femoral ligament [MPFL] reconstruction). To determine the best surgical strategy, an accurate analysis of the anatomical abnormalities must be performed with imaging. Many measurements describing trochlear dysplasia have been developed and reported.
We will describe these different measurement techniques, the available surgical techniques and the main outcomes of surgery for trochlear dysplasia.
Imaging findings
Imaging is essential in the assessment of patellar instability, providing an objective basis for the morphological abnormalities and thus allowing the surgeon to determine the appropriate surgical strategy according to the concept of ‘à la carte’ surgery described by Henri Dejour.3,4
Normal anatomy
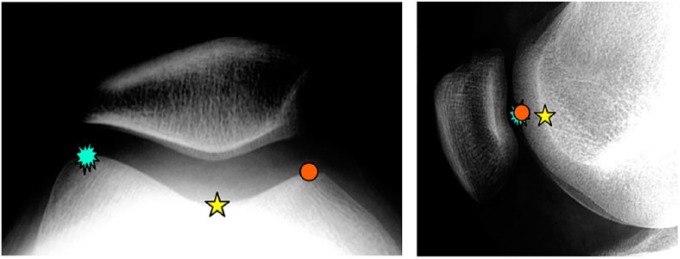
On a true lateral radiograph view of the knee, with perfect superimposition of the condyles posteriorly, three dense radiography lines are outlined on the anterior portion of the distal femoral epiphysis. The two most anterior lines correspond to the contours of the condyles. The curve directly posterior to these lines corresponds to the trough of the trochlear groove, which articulates with the patella during flexion-extension movements (Fig. 1).
Fig. 1.
Axial view and lateral view of a normal trochlea without dysplasia. The two most anterior lines (blue and orange pictures) corresponded to the contours of the condyles. The curve directly posterior to these lines corresponds to the trough of the trochlear groove (yellow star).
Crossing sign
On conventional radiographs, the line which represents the deepest part of the trochlear groove never crosses the anterior border of the two condyles in a normal knee. This line will join the anterior part of the condyles in a dysplastic trochlea; this means that the groove is flat at this precise point (Fig. 2). The crossing sign is repeatable and simple to perform. It is very useful for the diagnosis of trochlear dysplasia and the prediction of future risk of patellar dislocation. The importance of the crossing sign in predicting patellofemoral pain is uncertain.5
Fig. 2.
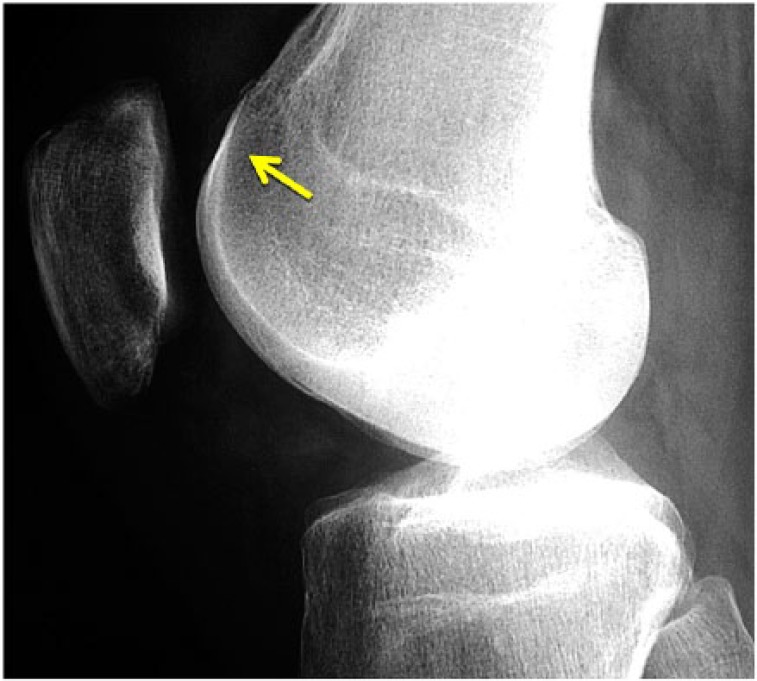
Lateral view radiograph of a right knee showing a crossing sign and a small double contour in the context of trochlear dysplasia type C (D. Dejour’s classification).
Trochlear bump
To analyse the trochlear bump,4 we draw a straight line tangential to the anterior femoral cortex (yellow line) on the true lateral view. The floor of the trochlea can be flush with this line (translation = 0), anterior to this line (positive translation) or posterior to this line (negative translation) (Fig. 3). A normal value is < 3 mm. The trochlear bump has proven useful for the diagnosis of trochlear dysplasia, particularly when it is steep (trochlear spur).
Fig. 3.
