Abstract
Background
To assess the relationship between rapidly destructive osteoarthritis (RDOA) of the hip and intra-articular steroid injections.
Methods
Coding records from 2000 to 2013 were used to identify all subjects who had a fluoroscopy-guided intra-articular hip injection to treat pain associated with primary osteoarthritis. Radiographic measurements from preinjection and postinjection imaging were evaluated with Luquesne's classification of RDOA to determine diagnosis (greater than 50% joint space narrowing or greater than 2 mm of cartilage loss in 1 year with no other forms of destructive arthropathy). Demographic information, health characteristics, and number of injections were collected and analyzed as other potential explanatory variables. Patient outcome assessed by need for total hip arthroplasty (THA) after injection was also recorded.
Results
One hundred twenty-nine injection events met the inclusion criteria in a total of 109 patients. From this sample, 23 cases of RDOA were confirmed representing a 21% incidence of RDOA. Twenty-one of the patients (91%) with RDOA had a THA at a median time of 10.2 months (interquartile range: 6.5-11.2) compared with 27 (31%) of those without RDOA at a median time of 24.9 months (interquartile range: 15.3-65.3). Older patients, patients with more severe osteoarthritis, and patients who identified themselves as white were more likely to have a diagnosis of RDOA (P = .008; P = .040; P = .009, respectively).
Conclusions
The potential for RDOA and faster progression to THA raises questions about the use of intra-articular steroid injections for hip osteoarthritis and should be discussed with patients. Additional studies are needed to define a true relationship.
Keywords: Rapidly destructive osteoarthritis, Total hip arthroplasty, Intra-articular injections, Steroids
Introduction
Rapidly destructive osteoarthritis (RDOA) of the hip is a debilitating and rare condition that is not fully understood. It was first mentioned in 1957 by Forestier [1]. Several reports soon followed, describing similar conditions with different nomenclature [2]. However, it was Lequesne who provided the most complete and standardized definition of greater than 50% joint space narrowing or greater than 2 mm of cartilage loss in 1 year with no other forms of destructive arthropathy identified [3].
RDOA of the hip has classically been seen in elderly females with a higher Kellgren and Lawrence (KL) [4] score at initial presentation with a tendency for unilateral involvement [5], [6]. However, the true incidence is unknown and may be as high as 16% [7]. Several risk factors leading to RDOA of the hip have been theorized including osteopenia and/or osteoporosis [8], [9], inversion of the acetabular labrum [10], [11], increased posterior pelvic tilt [12], idiopathic chondrolysis [13], intra-articular deposition of hydroxylapatite or pyrophosphate crystals [14], [15], [16], and intra-articular steroid injections [17], [18], [19]. RDOA of the hip initially presents with subjective and radiographic findings of osteoarthritis [20]. However, the rapid radiographic progression is also associated with severe femoral head and acetabular destruction that may involve a more complicated reconstructive procedure characterized by significant acetabular bone loss, increased blood loss, longer operative times, and the need for special implants [7].
The evidence supporting intra-articular steroid injections for painful hip osteoarthritis is mixed. Intra-articular steroid injections have been suggested as an effective and cost-saving treatment for symptomatic management of hip osteoarthritis, no matter the severity [21]. Deshmukh et al [22] found these steroid injections to offer better pain relief in those with more advanced hip osteoarthritis. In contrast, however, McCabe et al [23] performed a systematic review of the literature and concluded that intra-articular steroid injections may produce short-term pain relief and lead to a slight improvement in function; however, the quality of evidence was poor.
Intra-articular steroids have previously been implicated with chondrolysis and have also been postulated as a potential cause for RDOA. With few reports in the literature, the purpose of this study is to determine if there is a relationship between RDOA of the hip and intra-articular steroid injections and to evaluate radiographic changes in the hip joint after steroid injections.
