Abstract
The complex ultrastructure of the meniscus determines its vital functions for the knee, the lower extremity, and the body.
The most recent concise, reliable, and valid classification system for meniscal tears is the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) Classification, which takes into account the subsequent parameters: tear depth, tear pattern, tear length, tear location/rim width, radial location, location according to the popliteal hiatus, and quality of the meniscal tissue.
It is the orthopaedic surgeon’s responsibility to combine clinical information, radiological images, and clinical experience in an effort to individualize management of meniscal tears, taking into account factors related to the patient and lesion.
Surgeons should strive not to operate in most cases, but to protect, repair or reconstruct, in order to prevent early development of osteoarthritis by restoring the native structure, function, and biomechanics of the meniscus.
Currently, there are three main methods of modern surgical management of meniscus tears: arthroscopic partial meniscectomy; meniscal repair with or without augmentation techniques; and meniscal reconstruction. Meniscus surgery has come a long way from the old slogan, “If it is torn, take it out!” to the currently accepted slogan, “Save the meniscus!” which has guided evolving modern treatment methods for meniscal tears. This last slogan will probably constitute the basis for newer alternative biological treatment methods in the future.
Cite this article: EFORT Open Rev 2018;3 DOI: 10.1302/2058-5241.3.170067.
Keywords: knee injury, meniscus tears, investigation, treatment
Introduction
Meniscal tears are the most frequently encountered and treated injuries in the knee joint, with a bimodal age distribution in young, active sports people and in elderly people, and with a relatively high annual cost.1-3 Similarly, meniscal tear surgery is among the most commonly performed procedures in orthopaedic surgery.
There are two menisci, which are medial (U-shaped) and lateral (S-shaped) semilunar shaped, hydrated, biphasic fibrocartilaginous soft-tissue structures in the medial and lateral tibiofemoral compartments of the knee joint, respectively. They are not solely a separate structure; they are a part of the ‘meniscus-meniscal ligament complex’ together with the surrounding ligamentous structures (menisco-tibial, menisco-femoral, menisco-patellar, intermeniscal ligaments) and bony attachments as anterior and posterior roots. 4 Although the meniscus is totally vascularized at birth, its vascularity is limited to only the peripheral 10% to 30% zone in adulthood (Fig. 1).5,6 The morphology of this load-bearing complex structure, which contains radial fibrils centrally, circumferential fibrils peripherally and perforating fibres, determines its vital functions: load bearing, joint stability, joint congruity, increasing joint contact area, decreasing joint contact stresses, protection of articular cartilage, shock absorption, lubrication, limitation of extreme movement and proprioception.7-9 The structural degeneration or deterioration of the menisci due to senescence, trauma or surgery eventually leads to osteoarthritis of the knee joint, independent of meniscus morphology.10-16
Fig. 1.
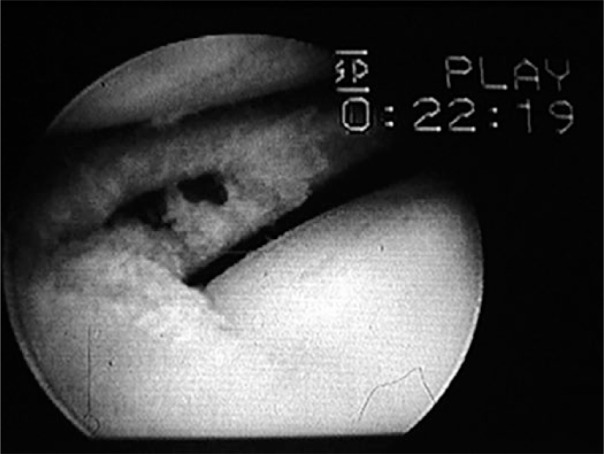
Arthroscopic view illustrating meniscal vascularity. Note the bleeding from the peripheral part of the lateral meniscus after partial meniscectomy.
The risk factors for meniscal tears were summarized in a recent systematic review.17 In this study, on the one hand, advanced age (> 60 years), male gender, work-related kneeling, squatting and climbing stairs (> 30 flights) were found as risk factors for degenerative tears with strong supporting evidence. On the other hand, daily sitting more than two hours was found to reduce the risk for degenerative tears with strong evidence. Moreover, for acute traumatic tears, playing soccer and rugby and waiting more than 12 months between anterior cruciate ligament (ACL) injury and reconstruction were found to be important risk factors with strong evidence.