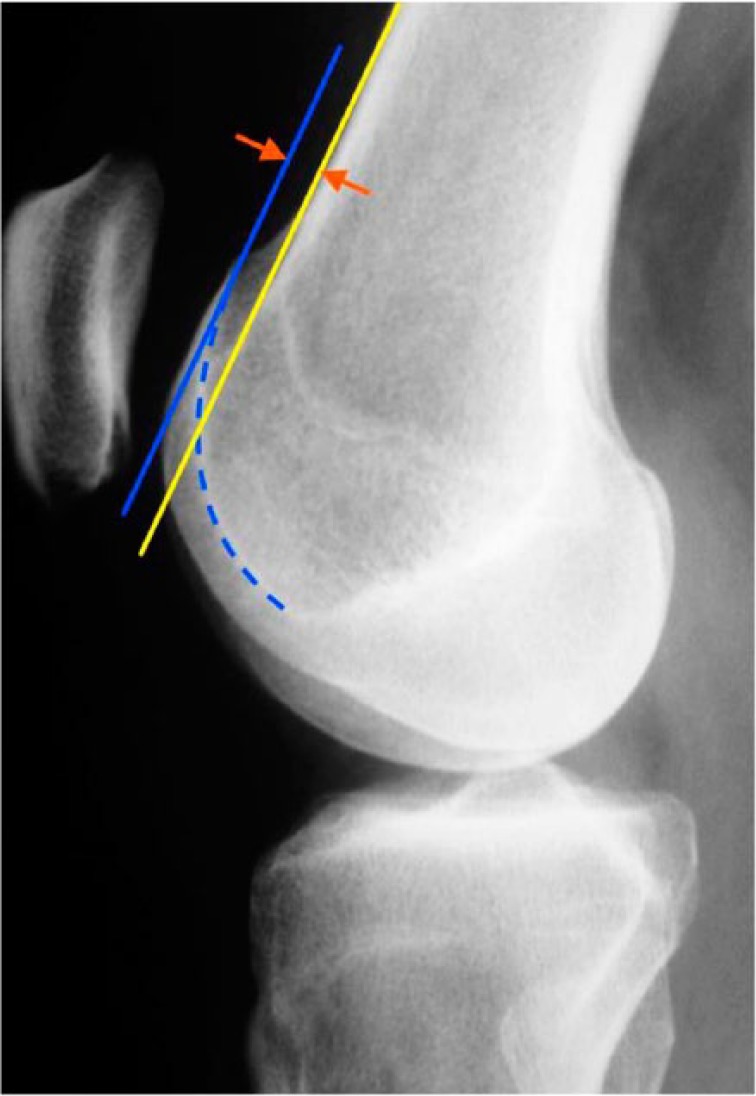
Lateral view radiograph showing the trochlear bump. The yellow line is a straight line tangential to the anterior femoral cortex. The floor of the trochlea (blue line) is anterior to this line, indicating a positive trochlear bump.
Trochlear depth
The measurement is performed on a true lateral view on a radiograph. A tangent to the posterior femoral cortex and a perpendicular line at the most proximal part of the posterior condyles is drawn. A line subtended 15° from the perpendicular line is then used to measure the trochlea depth (Fig. 4).3 The trochlea depth is a useful diagnostic tool for trochlear dysplasia and for predicting future risk of patellar dislocation. Theoretically, a shallow trochlea might increase the contact pressure in the patellofemoral joint, a condition already known as trochlear dysplasia.4 The increased contact pressure will elevate the stress in the subchondral bone of the patellofemoral joint, which is hypothesized to be a cause of patellofemoral pain.6 The role of trochlea depth in planning treatment is uncertain and the surgical procedures do not depend on this value.
Fig. 4.
