In spite of all the medical progress, hypertension remains a highly prevalent chronic disease worldwide, contributing importantly to cardiovascular morbidity and mortality in Europe1 and around the globe. Indeed, it has been estimated that in the not too distant future up to 50% of the adult population will develop high blood pressure according to currently used definitions.2 Since Franklin D. Roosevelt died of a cerebral haemorrhage in 1945 due to uncontrolled high blood pressure with values up to 300/190 mmHg, the management of hypertension has made impressive progress. Indeed, while at that time only Kempner's rice diet was available, after the war diuretics, reserpine, guanethidine, and later beta-blockers, spironolactone, calcium antagonists, and angiotensin-converting enzyme (ACE) inhibitors became available. Today, with the advent of angiotensin receptor blockers, renin inhibitors, eplerenone, and beta-blockers, the pharmacological armamentarium to treat high blood pressure has become quite vast, and most patients can be controlled with 1–3 antihypertensive drugs to levels of ≤140/90 mmHg.3
Treatment-resistant hypertension
Thanks to this success, it appeared that antihypertensive management had reached its goals and no further developments would be required. Nevertheless, it has been recognized that a small, but significant portion of patients remains uncontrolled in spite of the many drugs available today.4 The European Society of Cardiology together with the European Society of Hypertension, as well as their American counterparts have defined treatment-resistant hypertension as blood pressure values > 140/90 mmHg in spite of three antihypertensive drugs including a diuretic.2 It has been estimated that between 3% and 5% of the patients would fall into this category.5 As the event rates are staggeringly high in this patient population, additional treatment options are an unmet clinical need.6 It has been argued that many of the patients with so-called treatment-resistant hypertension are in fact just non-compliant and that their blood pressure is controlled upon witnessed intake of the drugs. Indeed, some observational data indicate that non-adherence to drug treatment affects up to 50% of patients referred to a tertiary care centre.7 Although this may be the case, such patients cannot be hospitalized for ever and thus may still have high event rates after discharge from hospital or exclusion from clinical trials. Furthermore, there is a group of patients with pseudo-resistant hypertension with elevated office blood pressures in spite of effective treatment, but a normal 24-h blood pressure profile.8 This group of patients with what is also called white-coat hypertension may have a completely different risk profile from those with true treatment-resistant hypertension. The situation is even more complex as some patients present with normal office blood pressure but high 24-h or home blood pressure. This patient cohort is characterized by having an increased cardiovascular risk and being difficult to examine because of their low office blood pressure.9
The sympathetic nervous system and blood pressure
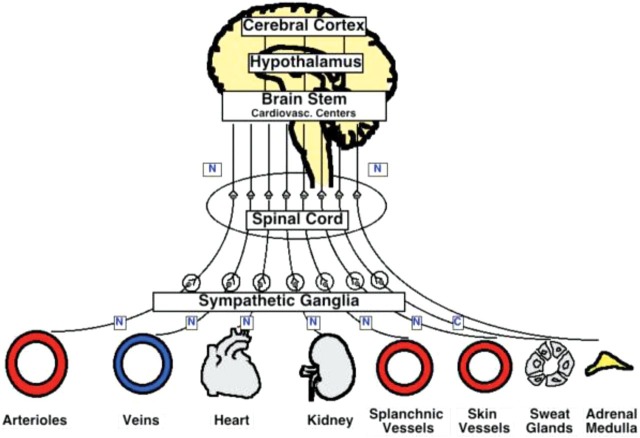
Blood pressure is regulated by many neurogenic and humoral systems, as well as by the functional and structural status of the microcirculation regulating peripheral vascular resistance (Figure 1).10 Early on it was recognized that the sympathetic nervous system is a crucial regulator of blood pressure under acute, but also chronic conditions. Indeed, in normotensive offspring of hypertensive parents, the reactivity of the sympathetic nerve traffic is increased under conditions of stress compared with offspring of normotensive parents. Sympathetic nerve activity is increased in almost all forms of hypertension when measured by muscle sympathetic nerve activity (MSNA). Furthermore, overall body norepinephrine spillover is markedly augmented in young hypertensives as compared with their normotensive counterparts. Thus, the sympathetic nervous system contributes importantly to long-term blood pressure regulation, and its activity seems to be increased early on in the hypertensive process.
