Highlights
-
•
Portal vein arterialization may be a bridging treatment for retransplantation.
-
•
This case demonstrates feasible of portal vein arterialization in sick patient.
-
•
Portal hypertension usually occurs after portal vein arterialization.
-
•
Calibration of fistula after recovery of liver allograft should be considered.
Abbreviations: AST, aspartate transaminase; ALT, alanine transaminase; CT, computerized tomographic; CTA, computed tomography angiogram; GDA, gastroduodenal artery; HAT, hepatic artery thrombosis; MELD, Model of end stage liver disease; MRCP, magnetic resonance cholangiopancreatography; PVA, portal vein arterialization; PDS, polydioxanone
Keywords: Living donor liver transplantation, Hepatic artery thrombosis, Portal vein arterialization, Case report
Abstract
Objective
Hepatic artery thrombosis (HAT) is one of the most serious complications of liver transplantation that can potentially lead to loss of the allograft. Retransplantation is the only option when revascularization can’t be performed but the donor may be not available in the short period of time. We report the technique of using portal vein arterialization (PVA) for bridging before retransplantation. There are few reports in living donor setting.
Case description
The recipient of the liver was a 59 year old male who received an extended right lobe graft from his son. Post operative day 41, HAT was diagnosed from angiogram and liver function got rapidly worse. We decided to re-anastomose the hepatic artery but this was not possible due to a thrombosis in the distal right hepatic artery. So PVA by anastomosis of the common hepatic artery to splenic vein was performed. During the early postoperative period liver function gradually improved. Unfortunately, he died from massive GI hemorrhage one month later.
Discussion
PVA has previously been reported as being useful when revascularization was not successful. The surgical technique is not complicated and can be performed in sick patient. Liver graft may be salvaged with oxygenated portal flow and recover afterwards. However, portal hypertension after PVA seem to be an inevitable complication.
Conclusions
PVA may be a bridging treatment for retransplantation in patients whom hepatic artery reconstruction is impossible after HAT. Regards to the high morbidity after procedure, retransplantation should be performed as definite treatment as soon as possible.
1. Introduction
Hepatic artery thrombosis (HAT) is one of the most serious complications of liver transplantation that can potentially lead to loss of the allograft. This complication is more frequent in pediatric and living related liver transplantation due to the size of the vessels involved and the complexity of the operation. The incidence varies from study to study, occurring in about 4–10% of cases following transplantation [1], [2], [3]. There are a few techniques available in the management of a HAT including revascularization or retransplantation in cases of failed revascularization or where massive graft necrosis has already occurred. However, retransplantation is regarded as being a rare option in some countries due to the lack of donors. Portal vein arterialization (PVA) has previously been reported as being useful when revascularization was not successful and there was a lack of a suitable donor [4], [5]. Nevertheless, patients who underwent PVA showed high levels of morbidity and mortality [6]. From our best knowledge, we report the first case of PVA by anastomosis splenic vein and common hepatic artery in living donor setting. The present work has been reported in line with SCARE criteria [7].
2. Case report
The recipient was a 59-year-old male patient. His underlying medical conditions were a chronic hepatitis B viral infection, cirrhosis and well controlled hypertension. A liver mass was found during a transabdominal ultrasound screening program. He subsequently underwent a multiphase computed tomography (CT) scan and was diagnosed with a single early hepatocellular carcinoma with a non-tumorous portal vein thrombosis. His Model of end stage liver disease (MELD) score was 18. After discussion with him and his family, a decision was made to perform a living related liver transplant using a extended right lobe graft from his son who was a 26 years old male with no underlying medical conditions. The blood group was compatible. There was no anatomical variation indicated from computed tomography angiogram (CTA) and magnetic resonance cholangiopancreatography (MRCP). There were no post-operative complications. During the back-table procedure, the right hepatic vein and middle hepatic vein were reconstructed with the triangular shape technique. After total hepatectomy of the recipient was performed a portal vein thromboendovenectomy was done. Then, the right lobe graft was anastomosed to the inferior vena cava with polypropylene 5/0 continuous technique and to the portal vein with polypropylene 6/0 continuous technique. Unfortunately, doppler ultrasound of the portal vein did not show a good inflow. So, intra-operative portal vein anastomosis balloon dilatation and stent placement was done through the inferior mesenteric vein. After this the right hepatic artery was anastomosed to the common hepatic artery proper using the polypropylene 8/0 interrupted technique. Finally, a hepaticojejunostomy was performed using polydioxanone (PDS) 6/0 interrupted technique. Total cold ischemic time and operative time was 202 and 805 min respectively. Total blood loss was 2500 ml.
