Abstract
Medial column (deltoid ligament) integrity is of key importance when considering the stability of isolated lateral malleolus ankle fractures.
Weight-bearing radiographs are the best method of evaluating stability of isolated distal fibula fractures.
Computed tomography (CT) scanning is mandatory for the assessment of complex ankle fractures, especially those involving the posterior malleolus.
Most isolated trans-syndesmotic fibular fractures (Weber-B, SER, AO 44-B) are stable and can safely be treated non-operatively.
Posterior malleolus fractures, regardless of size, should be considered for surgical fixation to restore stability, reduce the need for syndesmosis fixation, and improve contact pressure distribution.
Cite this article: EFORT Open Rev 2018;3 DOI: 10.1302/2058-5241.3.170057
Keywords: stability, ankle fractures, treatment, posterior malleolus
Introduction
Management of ankle fractures has evolved over the last 10 years. As scientific (laboratory, cadaveric and clinical) research has led to better understanding of the biomechanics and patho-anatomy of the ankle, this has allowed more accurate evaluation of all elements and characteristics of injuries to bone and soft tissues associated with malleolar fractures. As such, it has become apparent that the ‘key issue’ in achieving good outcomes when treating these common injuries is to follow the principle of restoring the stability and alignment of the fractured ankle, using either non-operative or operative treatment, as appropriate.1,2 The orthopaedic and trauma community needs to move away from the almost anecdotal ‘principles’ suggesting, for example, that 2 mm displacement of a distal fibula fracture requires surgical reduction and fixation, or that posterior malleolus fractures affecting less than 25% of the tibial plafond can be treated non-operatively. To illustrate, the second of these statements is based on an article published in 1940 reviewing only eight ankle fractures involving the posterior malleolus.1,3 Internal fixation can lead to surgical complications in up to 20% of cases4,5 and is therefore best avoided for those fractures where non-operative management can offer optimal outcomes. However, more complex injuries, such as those involving the posterior structures, require in-depth knowledge of the fracture pattern and careful evaluation and planning of any surgery.2
This review will analyse the principles of stability assessment for ankle fractures and provide a rationale for diagnosis and management.
Applied anatomy, biomechanics, and classifications
The ankle joint can be considered as a ‘ring’ in which bones and ligaments contribute to the overall stability. If this ‘ring’ is broken at one site only, it remains stable, but if it is broken at two or more sites, it becomes unstable. The ankle is also divided into two columns: lateral and medial. The lateral column consists of the fibula, the syndesmosis and the lateral ligaments. The syndesmosis between the fibula and tibia is formed by the anterior and posterior inferior tibiofibular ligaments (AITFL and PITFL) and the interosseus ligament, which is the lower part of the interosseus membrane. The lateral ligaments are the anterior talofibular (ATFL), calcaneofibular (CFL) and posterior talofibular (PTFL) and these connect the lateral malleolus to the talus. The medial column consists of the medial malleolus and the medial collateral ligament, known as the deltoid ligament, which is stronger than its lateral counterpart. It consists of superficial and deep components. Furthermore, the deep deltoid consists of two parts: the anterior and posterior talotibial ligaments (ATTL and PTTL). The posterior component is the stronger of the two. It originates from the posterior part of the medial malleolus and inserts into the posteromedial talus, plantar to its articular surface. It is important to note that this ligament is tight when the foot is plantigrade, and loose with the foot plantar-flexed. Thus, it is tight when the foot bears weight. It is these deep fibres of the deltoid ligament that play a key role in the stability of ankle fractures, especially if the PTTL remains intact following an injury.6,7
In the past, lateral column integrity was thought to be the key to a well-fixed and stable ankle fracture. Since 1997, however, it has been recognized that it is probably medial column (medial malleolus and deltoid ligament) integrity that is more important.1,2,7–11
Ankle injuries result in fractures or equivalent ligamentous damage. An ankle fracture occurs when an external rotation, adduction or abduction force is applied to a foot that is fixed on the ground in supination (70%) or pronation (30%). Although these injuries are described as if the talus rotates in relation to the tibia, it is of course the tibia that rotates in relation to the foot. Less commonly, the foot may move relative to a fixed tibia. In inversion injuries (supination or adduction), initial tension is on the lateral side. This will result either in a fracture of the lateral malleolus or rupture of the lateral ligaments, and the forces may then continue to affect posterior and then medial structures. In eversion ankle injuries (pronation or abduction) the forces will result first in fracture of the medial malleolus or a deltoid ligament rupture. Higher-energy injuries may further damage lateral and then posterior structures, bony or ligamentous.
Many classifications have been proposed to describe these fractures, based either on the anatomy of the fracture or the mechanism of injury. The Danis-Weber (1966) classification is still widely used, probably because it is simple. It is based on the level of the fibular fracture in relation to the distal tibiofibular syndesmosis, distinguishing between types A, B, C where the fracture is below, at, or above the syndesmosis. It was developed on the basis that the lateral column plays the major role in the treatment of ankle fractures and that the higher the fibular fracture, the higher the chance of instability. Although the second is partially true, the classification does not describe the medial bony or ligamentous injuries which contribute to overall stability more than their lateral counterparts, and it cannot therefore differentiate between stable and unstable fractures.9 It also does not guide management.
