Abstract
Objective:
The objective of this study is to determine the accuracy of the bedside lung ultrasound in emergency (BLUE) protocol in giving a correct diagnosis in patients presenting with acute respiratory distress in emergency department.
Materials and Methods:
Patients with acute respiratory distress were evaluated. Ultrasound findings such as artifacts (A line, B line), lung sliding, alveolar consolidation or pleural effusion, and venous analysis were recorded. Ultrasonography findings were correlated with final diagnosis made by the treating unit. Sensitivity and specificity were calculated.
Results:
A total 50 patients were evaluated. The A profile (predominant A line with lung sliding) indicated chronic obstructive pulmonary disease/asthma (n = 14) with 85.17% sensitivity and 88.88% specificity. B profile (predominant B + lines with lung sliding) indicated pulmonary edema (n = 13) with 92.30% sensitivity and 100% specificity. The A/B profile (A line on one side and B + line on other side) and the C profile (anterior consolidation) and the A profile plus posterolateral alveolar and/or pleural syndrome indicated pneumonia (n = 17) with 94.11 sensitivity and 93.93% specificity. The A profile plus venous thrombosis indicated pulmonary embolism (n = 1) with 100% sensitivity and specificity. A’ profile (predominant A line without lung sliding) with lung point indicated pneumothorax (n = 5) with 80% sensitivity and 100% specificity.
Conclusion:
BLUE protocol was successful in average 90.316% cases. BLUE performed in emergency department is equivalent to computed tomography scan. BLUE protocol aids in making diagnosis and saves time and cost; avoids the side effects related to radiation.
Keywords: Bedside lung ultrasound in emergency, emergency medicine, respiratory failure, ultrasound
INTRODUCTION
Point-of-care ultrasonography (USG) is emerging as an important bedside tool.[1] Lung ultrasound imaging is easily available at bedside, real-time, and free of radiation hazards in comparison to conventional imaging modalities of the lung in critically ill patients.[2] Acute respiratory failure cases do not always present in conditions that are ideal for an immediate diagnosis, which sometimes compromises outcome.[3] The bedside lung ultrasound in emergency (BLUE) protocol makes exclusive use of lung and venous ultrasound.[4] Its use as a primary survey tool in the acutely dyspneic or hypoxemic patient gives an immediate understanding of the state of the lung and influences therapeutic decisions.[5]
Study objective
The objective of this study is to determine the accuracy of the BLUE protocol in giving a correct diagnosis in patients presenting with acute respiratory distress in the emergency department.
MATERIALS AND METHODS
This was an observational study over a period of 2 months carried out at emergency medicine department of a tertiary care hospital in Ahmedabad.
Patients of acute respiratory distress requiring Intensive Care Unit (ICU) admission were evaluated. Ultrasound was performed in emergency department by same emergency physician without interrupting patients’ management. Micromax ultrasound system, sonosite was used to evaluate the patients. Both low frequency (2–5 MHz) curvilinear probe and high frequency (5–10 MHz) linear probe were used to get best possible findings.
Patients were examined in either supine or semirecumbent position. Areas of each chest were divide in anterior (sternum to anterior axillary line), lateral (between anterior and posterior axillary line), and posterolateral alveolar pleural syndrome (PLAPS) point. PLAPS point was observed at posterior region after minimal turning of the patient to opposite side. Each was further divided in the upper zone and lower zone (roughly by horizontal line passing through nipple), respectively. Each lung was thus divided in 6 zones.
Ultrasound findings such as artifacts (A line, B line), lung sliding, alveolar consolidation or pleural effusion, and venous analysis were recorded for each zone. Venous analysis was carried out after performing lung ultrasound in selected patients showing A profile. Venous analysis to visualize echogenic thrombus was carried out with high-frequency linear probe over internal jugular vein, subclavian vein, femoral vein, iliac veins, superior venacava, and inferior venacava. Combined results were noted in the pro forma to select diagnosis according to BLUE protocol.