Figure 1.
The sympathetic nervous system in the control of the cardiovascular system: sympathetic nerves innervate arteries and veins as well as the kidneys, adrenal gland, and other organs.25
Renal sympathetic nerves
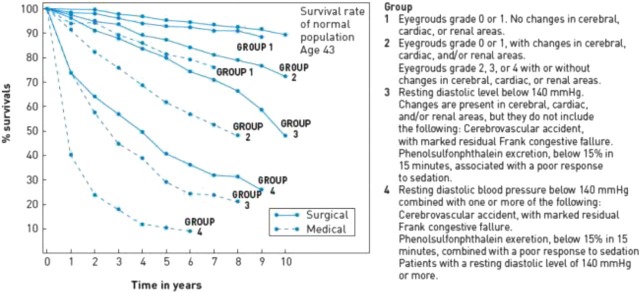
In this context, it is of interest that sympathetic nerves importantly regulate renal perfusion and function, an organ crucially involved in long-term blood pressure control. Afferent and efferent renal nerves reach the kidney from the aorta along the renal artery where they are located in the adventitia of the blood vessel wall. They not only regulate vascular tone of afferent and efferent renal arterioles and sodium retention, but via beta-receptors also increase renin release from juxtaglomerular cells and in turn transform angiotensin I into its active metabolite angiotensin II and increase aldosterone secretion from the adrenal glands. All these events importantly regulate renal water and sodium balance, and in turn blood pressure. As far back as the 1950s, surgeons attempted to treat uncontrolled and so-called malignant hypertension with sympathectomy. Although the clinical success of this procedure was remarkable not only in terms of blood pressure reduction, but also as regards the reduction of total mortality (Figure 2), the morbidity of the procedure was too important to allow it to become common practice. With the advent of effective antihypertensive drugs, therefore, the procedure was abandoned.
Figure 2.
Effects of surgical sympathectomy on mortality in patients with different severity of hypertension (solid lines; grade 1–4) as compared with those treated conservatively (dashed lines).
Selective renal nerve ablation
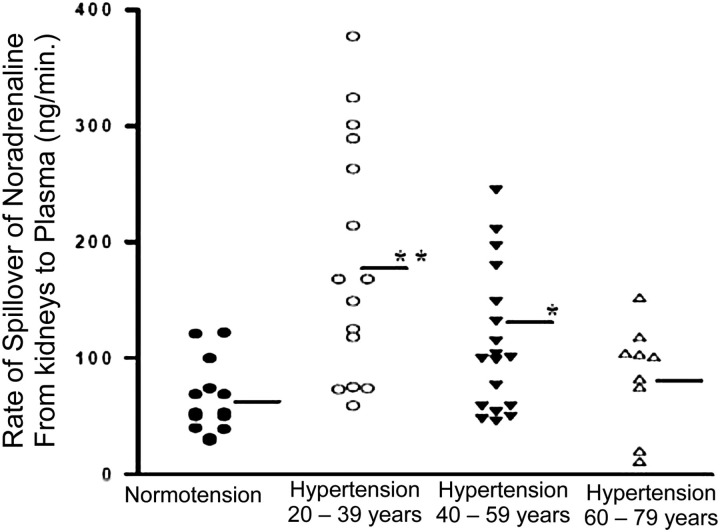
Experimental data in mice, rats, pigs, and dogs confirmed the role of afferent and efferent sympathetic nerves to and from the kidney in the control of blood pressure. Thus, the idea was proposed to develop a novel form of sympathectomy selectively focused on nerves innervating the kidney and regulating renal perfusion as well as water and sodium balance. Thanks to the work of Murray D. Esler, it became clear that also in patients with high blood pressure, in particular in younger individuals, norepinephrine spillover from the kidneys was markedly increased (Figure 3). Although this dysfunction was also notable in elderly hypertensives, the difference to normotensive patients was less impressive with increasing age. Furthermore, experimental studies demonstrated that denervation of the kidney was associated with a marked reduction in their tissue norepinephrine content.
