Abstract
Total knee arthroplasty (TKA) is a common treatment option for end-stage osteoarthritis of the tibiofemoral and patellafemoral joints. Diagnosis and treatment of the painful TKA can pose a significant challenge. In this report, we present the unusual case of a patient 12 years after total knee replacement presenting with isolated proximal tibial-fibular osteoarthritis as a cause of lateral knee pain. Proximal tibiofibular osteoarthritis is not typically on the differential diagnosis for a painful TKA but can be a rare cause of lateral knee pain. Proximal tibiofibular fusion may provide relief of pain and restoration of function.
Keywords: TKA, Painful TKA, Lateral knee pain
Introduction
Total knee arthroplasty (TKA) is a common treatment option for end-stage osteoarthritis of the tibiofemoral and patellafemoral joints. As the rate of primary TKA continues to rise, the demand for revision TKA has seen a similar trend [1]. Diagnosis and treatment of the painful TKA can pose a significant challenge [2].
Most commonly, knee replacements fail due to aseptic loosening, infection, instability, and arthrofibrosis [2], [3], [4]. Proximal tibiofibular osteoarthritis is not typically on the differential diagnosis for a painful TKA but can be a rare cause of lateral knee pain [5], [6].
In this report, we discuss the unusual case of a patient who developed lateral knee pain due to isolated proximal tibiofibular osteoarthritis 12 years after receiving a primary TKA on the same knee. We describe the surgical technique used to fuse the proximal tibiofibular joint in the setting of a prior total knee replacement.
Case history
A 71-year-old female presented with left knee pain 12 years after left TKA. The atraumatic pain began insidiously 1 year ago and had grown progressively worse despite conservative treatment options. It interfered with her ability to play tennis, because it was exacerbated with lateral motion. She presented to the surgeon who performed the primary TKA and who now had concerns for TKA failure. The patient was subsequently referred for further evaluation to the senior author (W.E.M.). On examination, she described the pain as predominantly lateral and posterior. The pain was worse with weight-bearing. She had painless range of motion of the knee while supine and no neurovascular abnormalities including normal peroneal nerve function. There was no effusion or ligamentous laxity. The patient had significant pain that was reproducible with compression of the fibular head. Laboratory assessment was without abnormality (C-reactive protein = 1.1 mg/L [normal less than or equal to 8.0 mg/L] and sedimentation rate 13 mm/h [normal 0-29 mm/h]) and there was no concern of infection. Initial plain radiographs did not demonstrate any significant radiographic findings in regards to osteolysis, loosening, or periprosthetic complication (Fig. 1a and b) related to her prosthesis. Subsequent workup with a computed tomography scan demonstrated severe degenerative changes at the proximal tibiofibular joint with no evidence of prosthetic loosening (Fig. 1c).
Figure 1.
(a and b) Preoperative plain films with anteroposterior (AP) and lateral views show no loosening of the TKA. (c) Preoperative computed tomography imaging shows a cyst in the fibular head.
The patient then underwent computed tomography–guided local anesthetic injection into the proximal tibiofibular joint. Before and after the injection, the patient was asked to perform a series of provocative movements. After the injection, the patient reported a subjective increase in the range of motion at the knee with less discomfort. At that point, a discussion was held with the patient about the likely source of pain and the possibility of fusing the proximal tibiofibular joint to address her pain.
Technique
After administration of a general anesthetic and skin antisepsis, a tourniquet was inflated. A large curvilinear incision over the fibular head was made extending proximally and distally beyond the fibular head. We carried the dissection down sharply to the subcutaneous fat. We identified the fascia of the biceps femoris and dissected posteriorly, where the peroneal nerve was identified. The nerve was dissected distally and tagged with a Vesi-Loop that aided in identification throughout the case (Fig. 2a). We then dissected anterior to the fibular head, identifying the tibiofibular joint. Using a rongeur and curette, we resected the joint and sent samples for pathological analysis. Analysis of a permanent path specimen demonstrated features consistent with osteoarthritis with no signs of a cyst or neoplastic lesion.