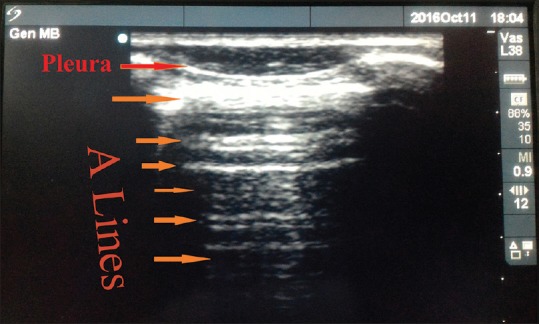
Treating units were blinded by the findings of ultrasound. The patient was prospectively followed and results of various investigations such as computed tomography (CT) scan, two-dimensional echo, chest X-ray, and other specific tests which were used by the treating unit to reach diagnosis were recorded [Table 1]. USG findings were correlated with final diagnosis made by the treating unit. Sensitivity and specificity were calculated for the each profile observed.
Table 1.
Methods of diagnosis
Ethical Committee approval was taken.
Inclusion criteria
Patients having age >12 years were included
Patients and/or relatives giving informed consent
Patients of acute respiratory distress requiring ICU admission were included.
Following were the ICU admission criteria:
Vital Signs
Pulse <40 or >150 beats/mine
Systolic arterial pressure <80 mm Hg or 20 mm Hg below the patient's usual pressure
Mean arterial pressure <60 mm Hg
Diastolic arterial pressure >120 mm Hg
Respiratory rate >35 breaths/min.
Arterial blood gas analysis
PaO2 <50 mm Hg
pH <7.1 or >7.7.
Exclusion criteria
Patients having prior diagnosis were excluded for nonbias study
Patients and/or relatives not giving consent were excluded.
RESULTS
Totally 50 patients of acute respiratory distress were evaluated with mean age of 59.64 years. 32 patients were male, and 18 patients were female.
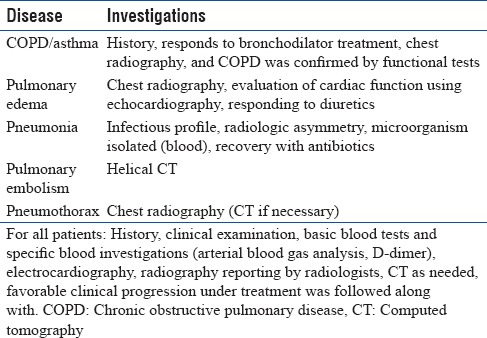
Normal lung ultrasound images are explained in Figures 1 and 2.
Figure 1.
Two rib shadows are shown in figure, hyper echoic pleura is seen, suggesting of normal lung ultrasound image
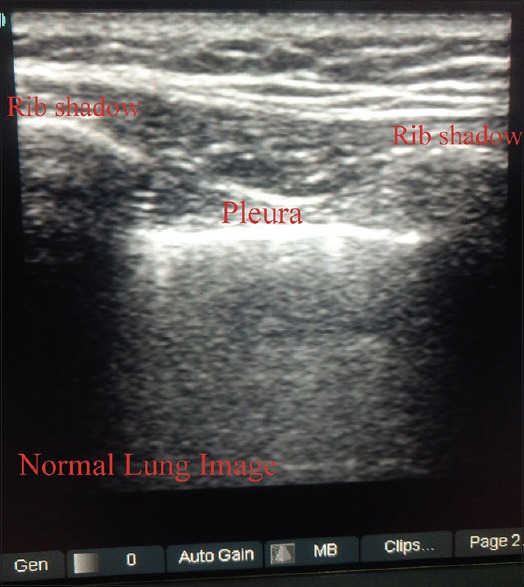
Figure 2.