Figure 3.
Renal norepinephrine spillover in normotensive and hypertensive subjects of different ages.
Radiofrequency ablation
Inspired by the success of radiofrequency ablation of rhythm disorders, a novel catheter was developed to destroy afferent and efferent nerves selectively using a minimally invasive catheter-based technique. With the Symplicity device developed by Ardian Inc. (Palo Alto, CA, USA) and later taken over by Medtronic, it has been shown that this procedure was effective in reducing renal norepinephrine content as well as renal spillover in experimental animals and humans, respectively. Furthermore, proof-of-concept studies confirmed that total and renal norepinephrine spillover, MSNA, and blood pressure markedly decreased after the procedure in patients with treatment-resistant hypertension.11
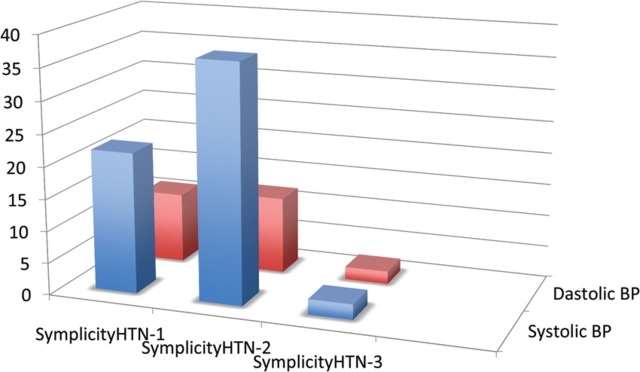
These preliminary experiences were then confirmed in a larger open-label registry (SYMPLICITY HTN-1); (Figure 4) and later in many registries reporting on office and ambulatory blood pressure,8 as well target organ damage such as diastolic dysfunction and left ventricular hypertrophy. Similar blood pressure results to those with the Symplicity Flex catheter were obtained in small patient series using the EnligHTN basket device (St. Jude, MN, USA) and with the Vessix V2 balloon (Boston Scientific, MN, USA).
Figure 4.
Comparison of the blood pressure reduction in SYMPLICITY HTN-1 (A), SYMPLICITY HTN-2 (B), and SYMPLICITY HTN-3 (C) at 6 months after renal nerve ablation using a monoelectrode system.12,16,26
The first randomized SYMPLICITY HTN-2 study in patients with treatment-resistant hypertension expanded, and confirmed a steady and important decrease of blood pressure of ∼ 30/10 mmHg up to 3 years (Figure 4).12 These initial successes led to great enthusiasm in the interventional community to perform this procedure in difficult to control hypertensives, and a consensus statement of European experts was published in the European Heart Journal13 and followed by position statements from different national and international societies.14 To date it has been estimated that up to 8000 renal nerve ablations have already been performed with different catheter-based technologies. Recently, different energy source and treatment modalities, such as ultrasound and chemical denervation, have been developed, with similar initial results in a small patient series.
SYMPLICITY HTN-3
At the American College of Cardiology 2013 in Washington, DC, the results of the SYMPLICITY HTN-3 trial15 were presented.16 SYMPLICITY HTN-3 included patients with a systolic blood pressure ≥160 mmHg in spite of three antihypertensive drugs including a diuretic at maximally tolerated dosages. A total of 1441 patients were assessed for eligibility, whereof 535 patients (37%) from 88 sites in the USA were enrolled. After initial screening, patients were observed for 2 weeks and eventually randomized to renal nerve ablation using the Symplicity Flex catheter (Medtronic, MN, USA) or renal angiography only (sham control). Patients were unaware of their group allocation. Both groups remained on treatment regimens of three or more antihypertensive drugs, including a diuretic, at the highest tolerated doses. The primary efficacy endpoint was the difference in office systolic office blood pressure between the groups; the secondary endpoint was the change in ambulatory blood pressure. The primary safety endpoint was a composite of major adverse events, and renal artery or other vascular complications within 6 months after treatment.