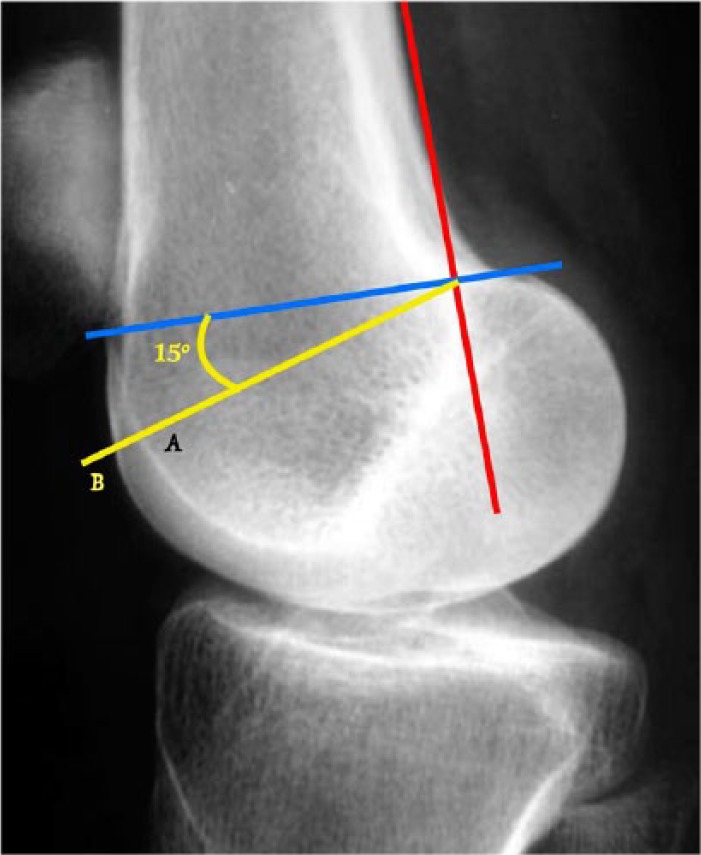
The trochlear depth measurement is performed on a true lateral radiograph view. A tangent to the posterior femoral cortex (red line) and a perpendicular line at the most proximal part of the posterior condyles (blue line) are drawn. A (yellow) line subtended 15° from the perpendicular line is now used to measure the trochlea depth (AB length).
Lateral trochlear inclination
To analyse the proximal portion of the trochlea, an area prone to dysplasia, the lateral trochlear inclination (LTI) is measured on the first cranio-caudal image that demonstrates the cartilaginous trochlea on MRI. LTI is calculated by means of a line tangential to the subchondral bone of the posterior aspect of the two femoral condyles crossed by a line tangential to the subchondral bone of the lateral trochlear facet.7 The mean value of the lateral trochlear inclination is reported to be 16.9° in knees without trochlear dysplasia. Using a diagnostic threshold of 11°, the measure has shown a sensitivity of 93% and a specificity of 87% for trochlear dysplasia.7
Other measurements have been described on radiography for many years, such as the trochlear angle, the patellar tilt and the patellar subluxation. Their roles in surgical management or in the prediction of patellofemoral pain are very uncertain.
Classification
A classification of trochlear dysplasia was described by Dejour et al in 1998, defining four types of trochlear dysplasia identified on lateral radiography and sectional imaging.8,9 Two new radiographic signs were also added to the previously described crossing sign: the ‘supratrochlear spur’, which represents a global prominence of the trochlea and acts like a ‘ski jump’ pushing the patella off the lateral facet when the knee flexes; and the ‘double contour’ sign, which is the radiographic line ending below the crossing sign and represents the chondral outline of the hypoplastic medial facet on the lateral view. The presence of a supratrochlear spur is characteristic of high-grade trochlear dysplasia. Trochlear dysplasia was classified (Fig. 5) into four types of dysplasia.
Fig. 5.
D. Dejour’s classification for the trochlear dysplasia: type A with an isolated crossing sign, type B with a crossing sign and a supratrochlear spur (flat or convex trochlea), type C with a crossing sign and a double contour (asymmetry of trochlear facets with a hypoplastic medial condyle) and type D with a crossing sign, a supratrochlear spur and a double contour (asymmetry of trochlear facets plus vertical join and cliff pattern). CT scan (or MRI) slices and lateral radiological view are both necessary in this classification.
Type A is characterized by the presence of a crossing sign in the lateral view, a shallow trochlea, and a sulcus angle > 145° on the axial view (fairly shallow trochlea).
Type B is characterized by a crossing sign and supratrochlear spur on lateral radiographs (flat or convex trochlea).
Type C is characterized by a crossing sign and a double contour sign (asymmetry of trochlear facets with a hypoplastic medial condyle) on the lateral view.
Type D is characterized by crossing sign, supratrochlear spur and double contour sign (asymmetry of trochlear facets plus vertical join and cliff pattern). This classification is useful for surgical management10. The definition of high-grade trochlear dysplasia is imprecise and has not been universally agreed upon. Both quantitative measurements and radiographic classifications are used. Many authors consider a high-grade trochlear dysplasia to be like a type B or D trochlear dysplasia including a supratrochlear spur of Dejour’s classification.
Treatment
Many surgical techniques have been described for the treatment of patellar dislocation.
Indications
High-grade trochlear dysplasia is characterized by the combination of a flat and/or prominent trochlea proud of the anterior femoral cortex, which does not allow the patella to engage the trochlea grove at approximately 25° of flexion.
The aim of trochleoplasty is to create a recentralized groove, correcting the trochlear depth abnormality and thus stabilizing the patella by a better entrance of the patella into the trochlear groove. Trochleoplasty can be proposed as a primary procedure for primary trochlear dysplasia or as a salvage procedure in case of failure after previous patellar alignment surgery.