Normal sea-shore pattern of lung on M-mode. M-mode shows horizontal lines suggestive of the chest wall and granular pattern suggestive of lungs
Chronic obstructive pulmonary disease/asthma
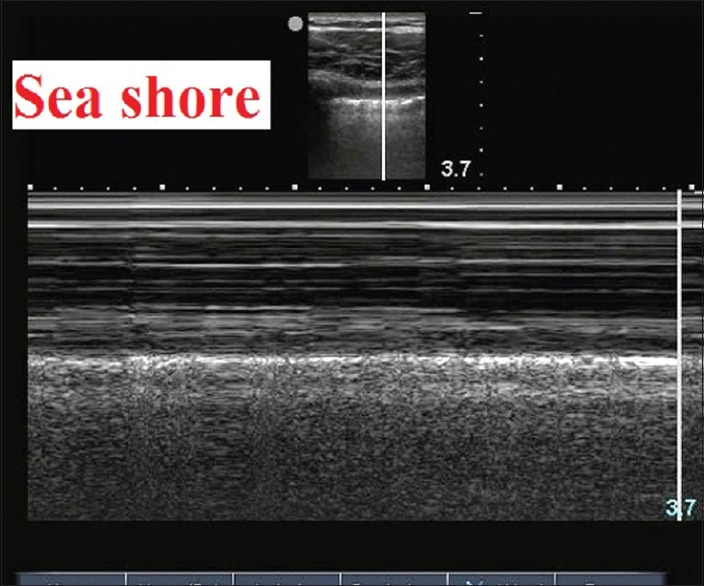
Chronic obstructive pulmonary disease (COPD) was diagnosed in 14 patients. The A profile (predominant A line with lung sliding) indicated COPD/asthma. A profile was found in 14 patients with 85.17% sensitivity and 88.88% specificity. In one case, A profile plus PLAPS (posterolateral alveolar syndrome) was observed and in one case A/B profile was observed. A lines are shown in Figure 3.
Figure 3.
A lines are the repetitive horizontal artifacts arising from the pleural line generated by subpleural air, which, either intraalveolar (normal) or abnormal (pneumothorax), blocks ultrasound waves
Pulmonary edema/interstitial syndrome
Interstitial syndrome was diagnosed in 13 patients. The B profile (predominant B + lines with lung sliding) indicated pulmonary edema. B profile was found in 12 patients with 92.30% sensitivity and 100% specificity. Normal profile was found in one case. B lines are shown in Figure 4.
Figure 4.
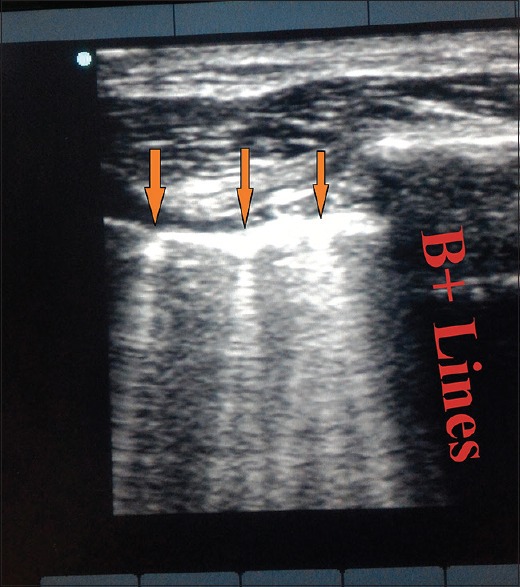
B lines reflect the coexistence of fluid and air. Fluid at the subpleural interlobular septum surrounded by air-filled alveoli gives B lines. 1 or 2 B lines in a single-ultrasound view have no significance
Pneumonia
Pneumonia was diagnosed in 17 patients. The A/B profile (A line on one side and B + line on other side), the C profile (anterior consolidation) and the A profile plus PLAPS indicated pneumonia. The A/B profile was found in 6 patients with 35.29% sensitivity and 96.96% specificity. The A profile plus PLAPS was found in 1 patient with 5.88% sensitivity and 96.96% specificity. The C profile was found in 9 patients with 52.94% sensitivity and 100% specificity. Combined (C profile + A/B profile + A profile plus PLAPS) profiles in 17 patients suggested pneumonia with 94.11% sensitivity and 93.93% specificity. Normal profile was seen in one case. Figure 5 shows pneumonia with irregular pleura.
Figure 5.
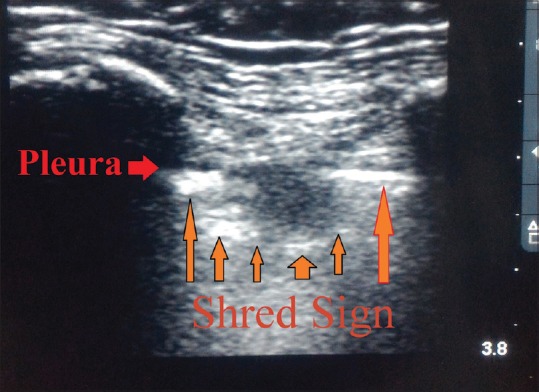
Consolidation which does not invade the whole lobe, will generate a shredded (Shred Sign), fractal boundary between the consolidation and the underlying aerated lung. Lung sliding may be present or absent
Pulmonary embolism
Pulmonary embolism was found in one patient showing A profile plus venous thrombosis. With 100% sensitivity and specificity, venous thrombosis was found in femoral vein.