The primary safety endpoint was met; however, disappointingly, renal nerve ablation using the Symplicity Flex system did not reach the primary efficacy endpoint of reduction in office systolic blood pressure or the powered secondary efficacy endpoint of a decrease in average 24-h levels by ambulatory blood pressure monitoring (Figure 4). Although both patient groups showed a statistically significant decrease of blood pressure at 6 months compared with baseline of 14.1 mmHg for renal denervation and 11.7 mmHg for the sham treatment group, the difference of –2.29 mmHg in office systolic blood pressure between the two arms was not significant (P = 0.26). The results were similar for the change in 24-h systolic blood pressure, with a non-significant difference between the two arms of –1.96 mmHg (P = 0.98).
Why did SYMPLICITY HTN-3 fail?
There are several possibilities why SYMPLICITY HTN-3 did not confirm the results of previous published registries and randomized trials.
Renal nerve ablation using radiofrequency ablation may simply not work in humans, in contrast to animals. Indeed, this is the largest and most rigorous trial so far testing the effecttiveness of renal nerve ablation using the Symplicity Flex system in patients with treatment-resistant hypertension. The more pronounced blood pressure reduction observed in registries may be subject to the regression-to-the-mean phenomenon as well as other biases typical of observational registry data. Furthermore, SYMPLICITY HTN-2 was a much smaller randomized trial with 106 patients included.
The statistical power of SYMPLICITY HTN-3 may not allow differences between usual medical care and radiofrequency ablation to be seen, as the sample size calculation was based on previous studies with a potentially overestimated treatment effect. This appears to be unlikely as the trial recruited > 500 patients with severe hypertension and represents the largest trial so far. However, when compared with hypertension drug trials, where several thousand patients are usually investigated, SYMPLICITY HTN-3 is a small study. On the other hand, the patients enrolled in the trial had truly severe hypertension and baseline blood pressure values of ∼180 mmHg systolic in spite of five antihypertensive drugs, a population in which the effects of radiofrequency ablation have been so far most notable.
The procedure may not have been performed effectively. It is notable that the 535 patients were recruited in 88 centres. Overall, 364 renal denervation procedures were performed by 111 operators. Thus, on average, operators performed around three procedures in the trial without previous experience, some even less. As the procedure is not approved in the USA and no roll-in phase was introduced, one has to assume that the learning curve of the operators fell within the period of the trial. Although renal nerve ablation is generally recognized as a technically relatively easy procedure for experienced interventionalists, it still has a learning curve that may have affected the results, especially using first-generation monoelectrode systems. This is especially important as there is still no test available allowing assessment of proper wall contact and effective destruction of renal nerves during or after the procedure.17
-
Antihypertensive drugs may have been maximized, but the patients may not have been stabilized appropriately before randomization. This is of note, as per protocol no changes in antihypertensive medications were allowed in the 2 weeks before randomization. For the next 2 weeks, patients had to record their blood pressure at home in the morning and evening and keep a diary ensuring their adherence to medical therapy. Then a confirmatory screening visit was scheduled ensuring that they met the blood pressure criteria for inclusion. It is known from many studies that it may take up to 8 weeks after introducing new antihypertensive drugs or after changing their dosages to reach their maximal effect. Thus, it is possible that in SYMPLICITY HTN-3 patients were not truly stabilized, although they were on the maximum tolerated dose. Indeed, the marked blood pressure drop in the sham controls supports this interpretation.