Material and methods
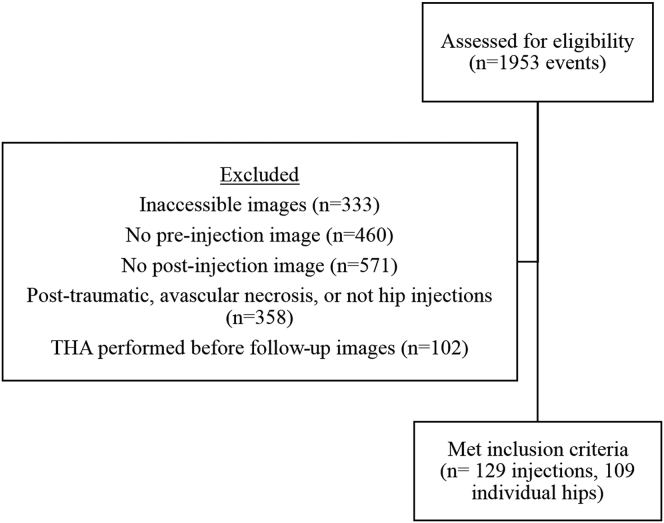
This retrospective cohort trial was approved by the local institutional review board. Following institutional review board's approval, the radiology department provided a comprehensive list of all hip injections between the years of 2000 and 2013. This resulted in 1953 events that were reviewed by the authors; however, only 129 (6.6%) were hip injections that met our inclusion criteria (Fig. 1). To be included in this study, patients required, at a minimum, radiographs within 6 months before and 1 year after the injection. Injections must have contained a steroid mixture and been injected into the femoroacetabular joint for diagnostic and or therapeutic purposes under fluoroscopic guidance. The active steroid medication was 1 mL of triamcinolone with a concentration of 40 mg/mL. Those with a diagnosis of post-traumatic osteoarthritis, inflammatory arthritis, osteonecrosis, who were undergoing infection workup, and who received previous hip surgery (including arthroscopy) were excluded from the group.
Figure 1.
Flowchart for patient selection process.
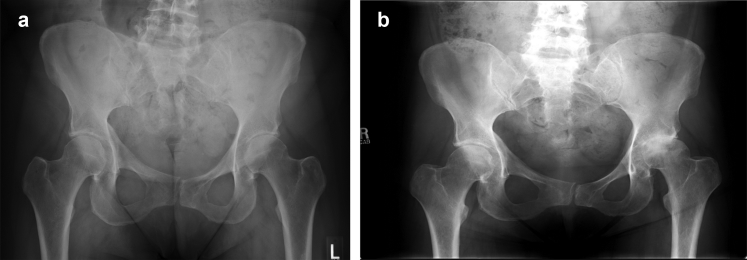
The primary outcomes of this study were the diagnosis of RDOA of the hip (Fig. 2a and b) and the occurrence of total hip arthroplasty (THA). RDOA of the hip was confirmed by progressive loss of cartilage (greater than 2 mm or 50% joint space narrowing) over a 12-month period or less. The time (months) between first injection and RDOA diagnosis and the time (months) between first injection and THA were considered as a secondary outcome.
Figure 2.
(a) Sixty-year-old woman with left hip pain; (b) 1 month after receiving a left hip intra-articular steroid injection.
Demographic information and health characteristics, including age at injection (years), sex (male, female), race (white, non-white), and body mass index (BMI; kg/m2) were collected as potential explanatory variables. The number of injections after the first was included to determine if there was an additive effect.
Trained study personnel reviewed preinjection radiographs to measure the lateral center edge angle (LCEA), KL score of osteoarthritis [4], and joint space in millimeters. LCEA was measured according to Clohisy et al [24]. The KL score ranges from 0 to 4, with higher scores indicating more severe osteoarthritis. The joint space was measured at the narrowest aspect of the weight-bearing dome (anywhere along the sourcil) in all cases for consistency. Postinjection images were also analyzed for loss of joint space. Those cases identified as having RDOA of the hip were reviewed by the study personnel to ensure diagnosis consensus.