As a primary intention, the trochleoplasty is indicated for a symptomatic patient with recurrent patellar instability, which has failed non-operative management. The trochleoplasties performed for trochlear dysplasia type B or D have better outcomes than for trochlear dysplasia without supratrochlear spur, regarding pain, Kujala score, sports activity and satisfaction.10 Dejour type C trochlear dysplasia may warrant a lateral facet elevation, proximal recession wedge trochleoplasty or groove-deepening trochleoplasty.11
Some authors recommend performing both trochleoplasty and MPFL reconstruction in all dysplastic knees12,13 associated with another procedure according to the anatomical abnormalities.
Surgical techniques
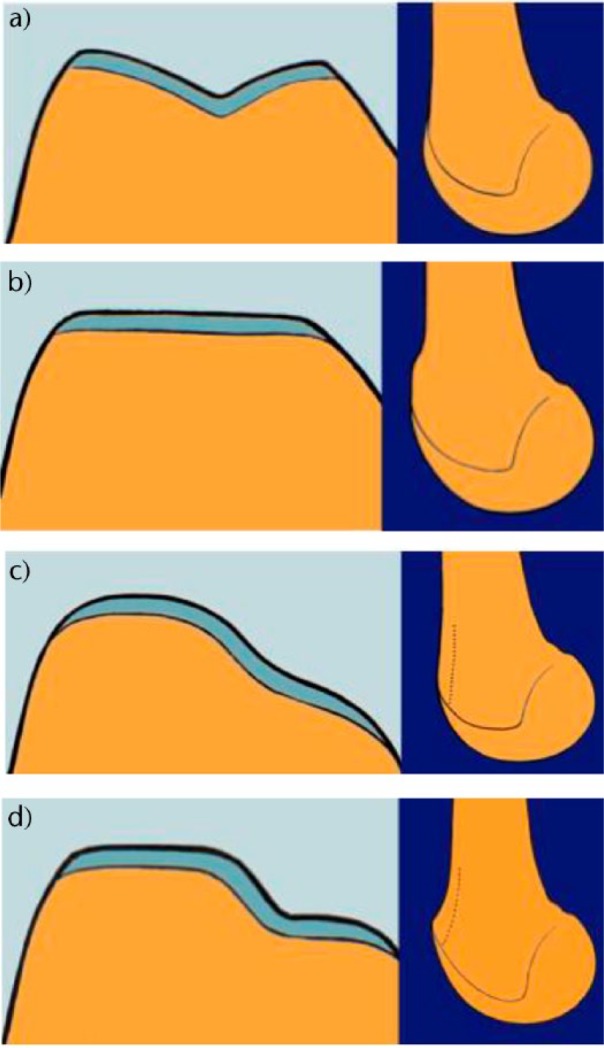
Several surgical techniques of trochleoplasty have been described to correct the trochlear anatomy.
Albee described the first trochleoplasty with elevation of the lateral trochlea facet.14 This addressed a flat trochlea by increasing the trochlear prominence. Kuroda et al15 have demonstrated that the Albee osteotomy significantly elevated average patellofemoral contact pressure (40% increased at 45° knee flexion with 10 mm lateral trochlear elevation), leading to secondary OA. Recently, another study reported the outcomes of 19 Albee osteotomies with a minimum of 12 years of follow-up.16 They confirmed the poor results of this technique, with 32% of persistent patellar instability and 21% of recurrent dislocations, 53% of patellofemoral OA grade 1 of Iwano’s classification and 27% of grade 2.
In 1966, Masse introduced the deepening trochleoplasty.17 He suggested the removal of subchondral bone and impaction of the articular cartilage with a punch to recreate a central sulcus. Henri Dejour modified this surgery with an osteotomy of both femoral condyles to create a V-shaped trochlear groove.9 Von Knoch et al18 described the results of another technique, known as ‘the Bereiter technique’, in which an osteochondral flap is raised from the trochlea and a bony sulcus is fashioned using burs. Deepening trochleoplasty, by whichever method is used, is logical because it reduces the flatness and the prominence and tries to restore a normal anatomy. Nevertheless, these surgical procedures are very demanding.
The third type of trochleoplasty has been described by Goutallier et al.19 This ‘recession’ type trochleoplasty consists of a recession of the prominent dome-shaped anterior surface of the distal femur to the level of the anterior femoral cortex without deepening the groove itself. The aim is not to fashion a groove but to reduce the prominent bump without modifying the patellofemoral congruence. This procedure is technically less demanding than a deepening trochleoplasty.