Clinical evaluation
History taking, which may give important diagnostic clues for experienced surgeons, must be the first step in clinical evaluation for meniscal tears. Patients may have the following complaints: pain, subacute swelling, hearing or sensation of a ‘pop’ during injury, and mechanical symptoms such as popping, limitation of range of movement, catching, locking, etc. It should also be noted that the type and severity of meniscal tears do not correlate with the patient’s symptoms.18
Physical examination should be performed systematically, beginning from the evaluation of lower extremity alignment to the evaluation of ligamentous and soft tissues. Although special provocative signs for meniscal tears (McMurray, Apley test, ‘Bounce’ test, Thessaly test and especially joint line tenderness, etc.) are present, their accuracy, specificity and sensitivity are highly variable and questionable.19,20 It should be kept in mind that these above-mentioned mechanical symptoms and physical findings may also be found secondary to articular cartilage or ligamentous injuries. Although an experienced surgeon may suspect meniscal tears following a careful history and physical examination, radiographic and arthroscopic evaluations should be made to confirm the diagnosis. Moreover, radiographic evaluation is performed for malalignment, concomitant bony pathology, presence of arthritic changes, etc. MRI and arthroscopy are still the benchmark non-invasive and invasive methods for the evaluation of meniscal tears, respectively.21-23
Classification
Meniscal tears can be classified according to the tear patterns, aetiology and MRI. However, the most recent concise, reliable and valid classification system for meniscal tears is the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine classification, which takes into account the following parameters: tear depth, tear pattern, tear length, tear location/rim width, radial location, location according to the popliteal hiatus, and quality of the meniscal tissue.24 The main limitations of this classification are reported as the absence of oblique tears, root ligament injuries, lesions of discoid variants and the evaluation of previously operated menisci.22 The most common meniscal tears in active young people and in the elderly are traumatic longitudinal-vertical and degenerative tears respectively. The most common side and site for tears are the medial meniscus and the posterior horn of the menisci.25
Management strategies
The vital functions of the meniscus and the development of osteoarthritis reported after its resection, has forced orthopaedic surgeons to protect as much as possible, to repair or to reconstruct the meniscus. The management decision to use non-operative or operative methods should take into consideration factors related to patients (age, expectations, activity level, lifestyle, general health status, etc.) and lesions (location, type, aetiology, tissue quality, associated lesions, etc.). It is the orthopaedic surgeon’s responsibility to combine clinical information, radiological images and clinical experience in an effort to tailor the correct management in an individualized way, according to the factors related to the patient and the lesion.26
Non-operative management
Non-operative management is useful for the initial treatment for acute knee trauma and as a first-line treatment method in degenerative meniscal tears. In the former situation, the ‘PRICE’ (protection, rest, ice, compression, elevation) protocol is applied. In the latter case, non-operative management (anti-inflammatory and analgesic medications, quadriceps strengthening, activity modification, unloader bracing and intra-articular injections, etc.) rather than surgical methods should be tried for at least three to six months, if the mechanical symptoms do not dominate the clinical picture.27-29 If the patient’s symptoms persist thereafter, the surgical alternatives, which are summarized below, are available.
Operative management
Currently, there are three main methods for the surgical management of meniscus tears: meniscectomy, meniscal repair, and meniscal reconstruction. In a recent meta-analysis, it was emphasized that there was a deficiency of high-level evidence to guide the surgical management of meniscal tears.30
Meniscectomy (open versus arthroscopic, total versus partial)
Meniscectomy can be performed totally or partially, open or arthroscopically. The first arthroscopic meniscectomy was believed to be performed by the ‘father’ of arthroscopy, Masaki Watanabe.26 In the current era, total meniscectomy is almost never performed or advised as a primary procedure in meniscal lesions. This is due to its detrimental effects, most importantly development of early osteoarthritis and unsuccessful long-term clinical results.10,11 Interestingly, although the rate of total knee arthroplasty due to symptomatic osteoarthritis of the knee after open total meniscectomy in adolescence was found to have increased comparatively in a prospective longitudinal 40-year follow-up study, it should also be noted that not all the patients had undergone surgery.31 Currently in the modern treatment of meniscal tears, neither open nor arthroscopic total meniscectomy are advised to be performed primarily in most cases.
Partial meniscectomy can be performed in an open or more frequently arthroscopic fashion. It is indicated in patients who have radial tears in the white-white zone and degenerative meniscal tears – which are considered as the precursor lesion of early stage osteoarthritis – with mechanical symptoms and refractory to at least 3-6 months of non-surgical management, and if meniscal repair is not possible due to factors related to the patient or lesion. Arthroscopic partial meniscectomy (APM) is the most frequently performed surgical procedure for the treatment of meniscal tears (Fig. 2).32,33 The three main reasons are the rapid speed of the procedure, low morbidity, and good short-term results.34 The details of the modern surgical techniques on APM for the above-mentioned commonly-described patterns of meniscal tears were recently described in detail.35 The short-term clinical results were found to be highly successful, but a high rate of progression to osteoarthritis at long term was also demonstrated.36 Moreover, even with degenerative and traumatic meniscal tears, recent, relatively high LoE studies have found low to moderate evidence regarding the absence of long-term comparative clinical benefit between APM and non-operative or sham treatments.37-41 In symptomatic, degenerative root tears of the medial meniscus, APM was found to provide no benefit at all, with female gender, increased body mass index and meniscal extrusion as bad prognostic factors.42
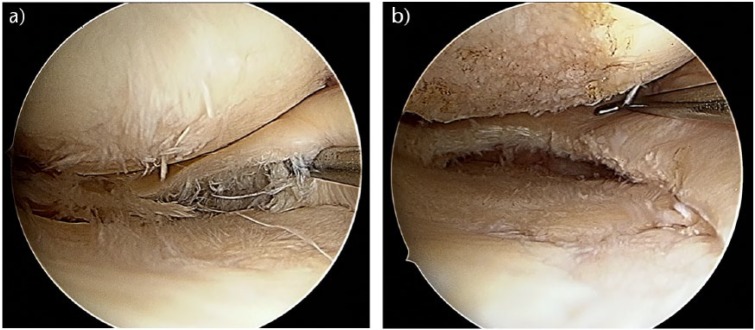
Fig. 2.
Arthroscopic view of a degenerative medial meniscus posterior horn tear, unresponsive to non-operative management (a). After arthroscopic partial meniscectomy (b).