The Lauge-Hansen classification (1950) is based on the mechanism of injury, with the first word describing the position of the foot and the second the direction of the force applied to the talus.12 According to this classification there are four basic types: supination external rotation (SER), supination adduction (SAD), pronation external rotation (PER) and pronation abduction (PAB) (Table 1). The advantage of the Lauge-Hansen classification is that it considers all the components of the injury, including those affecting posterior and medial structures. In a recent study by Warner et al., which correlated the intra-operative findings of 300 ankle fractures with magnetic resonance imaging (MRI) findings, this classification accurately predicted the ligamentous injuries in 94% of cases.13 In contrast, there are studies that have shown that this classification does not always predict the extent of bony injuries.14 To fairly appraise the Lauge-Hansen classification, one should probably say that it is old, not validated, and may fail to accurately describe and classify all fracture patterns. On the other hand, it is still useful because it makes us think about the fracture mechanism, predict ‘hidden’ injuries which may not be apparent on the initial set of standard non-weight-bearing radiographs taken in the emergency department and, possibly, it may guide management.
Table 1.
Classification systems of malleolar fractures
| Fibular fracture | Danis-Weber | Lauge-Hansen (stages) | AO/OTA |
|---|---|---|---|
| Infra- syndesmotic |
Type A |
Supination adduction (SAD)
1. Transverse fracture of lateral malleolus 2. Vertical fracture of medial malleolus |
44-A1 (isolated lateral) 44-A2 (lateral, medial) 44-A3 (lateral, medial, posterior) |
| Trans-syndesmotic | Type B |
Supination external rotation (SER)
1. Injury of AITFL 2. Low oblique/short spiral fracture of lateral malleolus 3. Injury of PITFL or fracture of posterior malleolus 4. Deltoid ligament injury or fracture of medial malleolus |
44-B1 (lateral) 44-B2 (lateral, medial) 44-B3 (lateral, medial, posterior) |
| Supra-syndesmotic | Type C |
Pronation external rotation (PER)
1. Deltoid ligament injury or fracture of medial malleolus 2. Injury of AITFL 3. High oblique/spiral fracture of distal fibula 4. Injury of PITFL or fracture of posterior malleolus Pronation abduction (PAB) 1. Deltoid ligament injury or fracture of medial malleolus 2. Injury of AITFL 3. Transverse or comminuted fracture of distal fibula |
44-C1 (simple diaphyseal) 44-C2 (multifragmentary) 44-C3 (proximal) |
Note. AITFL, anterior inferior tibiofibular ligament; AO, Arbeitsgemeinschaft für Osteosynthesefragen; OTA, ; PITFL, posterior inferior tibiofibular ligament
More recently the Arbeitsgemeinschaft für Osteosynthesefragen (AO) has comprehensively classified all fractures in the body according to a numerical system. According to this scheme, fractures affecting the malleoli are described as 44. They are subdivided into A, B, C with further subtypes 1, 2 and 3, combining features of the two previous classifications (Table 1). This classification system is not used in everyday practise, however, and it is probably more useful for documentation and research purposes.15
How can these classifications guide our treatment? A trans-syndesmotic fibular fracture, corresponding to type B according to the Weber classification, occurs more commonly when the foot is supinated and the body externally rotates (but the tibia internally rotates relative to talus). If the force stops on the lateral side then only two structures have been damaged: the AITFL and the lateral malleolus. These fractures are described as supination external rotation stage 2 (SER 2) and are considered stable injuries. If the rotational force on the foot continues, further sequential injuries involve the posterior malleolus or the PITFL (SER 3) and finally, injuries to either the medial malleolus or the deltoid ligament (SER 4), which are considered unstable injuries (Fig. 1).
Fig. 1.
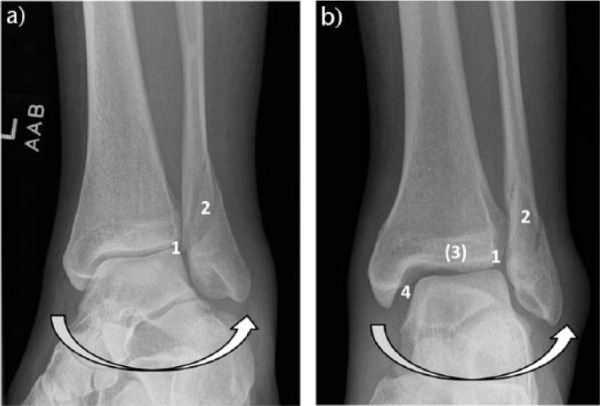
The foot is supinated while external rotation (arrow) causes injury to the anterior syndesmosis (1) and a trans-syndesmotic distal fibular fracture (2). This is classified as a SER 2 fracture. Higher-energy injuries can sequentially damage the posterior (3) and medial structures (4), which are classified as SER 3 and SER 4 injuries respectively. Injury to these structures can be either osseous or ligamentous (SER 3 either posterior malleolus or PITFL, and SER 4 either medial malleolus or deltoid).
When an external rotation force is applied on a pronated foot, the medial bony and ligamentous structures will be injured first. The external rotation force will then affect the lateral side and can disrupt the syndesmosis and the interosseus membrane, then cause a supra-syndesmotic fibular fracture and, finally, a posterior malleolus fracture or injury to the PITFL. So, when radiographs reveal a supra-syndesmotic (‘high fibula’) fracture, then, by definition, the medial malleolus is also fractured or the deltoid ligament is damaged and this indicates a more severe, unstable injury that usually requires operative management (Fig. 2). Lastly, a trans-syndesmotic fibular fracture can occur from an abduction force to the pronated foot (PAB), resulting in an irregular fracture pattern.