Pneumothorax
Pneumothorax was found in 5 patients. The A’ profile (predominant A line without lung sliding) with lung point indicated pneumothorax. A’ profile was found in 5 patients and with lung point in 4 patients with 80% sensitivity and 100% specificity. Barcode sign was observed. Figure 6 is suggestive of pneumothorax.
Figure 6.
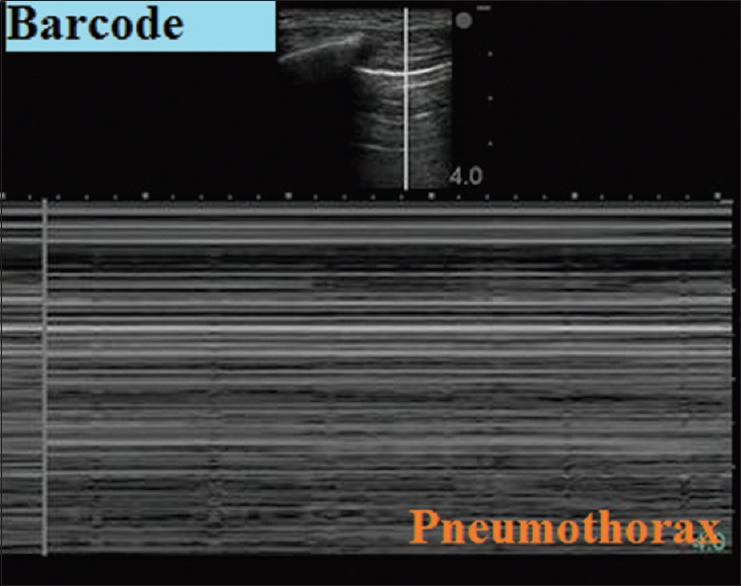
Ultrasound findings of absent lung sliding with stratosphere sign on M-mode suggests pneumothorax. The lung point (not featured here) confidently rules in the diagnosis
Figure 7 shows Pleural effusion on M-mode.
Figure 7.
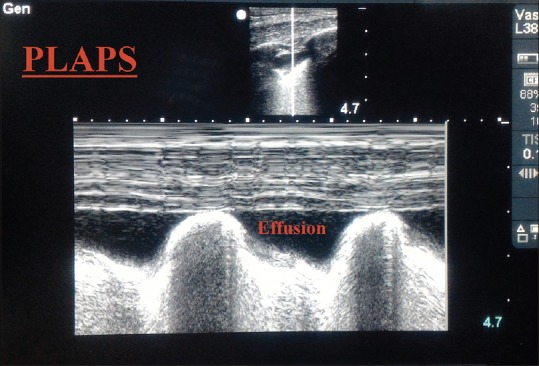
Ultrasound suggestive of pleural effusion (anechoic). The inspiratory shift of the lung line toward the pleural line is called the sinusoid sign visualized on M-mode
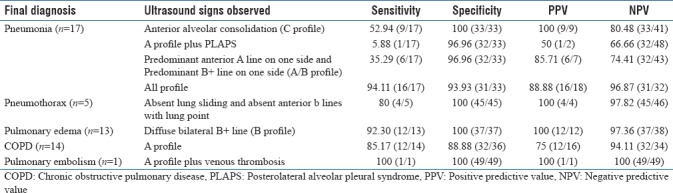
Profiles observed were as shown below in Table 2. Ultrasound Accuracy of various profiles is as shown in Table 3.
Table 2.
Combined results
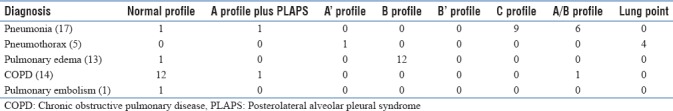
Table 3.
Ultrasound accuracy
BLUE protocol was successful in average 90.316% cases.