Currently, due to the above-mentioned reasons and clinical results, APM should be the last resort for most meniscal tears, even degenerative meniscal lesions, and should be limited as far as possible. It may be applicable in carefully selected patients, who have persistent mechanical symptoms from degenerative tears, symptomatic complex tears with a damaged meniscus and non-repairable tears in middle-aged patients with non-symptomatic ACL injury for traumatic tears.27 According to the current algorithm of the 2016 ESSKA Meniscus Consensus Project, the messages regarding APM were as follows:
APM should not be considered as the first-line treatment choice;
APM should only be proposed after a proper standardized imaging protocol;
APM can be proposed after three months of persistent pain/mechanical symptoms or earlier in cases with considerable mechanical symptoms;
No APM should be proposed with advanced osteoarthritis on Schuss view.43
Meniscal repair
Meniscal repair can be performed open or arthroscopically. Meniscal repair was initially performed by Annandale and DeHaven.44-46 After this milestone in the history of meniscus surgery, the first arthroscopic repair was performed by Ikeuchi.26 The era of meniscal preservation was based on three pillars: repair of the torn meniscus whenever reasonable; non-surgical treatment of asymptomatic meniscal pathologies despite a meniscal tear according to MRI; and partial meniscectomy and resection of as much as necessary and as little as possible.34 In this regard, the most amenable tears to be repaired are acute, traumatic tears within the peripheral well-vascularized red-red zone which are longitudinal-vertical in orientation.15 In traumatic tears, the first choice is repair or non-removal.27 Extended indications for meniscal repair were recommended for the subsequent clinical entities: horizontal cleavage tears in young athletes, root tears, ramp lesions, radial tears and tears in the red-white zone.47-52
Open repair may be still useful, especially for posterior meniscal tears with a very tight medial compartment, if percutaneous release of medial collateral ligament does not provide enough visualization of the compartment.21 Although successful clinical results were reported with open repair, there has been increasing evolution from open to arthroscopic repair and currently the latter predominates for meniscal tears.53
At present, there are three main techniques for meniscal repair: inside-out, outside-in, all-inside. Among them the strongest repair has been accepted as the inside-out technique, which was first described by Henning.54,55 In this technique, the tear is fixed by placement and fixation of the passing sutures from the intra-articular region with the use of special cannulae to a safe extracapsular area over the capsule with a posterolateral or posteromedial incision. For the posteriorly-placed tears, an open technique with the use of special retractors is used in order to protect the neurovascular structures. The benchmark currently remains an inside-out vertical mattress suture repair.56 Successful clinical results have been reported with inside-out meniscal repair.57,58
Outside-in techniques were described by Warren and Levy and Morgan and Casscells.59,60 In this less frequently used technique, passing sutures were passed through the previously passed two spinal needles from the meniscal rim to the meniscal body across the meniscal tear. The two ends of the passing sutures were tied onto the capsule, under direct vision. The improper apposition of the ends of the meniscal tear is an important disadvantage of this technique. The all-inside technique with the use of a suture hook device was first described by Morgan.61 Thereafter an absorbable polylactic acid tack implant was introduced by Albrecht-Olsen et al.62 Various polylactic acid-based implants have also been used: arrows, screws and staples, but due to implant-induced synovitis and cartilage damage etc., the use of these implants has fallen out of clinical practice.63 The flexible, suture-based devices have become more popular since 2006 (Fig. 3).64 The pull-out strength of the all-inside suture-based devices was found to be similar to traditional mattress sutures.65,66 This technique has been an increasingly used method for most meniscal tears due to its advantages: avoidance of opening accessory portals and additional incisions, easy applicability, use of bio-absorbable implants and relatively less risk for injury to posterior neurovascular structures. However, its use is limited to anteriorly placed meniscal tears.
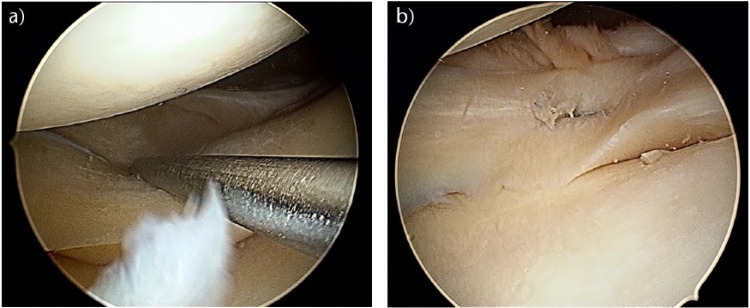
Fig. 3.
Arthroscopic view of acute, traumatic, longitudinal-vertical tear of the lateral meniscus posterior horn (a). ‘All-inside’ horizontal suture of the lateral meniscal tear (b).