Fig. 2.

The foot is pronated while external rotation (arrow) causes injury to the deltoid ligament (a, 1) or the medial malleolus (b, 1). The rotational forces will then cause syndesmosis disruption (2) and a supra-syndesmotic distal fibula fracture (3). With further force, the posterior malleolus or the posterior ligamentous structures may be injured (4).
The current view is that bi- and trimalleolar fractures are most likely unstable, as the ‘ankle ring’ has broken in at least two places. Unstable injuries are usually the ones which result from PER, producing a type C high fibular fracture and SER 4 injuries. All current classifications have drawbacks but irrespective of which a surgeon uses, it is of key importance to identify all bony and ligamentous components of the injury and to understand their implications for the stability of the fracture.
Diagnosis
Clinical assessment
A patient with an ankle injury usually presents to the emergency department unable to bear full weight. Obtaining a history of the injury circumstances, including the mechanism, is helpful, if not essential. Initial clinical assessment includes any gross deformity, such as fracture-dislocation, the condition of soft tissues (closed or open fracture, swelling, blisters), the exclusion of other injuries and neurovascular examination of the leg. Clinical examination should be undertaken in a methodical sequence on both lateral and medial sides, taking into consideration the severity of pain. Tenderness is normally present in areas where different structures have been affected by the injury. Proximal fibula tenderness should be specifically tested for (Maisonneuve injury). Medial clinical signs such as tenderness, swelling and bruising should be documented, but they are not reliable predictors of instability, as previously thought.10,11 Medial pain and ecchymosis can result from injury only to the superficial component of the deltoid ligament, whilst the deep deltoid remains intact, providing overall stability to the ankle.7
In the presence of dislocation or subluxation of the ankle with skin compromise, documentation is mandatory along with the neurovascular status and, after appropriate analgesia has been administered, closed manipulation and reduction is indicated as soon as possible (most surgeons advocate immediate reduction, prior to taking radiographs) to reduce neurovascular damage. Furthermore, the past medical history and social history of the patient should be assessed. Comorbidities such as diabetes mellitus and peripheral vascular disease, as well as previous mobility, activities of daily living and social habits (e.g. smoking) should be documented, as they affect decision-making and are prognostic factors.16,17
Imaging
Plain radiographs, anteroposterior and lateral (non-weight-bearing) projections, are part of the initial evaluation. We need to emphasize that currently, these initial ‘standard anteroposterior and lateral radiographs’ are rarely sufficient for an accurate assessment of all components of the injury. Further mortise and/or oblique views of the ankle can be requested if in doubt, as well as radiographs of the knee and proximal tibia if proximal fibular tenderness is present during the clinical examination, and a Maisonneuve fracture is suspected.
In isolated trans-syndesmotic SER, Weber-B, 44-B injuries (according to the Lauge-Hansen, Danis-Weber and AO-classifications, respectively), one needs to evaluate integrity of the deltoid ligament in order to assess stability. This is achieved by measuring the ‘true’ medial clear space (MCS) – the distance between medial malleolus and medial talus with the foot in a neutral position and not plantarflexed. Otherwise, in plantarflexion, the narrowest part of the talus is projected and can be one of the reasons why the MCS may appear wider. When the deltoid ligament is ruptured, this space is increased and lateral talar shift occurs (Fig. 3). A medial clear space of > 4 mm is considered to be abnormal,7 although accuracy of this measurement is debatable according to a recent cadaveric study.18 Therefore, all isolated lateral malleolus SER fractures require appropriate dynamic testing, by obtaining weight-bearing (WB) anteroposterior radiographs of the ankle, approximately 5–7 days after the injury, so as to assess fracture stability and decide on further management.5,7,19 The use of WB radiographs is based on the anatomical features of the deltoid ligament as described earlier. Thus, the foot is placed plantigrade as this reduces the talus in the mortise if the posterior part of the deep deltoid ligament, the PTTL, is intact. Manual stress views have been used historically but, as they cannot be routinely and easily standardized and are not always well tolerated by the patient, their practicality has been questioned. Gravity stress views seem to have fallen out of favour as well, given that they tend to overestimate fracture instability, whilst WB radiographs have been shown to be more accurate (Fig. 3 and Fig. 4).5,20–22
Fig. 3.

Gravity stress view with widening of medial clear space.
Fig. 4.

Weight-bearing radiograph revealing talar shift and widening of the medial clear space.