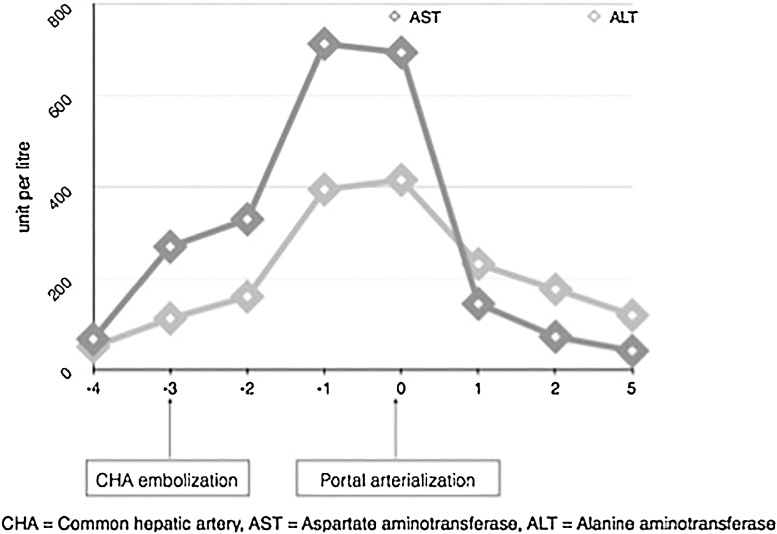
The patient was extubated at post-operative day 2 and transferred from the intensive care unit to the post-transplantation ward at post-operative day 3. The aspartate transaminase (AST) and alanine transaminase (ALT) level gradually decreased and his general clinical condition improved. However, at post-operative day 9, he experienced hypertension with sudden chest pain then collapsed. Cardio-pulmonary resuscitation was performed for 2 cycles. Spontaneous circulation returned and a CTA was performed. An aortic dissection Stanford A was found. Ascending aortic replacement with circulatory arrest was done. After the second operation, the patient’s clinical condition and liver function gradually improved until they returned to normal. However, he remained in intensive care unit due to intra-abdominal collection related to biliary leakage and sepsis. On post-operative day 41 the patient had a massive upper gastrointestinal hemorrhage with hemodynamic unstable. A gastro-duodeno scope showed massive bleeding from the duodenum and source of bleeding can’t be identified. An angiogram showed bleeding from the pseudoaneurysm of gastroduodenal artery (GDA) into the duodenum and thromboses of the hepatic artery proper. A coil embolization was done in the GDA and the common hepatic artery as shown in Fig. 1. Although, the bleeding was stopped and vital signs returned to normal, liver function got rapidly worse. Hence it was decided to re-operate to re-anastomose the hepatic artery inflow. Unfortunately, the right hepatic artery and common hepatic artery were extensively thrombosed so, portal vein arterialization was done by connection of the common hepatic artery to the splenic vein in end-to-side fashion using the polypropylene 6/0 running technique as shown in Fig. 2. During the early postoperative period liver function improved gradually as shown in Fig. 3. However, there was no deceased donor during that period. 24 days after portal vein arterialization, he experienced another massive upper gastrointestinal hemorrhage. The bleeding was identified as coming from portal hypertensive gastropathy. Embolization was carried out in the unnamed vein and also partially in the splenic artery. The patient died from recurrent upper gastrointestinal hemorrhage, uncontrolled intra-abdominal sepsis and a liver abscess one month later.
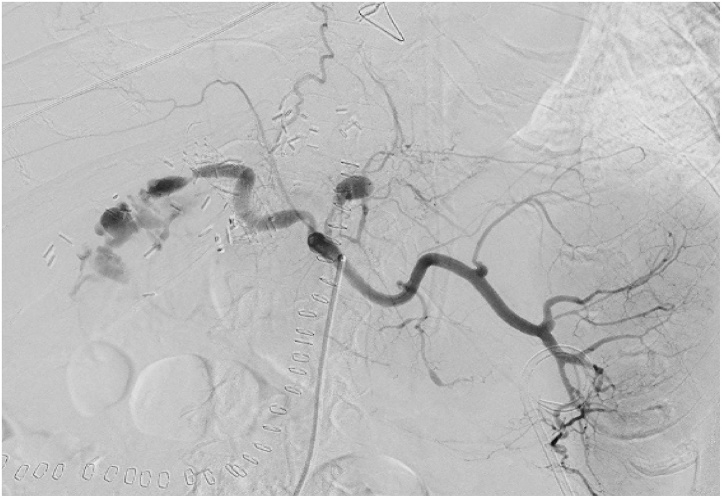
Fig. 1.
Angiogram from the celiac axis shows pseudoaneurysm at left gastric artery and active extravasation at gastroduodenal artery stump. The common hepatic artery proper can not be identified.
