Highlights
-
•
Decerebrate rigidity unreported complication of pseudomeningocoele.
-
•
Mechanism of developing such rigidity discussed.
-
•
Management of pseudomeningocoele highlighted.
Keywords: Pseudomeningocele, Dural tear, Raised intra cranial pressure, Decerebrate rigidity
Abstract
Introduction
Spinal pseudomeningoceles are extradural collections of cerebrospinal fluid that result following a breach in the dural-arachnoid layer and is reported as one of the complications of lumbar disc surgery. Although they are often self subsiding and asymptomatic, they may occasionally cause low-back pain, headaches, and even nerve root entrapment. The purpose of this case report is to present an unreported presentation of pseudomeningocele
Presentation of case
A 34 year obese male presented one month post lumbar discectomy with symptoms suggestive of raised intra cranial pressure presenting as repetitive decerebrate rigidity and altered sensorium lasting for few minutes when there is pressure on the pseudomeningocele sac and subsiding with change in position of the patient. He underwent surgical repair of the dural tear and was improved symptomatically with no recurrence of symptoms at five years follow up.
Discussion
Radiological investigation helped in ruling out the other causes of decerebrate rigidity and the possible mechanism of development of such symptom in pseudomeningocele is discussed.
Conclusion
To the best of our knowledge, this is the first reported case of pseudomeningooele presenting as decerebrate rigidity. Spinal pseudomeningocele can present in varied ways and earliest detection is the key to avoid such complications.
1. Introduction
Postoperative pseudomeningocele, a rare complication of spine surgery, is an extravasated collection of cerebrospinal fluid that results from dural tear. Though this entity is frequently asymptomatic, it can occasionally be associated with a range of symptoms including headaches, infection, back pain, radiculopathy, and myelopathy [1], [2], [3]. Computed tomography (CT) and magnetic resonance imaging (MRI) are useful for diagnosis. Treatment must be specific to each patient as the timing, size, symptoms, and location of the dural breach all affect the choice of therapy. Surgical treatment is required in symptomatic cases [4], [5], [6]. Here we report a unique case of lumbar pseudomeningocele, where the patient when received pressure on pseudomeningocele encountered decerebrate rigidity and altered sensorium. This complication of pseudomeningocele is noteworthy as it is not reported elsewhere. This case report has been reported in line with the SCARE criteria [7] and patient’s consent was duly obtained.
2. Case report
The patient, a 34- year- old obese male presented to us with bilateral L4 radiculopathy. On examination, he had mild left extensor hallucis longus weakness. MRI of the lumbosacral spine revealed L4–L5 large central herniation, which was causing distortion of the dural sac and cauda equina roots. (Fig. 1, Fig. 2). He underwent L4–L5 microdiscectomy via standard posterior midline approach with left sided exposure. The patient endured the surgery well and there were no obvious dural tear and CSF fluid leakage observed per-operatively. He was discharged on the following day with his only complaint of constipation. A week later, he presented with sudden onset of suboccipital pain while straining at stools and the same day, he noticed cerebrospinal fluid leak from upper end of the incision, which resolved after local suturing, diuretics and acetazolamide administration. The patient, back to his routine life, once more presented a month later with sudden episode of uprolling of eyes associated with opisthotonous posturing and altered sensorium for few minutes with vomiting and snoring while resting his back to the chair in sitting position. Similar episodes were noted whenever he was trying to lie supine. Before the onset of these episodes, he suffered an unusual feeling in occipital region with mild headache. On examination, he had a firm induration in and around operative region without any obvious swelling and the operative wound had completely healed. It was observed that even a mild pressure in indurated area troubled the patient with severe headache. An MRI brain had ruled out hydrocephalus and Chiari malformation (Fig. 3, Fig. 4). We performed an MRI of the lumbosacral spine, in prone position with difficulty, which showed an extradural cystic collection, which was hypointense on T1 weighted images and hyperintense on T2 weighted images. There was a clear communication with the dural sac along the tract through which the discectomy was performed (Fig. 5, Fig. 6). He underwent re-exploration of the incision and repair of the dural defect. Intraoperatively, large pseudomeningocele was present in fat layers with extension upto root sleeve level as depicted in axial MRI (Fig. 6). Due to the effect of persistent CSF, a smooth epithelialized cavity was noted within the fat layer, which was excised to help wound closure and healing. There was a small dural rent with rugged edges on anterior part of the root sleeve and the CSF was ejecting out through the rent with every spinal pulsation, and this was reconfirmed with valsalva maneuver. The rent was closed with muscle patch and fibrin glue. The wound was closed in multiple layers, mobilizing the fat from paraspinal region, creating superior and inferior flaps to cover the dead space. Postoperatively, the patient was put on a superficial drain without negative pressure and nursed in prone position. Diuretics and acetazolamide were added. Wound healed without any recurrence of pseudomeningocele and all symptoms of the patient completely subsided. He was followed up for period of 5years without recurrence of symptoms.