In the literature, the proportion of isolated distal fibula SER type fractures that required surgical fixation, using WB radiographs for assessment, ranges from 3% to 10%.5,19,23 Given that partial-incomplete rupture of the deep deltoid ligament can provide adequate integrity of the medial column, thus providing stability when the foot is plantigrade, in SER fractures, the same concept could potentially be applied to isolated fibula PER fractures, if only the anterior part of the deep deltoid was involved initially in stage 1. Magnetic resonance imaging and/or ultrasound scanning are not routinely used for the assessment of ankle fractures but can be useful in detecting ligamentous injuries.24,25 The authors believe, however, that these imaging modalities are not useful in the acute setting, as their accuracy in detecting complete versus partial deltoid ligament ruptures is controversial. Furthermore, WB radiographs for isolated fibula fractures offer a dynamic and pragmatic evaluation of the stability of the fracture.19,20,26
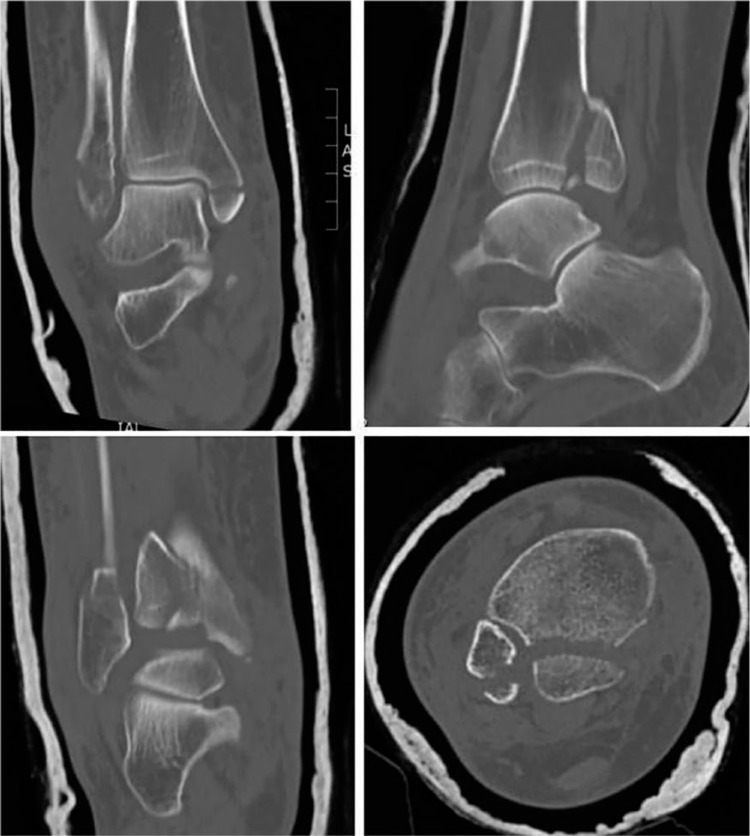
For more complex fractures, including fracture-dislocations and other high-energy injuries or, when a posterior malleolus fracture is suspected (such as in an SER 4 injury where there is no obvious osseous posterior – SER 3 – injury), or clearly detected on radiographs, a computed tomography (CT) scan of the distal tibia and hindfoot is mandatory. These fractures are usually unstable and require operative management. CT scanning is designed for assessing impaction, detecting all fracture components and to aid preoperative planning (Fig. 5).2 Although some centres in Europe and the United States advocate CT scanning of every ankle fracture, there is no evidence that it should be used routinely for simple fractures (e.g. isolated distal fibula fractures), provided that one can be certain that no posterior malleolus, or Maisonneuve fracture has been missed.
Fig. 5.
Trimalleolar fracture with computed tomography scan revealing details of the fracture pattern (loose intra-articular fragments) and allowing preoperative planning.
Treatment
The aim of treatment of ankle fractures is to reduce and hold the talus anatomically within the ankle mortise. Studies have shown that there is a significant increase in intra-articular contact stresses even with minimal residual displacement of the talus, leading to degenerative changes of the joint.27 The initial management of all ankle fractures involves immobilization in a splint – after reduction, if there is dislocation. Further decisions regarding definitive treatment, either conservative or surgical, depend on the stability of the fracture, as detected on the initial but also subsequent WB radiographs.
If the non-weight-bearing (NWB) AP or mortise radiograph shows no suspicion of widening of the medial clear space, and the weight-bearing X-ray also reveals no widening of the MCS, then this is an SER 2 fracture, which is stable and can be managed in a boot, splint (or cast if patient prefers) and weight bearing as tolerated (WBAT) should be the default instruction. If the presenting NWB views, however, do reveal widening of the MCS but the WB views do not, then this is an SER 4a injury, where the anterior deep deltoid ligament (DDL) is torn but the posterior DDL is not (or a significant proportion of it is still intact). Because the posterior DDL is tight when the ankle is neutral, and loose when plantarflexed, this fracture is potentially unstable if managed in a splint or boot. This is because, if in a removable device, the patient will remove it to bathe, sleep, and when at rest and so the ankle will often be allowed to plantarflex, meaning that the injured DDL will potentially heal “long”, resulting in later, chronic instability. Thus, this injury must be treated in a formal cast but again, WBAT should be the default instruction (even full weight bearing is allowed). If, however, the WB x-rays reveal widening of the MCS then, irrespective of the presenting emergency department NWB x-rays, this is an SER 4b fracture, which is definitely unstable (posterior DDL also torn), and therefore needs fixing. If a patient cannot bear weight at all (which is rare), then this must be treated as a potentially unstable fracture (Table 2).1,5,7,21,22,28–30
Table 2.
‘Surrey modification’ of Lauge-Hansen classification and treatment
| Fracture type | NWB X-ray | WB X-ray | Deep deltoid ligament ATTL & PTTL components |
Treatment |
|---|---|---|---|---|
| SER 2 | Stable | Stable | ATTL & PTTL intact | Boot/brace & WB |
| SER 4a | Unstable | Stable | PTTL fully or mostly intact | Cast & WB for 6 weeks |
| SER 4b | Unstable | Unstable | PTTL ruptured | ORIF |
Note. NWB, non-weight bearing; WB, weight bearing; ATTL, anterior tibiotalar ligament; PTTL, posterior tibiotalar ligament; ORIF: .