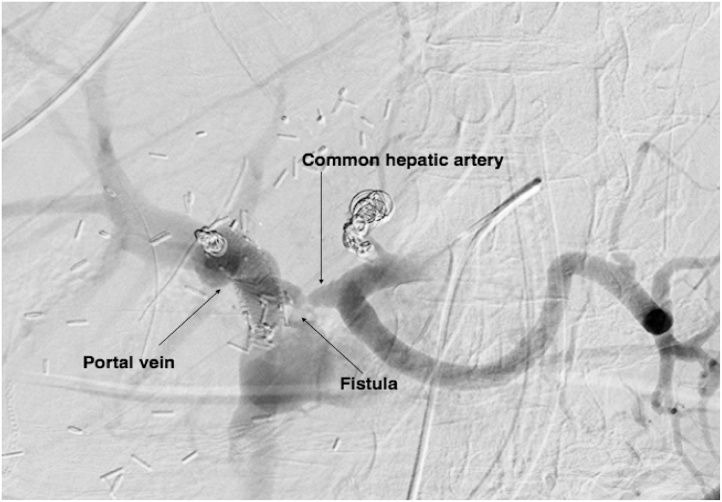
Fig. 2.
Angiogram from celiac axis after coil embolization and portal vein arterialization was carried out.
Fig. 3.
Fig. 3 shows AST and ALT level related to total hepatic de-arterialization and portal vein arterialization.
3. Discussion
The oxygenated blood supply to the liver allograft is obligated by the hepatic artery. Due to the lack of collateral vessels after liver transplantation, HAT may lead to serious complications including acute fulminant hepatic failure [8]. The incidence of HAT is higher in pediatric transplant and living donor liver transplantation regards to small size of hepatic artery [1], [9], [10]. The treatment strategy of HAT is dependent on the clinical status of the patient. The recipient of a transplant with early HAT who has markedly elevated serum transaminase levels without allograft necrosis may potentially benefit from graft salvage with emergency revascularization by surgery or endovascular treatment. However, revascularization may be impossible if there were no appropriate inflow and outflow from extensive thrombosis. In one study, only 10% of patients who had HAT can be salvaged by revascularization [11]. Retransplantation is the only option when extensive liver necrosis was developed and revascularization can’t be performed but the donor may be not available in the short period of time. Even retransplantation can be performed, 50% of cases are died because of sepsis [12]. There are several studies which show that effective treatment of HAT may be as a result of portal vein arterialization as a bridge for re-transplantation. Partial portal arterialization from side to side or end to end ileocolic artery and vein anastomosis has shown good short term results and no sign of portal hypertension for 2 months after surgery [5], [13]. Some patients developed ascites after PVA then recovered spontaneously and alive for a year [6]. However, some cases, about 44%, have demonstrated complications related to portal hypertension including upper gastrointestinal bleeding after PVA [6]. Shunt calibration was recommended by some authors to prevent sequelae from portal hypertension [14], [15]. Incidence of HAT is more frequent in living donor liver transplantation. When it occurs, hepatic artery revascularizaiton should be performed and re-transplantation should be planned. Nevertheless, in some situations such those involving extensive thromboses, revascularization cannot be done and there may also be a lack of donors for retransplantation. Portal vein arterialization is a simple and useful operation in such situations. However, this operation has a history of high morbidity especially portal hypertension associated complications and should be used as a bridging treatment for retransplantation.
From our best knowledge, there was only one case series about PVA in LDLT setting [13]. The PVA from the previous report were created with arterioportal shunt in the mesenteric vascular branch. In this case we report the technique of PVA by anastomose CHA and splenic vein in side to side fashioned. The technique is straightforward and can be perform in unstable patient like this case. The liver function was dramatically improved after PVA. Unfortunately, this case was suffered from portal hypertension afterwards resulting from PVA. This case was demonstrated even the PVA was feasible but the calibration of shunt is obviously necessary after the liver allograft recovers.
4. Conclusion
Portal vein arterialization may be a bridging treatment for retransplantation in patients whom hepatic artery reconstruction is impossible. However, retransplantation should be performed as soon as possible to avoid complication from portal hypertension.
Conflicts of interest
All authors have no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study was exempt from ethical approval in my institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Lapisatepun W; writing the paper, study concept.
Chotirosniramit A; study concept.
Sandhu T; study concept.
Udomsin K; data collection.
Ko-iam W; writing the paper.
Chantima P; study concept.
Lapisatepun Wa; study concept.
Boonsri S; study concept.
Lorsomradee S; study concept.
Kaewpoowat Q; study concept.
Junnrungsee S; writing the paper, study concept and interpretation.
Registration of research studies
This is a case report and not first in human trial.
Guarantor
Sunhawit Junrungsee.
Acknowledgments
The authors thank for all Chiang Mai Liver Transplantation members and research unit of the Department of Surgery, Faculty of Medicine, Chiang Mai University, for helping in this study.