Deepening trochleoplasty
This technique was developed in Lyon. Arthrotomy is performed through a midvastus medial approach. The patella is translated laterally. The new trochlear sulcus is then drawn starting from the top of the intercondylar notch and directed proximally with 3° to 6° of valgus. To access the under surface of the trochlea, a thin strip of cortical bone is removed from the osteochondral edge. Cancellous bone is removed from the undersurface of the trochlea. A drill with a depth guide of 5 mm is used to ensure uniform thickness of the osteochondral flap; this maintains an adequate amount of bone beneath the trochlear articular cartilage. The shell produced must be thin enough to be modelled without sustaining a fracture. More bone is removed from the central portion at the location of the new sulcus. The groove and sometimes the medial and lateral margin must be osteotomized. The osteochondral flap is then replaced and moulded by gentle tapping with a punch. The new trochlea is then fixed with two small staples or anchors, one in each side of the groove. One arm is fixed in the upper part of the trochlear cartilage, the other one in the anterior femoral cortex. The staple is sunk deep to the superior surface of the cartilage. Absorbable screws are an alternative.
‘Bereiter technique’
The femoral trochlea is exposed through a lateral parapatellar arthrotomy with retraction of the patella medially to facilitate exposure of the femoral trochlea. The articular cartilage is separated from the synovium. An osteochondral flap is raised from the trochlea, extending to the intercondylar notch using different curved osteotomes. The subchondral groove is then deepened using osteotomes and a high-speed burr. Because the trochlea is typically medialized in patients with trochlear dysplasia, the aim is to create a recentralized groove. The osteochondral flap is then pressed into the newly formed groove and fixed with two transosseous 3-mm Vicryl bands. The synovium is reattached to the margins of the articular cartilage with an absorbable suture and closure of the lateral retinaculum is performed.
Recession-wedge trochleoplasty
A lateral approach is usually performed, with an incision just lateral to the patella, extending from the superior pole of the patella to beyond the tibial tubercle onto the anterior ridge of the tibia. The size of the wedge to be excised and the angle to be corrected are guided by preoperative imaging and measured intra-operatively. Using a saw, the antero-posterior cut is performed first, 5 mm above the trochlea. Then the posterior cut is made, parallel to the frontal plane of the femur, from the lateral side, and directed medially. The distal extent of the osteotomy should be approximately 5 mm away from the sulcus terminalis in order to give an optimal distal osteochondral hinge and to allow closing the wedge easily. Then, the anterior oblique osteotomy completes the bone cuts linking the first two cuts. The proximally based bone wedge is then removed and correction is achieved by progressively applying sustained gentle digital pressure on the trochlea, without modifying the trochlear groove. The correction is secured using 3.5 mm cancellous screws, positioned just laterally to the cartilage surface. This technique is indicated when there is an abnormal bump with anterior knee pain. It does not change the shape of the articular surface but it reduces the bump.
Outcomes
The aims of the trochleoplasty are to restore the anatomical shape of the trochlea in order to avoid instability, recurrent pain and long-term patellofemoral OA. Several studies reported clinical results after deepening trochleoplasty, but the number of patients is often small and the long-term follow-up is not available.
Clinical outcomes
The different studies report a postoperative improvement in clinical scores in the short term, with a low rate of recurrence of instability.20,21 However, it is not possible to assess the impact of trochleoplasty by patellofemoral stability, because it is rarely solely performed and other abnormalities are corrected as part of the surgical procedure. As a result of this, there is a lack of high-level studies reported in the literature. The different studies are very variable depending on the surgical technique, on the inclusion and exclusion criteria, and thus on the severity of the trochlear dysplasia. A recent systematic review, which described the outcomes of trochleoplasty in 25 clinical outcome studies, reported that before trochleoplasty, a positive apprehension test was found in 100% of patients and postoperatively a positive apprehension test was found in 20%. After surgery, the dislocation rate was 2% and the rate of subluxation was 6% at a mean follow-up of 54 months.20
A recent systematic review,22 reporting the outcomes of 14 studies on trochleoplasty, described a significant improvement of the Kujala score after surgery, with the overall mean value of preoperative and postoperative Kujala score being 53.8 (sd 22.2) and 74 (sd 6.3) points, respectively. The H. Dejour V-shaped trochleoplasty procedure showed a mean preoperative Kujala score of 54 (sd 5.6) and a mean postoperative Kujala score of 79.3 (sd 8.4). The Bereiter U-shaped deepening trochleoplasty had a mean preoperative and postoperative value of 53.8 (sd 29.1) and 64.5 (sd 4.9) points, respectively.