As a result, in a recent systematic review by Fillingham et al,63 two important conclusions were reported. First, the quality of evidence comparing inside-out and all-inside meniscal repair remained low, with a majority of the literature being evidence level 4 studies. Secondly, there were no significant differences in terms of anatomical and clinical failure rates, functional outcome scores and complication rates. In a meta-analysis, it was concluded that although meniscal repairs had a higher re-operation rate than meniscectomy, they result in a better long-term functional outcome, better activity level and lower failure rate.67 Moreover, meniscal repair was found to be more cost-effective than meniscectomy.68 Although the advantages of meniscal repair outweigh those of meniscectomy, interestingly, APM is still more frequently performed. This may be due to the fact that repair is technically more demanding, more time-consuming, needs longer rehabilitation time and is more expensive.34
In order to enhance healing after meniscal repair, a variety of augmentation techniques and biological products have been introduced: needling, trephination, platelet-rich plasma, bone marrow aspirate, hyaluronan-collagen scaffold, fibrin clot, fibrin glue, mesenchymal stem cells, growth factors, etc.69-73 Except for needling and trephination, the evolving significant potential for biological augmentation and tissue engineering strategies in the enhancement of meniscal repair and reconstruction still requires high level of evidence comparative studies in order to be translated clinically to be put forward as the optimal method of treatment.27,74,75
Meniscal reconstruction
Meniscal reconstruction techniques, which are used to replace the partially or totally resected meniscus in symptomatic patients unresponsive to conservative management, mainly consist of two main procedures: meniscal scaffolds and meniscal allograft transplantation (MAT). Although saving meniscal tissue is the ideal management method, partial or total meniscal resection are also used, especially in irreparable meniscal lesions or by inexperienced surgeons for meniscal repair. In the latter cases, meniscal reconstruction is a last chance to fill the defect after meniscectomy in patients who are unresponsive to other treatments. They have been relatively rarely performed compared with previously discussed procedures.
The main aims of meniscal reconstruction procedures are to place safely a functional meniscus that is anatomically and structurally similar to the native meniscus, to restore the knee and lower extremity biomechanics, to improve joint function, to relieve pain and eventually to prevent or delay the degenerative process in the knee joint.
Meniscal scaffolds
Highly porous, cell-free and biodegradable meniscal scaffolds are used to fill the defect in the previously partially-resected meniscus and to develop the meniscal tissue by allowing migration and growth of vascular channels and precursor cells into the scaffold.76-78
In clinical practice, there are two main types of meniscal scaffolds: the Collagen Meniscus Implant (CMI) and polyurethane-based scaffold.79-81 The indications and surgical techniques are similar for these two implants. These procedures can be performed arthroscopically, as described previously.78 Regarding clinical efficacy, good mid-term and long-term clinical outcomes of polyurethane-based scaffolds and CMI were recently reported.82-85 Currently, it is concluded that the mid-term survival rate of scaffolds is favourable compared with meniscal repair, but unfavourable compared with MAT.82 In conclusion, the chondroprotective effects of these implants are still controversial, and long-term higher level of evidence comparative studies are required to clarify the clinical efficacy of these implants.
MAT
MAT procedure is not actually a new concept. The interposition arthroplasty with autogenic fat pad was first reported at the beginning of the 1900s.26 Since the more recent performance of MAT by Wirth in the 1980s, the MAT procedure has evolved to be what it is now; an increasingly performed, safe, reliable and highly specialized knee procedure, rather than an experimental or investigational surgery in patients whose meniscus is lost for any reason, and who have refractory persistent symptoms.86-89
The current indications for MAT were summarized according to the recommendations of consensus statements developed from the 2015 International Meniscus Reconstruction Experts Forum, which were based on current evidence from clinical results following MAT: unicompartmental pain in the presence of total or partial ‘functional’ meniscectomy; as a concomitant procedure to revision ACL reconstruction to aid in joint stability when meniscus deficiency is believed to be a contributing factor to failure; or as a concomitant procedure with articular cartilage repair in a meniscus-deficient compartment.90
Currently, the MAT can be performed as an open procedure or arthroscopically in carefully selected patients by experienced surgeons. The malalignment, instability and limb length inequality of the patients must be corrected beforehand or concomitantly. Among four storage methods of meniscal allografts (fresh viable, fresh-frozen, cryopreserved and lyophilized), fresh viable and fresh-frozen allograft are recommended.90,91 The optimal-sized allograft, according to the MRI or radiological knee films of the patient, can be fixed with or without bone plugs or block. In order to obtain conclusive results regarding the relative technical and clinical superiority, the relevant literature requires comparative studies with higher LoE, involving higher numbers of patients and longer follow-up periods.