Statistical analysis
All study variables were summarized by means and standard deviations or frequencies and proportions. Medians and interquartile ranges were used to summarize the time from first injection to the diagnosis of RDOA (as defined as date of last image) as measured by a Kaplan–Meier survival curve. Simple logistic regression models were used to assess the marginal relationship between each of the demographic, injury, and health characteristics with RDOA status and arthroplasty. RDOA of the hip diagnosis was considered as a predictor of arthroplasty. Multivariable models for each outcome were constructed with each explanatory variable that had a corresponding P-value from the marginal models that was <.25. Sensitivity analyses were performed using both the time from first injection until diagnosis of RDOA and the time from first injection until arthroplasty. A time-varying covariate method was used to assess the proportional hazards assumption. The statistical software SAS, version 9.4 (Cary, NC) was used for all statistical methods.
Results
One hundred twenty-nine injection events met the inclusion criteria in a total of 109 patients. Intra-articular injection composition and other summaries are reported in Tables 1 and 2. Overall, 23 patients (21%) had an RDOA diagnosis and 48 (44%) had a THA. Twenty-one of the patients (91%) with RDOA had a THA and 27 (31%) of those without RDOA had a THA (Table 3). The median time until THA can bee seen in Table 3.
Table 1.
Intra-articular injection composition for the entire study group and for those diagnosed with RDOA.
| Injection for entire study groupa | Number of injections (n = 129) | Percentage of total injections (%) |
|---|---|---|
| 40-mg triamcinolone acetonide/4 mL 1% Lidocaine | 93 | 72.1 |
| 40-mg triamcinolone acetonide/4 mL 0.25% bupivacaine | 25 | 19.4 |
| 40-mg triamcinolone acetonide/2 mL 0.25% bupivacaine | 3 | 2.3 |
| 40-mg triamcinolone acetonide/4 mL 0.2% ropivacaine | 4 | 3.1 |
| Other |
4 |
3.1 |
| Injection for RDOA groupa |
Number of injections (n = 27) |
Percentage of total injections (%) |
| 40-mg triamcinolone acetonide/4 mL 1% Lidocaine | 21 | 77.8 |
| 40-mg triamcinolone acetonide/4 mL 0.25% bupivacaine | 5 | 18.5 |
| 40-mg triamcinolone acetonide/2 mL 0.25% bupivacaine | 1 | 3.7 |
All injections were without epinephrine.
Table 2.
Summary statistics for each explanatory variable.
| Characteristic | Level | Summary |
|---|---|---|
| Sex | Male | 29 (27%) |
| Female | 80 (73%) | |
| Race | White | 67 (61%) |
| Non-white | 42 (39%) | |
| Extra injection | Yes | 16 (15%) |
| No | 93 (85%) | |
| KL score | 2.2 (1.1) | |
| Age | 53.9 (13.5) | |
| LCEA | 31.6 (8.6) | |
| BMI | 30.1 (7.9) |
Summaries are means (standard deviations) or frequencies and percentages.
Table 3.
RDOA of the hip and THA in those patients who received an intra-articular steroid injection.
| RDOA | No RDOA | |
|---|---|---|
| Patient diagnoses | 21% (23/109) | 79% (86/109) |
| Progression to THA | 91% (21/23) | 31% (27/86) |
| Median time to THA | 10.2 mo (IQR: 6.5-11.2) | 24.9 mo (IQR: 15.3-65.3) |
IQR, interquartile range.
The marginal relationships between each of the demographic, injury, and health characteristics with RDOA status are reported in the upper portion of Table 4. Older patients, patients with more severe osteoarthritis (based on KL score), and patients who identified themselves as white were more likely to have a diagnosis of RDOA (P = .008; P = .040; P = .009, respectively). Gender was not associated with an RDOA diagnosis, and no relationship was observed between RDOA status and the occurrence of more than one injection in the same joint, LCEA, and BMI. Similar results were observed in the multivariable model. Self-identified race (white) (odds ratio [OR] = 6.24, 95% confidence interval (CI): 1.58-24.7), patients with higher KL scores (OR = 1.75, 95% CI: 1.04-2.93), and age (OR = 1.30, 95% CI: 1.02-1.65) had higher odds of an RDOA diagnosis. The multivariate regression model had adequate fit (P = .624) and had a c-statistic of 0.806.
Table 4.