The study by Verdonk et al did not find that the severity of dysplasia or the type of instability influenced the final functional score.23
Deepening trochleoplasty
In one of a few long-term studies, Rouanet et al reported the outcomes of 34 patients at a mean follow-up of 15 years after sulcus deepening trochleoplasty.24 Seventeen anterior tibial tubercle transfers were associated with the trochleoplasty. Seven patients (20%) were considered failures. Six underwent revision arthroplasty (three total knee arthroplasties and three patellofemoral arthroplasties) which were performed at two years, five years, eight years, 12 years and 16 years postoperatively. One patient underwent revision surgery by anterior tibial tubercle transfer due to pain at three years. None of the patients presented with recurrent patellofemoral dislocation. All functional scores were significantly improved. Functional scores were significantly better in patients operated on for high-grade trochlear dysplasia (grades B and D in the Dejour classification) and in patients with objective instability. Among the 27 patients without revision, 22 (81%) were satisfied or very satisfied. The apprehension test was negative in 24 cases (89%). Ten patients reported occasional instability (37%). Eighteen patients (66%) did not report any pain or only occasional pain.
McNamara reported that 67% of patients returned to sports after deepening trochleoplasty at a mean time of 24 weeks compared with 40% of patients who practised sports preoperatively.25
‘Bereiter trochleoplasty’
The clinical outcomes after a Bereiter trochleoplasty are encouraging, in particular in terms of clinical scores and patient satisfaction;10,26 nevertheless, some patellar instability can occur again.
Recently Nelitz et al described the outcomes of 28 patients operated on with ‘Bereiter trochleoplasty’ associated with MPFL reconstruction.12 At a mean follow-up of 2.5 years, they reported no recurrent dislocation; 79% of patients were satisfied or very satisfied; only one patient (4%) was still apprehensive and 16 patients (57%) returned to sports at the preoperative level. The median Kujala score improved significantly from 79 (range 21 to 100) preoperatively to 96 (range 74 to 100) at the last follow-up. The median IKDC score improved significantly from 74 (range 32 to 95) preoperatively to 90 (range 65 to 98) at the last follow-up. These good outcomes are probably a result of the association of trochleoplasty and MPFL reconstruction.
In the long term, Metcalfe et al27 described the clinical and radiological outcomes of 199 cases operated with ‘Bereiter trochleoplasty’ at a mean follow-up of 4.4 years, of whom 29 patients were followed for more than eight years (mean follow-up of 8.9 years). They reported that 88% of 199 cases were satisfied with the operation and 90% had improved symptoms. Nevertheless, 8% of patients reported further dislocation of the patella after surgery and needed another surgical procedure to improve the patellar stabilization.
Recession wedge trochleoplasty
Goutallier19 reported a case series with 67% of patients reporting that they were satisfied or very satisfied with the outcome of surgery in 12 cases. In the Thaunat and Beaufils series reporting on 17 patients,28 the operation failed to stabilize the patellofemoral joint in only two cases. The average objective knee score at last follow-up was 80 (sd 17) for the Kujala score, 70 (sd 18) for the KOOS and 67 (sd 17) for the IKDC. The majority of studies have also reported a high rate (80% to 100%) of slight pain after trochleoplasty, in particular for the patients operated for pain-free instability.29
The short-term results of recession wedge trochleoplasty (34 months) were identical to those of sulcus deepening trochleoplasty, but the procedure is technically much simpler.28
Radiological outcomes
Radiological signs of trochlear dysplasia
Both deepening and recession trochleoplasty are able to reduce the trochlea bump. On a series of 20 recession wedge trochleoplasties,28 the trochlear groove height changed from an average of 4.8 mm preoperatively to an average of -0.8 mm postoperatively. Patellar tilt changed from an average of 14° (6° to 26°) preoperatively to an average of 6° (range -1° to 24°). There was no significant difference in the correction of the patellar tilt angle when comparing the groups who had or did not have the addition of a MPFL reconstruction. Most authors had similar results with correction of the crossing sign, the prominence, the depth of the trochlear groove and of patellar tilt, confirming that sulcus deepening trochleoplasty does create a good track for the patella.18,24,30 Sulcus deepening trochleoplasty often requires additional procedures during the same operation to optimize patellar tracking.
Osteoarthritis
Although the deepening or recession trochleoplasty is effective in reducing anterior knee pain, it does not halt the progression of patellofemoral arthritis, although the follow-up of the above studies is too short to draw any definitive conclusions.
In the Rouanet study, the percentage of knees with an Iwano score ⩾ 2 changed from 0% preoperatively to 65% at a mean follow-up of 15 years after a sulcus deepening trochleoplasty, although 23 knees (68%) had no tibiofemoral OA according to the Kellgren and Lawrence classification at the final follow-up.24
After ‘Bereiter trochleoplasty,’ a study of 132 knees described a rate of patellofemoral OA of 5.3% at a mean follow-up of 3.7 years and of 7.7% at five-year follow-up.27
From Mulford et al,31 there was no proof that surgical stabilization of the patellofemoral joint results in a long-term decrease in the development of OA. The development of OA may be associated with patellofemoral incongruence caused by the sulcus deepening trochleoplasty itself. Indeed, a flat and dysplastic patella tracks in a newly deepened trochlear groove. Recession trochleoplasty may reduce the risk of OA because it respects patellofemoral congruence, but the long-term results should be evaluated.