Management of special lesions
Root tears and ramp lesions
Lateral and medial menisci are attached to the tibial plateau anteriorly and posteriorly via meniscal root ligaments. Their tear was firstly described by Pagnani.92 Although tears of meniscal roots are relatively less common than meniscal body tears, their biomechanical and clinical impact is more significant in terms of stability and shock absorption functions.93 Their injuries are frequently underestimated and unrecognized by inexperienced, or sometimes experienced, surgeons. A high index of suspicion is necessary for diagnosis. The pathognomonic signs are found on MRI: ‘ghost’ signs (absence of posterior root on sagittal images) and meniscal extrusion.94 Three specific lesions related especially to posterior meniscal roots are present: root avulsion injuries, radial tears and degenerative changes.95 Meniscal extrusion, which is also present with posterior root tears, impairs the stability and biomechanical functions of the menisci.96 Although the management of these lesions is relatively new, a current algorithm was suggested by Bhatia et al:52 non-operative treatments (anti-inflammatory medication, activity modification, unloader bracing and intra-articular chondroprotective injections, etc.) for improper surgical candidates; meniscal root repair for acute tears and chronic tears without pre-existing arthritis; and partial meniscectomy for chronic and symptomatic tears with pre-existing arthritis. Regarding meniscal repair, the subsequently described techniques at present are: trans-osseous pull-out suture, suture anchor and side-to-side repairs.95,97,98
Ramp lesions, which are longitudinal peripheral lesions of the posterior medial meniscus or menisco-capsular junction, previously called ‘hidden lesions’, mostly associated with ACL tears, form a relatively new terminology after the systematic arthroscopic exploration of the knee joint.50,99 Although their diagnosis requires a high index of suspicion, posteromedial tibial bone bruising was found to be an important secondary MRI finding of ramp lesions.100 They were also classified by Thaunat et al.51 The treatment alternatives were reported as non-operative, inside-out repair and all-inside repair.50,51
Currently, the optimal management and technique regarding meniscal repair in root tears and ramp lesions is still evolving and remains debatable and controversial.50-52,101
Discoid meniscus tears
Since the first observation and description of discoid meniscus, which was more frequently seen laterally than medially, it is established that it is more prone to tearing than a normal meniscus.102 The current management depends mostly on the symptomatology of the patient. Asymptomatic discoid meniscus is classically treated conservatively. If the patient is symptomatic, the preferred method is APM (saucerization) with preservation of the stable peripheral rim, which has seen successful clinical results.102
Conclusions
The enthusiastic evolution of meniscus surgery has seen a great change from interest in repair in the 1800s to total resection in the 1970s, and finally to protection, or reconstruction if resected, from the 1990s to the present day.103 The rapid developments in cell biology and tissue engineering will advance new alternative biological methods in the treatment of meniscal tears in the future. Finally, meniscus surgery has come a long way from the old slogan ‘if it is torn, take it out!’, to the currently accepted ‘Save the meniscus!’, which now guides the evolving modern treatment methods for meniscal tears. ‘Save the meniscus!’ is the slogan which will probably constitute the basis for newer alternative biological treatment methods in the future.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Baker BE, Peckham AC, Pupparo F, Sanborn JC. Review of meniscal injury and associated sports. Am J Sports Med 1985;13:1-4. [DOI] [PubMed] [Google Scholar]
- 2. Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 2008;39:1338-1344. [DOI] [PubMed] [Google Scholar]
- 3. Mather RC, III, Garrett WE, Cole BJ, et al. Cost-effectiveness analysis of the diagnosis of meniscus tears. Am J Sports Med 2015;43:128-137. [DOI] [PubMed] [Google Scholar]
- 4. Masouros SD, McDermott ID, Amis AA, Bull AMJ. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc 2008;16:1121-1132. [DOI] [PubMed] [Google Scholar]
- 5. Petersen W, Tillmann B. Age-related blood and lymph supply of the knee menisci. A cadaver study. Acta Orthop Scand 1995;66:308-312. [DOI] [PubMed] [Google Scholar]
- 6. Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-95. [DOI] [PubMed] [Google Scholar]
- 7. Fox AJ, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat 2015;28:269-287. [DOI] [PubMed] [Google Scholar]
- 8. Danso EK, Oinas JMT, Saarakkala S, et al. Structure-function relationships of human meniscus. J Mech Behav Biomed Mater 2017;67:51-60. [DOI] [PubMed] [Google Scholar]
- 9. Verdonk R, Madry H, Shabshin N, et al. The role of meniscal tissue in joint protection in early osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2016;24:1763-1774. [DOI] [PubMed] [Google Scholar]
- 10. Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg [Br] 1948;30-B:664-670. [PubMed] [Google Scholar]
- 11. Neyret PH, Walch G, Dejour H. La méniscectomie interne intra-murale selon la technique de A. Trillat. Résultats à long terme de 258 interventions. Rev Chir Orthop Repar Appar Mot 1988;74:637-646. [PubMed] [Google Scholar]