Results from the unadjusted and adjusted logistic regression models predicting the presence of RDOA and arthroplasty.
| Characteristic | Comparison | Unadjusted |
Adjusted |
||
|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | ||
| RDOA diagnosis | |||||
| Sex | Male – Female | 2.12 (0.80-5.63) | .131 | 2.64 (0.85-8.23) | .095 |
| Race | White – Non-white | 5.53 (1.53-20.0) | .009 | 6.24 (1.58-24.7) | .009 |
| Extra injection | Yes – No | 1.30 (0.38-4.48) | .680 | - | - |
| KL score | (1 unit increase) | 1.58 (1.02-2.43) | .040 | 1.75 (1.04-2.93) | .035 |
| Age | (5 y increase) | 1.37 (1.10-1.72) | .008 | 1.30 (1.02-1.65) | .034 |
| LCEA | (1 unit increase) | 0.97 (0.92-1.03) | .345 | - | - |
| BMI | (1 unit increase) | 0.98 (0.92-1.04) | .548 | - | - |
| Arthroplasty | |||||
| RPOA | Yes – No | 22.9 (2.02-105) | <.001 | 19.1 (3.68-99.3) | <.001 |
| Sex | Male – Female | 1.26 (0.54-2.96) | .592 | - | - |
| Race | White – Non-white | 2.44 (1.08-5.49) | .031 | 2.15 (0.76-6.03) | .148 |
| Extra injection | Yes – No | 1.78 (0.61-5.19) | .291 | - | - |
| KL score | (1 unit increase) | 2.48 (1.64-3.75) | <.001 | 2.60 (1.61-4.19) | <.001 |
| Age | (5 y increase) | 1.09 (0.94-1.26) | .234 | 0.89 (0.73-1.08) | .242 |
| LCEA | (1 unit increase) | 0.98 (0.94-1.03) | .441 | - | - |
| BMI | (1 unit increase) | 1.00 (0.95-1.05) | .925 | - | - |
OR, odds ratio.
All variables with P < .25 in the unadjusted models were included in the adjusted models. Values in bold are statistically significant at a P-value of <.05.
In the marginal models predicting THA, only RDOA status, race, and KL score were significant (P < .001; P = .031; P < .001, respectively) (lower portion of Table 4). Those with an RDOA diagnosis, self-identified as white, and had more severe osteoarthritis at first injection were more likely to have a THA. In the adjusted model, those with an RDOA diagnosis (P < .001) and with a higher KL score (P < .001) were predictors of THA. Patients diagnosed with RDOA of the hip had 19.1 times higher odds (95% CI: 3.68-99.3) than those without a RDOA of the hip diagnosis of eventually having a THA, while 1 unit increases in the KL score were related to a 2.48 (95% CI: 1.64-3.75) times higher odds of having a THA. No other variables were significantly related to THA. The model had adequate fit (P = .509) and had a c-statistic of 0.872.
Discussion
RDOA of the hip is a phenomenon that is not well understood. It is a debilitating condition that results in rapid destruction of the femoroacetabular joint, leading to pain and decline in function, ultimately resulting in THA. First described in 1957 [1], this condition is usually diagnosed when there is greater than 50% joint space narrowing or greater than 2 mm of cartilage loss in 1 year with no other forms of destructive arthropathy identified [3]. With many proposed etiologies, it has been classically seen as a unilateral condition in elderly females with a higher KL score at presentation [5], [6]. In 2013, Pivec et al [20] noted only 20 published reports in the literature. Furthermore, no publications have completely elucidated the etiology of RDOA nor have they demonstrated successful nonarthroplasty management options [7], [20], [25], [26], [27].