Furthermore, 40% of the patients were taking direct-acting vasodilators, drugs known to reduce blood pressure effectively. However, they are also prone to serious side effects, such as tachycardia, pericardial effusion, oedema, and hirsutism, associated with low adherence rates. It is of note that the percentage of patients on vasodilators in SYMPLICITY HTN-3 was twice as high as in previous studies.16,18 Interestingly, treatment with a direct vasodilatator is a predictor of non-response to renal denervation. Statistically, the neutral SYMPLICITY HTN-3 results could thus be related to high variability in adherence and consequently in office and ambulatory blood pressure readings during follow-up, introducing a significant amount of ‘noise’ that may have masked any true antihypertensive signal of the procedure. It is therefore important to continue to monitor the blood pressure differences between the groups during long-term follow-up.
Finally, it appears difficult to demonstrate any significant incremental blood pressure-lowering effect of any intervention in patients already on more than five antihypertensive drugs. Thus, in the future, it may be important to test the effects of renal nerve ablation on blood pressure in patients with values > 140 mmHg systolic in spite of three antihypertensive drugs including a diuretic, leaving room for the investigation of a potential additional antihypertensive effect.
The patient population may differ from Caucasians recruited in previous trials, mainly performed in centres of excellence in Europe and Australia. Indeed, patients with hypertension are heterogeneous as regards their pathophysiology. It is of note that low renin hypertension, commonly seen in Afro-Americans, typically does not respond well to ACE inhibitors and beta-blockers, while diuretics and vasodilators are particularly effective.19 In the SYMPLICITY HTN-3 study, a quarter of the recruited patients were black and a subgroup analysis suggested that Afro-Americans respond better to sham than to renal denervation. Interestingly, the change in office systolic blood pressure in Afro-Americans allocated to the sham group was more pronounced when compared with Caucasian and Asian patients (–17.8 mmHg vs. –8.6 mmHg).
The results may just be accidental. Indeed, in many instances in medicine, effective treatment modalities proved ineffective or failed to show superiority in one of many trials. Examples are ACE inhibitors after myocardial infarction,20 and percutaneous coronary intervention vs. medical therapy,21 among others. Due to the overall evidence, such treatment modalities still remain heavily used.
The future of renal nerve ablation
So far, renal nerve ablation has been investigated in patients with resistant hypertension, a condition characterized by high cardiovascular morbidity and mortality. Undoubtedly, renal denervation increased the awareness of uncontrolled hypertension and stimulated the scientific community to investigate further this high-risk patient population and to develop novel strategies for this condition. The SYMPLICITY HTN-3 trial provides a valuable opportunity to reconsider the evidence of this novel technique.
Pre-clinical data are urgently needed to better understand the physiology and anatomy of the renal sympathetic nervous system and to characterize the effectiveness of the different catheter-based renal denervation systems including histopathological analyses. Most importantly, it would be essential to develop reliable and practical tools to determine the degree of renal nerve ablation after the procedure. This would allow identification of treatment failures and ensure successful renal nerve ablation. Indeed, until reliable techniques to assess successful renal nerve ablation become available, the interpretation of any, and especially neutral clinical trials will remain uncertain. Once it is confirmed that current available or future devices consistently modulate sympathetic nervous system activity in humans and the above-mentioned device-related questions have been adequately addressed, renal nerve ablation might be particularly beneficial in conditions with high sympathetic activity, such as heart failure with impaired or preserved left ventricular ejection fraction and arrhythmias.
Innovative and refined clinical trials should be conducted to investigate further the potential of renal nerve ablation in distinct hypertension populations. Thoroughly designed clinical trials could offer the opportunity to test the hypothesis that increased sympathetic activity maintains blood pressure in some, but not other, patient populations.
Finally, randomized, controlled trials investigating the impact of decreasing sympathetic tone by renal nerve ablation on clinical outcomes will eventually remain the gold standard to determine the ultimate role of any new treatment option. Indeed, both the LIFE trial22 and the ASCOTT trial23 in hypertensive patients suggest that clinical outcome may differ depending on which blood pressure-regulating mechanism is blocked. It is of note that renal nerve ablation may be metabolically advantageous as in hypertensives it also improves insulin resistance.24
Thus, for now, more questions than definite answers remain after the publication of SYMPLICITY HTN-3 in the still very young field of catheter-based renal denervation, and obviously much more scientifically sound evidence is needed before any definite conclusion can be drawn.