- 12. Tsujii A, Nakamura N, Horibe S. Age-related changes in the knee meniscus. Knee 2017;24:1262-1270. [DOI] [PubMed] [Google Scholar]
- 13. Goebel L, Reinhard J, Madry H. Meniscal lesion. A pre-osteoarthritic condition of the knee joint. Orthopade 2017;46:822-830. [DOI] [PubMed] [Google Scholar]
- 14. Englund M. The role of the meniscus in osteoarthritis genesis. Rheum Dis Clin North Am 2008;34:573-579. [DOI] [PubMed] [Google Scholar]
- 15. Vaquero J, Forriol F. Meniscus tear surgery and meniscus replacement. Muscles Ligaments Tendons J 2016;6:71-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jarraya M, Roemer FW, Englund M, et al. Meniscus morphology: does tear type matter? A narrative review with focus on relevance for osteoarthritis research. Semin Arthritis Rheum 2017;46:552-561. [DOI] [PubMed] [Google Scholar]
- 17. Snoeker BAM, Bakker EWP, Kegel CAT, Lucas C. Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther 2013;43:352-367. [DOI] [PubMed] [Google Scholar]
- 18. Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med 2008;359:1108-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Smith BE, Thacker D, Crewesmith A, Hall M. Special tests for assessing meniscal tears within the knee: a systematic review and meta-analysis. Evid Based Med 2015;20:88-97. [DOI] [PubMed] [Google Scholar]
- 20. Blyth M, Anthony I, Francq B, et al. Diagnostic accuracy of the Thessaly test, standardised clinical history and other clinical examination tests (Apley’s, McMurray’s and joint line tenderness) for meniscal tears in comparison with magnetic resonance imaging diagnosis. Health Technol Assess 2015;19:1-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maffulli N, Longo UG, Campi S, Denaro V. Meniscal tears. Open Access J Sports Med 2010;1:45-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wadhwa V, Omar H, Coyner K, et al. ISAKOS classification of meniscal tears-illustration on 2D and 3D isotropic spin echo MR imaging. Eur J Radiol 2016;85:15-24. [DOI] [PubMed] [Google Scholar]
- 23. Wong KP, Han AX, Wong JL, Lee DY. Reliability of magnetic resonance imaging in evaluating meniscal and cartilage injuries in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc 2017;25:411-417. [DOI] [PubMed] [Google Scholar]
- 24. Anderson AF, Irrgang JJ, Dunn W, et al. Interobserver reliability of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) classification of meniscal tears. Am J Sports Med 2011;39:926-932. [DOI] [PubMed] [Google Scholar]
- 25. Metcalf MH, Barrett GR. Prospective evaluation of 1485 meniscal tear patterns in patients with stable knees. Am J Sports Med 2004;32:675-680. [DOI] [PubMed] [Google Scholar]
- 26. Di Matteo B, Moran CJ, Tarabella V, et al. A history of meniscal surgery: from ancient times to the twenty-first century. Knee Surg Sports Traumatol Arthrosc 2016;24:1510-1518. [DOI] [PubMed] [Google Scholar]
- 27. Beaufils P, Becker R, Kopf S, Matthieu O, Pujol N. The knee meniscus: management of traumatic tears and degenerative lesions. EFORT Open Rev 2017;2:195-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yim JH, Seon JK, Song EK, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med 2013;41:1565-1570. [DOI] [PubMed] [Google Scholar]
- 29. Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM. Treatment of meniscal tears: an evidence based approach. World J Orthop 2014;5:233-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mutsaerts ELAR, van Eck CF, van de Graaf VA, Doornberg JN, van den Bekerom MPJ. Surgical interventions for meniscal tears: a closer look at the evidence. Arch Orthop Trauma Surg 2016;136:361-370. [DOI] [PubMed] [Google Scholar]
- 31. Pengas IP, Assiotis A, Nash W, et al. Total meniscectomy in adolescents: a 40-year follow-up. J Bone Joint Surg [Br] 2012;94-B:1649-1654. [DOI] [PubMed] [Google Scholar]
- 32. Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report 2009;11:1-25. [PubMed] [Google Scholar]
- 33. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg [Am] 2011;93-A:994-1000. [DOI] [PubMed] [Google Scholar]
- 34. Beaufils P, Becker R, Verdonk R, Aagaard H, Karlsson J. Focusing on results after meniscus surgery. Knee Surg Sports Traumatol Arthrosc 2015;23:3-7. [DOI] [PubMed] [Google Scholar]
- 35. Doral MN, Turhan E, Donmez G, et al. Meniscectomy. Tech Knee Surg 2010;9:150-158. [Google Scholar]
- 36. Faunø P, Nielsen AB. Arthroscopic partial meniscectomy: a long-term follow-up. Arthroscopy 1992;8:345-349. [DOI] [PubMed] [Google Scholar]
- 37. Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ 2014;186:1057-1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 2013;369:2515-2524. [DOI] [PubMed] [Google Scholar]
- 39. Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med 2013;368:1675-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Ann Rheum Dis 2017. May 18. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sihvonen R. Meniscal resection may not benefit patients with traumatic meniscal tears. Evid Based Med 2017;22:193. [DOI] [PubMed] [Google Scholar]
- 42. Krych AJ, Johnson NR, Mohan R, et al. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc 2017. February 09. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 43. Beaufils P, Becker R, Kopf S, et al. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc 2017;25:335-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Annandale T. An operation for displaced semilunar cartilage. BMJ 1885;1:779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Di Matteo B, Tarabella V, Filardo G, et al. Thomas Annandale: the first meniscus repair. Knee Surg Sports Traumatol Arthrosc 2013;21:1963-1966. [DOI] [PubMed] [Google Scholar]