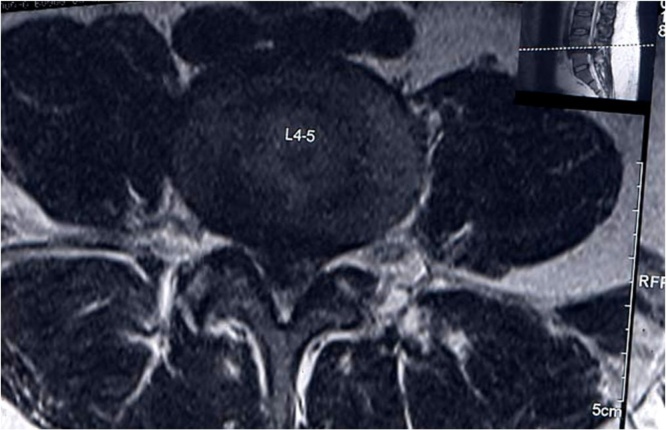
Fig. 1.
T2W image showing L4–L5 prolapsed intervertebral disc.
Fig. 2.
axial section showing the prolapsed disc.
Fig. 3.
T2W axial (prone position) did not show hydrocephalus.
Fig. 4.
T2W sagittal section ruled out chiari malformation.
Fig. 5.
Sagittal section T2W image showing communication of the pseudomeningocele with thecal sac.
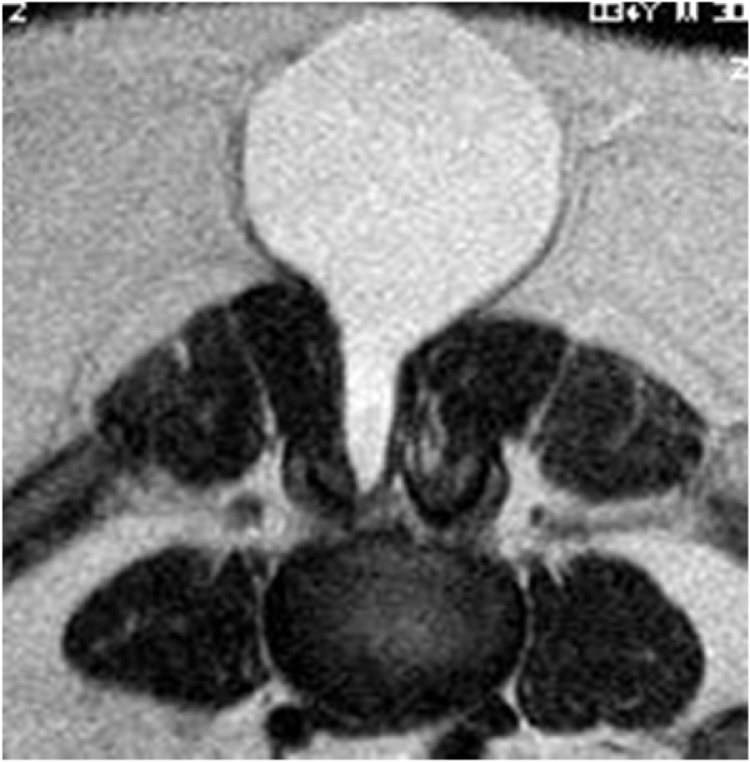
Fig. 6.
axial section T2W image showing the communication of the pseudomeningocele along the discectomy tract. (Prone position).