Conflict of interest: T.F.L. and F.M. have received research contracts and consultant honoraria from Medtronic, St. Jude, Boston, and Cordis.
References
- 1.Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J. 2013;34:3028–3034. doi: 10.1093/eurheartj/eht356. [DOI] [PubMed] [Google Scholar]
- 2.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press. 2014;23:3–16. doi: 10.3109/08037051.2014.868629. [DOI] [PubMed] [Google Scholar]
- 3.Burnier M, Vuignier Y, Wuerzner G. State-of-the-art treatment of hypertension: established and new drugs. Eur Heart J. 2014;35:557–562. doi: 10.1093/eurheartj/eht465. [DOI] [PubMed] [Google Scholar]
- 4.Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC, Jr, Crowley K, Goto S, Ohman EM, Bakris GL, Perlstein TS, Kinlay S, Bhatt DL REACH Registry Investigators. Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis. Eur Heart J. 2013;34:1204–1214. doi: 10.1093/eurheartj/ehs368. [DOI] [PubMed] [Google Scholar]
- 5.Pimenta E, Calhoun DA. Resistant hypertension: incidence, prevalence, and prognosis. Circulation. 2012;125:1594–1596. doi: 10.1161/CIRCULATIONAHA.112.097345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, O'Connor PJ, Selby JV, Ho PM. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125:1635–1642. doi: 10.1161/CIRCULATIONAHA.111.068064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H, Toennes SW. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens. 2013;31:766–774. doi: 10.1097/HJH.0b013e32835e2286. [DOI] [PubMed] [Google Scholar]
- 8.Mahfoud F, Ukena C, Schmieder RE, Cremers B, Rump LC, Vonend O, Weil J, Schmidt M, Hoppe UC, Zeller T, Bauer A, Ott C, Blessing E, Sobotka PA, Krum H, Schlaich M, Esler M, Böhm M. Ambulatory blood pressure changes after renal sympathetic denervation in patients with resistant hypertension. Circulation. 2013;128:132–140. doi: 10.1161/CIRCULATIONAHA.112.000949. [DOI] [PubMed] [Google Scholar]
- 9.Brguljan-Hitij J, Thijs L, Li Y, Hansen TW, Boggia J, Liu YP, Asayama K, Wei FF, Bjorklund-Bodegard K, Gu YM, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Katarzyna SS, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Filipovsky J, Imai Y, Wang J, O'Brien E, Staessen JA on behalf of the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcome Investigators. Risk stratification by ambulatory blood pressure monitoring across JNC classes of conventional blood pressure. Am J Hypertens. 2014 doi: 10.1093/ajh/hpu002. in press. [DOI] [PubMed] [Google Scholar]
- 10.Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370:591–603. doi: 10.1016/S0140-6736(07)61299-9. [DOI] [PubMed] [Google Scholar]
- 11.Hering D, Lambert EA, Marusic P, Walton AS, Krum H, Lambert GW, Esler MD, Schlaich MP. Substantial reduction in single sympathetic nerve firing after renal denervation in patients with resistant hypertension. Hypertension. 2013;61:457–464. doi: 10.1161/HYPERTENSIONAHA.111.00194. [DOI] [PubMed] [Google Scholar]
- 12.Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376:1903–1909. doi: 10.1016/S0140-6736(10)62039-9. [DOI] [PubMed] [Google Scholar]
- 13.Mahfoud F, Luscher TF, Andersson B, Baumgartner I, Cifkova R, Dimario C, Doevendans P, Fagard R, Fajadet J, Komajda M, Lefèvre T, Lotan C, Sievert H, Volpe M, Widimsky P, Wijns W, Williams B, Windecker S, Witkowski A, Zeller T, Böhm M European Society of Cardiology. Expert consensus document from the European Society of Cardiology on catheter-based renal denervation. Eur Heart J. 2013;34:2149–2157. doi: 10.1093/eurheartj/eht154. [DOI] [PubMed] [Google Scholar]