Surgical treatment involves open reduction and internal fixation, following the AO principles. Regarding the lateral malleolus, lag screw fixation with a neutralization 1/3 tubular plate is the most common technique. If the fracture pattern/obliquity of the fracture allows more than one lag screw a neutralization plate is not mandatory, and excellent results have been described in young patients, especially in long oblique fractures, avoiding complications related to prominent metalwork.31 Comminuted or transverse high-energy fibula fractures require stronger fixation with locking or reconstruction plates. Locking plates are also an option, as well as posterior plating of the fibula, when the configuration of the fracture allows it, and studies have shown improved stability on biomechanical testing in osteoporotic bone.32,33 The clinical results, however, for the use of locking plates in elderly patients have been less satisfactory, showing a higher infection rate when compared with the standard technique.34 This should be considered along with their higher cost. Intramedullary fixation of the fibula has also been described, especially for elderly patients with poor soft tissues, as producing satisfactory results.35
Fixation of the medial malleolus can be achieved using lag screws or a tension band wire technique (or smaller-gauge cortical screws, e.g. 2.7 mm) if the fragment is small. Two partially threaded cancellous screws are traditionally placed perpendicular to the fracture and parallel to each other. However, in good bone, fully threaded cortical screws, used in lag fashion, have been shown to be equal to, or superior to partially threaded cancellous lag screws.36 For comminuted medial malleolar fractures, smaller sized screws can and should be utilized. In vertical fractures of the medial malleolus, such as in those resulting from SAD type injuries, fixation is achieved using a buttress plate, or a plate with lag screws inserted through it, after reduction of the impacted medial plafond.
Assessment of the syndesmosis with an intraoperative hook test should follow fixation of the fractures. No consensus exists regarding the optimum method of stabilization of the syndesmosis. Small fragment screws (3.5 mm) or large fragment screws (4.5 mm), engaging three or four cortices, sometimes through a plate, as well as flexible suture devices, have been used (Fig. 6). No method has been shown to produce superior results compared with the others.37,38 Syndesmosis screw insertion should only be performed after the syndesmosis has been reduced (preferably open). A large (pelvic) clamp should be used, with the tines of the clamp positioned appropriately following normal anatomical relations, from the lateral fibular apex to the anterior half of the medial malleolus (from posterolateral fibula to anteromedial supramalleolar area), so as not to mal-reduce the fibula into the incisura. Care is taken not to over-compress the syndesmosis as the screw(s) needs to be in a position 2–3 cm above the joint line. The necessity of screw removal is debatable, as well as the appropriate time for removal. Many surgeons advocate leaving the screws in situ for at least 3 months, in order for the syndesmotic ligaments to heal adequately. The patient has to be warned that the screws might break. Other surgeons remove the screws at 6 weeks, and an increasing number of surgeons are leaving them in with the expectation that they break, but with no detriment to the patient or to function.39,40
Fig. 6.

Syndesmosis screw fixation.
The literature does not provide any high-quality evidence regarding the superiority/inferiority of the different options.41 The Tightrope™ (‘suture-button’) device is an alternative to screw fixation of the syndesmosis, but results are unproven. The theoretical advantage is that it does not require removal and allows some motion at the syndesmosis, thereby possibly allowing some degree of self-reduction if not accurately placed. However, it is more expensive, neither its tension nor stability is adjustable and its use has been associated with adverse reactions, pain and the need for removal. Generally, it has not been shown to offer superior results compared with ‘conventional’ screw fixation.42,43 Certainly, it should not be used where there is vertical instability, such as when a syndesmotic injury is associated with a multifragmented high Weber C-type/PER fibula fracture.44
We would like to draw readers’ attention to two issues related to syndesmosis screw fixation. Firstly, syndesmosis mal-reduction is more common than previously thought (up to 30% in some studies) if postoperative CT scanning is used for evaluation.45 Therefore, many surgeons advocate open (not percutaneous) reduction of the syndesmosis before fixation. Arthroscopic evaluation is an alternative, to ensure reduction of the fibula into the incisura. Secondly, fixation of the syndesmosis alone, especially in ‘high fibula’ fractures does not compensate for lack of accuracy in restoring fibula length and rotation. Thus, anatomical fixation of the fractures first is mandatory, and then the need for syndesmosis fixation should be assessed.
When the ankle injury involves a fracture of the posterior malleolus, this should be anatomically fixed in order to restore stability, after appropriate investigation with a CT scan.2,46. A recent systematic review showed that, according to published studies, surgeons most commonly perform surgical fixation of posterior malleolar fractures only when these exceed 25% of the articular surface of the tibial plafond.47 We mentioned earlier that this ‘principle’ is based on a study from the 1940s! In the last decade there have been a number of studies that have shown that internal fixation of posterior malleolus fractures stabilizes the syndesmosis more than syndesmotic screws or suture buttons, thus making syndesmotic fixation unnecessary, with intra-operative testing still being applicable.48,49 It also affects the clinical outcome as shown in studies using patient-related outcome measures.50,51 Recent evidence has also shown that the smaller the fragment, the more likely it is to affect syndesmotic stability.52 Thus, many posterior malleolus fractures require surgical fixation. Large ones are carried out to restore normal anatomy of the tibial plafond and small ones to help restore syndesmotic stability and to improve contact pressure distribution (Figs. 7–10).52 Operative treatment is better undertaken with the patient in the prone or recovery position.53 A posterolateral or posteromedial approach is utilized depending on the location of the posterior fracture, as identified on preoperative CT imaging. The fragment needs to be reduced and fixed with a small plate or screw(s). A posterior 1/3 tubular buttress plate can also be used to facilitate reduction. Extra care with the reduction should be taken in the presence of joint impaction or intercalary fragments. Furthermore, the lateral malleolus can be approached through the same incision if a posterolateral incision is used. For the majority of cases, the authors do not recommend fixing the posterior malleolus with anterior to posterior inserted screws. It is riskier to insert a screw from the anterior tibia due to the anterior neurovascular bundle; mal-reductions are common and biomechanically it is not logical to fix the tibia into the smaller fragment.