3. Discussion
Postoperative pseudomeningocele formation is reported with an incidence ranging from 0.068% to 2%. Dural tears are a well recognized complication of spinal surgery. When the dura is torn, CSF may be forced through the tear to form a pseudomeningocele that can displace paravertebral soft tissues and subcutaneous space [8], [9]. In our patient, the dural tear was not noted per-operatively at the initial surgery. Instead, all his symptoms were noticed following straining at stools suggestive of tear of the arachnoid during straining. However, it is likely that there must have been dural rent without arachnoidal rupture during initial surgery. The symptoms associated with pseudomeningocele vary widely, including back pain, sciatic pain, headache, neck pain, nausea, vomiting, tinnitus and a palpable mass. However most of the pseudomeningoceles remain asymptomatic [10], [11]. Symptoms may appear at any time and the severity of symptoms does not necessarily correlate with the size. The major symptom is a severe postural headache that develops minutes after arising from a recumbent position and is relieved minutes after lying down suggesting low pressure headache [9]. Endriga et al. demonstrated occurrence of hydrocephalus in his case who presented as constant headache and increase in size of ventricles, which resolved with ventriculoperitoneal shunt [12]. Our patient had symptoms suggestive of raised intracranial pressure presenting as repetitive decerebrate rigidity with altered sensorium on whichever posture that compressed the pseudomeneningocele, but with normal MRI brain unlike the case demonstrated by previous author [12]. Diagnosis of pseudomeningocele typically depends on MRI which shows low signal intensity on T1- weighted image and high signal intensity on T2- weight image. In our patient MRI has been used as the modality to prove the communication between the subarachnoid space and extradural space radiologically. Conservative measures alone [13], including hydration, prolonged bed rest and analgesics, are generally not considered adequate to control large CSF leaks with pseudomeningocele. The standard treatment for persistent CSF leak is open revision surgery and closure of dura arachnoid layer [4], [10], [14], [15], [16]. Our patient underwent re-exploration of the incision and repair of the dural defect, considering the life threatening manifestation of the disease. The postural decerebrate rigidity developed in our patient represents a unique complication of pseudomeningocele which is not reported. The probable cause of raised intracranial tension can be best explained as a retrograde pressure of the collected CSF fluid getting transmitted into the spinal subarachnoid space secondary to pressure on the sac either with supine position or by any means of pressure on the sac. Normally raised intracranial tension of 40–50 mm HG above the cerebral perfusion pressure leads to decerebrate rigidity. Because of presence of large amount of fat in the subcutaneous plane, patient have developed large pseudomeningocele which after a month must have decompensated to produce his symptoms.
4. Conclusion
Our case report clearly depicts possibility of raised intracranial pressure in cases of large pseudomeningocele with persistent communication with sub arachnoid space. This was confirmed by complete relief of the symptoms, once the pseudomeningocoele was repaired surgically.
Conflicts of interest
NIL.
Funding
NIL.
Ethical approval
IRB/Ethics Committee ruled that approval was not required for this study − This case report mentions only the rarest presentation and the treatment is not altered in any way from the previous methods of managing such patients and it is a retrospective case study.
Consent
OBTAINED FROM PATIENT.
Author contribution
Dr Satish Rudrappa – conception and design of study.
Dr Ramachandran G – analysis and/or interpretation of data, drafting the manuscript.
Dr Venkata R Tukkapuram – acquisition of data.
Dr Swaroop Gopal – revising the manuscript critically for important intellectual content.
Registration of research studies
N/A.
Guarantor
Ramachandran Govindasamy.
Contributor Information
Satish Rudrappa, Email: drsatishr@gmail.com.
Ramachandran Govindasamy, Email: mail2ram8544@gmail.com.
Venkata Ramakrishna Tukkapuram, Email: dr.tvramakrishna@gmail.com.