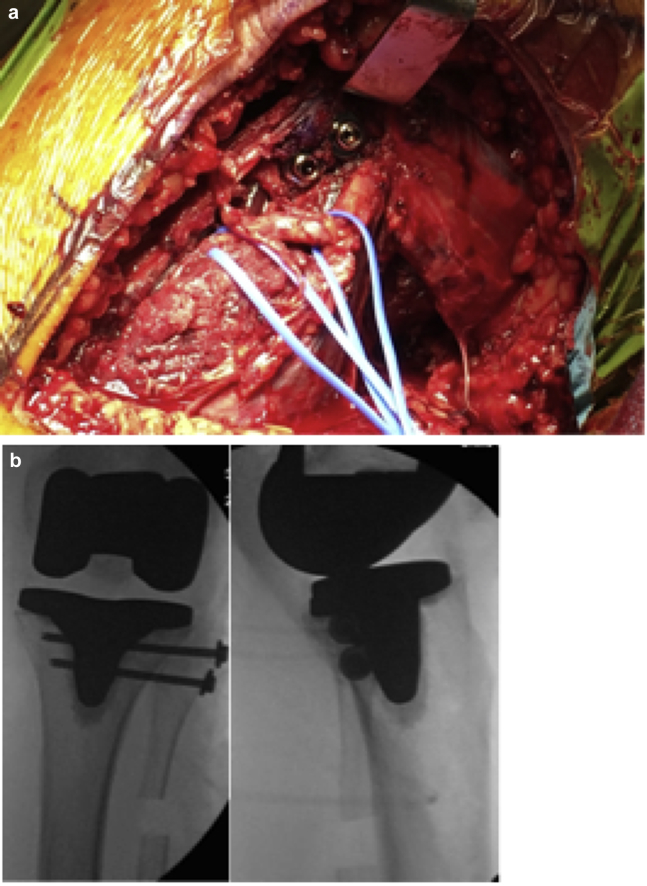
Figure 2.
(a) Intraoperative photograph showing fixation hardware. (b) AP and lateral knee images showing screw fixation of the proximal fibula to the proximal tibia.
A fibular ostectomy was performed to help offload the joint while weight-bearing. We dissected distally on the fibula approximately 5-7 cm. Care was taken to protect the peroneal nerve. A subperiosteal dissection was performed, and small Bennet retractors were placed around the fibula to protect the surrounding soft-tissue structures. Intraoperative fluoroscopy confirmed the location of our planned cut, and before ostectomy, we protected the distal peroneal nerve and tracked its course proximally to the fibular head. Using a microsagittal saw, we removed approximately 1 cm of the bone from the fibula in the region of the metaphyseal-diaphyseal junction.
Under fluoroscopic guidance, 2 guidewires were then placed through the fibular head into the tibia, directing them posterior to the keel of the implant and parallel to the joint. We morselized the resected bone, mixed it with 10 mL of allograft bone chips, and then packed the graft into the tibiofibular joint. The screws' lengths were determined using a depth gauge, and a cannulated drill was placed over the wires. We then achieved compression of the graft using two 4.5 mm cannulated screws placed across the tibiofibular joint. The position of the screws was confirmed using fluoroscopy (Fig. 2b). We removed the guidewires, irrigated the surgical site, deflated the tourniquet, and obtained hemostasis using electrocautery. The wound was then closed in layers. The patient was placed into a hinged knee brace with no limits on flexion and extension. She was kept limited weight-bearing for 3 months.
Outcomes
The patient was kept overnight in the hospital and discharged the next day. Shortly after surgery, she reported a significant improvement in her pain. Postoperatively, she had some transient peroneal nerve weakness that resolved over time without intervention. At 6 months, she had no pain with weight-bearing, was back to activity including tennis and golf, and had no evident peroneal nerve weakness. Radiographs are shown in Figure 3.