The results of our data set suggest that 21% of patients who have an intra-articular steroid hip injection develop RDOA of the hip (Fig. 2). Whether this is causal or coincidental is not clear; however, in most cases the intra-articular injection did not prolong the time to arthroplasty. We found that older patients who had a higher KL score at presentation and who identified themselves as white were more likely to be diagnosed. In essence, as age and KL score increase, the likelihood of RDOA of the hip after intra-articular steroid injection increases. Our data showed no association with male or female sex, which is contradictory to previous data [5], [6]. Multiple injections, LCEA, and BMI appeared to have no relationship with diagnosis of RDOA of the hip. We found that patients diagnosed with RDOA of the hip had almost 20 times higher odds of having THA than those without an RDOA of the hip diagnosis, which intuitively makes sense as the arthritic process progressed significantly. Using THA as a proxy for effectiveness of injections, 44% of patients ended up with a THA within our study period. The median time until THA was shorter in RDOA of the hip patients at 10.2 months than in those without RDOA of the hip at 24.9 months.
The efficacy of intra-articular steroid injections is not clear. However, previous studies have showed that the pain relief is greater with more severe arthritis [22]. Our study shows that with severe disease, many progressed quickly to THA and therefore, the benefit of an intra-articular steroid injection should be called into question. Furthermore, a recent randomized clinical trial showed that intra-articular knee injections of triamcinolone led to significantly greater cartilage loss than its saline control, with no change in pain improvement or patient-reported outcomes [28].
There are few reports in the literature suggesting a linkage between intra-articular steroid injection and RDOA. Laroche et al [18] presented 2 cases where osteonecrosis of the femoral head developed after multiple intra-articular injections of triamcinolone acetonide. However, the intra-articular injections were provided to other major joints and not the femoroacetabular joint, suggesting a possible mechanism of cortisol excess from long-acting corticosteroids. McCarty et al [19] describe the case of a 67-year-old white woman, who had received a total of 120 mg of triamcinolone hexacetonide to each knee over a 4-month period, subsequently developed osteonecrosis of her distal femur and proximal tibia. Yamamoto et al [17] describe a case of a 50-year-old woman with a BMI of 29.4 kg/m2 and minimal hip osteoarthritis, who had rapid collapse of her femoral head within 3 months after a single intra-articular steroid injection. The injection consisted of Depo-Medrol (methylprednisolone acetate 80 mg) and Sensorcaine (0.5%) at an unknown amount. Interestingly, this patient was also described to have osteopenia at the time of injection.
Villoutreix et al [27] evaluated the role of intra-articular steroids in 24 patients who already had a diagnosis of RDOA in 28 hips. These patients were provided intra-articular steroid injections with or without weight-bearing restrictions to evaluate the effect on timing of THA. They found that intra-articular steroid injections with or without weight-bearing restrictions did not change the need for THA and furthermore, intra-articular steroid injections did not accelerate the course of hip destruction. Therefore, a relationship between intra-articular steroid injections into the femoroacetabular joint and RDOA is not clear.
A recent case series by Hart and Fehring [29] discussed the clinical implication that RDOA can be confused with septic arthritis. Intraoperatively, they found that there can be a fluid that mimics infection and propose an algorithm for diagnosis that includes preoperative erythrocyte sedimentation rate and C-reactive protein and if elevated a hip aspirate to rule out infection and avoid unnecessary two-stage procedures. Fully understanding the risk factors and inciting events for RDOA will hopefully help differentiate between infectious cases of rapid joint destruction.
At our institution, the total hospital and professional charges are approximately $3108.00 for a single fluoroscopy-guided intra-articular hip steroid injection. In addition, if a patient develops RDOA of the hip, we know they require THA at an earlier interval compared with those who do not develop RDOA of the hip. This is concerning, given the current state of health care in regard to cost containment and value-based health care. If patients at risk for RDOA of the hip are being provided intra-articular steroid injections into the femoroacetabular joint, the cost-benefit ratio may not be justified.