Swaroop Gopal, Email: swaroopdr@gmail.com.
References
- 1.Aldrete J.A., Ghaly R. Postlaminectomy pseudomeningocele. An unsuspected cause of low back pain. Reg. Anesth. 1995;20(1):75–79. [PubMed] [Google Scholar]
- 2.O’Connor D., Maskery N., Griffiths W.E. Pseudomeningocele nerve root entrapment after lumbar discectomy. Spine. 1998;23:1501–1502. doi: 10.1097/00007632-199807010-00014. [DOI] [PubMed] [Google Scholar]
- 3.Pavlou G., Bucur S.D., van Hille P.T. Entrapped spinal nerve roots in a pseudomeningocoele as a complication of previous spinal surgery. Acta Neurochir. (Wien) 2006;148(February (2)):215–219. doi: 10.1007/s00701-005-0696-y. discussion 219-20. Epub 2005 Dec 27. [DOI] [PubMed] [Google Scholar]
- 4.B.M. McCormack, B.M. Zide, I.H. Kalfas: Cerebrospinal fluid fistula and pseudomeningocele after spine surgery. Spine Surgery, techniques, complication avoidance and management Edward C, Benzel EC 2005, 2:2033–2042.
- 5.Hadani M., Findler G., Knoler N., Tadmor R., Sahar A., Shacked I. Entrapped lumbar nerve root in pseudomeningocele after laminectomy: report of three cases. Neurosurgery. 1986;19:405–407. doi: 10.1227/00006123-198609000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Kaar G.F., Briggs M., Bashir S.H. Thecal repair in post-surgical pseudomeningocoele. Br. J. Neurosurg. 1994;8(6):703–707. doi: 10.3109/02688699409101184. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., The SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Barron J.T. Radiologic case study. Lumbar pseudomeningocele. Orthopedics. 1990;13:608–609. doi: 10.3928/0147-7447-19900501-20. [DOI] [PubMed] [Google Scholar]
- 9.Pau A. Postoperative meningocele spurius. Report of two cases. J. Neurosurg. Sci. 1974;18:150–152. [PubMed] [Google Scholar]
- 10.Teplick J.G., Peyster R.G., Teplick S.K., Goodman L.R., Haskin M.E. CT Identification of postlaminectomy pseudomeningocele. AJR Am. J. Roentgenol. 1983;140:1203–1206. doi: 10.2214/ajr.140.6.1203. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A.J., Nambiar C.S., Kanse P. Spontaneous resolution of lumbar pseudomeningocoele. Spinal Cord. 2003;41(8):470–472. doi: 10.1038/sj.sc.3101462. [DOI] [PubMed] [Google Scholar]
- 12.Endriga D.T., Dimar J.R., 2nd, Carreon L.Y. Communicating hydrocephalus, a long-term complication of dural tear during lumbar spine surgery. Eur. Spine J. 2016;25(May Suppl. 1):157–161. doi: 10.1007/s00586-015-4308-0. Epub 2015 Oct 31. [DOI] [PubMed] [Google Scholar]
- 13.Solomon P., Sekharappa V., Krishnan V., David K.S. Spontaneous resolution of postoperative lumbar pseudomeningoceles: a report of four cases. Indian J. Orthop. 2013;47(July (4)):417–421. doi: 10.4103/0019-5413.114937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawk M.W., Kim K.D. Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg. Focus. 2000;9(1):e5. doi: 10.3171/foc.2000.9.1.5. [DOI] [PubMed] [Google Scholar]
- 15.Wolff S., Kheirredine W., Riouallon G. Surgical dural tears: prevalence and updated management protocol based on 1359 lumbar vertebra interventions. Orthop. Traumatol. Surg. Res. 2012;98(8):879–886. doi: 10.1016/j.otsr.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 16.Khan M.H., Rihn J., Steele G., Davis R., Donaldson W.F., 3rd, Kang J.D., Lee J.Y. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006;31(22):2609–2613. doi: 10.1097/01.brs.0000241066.55849.41. [DOI] [PubMed] [Google Scholar]