Figure 3.
Six month follow-up radiograph (AP [a], lateral [b], and sunrise [c]) demonstrating a successful fusion of the fibula and tibia.
Discussion
Revision arthroplasty after TKA has serious consequences both clinically and economically. Each TKA revision costs $49,000 or more, and hospital charges for revision knee arthroplasty for osteoarthritis are $2.7 billion annually [1]. Indications for revision TKA include aseptic and septic causes, with the latter accounting for 25%-31% of cases [2], [3], [4]. Despite the many known indications for TKA revision and causes for TKA failure, proximal tibiofibular osteoarthritis is not typically thought of as a cause of the painful TKA. As outlined in this case, this can undoubtedly lead to pain around a previously well-functioning TKA. A review of the literature regarding the basic science, epidemiology, and surgical treatment of the tibiofibular joint informs our approach to our patient.
Recent biomechanical studies have brought attention to the role of the proximal tibiofibular joint both in health and states of disease [5], [6], [7]. Cadaveric studies provide evidence that the joint experiences significant rotational stress even in healthy individuals and provides a stabilizing role analogous to the distal tibiofibular joint. In a robotic cadaveric model, TKA balancing altered tibiofibular kinematics [7]. Future biomechanical studies may help further characterize how altered motion can affect the long-term health of the joint. Cadaveric-radiologic investigation has provided insight into the structure of the joint [8]. Researchers have shown that up to 10% of patients may have a channel of communication between the primary knee joint and proximal tibiofibular joint, and this may provide an avenue for extension of infectious and inflammatory conditions between the 2 compartments [9].
Emerging clinical and epidemiological evidence suggests proximal tibiofibular osteoarthritis may represent an underappreciated cause of posterior and lateral knee pain [8]. For example, patients with presumed peroneal nerve dysfunction have been later found to suffer from tibiofibular articular pathology [10]. While patients with proximal tibiofemoral osteoarthritis classically present with lateral knee pain, studies have correlated posterior knee pain with imaging consistent with the disease [11]. Prior literature has described arthritis of this joint secondary to trauma, idiopathic dislocations, and inflammatory conditions, but primary osteoarthritis of this joint can also occur. In all primary or revision TKA candidates, clinical evaluation of the joint and review of standard plain film radiographs can inform the need for advanced imaging. Clinicians can often rule-out compressive neuropathy based on the absence of sensory and motor signs. Radiographic plain film findings include articular erosion in the tibiofibular joint and concurrent dislocation [12]. Magnetic resonance imaging provides an additional imaging modality in suspected cases in which plain films are not definitive [9], [11], [12].
In our survey of the literature, the authors have reported cases of successful treatment of inflammatory and traumatic proximal tibiofibular instability with proximal tibiofibular fusion, although nonoperative treatment and reconstruction represent alternative options [13], [14]. The authors have described the use of arthrodesis to successfully treat recurrent cysts in the same location [15], [16]. Most of the prior literature has reported on patients in native knees with or without a history of underlying tibiofibular instability. The authors have reported using arthrodesis alone to treat the condition in a post-TKA patient [17]. Many authors advocate the addition of fibular ostectomy to address the theoretical risk of increased stress on the distal tibiofibular joint after proximal arthrodesis, and we concur with this suggestion [14], [15], [16].
Summary
Tibiofibular disease likely represents an uncommon cause of lateral knee pain after TKA. Radiographic findings include articular erosion with or without joint dislocation. We report successful resolution of pain following fusion of the proximal tibiofibular joint with fibular ostectomy.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2018.02.006.