Complications
Trochleoplasty is a very demanding surgical procedure, which can present several complications.
Longo et al, in a systematic review, described 157 complications (40% of the treated knees) in 392 knees operated on with trochleoplasty (Bereiter technique and sulcus deepening technique mainly), including increased pain (11%) without difference between the surgical techniques, reduction in range of motion (6.7%; 2% with the Bereiter technique and 16% with the sulcus deepening trochleoplasty), OA (12%; 4.4% with Bereiter trochleoplasty, 16% with Goutallier trochleoplasty and 26.5% with sulcus deepening trochleoplasty).22
Chondral lesions
The main complication of these procedures concerns the viability of the trochlear cartilage. Indeed, the risks after a deepening trochleoplasty are breaking of the osteochondral flap, distal detachment of this flap and a too-thin flap, decreasing its blood supply, resulting in osteochondral necrosis. These complications are very uncommon with a recession wedge trochleoplasty. For older patients with less pliable cartilage and a risk of osteochondral fracture, the recession trochleoplasty is safer. Nevertheless, very few cases have been described. Metcalfe et al described one case of a partial detachment of the cartilage flap, which occurred while playing football six weeks after a ‘Bereiter trochleoplasty’.27 Schöttle et al32 studied the cartilage viability after Bereiter trochleoplasty and reported that the tissue in the trochlear groove remained viable.
Stiffness
Postoperative stiffness is a common complication, which sometimes needs a revision with arthrolysis. Its rate is in the range of 2% to 46% according to the surgical technique and to the study.17-19,23,24,28,30,33 This complication seems to occur a little more frequently with deepening trochleoplasty compared with recession wedge trochleoplasty. However, the comparisons between different studies are difficult due to the different populations.
Failures with patellar instability
A recent systematic review reported 2% of patellar re-dislocations out of 392 knees operated on by trochleoplasty.22 In particular, the procedure that showed the highest rate was the Goutallier trochleoplasty with a rate of 10.5%,28 followed by Dejour34 and Bereiter 10,33 trochleoplasty with rates of 3.2% and 0.8%, respectively.22
Re-operations
In the systematic review by Testa,20 a re-operation rate of 25% in the trochleoplasty group20 was found, including mainly arthrolysis, material removal, patellofemoral arthroplasties and chondral procedures. This rate is similar to the results in other studies. McNamara et al described a re-operation rate of 19% after deepening trochleoplasty, including mainly MPFL reconstructions and arthroscopic arthrolysis.25 Metcalfe et al reported a 14% rate of re-operation in 199 ‘Bereiter trochleoplasties’, with MPFL reconstructions and ATT transfer, mainly for patients with persistent patellar instability.27
Footnotes
ICMJE Conflict of interest statement: P. Neyret declares board membership of EFORT; consultancy and expert testimony for Latilini; royalties from Tornier; travel/accommodation/meetings expenses from Amplitude and Latilini, activities outside the submitted work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [DOI] [PubMed] [Google Scholar]
- 2. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med 2010;38:1997-2004. [DOI] [PubMed] [Google Scholar]
- 3. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26. [DOI] [PubMed] [Google Scholar]
- 4. Dejour H, Walch G, Neyret P, Adeleine P. [Dysplasia of the femoral trochlea]. Rev Chir Orthop Repar Appar Mot 1990;76:45-54. [PubMed] [Google Scholar]
- 5. Ntagiopoulos PG, Bonin N, Sonnery-Cottet B, Badet R, Dejour D. The incidence of trochlear dysplasia in anterior cruciate ligament tears. Int Orthop 2014;38:1269-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med 2002;30:447-56. [DOI] [PubMed] [Google Scholar]
- 7. Carrillon Y, Abidi H, Dejour D, et al. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology 2000;216:582-5. [DOI] [PubMed] [Google Scholar]
- 8. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev 2007;15:39-46. [DOI] [PubMed] [Google Scholar]
- 9. Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon’s procedure. Int Orthop 2010;34:311-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fucentese SF, Zingg PO, Schmitt J, et al. Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc 2011;19:1655-61. [DOI] [PubMed] [Google Scholar]
- 11. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg [Am] 2016;98-A:417-27. [DOI] [PubMed] [Google Scholar]