This study has several limitations. First, while our data suggest an incidence of RDOA of the hip of 21%, our sample size was small and may not be generalizable. Our population was from a single institution; therefore, the incidence is for 1 particular clinic and should not be interpreted as a population incidence. Second, the retrospective nature of this study leads to including a small fraction of the original data set. Out of the 1953 injection events available for review, only 129 injection events (6.6%) met the inclusion criteria. Four hundred sixty events were excluded because of a diagnosis of osteonecrosis, post-traumatic arthritis, or were mislabeled (the injection was to a different part of the body). One hundred two patients were excluded due to a lack of postinjection imaging before undergoing THA. A majority of the exclusions, however, were due to having either inadequate images or having inaccessible images. Requests were made to unarchive missing images; however, only a small portion of these could be uploaded back onto the image-viewing system. This is a potential source of selection bias for patients with severe symptomatology who might obtain more frequent imaging. Third, the subjective element of radiographic measurements inherently creates potential for error. While measurement technique was standardized, the reliability of these measurements depends on the accuracy of the radiographic images. These measurements could be affected by multiple variables including rotation, distance to imaging source, and magnification. Finally, the retrospective nature of this study did not allow for either a control group or randomization of patients. The radiographic progression of joint space loss could represent the natural evolution of the more traditional arthritic process and might not be truly the disease process known as “RDOA”. The choice of steroid and anesthetic were not standardized, so any relationship between RDOA of the hip and injection composition is difficult to truly identify. Future prospective randomized controlled studies are needed to show causation and to help control for bias.
Conclusions
Despite the limitations of this study, a 21% incidence of RDOA of the hip in patients receiving intra-articular steroid injections merits several considerations. Patients contemplating intra-articular steroid injections into the hip should be educated about the possibility of RDOA of the hip or progression of preexisting arthritic process, especially those who are elderly or have higher preinjection KL scores. Finally, given the relatively high progression to THA within 1 year, the cost-effectiveness and safety of this treatment needs scrutiny.
Acknowledgments
We would like to acknowledge Dr. Adam Sima for help with statistical analysis.
Footnotes
One or more of the authors of this article have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field, which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2017.12.002.
Appendix A. Supplementary data
References
- 1.Forestier F. 1957. Coxite rhumatismales subaigues et chnoniques. [Thesis]. Paris. [Google Scholar]
- 2.Delia Torre P., Picuti G., Di Filippo P. Rapidly progressive osteoarthritis of the hip. Ital J Orthop Traumatol. 1987;13:187. [PubMed] [Google Scholar]
- 3.Lequesne M. Rapid destructive coxarthritis. Rhumatologie. 1970;22:51. [PubMed] [Google Scholar]
- 4.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenberg Z.S., Shankman S., Steiner G.C., Kastenbaum D.K., Norman A., Lazansky M.G. Rapid destructive osteoarthritis: clinical, radiographic, and pathologic features. Radiology. 1992;182:213. doi: 10.1148/radiology.182.1.1727284. [DOI] [PubMed] [Google Scholar]
- 6.Ledingham J., Dawson S., Preston B., Milligan G., Doherty M. Radiographic progression of hospital referred osteoarthritis of the hip. Ann Rheum Dis. 1993;52:263. doi: 10.1136/ard.52.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Batra S., Batra M., McMurtrie A., Sinha A. Rapidly destructive osteoarthritis of the hip joint: a case series. J Orthop Surg Res. 2008;3:3. doi: 10.1186/1749-799X-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamamoto T., Bullough P.G. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42:2719. doi: 10.1002/1529-0131(199912)42:12<2719::AID-ANR31>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T., Bullough P.G. The role of subchondral insufficiency fracture in rapid destruction of the hip joint: a preliminary report. Arthritis Rheum. 