Fig. 7.
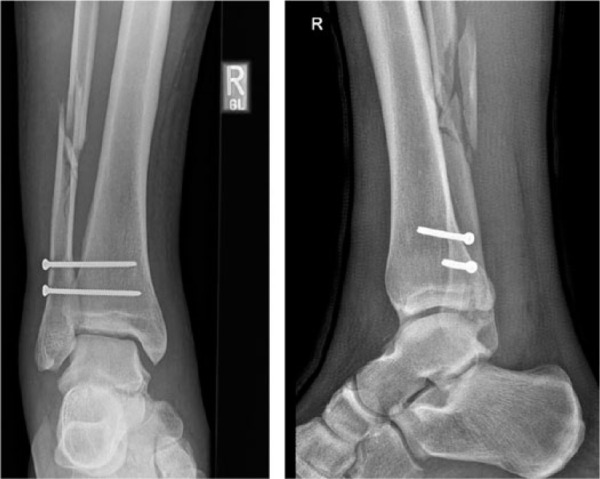
28-year-old male soldier sustained a high-energy injury and was treated with syndesmosis screw fixation, only, at another institution. He came to us for follow-up at 3 weeks post surgery, in a lot of pain. It was felt that fibula length and rotation had not been restored. A CT scan was requested.
Fig. 10.

The patient made an uneventful recovery and resumed ordinary activities, including high-impact physical exercise, at 6 months.
Fig. 8.
The CT scan revealed intra-articular fragments and slight mal-reduction of the syndemsosis.
Fig. 9.
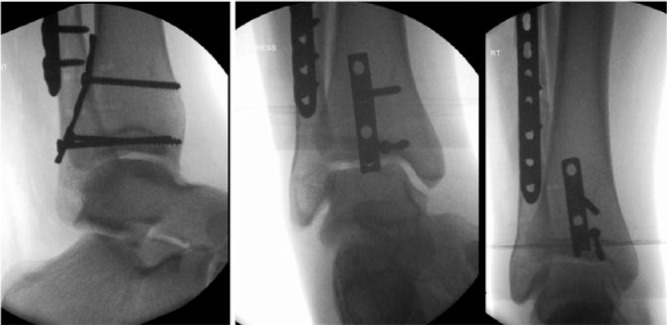
Revision surgery was undertaken. The posterior malleolus and fibula fractures were fixed through a posterolateral approach. Stress examination (middle view) revealed no syndesmosis instabililty, and no syndesmosis screws were needed.
Conclusions
The medial column, and especially the deep portion of the deltoid ligament with its anterior and posterior parts, has been recognized as being of key importance to the stability of ankle fractures, especially SER-type isolated lateral malleolus fractures. The lateral and posterior columns have a significant role as well, especially in PER-type injuries. Irrespective of what classification a surgeon uses, correct identification of all the osseo-ligamentous components of the injury is important in guiding treatment. If there is doubt regarding the stability of a fracture on the initial radiographs, as with isolated trans-syndesmotic fibular fractures (i.e. SER 2 versus ‘hidden’ deltoid SER 4), weight-bearing radiographs should be taken within a week. Fractures that are considered stable can safely be treated non-operatively. Fractures that are unstable will need open reduction and internal fixation and preoperative planning is essential. Computed tomography scanning of the ankle is mandatory, as part of this planning, in the presence or suspicion of a fracture of the posterior malleolus. Likewise, if there is impaction, or intercalary fragments are suspected. Fixation of the posterior fragment through a posterior approach should be undertaken as this can reduce the need for syndesmotic fixation.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Gougoulias N, Khanna A, Sakellariou A, Maffulli N. Supination-external rotation ankle fractures: stability a key issue. Clin Orthop Relat Res 2010;468:243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gougoulias N, Sakellariou A. Ankle fractures. In: Bentley G, ed. European surgical orthopaedics and traumatology: The EFORT textbook. Berlin: Springer, 2014:3735–3765. [Google Scholar]
- 3. Nelson MC, Jensen NK. The treatment of trimalleolar fractures of the ankle. Surg Gynecol Obstet 1940;71:509–514. [Google Scholar]
- 4. Redfern DJ, Sauvé PS, Sakellariou A. Investigation of incidence of superficial peroneal nerve injury following ankle fracture. Foot Ankle Int 2003;24:771–774. [DOI] [PubMed] [Google Scholar]
- 5. Dawe EJ, Shafafy R, Quayle J, Gougoulias N, Wee A, Sakellariou A. The effect of different methods of stability assessment on fixation rate and complications in supination external rotation (SER) 2/4 ankle fractures. Foot Ankle Surg 2015;21:86–90. [DOI] [PubMed] [Google Scholar]
- 6. Kelikian AS, Sarrafian SK. Sarrafian’s anatomy of the foot and ankle: descriptive, topographical, functional. Third ed. Philadelphia: JB Lippincott Williams & Wilkins, 2011. [Google Scholar]
- 7. Gougoulias N, Sakellariou A. When is a simple fracture of the lateral malleolus not so simple? How to assess stability, which ones to fix and the role of the deltoid ligament. Bone Joint J 2017;99-B:851–855. [DOI] [PubMed] [Google Scholar]
- 8. Michelson J, Solocoff D, Waldman B, Kendell K, Ahn U. Ankle fractures: the Lauge-Hansen classification revisited. Clin Orthop Relat Res 1997;345:198–205. [PubMed] [Google Scholar]
- 9. Michelson JD, Magid D, McHale K. Clinical utility of a stability-based ankle fracture classification system. J Orthop Trauma 2007;21:307–315. [DOI] [PubMed] [Google Scholar]
- 10. DeAngelis NA, Eskander MS, French BG. Does medial tenderness predict deep deltoid ligament incompetence in supination-external rotation type ankle fractures? J Orthop Trauma 2007;21:244–247. [DOI] [PubMed] [Google Scholar]