References
- 1.Bekker J., Ploem S., de Jong K.P. Early hepatic artery thrombosis after liver transplantation: a systematic review of the incidence, outcome and risk factors. Am. J. Transplant. 2009;9(4):746–757. doi: 10.1111/j.1600-6143.2008.02541.x. [DOI] [PubMed] [Google Scholar]
- 2.Panaro F., Gallix B., Bouyabrine H., Ramos J., Addeo P., Testa G. Liver transplantation and spontaneous neovascularization after arterial thrombosis: the neovascularized liver. Transpl. Int. 2011;24(9):949–957. doi: 10.1111/j.1432-2277.2011.01293.x. [DOI] [PubMed] [Google Scholar]
- 3.Radunz S., Saner F.H., Treckmann J., Rekowski J., Theysohn J.M., Muller S. Hepatic artery and biliary complications in liver transplant recipients with radioembolization bridging treatment for hepatocellular carcinoma. Clin. Transplant. 2017:e13096. doi: 10.1111/ctr.13096. [DOI] [PubMed] [Google Scholar]
- 4.Cavallari A., Nardo B., Caraceni P. Arterialization of the portal vein in a patient with a dearterialized liver graft and massive necrosis. N. Engl. J. Med. 2001;345(18):1352–1353. doi: 10.1056/NEJM200111013451819. [DOI] [PubMed] [Google Scholar]
- 5.Melandro F., Lai Q., Levi Sandri G.B., Guglielmo N., Di Laudo M., Morabito V. A case of portal vein arterialization after a liver transplant. Exp. Clin. Transplant. 2013;11(3):287–289. doi: 10.6002/ect.2012.0172. [DOI] [PubMed] [Google Scholar]
- 6.Bhangui P., Salloum C., Lim C., Andreani P., Ariche A., Adam R. Portal vein arterialization: a salvage procedure for a totally de-arterialized liver. The Paul Brousse Hospital experience. HPB (Oxford) 2014;16(8):723–738. doi: 10.1111/hpb.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Pareja E., Cortes M., Navarro R., Sanjuan F., Lopez R., Mir J. Vascular complications after orthotopic liver transplantation: hepatic artery thrombosis. Transplant. Proc. 2010;42(8):2970–2972. doi: 10.1016/j.transproceed.2010.07.063. [DOI] [PubMed] [Google Scholar]
- 9.Heffron T.G., Welch D., Pillen T., Fasola C., Redd D., Smallwood G.A. Low incidence of hepatic artery thrombosis after pediatric liver transplantation without the use of intraoperative microscope or parenteral anticoagulation. Pediatr. Transplant. 2005;9(4):486–490. doi: 10.1111/j.1399-3046.2005.00327.x. [DOI] [PubMed] [Google Scholar]
- 10.Kamel R., Hatata Y., Taha M., Hosny K., Amin A. Major vascular complications in living-donor liver transplant recipients: single center team experience. Exp. Clin. Transplant. 2015;13(Suppl. 1):64–70. [PubMed] [Google Scholar]
- 11.Duffy J.P., Hong J.C., Farmer D.G., Ghobrial R.M., Yersiz H., Hiatt J.R. Vascular complications of orthotopic liver transplantation: experience in more than 4,200 patients. J. Am. Coll. Surg. 2009;208(5):896–903. doi: 10.1016/j.jamcollsurg.2008.12.032. discussion -5. [DOI] [PubMed] [Google Scholar]
- 12.Gunsar F., Rolando N., Pastacaldi S., Patch D., Raimondo M.L., Davidson B. Late hepatic artery thrombosis after orthotopic liver transplantation. Liver Transpl. 2003;9(6):605–611. doi: 10.1053/jlts.2003.50057. [DOI] [PubMed] [Google Scholar]
- 13.Hayashi H., Takamura H., Tani T., Makino I., Nakagawara H., Tajima H. Partial portal arterialization for hepatic arterial thrombosis after living-donor liver transplant. Exp. Clin. Transplant. 2012;10(3):247–251. doi: 10.6002/ect.2011.0173. [DOI] [PubMed] [Google Scholar]
- 14.Bonnet S., Sauvanet A., Bruno O., Sommacale D., Francoz C., Dondero F. Long-term survival after portal vein arterialization for portal vein thrombosis in orthotopic liver transplantation. Gastroenterol. Clin. Biol. 2010;34(1):23–28. doi: 10.1016/j.gcb.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y.L., Huang Z.Q., Huang X.Q., Dong J.H., Duan W.D., Liu Z.W. Effect of arterioportal shunting in radical resection of hilar cholangiocarcinoma. Chin. Med. J. (Engl.) 2010;123(22):3217–3219. [PubMed] [Google Scholar]