Appendix A. Supplementary data
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Bozic K.J., Kamath A.F., Ong K. Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res. 2015;473(6):2131. doi: 10.1007/s11999-014-4078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan M., Osman K., Green G., Haddad F.S. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J. 2016;98-B(1 Suppl A):105. doi: 10.1302/0301-620X.98B1.36293. [DOI] [PubMed] [Google Scholar]
- 4.Kim K.T., Lee S., Ko D.O., Seo B.S., Jung W.S., Chang B.K. Causes of failure after total knee arthroplasty in osteoarthritis patients 55 years of age or younger. Knee Surg Relat Res. 2014;26(1):13. doi: 10.5792/ksrr.2014.26.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lambert K.L. The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am. 1971;53(3):507. [PubMed] [Google Scholar]
- 6.Scott J., Lee H., Barsoum W., van den Bogert A.J. The effect of tibiofemoral loading on proximal tibiofibular joint motion. J Anat. 2007;211:647. doi: 10.1111/j.1469-7580.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barosum W.K. Robotic testing of proximal tibio-fibular joint kinematics for Measuring instability following total knee arthroplasty. J Orthop Res. 2011;29:47. doi: 10.1002/jor.21207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oztuna V., Yildiz A., Ozer C., Milcan A., Kuyurtar F., Turgut A. Involvement of the proximal tibiofibular joint in osteoarthritis of the knee. Knee. 2003;10:347. doi: 10.1016/s0968-0160(03)00004-8. [DOI] [PubMed] [Google Scholar]
- 9.Resnick D., Newell J.D., Guerra J.Jr, Danzig L.A., Niwayama G., Goergen T.G. Proximal tibiofibular joint: anatomic-pathologic-radiographic correlation. Am J Roentgenol. 1978;131:133. doi: 10.2214/ajr.131.1.133. [DOI] [PubMed] [Google Scholar]
- 10.Özcan Ö., Eroglu M., Boya H., Kaya Y. Proximal tibiofibular joint pain versus peroneal nerve dysfunction: clinical results of closed-wedge high tibial osteotomy performed with proximal tibiofibular joint disruption. Knee Surg Sports Traumatol Arthrosc. 2017;25:2936. doi: 10.1007/s00167-016-4066-5. [DOI] [PubMed] [Google Scholar]
- 11.Nozkurt M., Yilmaz E., Akseki D., Havitcioğlu H., Günal I. The evaluation of the proximal tibiofibular joint for patients with lateral knee pain. Knee. 2004;11:307. doi: 10.1016/j.knee.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Boya H., Ozcan O., Oztekin H.H. Radiological evaluation of the proximal tibiofibular joint in knees with severe primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2008;16:157. doi: 10.1007/s00167-007-0442-5. [DOI] [PubMed] [Google Scholar]
- 13.Dennis J.B., Rutledge B.A. Bilateral recurrent dislocations of the tibiofibular joint with peroneal-nerve palsy: a case summary. J Bone Joint Surg. 1958;40:1146. [PubMed] [Google Scholar]
- 14.Delos D., Schneidkraut J., Rodeo S. Successful fusion of the proximal tibiofibular joint with osteogenic protein-1 (OP-1) augmentation. HSS J. 2013;9:90. doi: 10.1007/s11420-012-9271-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miskovsky S., Kaeding C., Weis L. Proximal tibiofibular joint ganglion cysts: excision, recurrence, and joint arthrodesis. Am J Sports Med. 2004;32(4):1022. doi: 10.1177/0363546503258706. [DOI] [PubMed] [Google Scholar]
- 16.Lateur, G. Pailhé R, Refaie R, et al. Ganglion cysts of the proximal tibiofibular articulation: the role of arthrodesis and combined partial fibular excision [Epub ahead of print]. Int Orthop. https://doi.org/10.1007/s00264-017-3542-y, accessed December 1, 2017. [DOI] [PubMed]
- 17.Bedard M., Corriveau S. Instability of the proximal tibiofibular joint associated with total knee arthroplasty. Arthroplast Today. 2016;2:93. doi: 10.1016/j.artd.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.