- 11. Egol KA, Amirtharajah M, Tejwani NC, Capla EL, Koval KJ. Ankle stress test for predicting the need for surgical fixation of isolated fibular fractures. J Bone Joint Surg Am 2004;86-A:2393–2398. [DOI] [PubMed] [Google Scholar]
- 12. Lauge-Hansen N. Fractures of the ankle. III. Genetic roentgenologic diagnosis of fractures of the ankle. Am J Roentgenol Radium Ther Nucl Med 1954;71:456–471. [PubMed] [Google Scholar]
- 13. Warner SJ, Garner MR, Hinds RM, Helfet DL, Lorich DG. Correlation between the Lauge-Hansen classification and ligament injuries in ankle fractures. J Orthop Trauma 2015;29:574–578. [DOI] [PubMed] [Google Scholar]
- 14. Haraguchi N, Armiger RS. A new interpretation of the mechanism of ankle fracture. J Bone Joint Surg Am 2009;91:821–829. [DOI] [PubMed] [Google Scholar]
- 15. AO Surgery reference. http://www.aofoundation.org (date last accessed 20 September 2017).
- 16. Costigan W, Thordarson DB, Debnath UK. Operative management of ankle fractures in patients with diabetes mellitus. Foot Ankle Int 2007;28:32–37. [DOI] [PubMed] [Google Scholar]
- 17. Nåsell H, Ottosson C, Törnqvist H, Lindé J, Ponzer S. The impact of smoking on complications after operatively treated ankle fractures: a follow-up study of 906 patients. J Orthop Trauma 2011;25:748–755. [DOI] [PubMed] [Google Scholar]
- 18. Metitiri O, Ghorbanhoseini M, Zurakowski D, Hochman MG, Nazarian A, Kwon JY. Accuracy and measurement error of the medial clear space of the ankle. Foot Ankle Int 2017;38:443–451. [DOI] [PubMed] [Google Scholar]
- 19. Weber M, Burmeister H, Flueckiger G, Krause FG. The use of weightbearing radiographs to assess the stability of supination-external rotation fractures of the ankle. Arch Orthop Trauma Surg 2010;130:693–698. [DOI] [PubMed] [Google Scholar]
- 20. Gill JB, Risko T, Raducan V, Grimes JS, Schutt RC., Jr Comparison of manual and gravity stress radiographs for the evaluation of supination-external rotation fibular fractures. J Bone Joint Surg Am 2007;89:994–999. [DOI] [PubMed] [Google Scholar]
- 21. Seidel A, Krause F, Weber M. Weightbearing vs gravity stress radiographs for stability evaluation of supination-external rotation fractures of the ankle. Foot Ankle Int 2017;38:736–744. [DOI] [PubMed] [Google Scholar]
- 22. Hastie GR, Akhtar S, Butt U, Baumann A, Barrie JL. Weightbearing radiographs facilitate functional treatment of ankle fractures of uncertain stability. J Foot Ankle Surg 2015;54:1042–1046. [DOI] [PubMed] [Google Scholar]
- 23. Hoshino CM, Nomoto EK, Norheim EP, Harris TG. Correlation of weightbearing radiographs and stability of stress positive ankle fractures. Foot Ankle Int 2012;33:92–98. [DOI] [PubMed] [Google Scholar]
- 24. Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: an MRI study. J Orthop Trauma 2006;20:267–272. [DOI] [PubMed] [Google Scholar]
- 25. Nortunen S, Lepojärvi S, Savola O, et al. Stability assessment of the ankle mortise in supination-external rotation-type ankle fractures: lack of additional diagnostic value of MRI. J Bone Joint Surg Am 2014;96:1855–1862. [DOI] [PubMed] [Google Scholar]
- 26. Schock HJ, Pinzur M, Manion L, Stover M. The use of gravity or manual-stress radiographs in the assessment of supination-external rotation fractures of the ankle. J Bone Joint Surg Br 2007;89:1055–1059. [DOI] [PubMed] [Google Scholar]
- 27. Lloyd J, Elsayed S, Hariharan K, Tanaka H. Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int 2006;27:793–796. [DOI] [PubMed] [Google Scholar]
- 28. Fox A, Wykes P, Eccles K, Barrie J. Five years of ankle fractures grouped by stability. Injury 2005;36:836–841. [DOI] [PubMed] [Google Scholar]
- 29. Hutchinson RH, Barrie JL. The effects of shared decision making in the conservative management of stable ankle fractures. Injury 2015;46:1116–1118. [DOI] [PubMed] [Google Scholar]
- 30. Mittal R, Harris IA, Adie S, Naylor JM, CROSSBAT Study Group. Surgery for type B ankle fracture treatment: a combined randomised and observational study (CROSSBAT). BMJ Open 2017;7:e013298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tornetta P, III, Creevy W. Lag screw only fixation of the lateral malleolus. J Orthop Trauma 2001;15:119–121. [DOI] [PubMed] [Google Scholar]