- 46. DeHaven KE, Black KP, Griffiths HJ. Open meniscus repair. Technique and two to nine year results. Am J Sports Med 1989;17:788-795. [DOI] [PubMed] [Google Scholar]
- 47. Kurzweil PR, Lynch NM, Coleman S, Kearney B. Repair of horizontal meniscus tears: a systematic review. Arthroscopy 2014;30:1513-1519. [DOI] [PubMed] [Google Scholar]
- 48. Bhatia S, Civitarese DM, Turnbull TL, et al. A novel repair method for radial tears of the medial meniscus: biomechanical comparison of transtibial 2-tunnel and double horizontal mattress suture techniques under cyclic loading. Am J Sports Med 2016;44:639-645. [DOI] [PubMed] [Google Scholar]
- 49. Barber-Westin SD, Noyes FR. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy 2014;30:134-146. [DOI] [PubMed] [Google Scholar]
- 50. Chahla J, Dean CS, Moatshe G, et al. Meniscal ramp lesions: anatomy, incidence, diagnosis, and treatment. Orthop J Sports Med 2016;4:eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Thaunat M, Fayard JM, Guimaraes TM, et al. Classification and Surgical Repair of Ramp Lesions of the Medial Meniscus. Arthrosc Tech 2016;5:e871-e875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 2014;42:3016-3030. [DOI] [PubMed] [Google Scholar]
- 53. DeHaven KE, Sebastianelli WJ. Open meniscus repair. Indications, technique, and results. Clin Sports Med 1990;9:577-587. [PubMed] [Google Scholar]
- 54. Henning CE, Clark JR, Lynch MA, et al. Arthroscopic meniscus repair with a posterior incision. Instr Course Lect 1988;37:209-221. [PubMed] [Google Scholar]
- 55. Scott GA, Jolly BL, Henning CE. Combined posterior incision and arthroscopic intra-articular repair of the meniscus. An examination of factors affecting healing. J Bone Joint Surg [Am] 1986;68-A:847-861. [PubMed] [Google Scholar]
- 56. Turman KA, Diduch DR, Miller MD. All-inside meniscal repair. Sports Health 2009;1:438-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Haklar U, Donmez F, Basaran SH, Canbora MK. Results of arthroscopic repair of partial- or full-thickness longitudinal medial meniscal tears by single or double vertical sutures using the inside-out technique. Am J Sports Med 2013;41:596-602. [DOI] [PubMed] [Google Scholar]
- 58. Steadman JR, Matheny LM, Singleton SB, et al. Meniscus suture repair: minimum 10-year outcomes in patients younger than 40 years compared with patients 40 and older. Am J Sports Med 2015;43:2222-2227. [DOI] [PubMed] [Google Scholar]
- 59. Warren RF, Levy IM. Meniscal lesions associated with anterior cruciate ligament injury. Clin Orthop Relat Res 1983;172:32-37. [PubMed] [Google Scholar]
- 60. Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy 1986;2:3-12. [DOI] [PubMed] [Google Scholar]
- 61. Morgan CD. The “all-inside” meniscus repair. Arthroscopy 1991;7:120-125. [DOI] [PubMed] [Google Scholar]
- 62. Albrecht-Olsen P, Kristensen G, Törmälä P. Meniscus bucket-handle fixation with an absorbable Biofix tack: development of a new technique. Knee Surg Sports Traumatol Arthrosc 1993;1:104-106. [DOI] [PubMed] [Google Scholar]
- 63. Fillingham YA, Riboh JC, Erickson BJ, Bach BR, Jr, Yanke AB. Inside-out versus all-inside repair of isolated meniscal tears. An updated systematic review. Am J Sports Med 2017;45:234-242. [DOI] [PubMed] [Google Scholar]
- 64. Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy 2006;22:3-9. [DOI] [PubMed] [Google Scholar]
- 65. Dervin GF, Downing KJ, Keene GC, McBride DG. Failure strengths of suture versus biodegradable arrow for meniscal repair: an in vitro study. Arthroscopy 1997;13:296-300. [DOI] [PubMed] [Google Scholar]
- 66. Barber FA, Herbert MA, Richards DP. Load to failure testing of new meniscal repair devices. Arthroscopy 2004;20:45-50. [DOI] [PubMed] [Google Scholar]
- 67. Xu C, Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc 2015;23:164-170. [DOI] [PubMed] [Google Scholar]
- 68. Feeley BT, Liu S, Garner AM, Zhang AL, Pietzsch JB. The cost-effectiveness of meniscal repair versus partial meniscectomy: A model-based projection for the United States. Knee 2016;23:674-680. [DOI] [PubMed] [Google Scholar]
- 69. Anz AW, Hackel JG, Nilssen EC, Andrews JR. Application of biologics in the treatment of the rotator cuff, meniscus, cartilage, and osteoarthritis. J Am Acad Orthop Surg 2014;22:68-79. [DOI] [PubMed] [Google Scholar]
- 70. Kamimura T, Kimura M. Meniscal repair of degenerative horizontal cleavage tears using fibrin clots: clinical and arthroscopic outcomes in 10 cases. Orthop J Sports Med 2014;2:eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Fox JM, Rintz KG, Ferkel RD. Trephination of incomplete meniscal tears. Arthroscopy 1993;9:451-455. [DOI] [PubMed] [Google Scholar]
- 72. Tetik O, Kocabey Y, Johnson DL. Synovial abrasion for isolated, partial thickness, undersurface, medial meniscus tears. Orthopedics 2002;25:675-678. [DOI] [PubMed] [Google Scholar]
- 73. Pujol N, Salle De, Chou E, Boisrenoult P, Beaufils P. Platelet-rich plasma for open meniscal repair in young patients: any benefit? Knee Surg Sports Traumatol Arthrosc 2015;23:51-58. [DOI] [PubMed] [Google Scholar]
- 74. Moran CJ, Busilacchi A, Lee CA, Athanasiou KA, Verdonk PC. Biological augmentation and tissue engineering approaches in meniscus surgery. Arthroscopy 2015;31:944-955. [DOI] [PubMed] [Google Scholar]