2000;43:2423. doi: 10.1002/1529-0131(200011)43:11<2423::AID-ANR8>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 10.Fukui K., Kaneuji A., Fukushima M., Matsumoto T. Inversion of the acetabular labrum triggers rapidly destructive osteoarthritis of the hip: representative case report and proposed etiology. J Arthroplasty. 2014;29:2468. doi: 10.1016/j.arth.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Fukui K., Kaneuji A., Fukushima M., Matsumoto T. Early MRI and intraoperative findings in rapidly destructive osteoarthritis of the hip: a case report. Int J Surg Case Rep. 2015;8:13. doi: 10.1016/j.ijscr.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watanabe W., Itoi E., Yamada S. Early MRI findings of rapidly destructive coxarthrosis. Skeletal Radiol. 2002;31:35. doi: 10.1007/s00256-001-0445-0. [DOI] [PubMed] [Google Scholar]
- 13.Komiya S., Inoue A., Sasaguri Y., Minamitani K., Morimatsu M. Rapidly destructive arthropathy of the hip. Studies on bone resorptive factors in joint fluid with a theory of pathogenesis. Clin Orthop Relat Res. 1992:273. [PubMed] [Google Scholar]
- 14.Dieppe P.A., Doherty M., Macfarlane D.G., Hutton C.W., Bradfield J.W., Watt I. Apatite associated destructive arthritis. Br J Rheumatol. 1984;23:84. doi: 10.1093/rheumatology/23.2.84. [DOI] [PubMed] [Google Scholar]
- 15.Dieppe P., Watt I. Crystal deposition in osteoarthritis: an opportunistic event? Clin Rheum Dis. 1985;11:367. [PubMed] [Google Scholar]
- 16.Martel W., Champion C.K., Thompson G.R., Carter T.L. A roentgenologically distinctive arthropathy in some patients with the pseudogout syndrome. Am J Roentgenol Radium Ther Nucl Med. 1970;109:587. doi: 10.2214/ajr.109.3.587. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto T., Schneider R., Iwamoto Y., Bullough P. Rapid destruction of the femoral head after a single intraarticular injection of corticosteroid into the hip joint. J Rheumatol. 2006;33:1701. [PubMed] [Google Scholar]
- 18.Laroche M., Arlet J., Mazieres B. Osteonecrosis of the femoral and humeral heads after Intraarticular corticosteroid injections. J Rheumatol. 1990;17:549. [PubMed] [Google Scholar]
- 19.McCarty D.J., McCarthy G., Carrera G. Intraarticular corticosteroids possibly leading to local osteonecrosis and marrow fat induced synovitis. J Rheumatol. 1991;18:1091. [PubMed] [Google Scholar]
- 20.Pivec R., Johnson A.J., Harwin S.F., Mont M.A. Differentiation, diagnosis, and treatment of osteoarthritis, osteonecrosis, and rapidly progressive osteoarthritis. Orthopedics. 2013;36:118. doi: 10.3928/01477447-20130122-04. [DOI] [PubMed] [Google Scholar]
- 21.Subedi N., Chew N.S., Chandramohan M., Scally A.J., Groves C. Effectiveness of fluoroscopy-guided intra-articular steroid injection for hip osteoarthritis. Clin Radiol. 2015;70:1276. doi: 10.1016/j.crad.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Deshmukh A.J., Panagopoulos G., Alizadeh A., Rodriguez J.A., Klein D.A. Intra-articular hip injection: does pain relief correlate with radiographic severity of osteoarthritis? Skeletal Radiol. 2011;40:1449. doi: 10.1007/s00256-011-1120-8. [DOI] [PubMed] [Google Scholar]
- 23.McCabe P.S., Maricar N., Parkes M.J., Felson D.T., O’Neill T.W. The efficacy of intra-articular steroids in hip osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2016;24:1509. doi: 10.1016/j.joca.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 24.Clohisy J.C., Carlisle J.C., Beaulé P.E. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90:47. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Richette P. La coxarthrose destructrice rapide. Rev Rhum. 2009;76:341. [Google Scholar]
- 26.Ruiz E.J., Calatayud M.R., Rodríguez J.A., Alberdi E.G. Rapidly destructive osteoarthritis of the hip: case presentation. Reumatol Clin. 2011;7:56. doi: 10.1016/j.reuma.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 27.Villoutreix C., Pham T., Tubach F., Dougados M., Ayral X. Intraarticular glucocorticoid injections in rapidly destructive hip osteoarthritis. Joint Bone Spine. 2006;73:66. doi: 10.1016/j.jbspin.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 28.McAlindon T.E., LaValley M.P., Harvey W.F. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. JAMA. 2017;317:1967. doi: 10.1001/jama.2017.5283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hart G., Fehring T. Rapidly destructive osteoarthritis can miic infection. Arthroplasty Today. 2016;2(1):15. doi: 10.1016/j.artd.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.