- 32. Zahn RK, Frey S, Jakubietz RG, et al. A contoured locking plate for distal fibular fractures in osteoporotic bone: a biomechanical cadaver study. Injury 2012;43:718–725. [DOI] [PubMed] [Google Scholar]
- 33. Minihane KP, Lee C, Ahn C, Zhang LQ, Merk BR. Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma 2006;20:562–566. [DOI] [PubMed] [Google Scholar]
- 34. Schepers T, Van Lieshout EM, De Vries MR, Van der Elst M. Increased rates of wound complications with locking plates in distal fibular fractures. Injury 2011;42:1125–1129. [DOI] [PubMed] [Google Scholar]
- 35. Jain S, Haughton BA, Brew C. Intramedullary fixation of distal fibular fractures: a systematic review of clinical and functional outcomes. J Orthop Traumatol 2014;15:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Parker L, Garlick N, McCarthy I, Grechenig S, Grechenig W, Smitham P. Screw fixation of medial malleolar fracutures. Bone Joint J 2013;95:1662–1666. [DOI] [PubMed] [Google Scholar]
- 37. Hansen M, Le L, Wertheimer S, Meyer E, Haut R. Syndesmosis fixation: analysis of shear stress via axial load on 3.5-mm and 4.5-mm quadricortical syndesmotic screws. J Foot Ankle Surg 2006;45:65–69. [DOI] [PubMed] [Google Scholar]
- 38. Moore JA, Jr, Shank JR, Morgan SJ, Smith WR. Syndesmosis fixation: a comparison of three and four cortices of screw fixation without hardware removal. Foot Ankle Int 2006;27:567–572. [DOI] [PubMed] [Google Scholar]
- 39. Hamid N, Loeffler BJ, Braddy W, Kellam JF, Cohen BE, Bosse MJ. Outcome after fixation of ankle fractures with an injury to the syndesmosis: the effect of the syndesmosis screw. J Bone Joint Surg Br 2009;91:1069–1073. [DOI] [PubMed] [Google Scholar]
- 40. Boyle MJ, Gao R, Frampton CM, Coleman B. Removal of the syndesmotic screw after the surgical treatment of a fracture of the ankle in adult patients does not affect one-year outcomes: a randomised controlled trial. Bone Joint J 2014;96-B:1699–1705. [DOI] [PubMed] [Google Scholar]
- 41. Michelson JD, Wright M, Blankstein M. Syndesmotic ankle fractures: a systematic review. J Orthop Trauma 2017. https://doi.org/10.1097/BOT.0000000000000937 [Epub ahead of print]. [DOI] [PubMed]
- 42. Kortekangas T, Savola O, Flinkkilä T, et al. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury 2015;46:1119–1126. [DOI] [PubMed] [Google Scholar]
- 43. Zhang P, Liang Y, He J, Fang Y, Chen P, Wang J. A systematic review of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury. BMC Musculoskelet Disord 2017;18:286–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Solan MC, Davies MS, Sakellariou A. Syndesmosis stabilisaton: screws versus flexible fixation. Foot Ankle Clin 2017;22:35–63. [DOI] [PubMed] [Google Scholar]
- 45. Futamura K, Baba T, Mogami A, et al. Malreduction of syndesmosis injury associated with malleolar ankle fracture can be avoided using Weber’s three indexes in the mortise view. Injury 2017;48:954–959. [DOI] [PubMed] [Google Scholar]
- 46. Bartoníček J, Rammelt S, Tuček M. Posterior malleolar fractures: changing concepts and recent developments. Foot Ankle Clin 2017;22:125–145. [DOI] [PubMed] [Google Scholar]
- 47. Veltman ES, Halma JJ, de Gast A. Longterm outcome of 886 posterior malleolar fractures: a systematic review of the literature. Foot Ankle Surg 2016;22:73–77. [DOI] [PubMed] [Google Scholar]
- 48. Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2006;447:165–171. [DOI] [PubMed] [Google Scholar]
- 49. Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res 2010;468:1129–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Egol KA, Pahk B, Walsh M, Tejwani NC, Davidovitch RI, Koval KJ. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. J Orthop Trauma 2010;24:7–11. [DOI] [PubMed] [Google Scholar]
- 51. Kortekangas TH, Pakarinen HJ, Savola O, et al. Syndesmotic fixation in SER ankle fractures: a prospective randomised study. Foot Ankle Int 2014;35:988–995. [DOI] [PubMed] [Google Scholar]
- 52. Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int 2017. https://doi.org/10.1177/1071100717719533 [Epub ahead of print]. [DOI] [PubMed]
- 53. Gougoulias N, Dawe EJ, Sakellariou A. The recovery position for posterior surgery of the ankle and hindfoot. Bone Joint J 2013;95-B:1317–1319. [DOI] [PubMed] [Google Scholar]