- 75. Korpershoek JV, de Windt TS, Hagmeijer MH, Vonk LA, Saris DB. Cell-based meniscus repair and regeneration: at the brink of clinical translation?: A systematic review of preclinical studies. Orthop J Sports Med 2017;5:eCollection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Reguzzoni M, Manelli A, Ronga M, Raspanti M, Grassi FA. Histology and ultrastructure of a tissue-engineered collagen meniscus before and after implantation. J Biomed Mater Res B Appl Biomater 2005;74:808-816. [DOI] [PubMed] [Google Scholar]
- 77. Verdonk PCM, Can Laer MEE, Verdonk R. Meniscus replacement: from allograft to tissue engineering. Sport-Orthop-Traumatol 2008;24:78-82. [Google Scholar]
- 78. Verdonk R, Verdonk P, Huysse W, Forsyth R, Heinrichs EL. Tissue ingrowth after implantation of a novel, biodegradable polyurethane scaffold for treatment of partial meniscal lesions. Am J Sports Med 2011;39:774-782. [DOI] [PubMed] [Google Scholar]
- 79. Stone KR, Steadman JR, Rodkey WG, Li ST. Regeneration of meniscal cartilage with use of a collagen scaffold. Analysis of preliminary data. J Bone Joint Surg [Am] 1997;79-A:1770-1777. [DOI] [PubMed] [Google Scholar]
- 80. Groot JH, Vrijer R, Pennings AJ, Klompmaker J, Veth RPH, Jansen HWB. Use of porous polyurethanes for meniscal reconstruction and prosthesis. Biomaterials 1996;17:162-173. [DOI] [PubMed] [Google Scholar]
- 81. Verdonk P, Beaufils P, Bellemans J, et al. Successful treatment of painful irreparable partial meniscal defects with a polyurethane scaffold: two-year safety and clinical outcomes. Am J Sports Med 2012;40:844-853. [DOI] [PubMed] [Google Scholar]
- 82. Dhollander A, Verdonk P, Verdonk R. Treatment of painful, irreparable partial meniscal defects with a polyurethane scaffold. Midterm clinical outcomes and survivor analysis. Am J Sports Med 2016;44:2615-2621. [DOI] [PubMed] [Google Scholar]
- 83. Filardo G, Kon E, Perdisa F, et al. Polyurethane-based cell-free scaffold for the treatment of painful partial meniscus loss. Knee Surg Sports Traumatol Arthrosc 2017;25:459-467. [DOI] [PubMed] [Google Scholar]
- 84. Steadman JR, Rodkey WG. Tissue-engineered collagen meniscus implants: 5- to 6-year feasibility study results. Arthroscopy 2005;21:515-525. [DOI] [PubMed] [Google Scholar]
- 85. Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Benzi A, Marcacci M. Clinical outcomes and complications of a collagen meniscus implant: a systematic review. Int Orthop 2014;38:1945-1953. [DOI] [PubMed] [Google Scholar]
- 86. Wirth CJ, Milachowski KA, Weismeier K. Meniscus transplantation in animal experiments and initial clinical results. Z Orthop Ihre Grenzgeb 1986;124:508-512. [PubMed] [Google Scholar]
- 87. Canham W, Stanish W. A study of the biological behavior of the meniscus as a transplant in the medial compartment of a dog’s knee. Am J Sports Med 1986;14:376-379. [DOI] [PubMed] [Google Scholar]
- 88. Elattar M, Dhollander A, Verdonk R, Almqvist KF, Verdonk P. Twenty-six years of meniscal allograft transplantation: is it still experimental? A meta-analysis of 44 trials. Knee Surg Sports Traumatol Arthrosc 2011;19:147-157. [DOI] [PubMed] [Google Scholar]
- 89. Moens K, Dhollander A, Moens P, et al. Meniscal transplantation: still experimental surgery? A review. Acta Orthop Belg 2014;80:403-413. [PubMed] [Google Scholar]
- 90. Getgood A, LaPrade RF, Verdonk P, et al. International Meniscus Reconstruction Experts Forum (IMREF) 2015 Consensus Statement on the Practice of Meniscal Allograft Transplantation. Am J Sports Med 2016;45:1195-1205. [DOI] [PubMed] [Google Scholar]
- 91. Verdonk PC, Demurie A, Almqvist KF, et al. Transplantation of viable meniscal allograft. Surgical technique. J Bone Joint Surg [Am] 2006;88-A(Suppl):109-118. [DOI] [PubMed] [Google Scholar]
- 92. Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy 1991;7:297-300. [DOI] [PubMed] [Google Scholar]
- 93. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg [Am] 2008;90-A:1922-1931. [DOI] [PubMed] [Google Scholar]
- 94. Bonasia DE, Pellegrino P, D’Amelio A, Cottino U, Rossi R. Meniscal root tear repair: why, when and how? Orthop Rev (Pavia) 2015;7:5792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Bolog NV, Andreisek G. Reporting knee meniscal tears: technical aspects, typical pitfalls and how to avoid them. Insights Imaging 2016;7:385-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Furumatsu T, Kamatsuki Y, Fujii M, et al. Medial meniscus extrusion correlates with disease duration of sudden symptomatic medial meniscus posterior root tear. Orthop Traumatol Surg Res 2017;103:1179-1182. [DOI] [PubMed] [Google Scholar]
- 97. Engelsohn E, Umans H, Difelice GS. Marginal fractures of the medial tibial plateau: possible association with medial meniscal root tear. Skeletal Radiol 2007;36:73-76. [DOI] [PubMed] [Google Scholar]
- 98. Kim YM, Rhee KJ, Lee JK, et al. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy 2006;22:e1-e4. [DOI] [PubMed] [Google Scholar]
- 99. Papalia R, Vasta S, Franceschi F, et al. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull 2013;106:91-115. [DOI] [PubMed] [Google Scholar]
- 100. Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 2014;42:921-926. [DOI] [PubMed] [Google Scholar]
- 101. DePhillipo NN, Cinque ME, Chahla J, et al. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med 2017;45:2233-2237. [DOI] [PubMed] [Google Scholar]
- 102. Kim JG, Han SW, Lee DH. Diagnosis and treatment of discoid meniscus. Knee Surg Relat Res 2016;28:255-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Verdonk R. The meniscus: past, present and future. Knee Surg Sports Traumatol Arthrosc 2011;19:145-146. [DOI] [PubMed] [Google Scholar]