- 14.Schmieder RE, Redon J, Grassi G, Kjeldsen SE, Mancia G, Narkiewicz K, Parati G, Ruilope L, van de Borne P, Tsioufis C European Society of Hypertension. Updated ESH position paper on interventional therapy of resistant hypertension. EuroIntervention. 2013;9(Suppl R) doi: 10.4244/EIJV9SRA11. R58–R66. [DOI] [PubMed] [Google Scholar]
- 15.Kandzari DE, Bhatt DL, Sobotka PA, O'Neill WW, Esler M, Flack JM, Doevendans P, Fagard R, Fajadet J, Komajda M, Lefèvre T, Lotan C, Sievert H, Volpe M, Widimsky P, Wijns W, Williams B, Windecker S, Witkowski A, Zeller T, Böhm M European Society of Cardiology. Catheter-based renal denervation for resistant hypertension: rationale and design of the SYMPLICITY HTN-3 Trial. Clin Cardiol. 2012;35:528–535. doi: 10.1002/clc.22008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Cohen SA, Oparil S, Rocha-Singh K, Townsend RR, Bakris GL SYMPLICITY HTN-3 Investigators. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393–1401. doi: 10.1056/NEJMoa1402670. [DOI] [PubMed] [Google Scholar]
- 17.Mahfoud F, Bhatt DL. Catheter-based renal denervation: the black box procedure. JACC Cardiovasc Interv. 2013;6:1092–1094. doi: 10.1016/j.jcin.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Laurent S, Schlaich M, Esler M. New drugs, procedures, and devices for hypertension. Lancet. 2012;380:591–600. doi: 10.1016/S0140-6736(12)60825-3. [DOI] [PubMed] [Google Scholar]
- 19.Rifkin DE, Khaki AR, Jenny NS, McClelland RL, Budoff M, Watson K, Ix JH, Allison MA. Association of renin and aldosterone with ethnicity and blood pressure: the multi-ethnic study of atherosclerosis. Am J Hypertens. 2014 doi: 10.1093/ajh/hpt276. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Kober L, Maggioni AP, Solomon SD, Swedberg K, Van de Werf F, White H, Leimberger JD, Henis M, Edwards S, Zelenkofske S, Sellers MA, Califf RM Valsartan in Acute Myocardial Infarction Trial Investigators. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003;349:1893–906. doi: 10.1056/NEJMoa032292. [DOI] [PubMed] [Google Scholar]
- 21.Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GB, Weintraub WS COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. doi: 10.1056/NEJMoa070829. [DOI] [PubMed] [Google Scholar]
- 22.Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, Fyhrquist F, Julius S, Kjeldsen SE, Kristiansson K, Lederballe-Pedersen O, Nieminen MS, Omvik P, Oparil S, Wedel H, Aurup P, Edelman J, Snapinn S LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- 23.Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–1158. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 24.Mahfoud F, Schlaich M, Kindermann I, Ukena C, Cremers B, Brandt MC, Hoppe UC, Vonend O, Rump LC, Sobotka PA, Krum H, Esler M, Böhm M. Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: a pilot study. Circulation. 2011;123:1940–1946. doi: 10.1161/CIRCULATIONAHA.110.991869. [DOI] [PubMed] [Google Scholar]
- 25.Lüscher TF, Wolfrum M, Noll G, Sudano I. Renal sympathetic denervation. In: Eckhout E. SPW, Wijns W, Vahanian A, van Sambeek M, de Palma R, editors. The PCR-EAPCI Textbook. Paris: Europa Edition; 2012. [Google Scholar]
- 26.Krum H, Schlaich MP, Sobotka PA, Bohm M, Mahfoud F, Rocha-Singh K, et al. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet. 2014;383:622–629. doi: 10.1016/S0140-6736(13)62192-3. [DOI] [PubMed] [Google Scholar]