- 12. Nelitz M, Dreyhaupt J, Lippacher S. Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med 2013;41:1005-12. [DOI] [PubMed] [Google Scholar]
- 13. Banke IJ, Kohn LM, Meidinger G, et al. Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc 2014;22:2591-8. [DOI] [PubMed] [Google Scholar]
- 14. Albee FH. The bone graft wedge in the treatment of habitual dislocation of the patella. Med Rec 1915;88:257-9. [Google Scholar]
- 15. Kuroda R, Kambic H, Valdevit A, Andrish J. Distribution of patellofemoral joint pressures after femoral trochlear osteotomy. Knee Surg Sports Traumatol Arthrosc 2002;10:33-7. [DOI] [PubMed] [Google Scholar]
- 16. Tigchelaar S, van Sambeeck J, Koeter S, van Kampen A. A stand-alone lateral condyle-elevating trochlear osteotomy leads to high residual instability but no excessive increase in patellofemoral osteoarthritis at 12-year follow-up. Knee Surg Sports Traumatol Arthrosc 2017. https://doi.org/10.1007/s00167-017-4602-y. [DOI] [PMC free article] [PubMed]
- 17. Masse Y. [Trochleoplasty. Restoration of the intercondylar groove in subluxations and dislocations of the patella]. Rev Chir Orthop Repar Appar Mot 1978;64:3-17. [PubMed] [Google Scholar]
- 18. vonKnoch F Böhm T Bürgi ML von Knoch M Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg [Br] 2006;88-B:1331-5. [DOI] [PubMed] [Google Scholar]
- 19. Goutallier D, Raou D, Van Driessche S. [Retro-trochlear wedge reduction trochleoplasty for the treatment of painful patella syndrome with protruding trochleae. Technical note and early results]. Rev Chir Orthop Repar Appar Mot 2002;88:678-85. [PubMed] [Google Scholar]
- 20. Testa EA, Camathias C, Amsler F, et al. Surgical treatment of patellofemoral instability using trochleoplasty or MPFL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 2017;25:2309-20. [DOI] [PubMed] [Google Scholar]
- 21. Balcarek P, Rehn S, Howells NR, et al. Results of medial patellofemoral ligament reconstruction compared with trochleoplasty plus individual extensor apparatus balancing in patellar instability caused by severe trochlear dysplasia: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2017;25:3869-77. [DOI] [PubMed] [Google Scholar]
- 22. Longo UG, Vincenzo C, Mannering N, et al. Trochleoplasty techniques provide good clinical results in patients with trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 2017. https://doi.org/10.1007/s00167-017-4584-9. [DOI] [PubMed]
- 23. Verdonk R, Jansegers E, Stuyts B. Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc 2005;13:529-33. [DOI] [PubMed] [Google Scholar]
- 24. Rouanet T, Gougeon F, Fayard JM, et al. Sulcus deepening trochleoplasty for patellofemoral instability: A series of 34 cases after 15 years postoperative follow-up. Orthop Traumatol Surg Res 2015;101:443-7. [DOI] [PubMed] [Google Scholar]
- 25. McNamara I, Bua N, Smith TO, Ali K, Donell ST. Deepening trochleoplasty with a thick osteochondral flap for patellar instability: clinical and functional outcomes at a mean 6-year follow-up. Am J Sports Med 2015;43:2706-13. [DOI] [PubMed] [Google Scholar]
- 26. Ryzek DF, Schöttle P. Patellofemoral dysfunction in sports trochleoplasty: indications and techniques. J Knee Surg 2015;28:297-302. [DOI] [PubMed] [Google Scholar]
- 27. Metcalfe AJ, Clark DA, Kemp MA, Eldridge JD. Trochleoplasty with a flexible osteochondral flap: results from an 11-year series of 214 cases. Bone Joint J 2017;99-B:344-50. [DOI] [PubMed] [Google Scholar]
- 28. Thaunat M, Bessiere C, Pujol N, Boisrenoult P, Beaufils P. Recession wedge trochleoplasty as an additional procedure in the surgical treatment of patellar instability with major trochlear dysplasia: early results. Orthop Traumatol Surg Res 2011;97:833-45. [DOI] [PubMed] [Google Scholar]
- 29. Beaufils P, Thaunat M, Pujol N, et al. Trochleoplasty in major trochlear dysplasia: current concepts. Sports Med Arthrosc Rehabil Ther Technol 2012;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Donell ST, Joseph G, Hing CB, Marshall TJ. Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee 2006;13:266-73. [DOI] [PubMed] [Google Scholar]
- 31. Mulford JS, Wakeley CJ, Eldridge JD. Assessment and management of chronic patellofemoral instability. J Bone Joint Surg [Br] 2007;89-B:709-16. [DOI] [PubMed] [Google Scholar]
- 32. Schöttle PB, Schell H, Duda G, Weiler A. Cartilage viability after trochleoplasty. Knee Surg Sports Traumatol Arthrosc 2007;15:161-7. [DOI] [PubMed] [Google Scholar]
- 33. Utting MR, Mulford JS, Eldridge JD. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg [Br] 2008;90-B:180-5. [DOI] [PubMed] [Google Scholar]
- 34. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc 2014;22:2491-8. [DOI] [PubMed] [Google Scholar]