DISCUSSION
Briefly, a normal profile indicated COPD/asthma in an acutely breathless patient. The B profile (anterior interstitial syndrome with lung sliding) indicated pulmonary edema. The B’ profile (lung sliding abolished) indicated pneumonia. The A/B profile (asymmetric anterior interstitial syndrome) and the C profile (anterior consolidation) indicated pneumonia, as did the A profile plus PLAPS. The A profile plus venous thrombosis indicated pulmonary embolism.[3]
The pleural line is superficial. Most acute disorders reach it; acute interstitial changes involve deep as well as subpleural areas; most (98.5%) cases of acute alveolar consolidation abut the pleura; pneumothorax and pleural effusions always abut the wall. The high-acoustic impedance gradient between air and fluid generates artifacts. Air stops ultrasounds, and fluid facilitates their transmission.[3]
Chronic obstructive pulmonary disease/asthma
In COPD/Asthma, subpleural aeration is not disturbed and lung sliding is present.[2] Our study showed normal profile/A profile in 14 cases. 1 case was with A profile plus PLAPS. 1 case was with A/B profile which was later found to be associated with acute heart failure.
Pulmonary edema
Bilateral B + lines (more than two B lines) in two or more zones out of six-zone examination with or without pleural line and subpleural abnormalities are suggestive of diagnosis. Regularly spaced B lines suggest septal or interstitial edema. Crowded or coalescent B lines are suggestive of alveolar edema. Inhomogeneous B lines with pleural abnormalities irregularly spaced suggest acute respiratory distress syndrome, pleural fibrosis, or some other condition.[2] 12 cases B profile was observed. 1 case normal profile was seen. Causes of B + lines can be differentiated with the help of echocardiography and clinical features.
Pneumonia
The appearance of ultrasound images depends on the relative aeration of alveoli.[2] Pleural abnormalities may be found. Lung sliding may be abolished because of inflammatory exudates.[3] Early small alveolar consolidations appear as subpleural defects showing shred sign which gradually enlarges to form wedge-shaped deformity. Fully formed consolidation appears solid liver-like, suggestive of tissue sign.[5] Inhomogeneous unilateral/bilateral and focal/multifocal positive areas for B lines with pleural abnormalities (thickened, fragmented pleura, and subpleural consolidation) and reduced or absent lung sliding are seen in LUS in interstitial and bronchopneumonia.[2] These explain various signs observed in pneumonia. B’ profile (bilateral B + lines with abolished lung sliding) was not observed in our study. In our study A/B profile was found in 6 patients, A profile plus PLAPS was found in 1 patient, and C profile was found in 9 patients.
Pulmonary embolism
Normal profile is found mostly in pulmonary embolism. Venous scans improved sensitivity of diagnosis.[3] In our study, only 1 patient had normal profile with femoral vein thrombosis. Pulmonary embolism was proved by high-resolution CT thorax.
Pneumothorax
With collection of air between pleural layers results in the absence of lung sliding and as air blocks ultrasound waves, thus producing A’ profile. M-mode shows horizontal lines, stratosphere sign.[2] Localized pneumothorax will produce lung point whereas gross pneumothorax does not produce lung point. Lung point indicates junction of normal lung and pneumothorax.[5] In our study, A’ profile was found in 5 cases, 4 cases showed lung point.
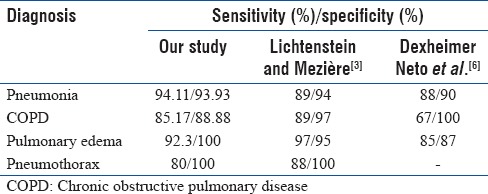
In our study, BLUE protocol was successful in average 90.316% cases. Lichtenstein and Mezière found similar accuracy of 90.5% in their study. Comparision of Efficacy is as shown in Table 4.
Table 4.
Comparison of efficacy
Stefano Parlamento et al., in their study, found pneumonia in 96.9% cases with the use of ultrasound.[7] Blaivas et al. in their study found pneumothorax with 98.1% sensitivity and 99.2% specificity.[8]
Limitation
The limitation of this study was its small sample size and the fact that it was conducted in a single center. Micro convex probe with small footprint gives better visualization. It was unavailable in our setting and thus linear probe and curvilinear probes were used. Observers were not blinded to the patient's clinical presentation.
CONCLUSION
Lung ultrasound provided the accuracy of 90.31% in diagnosis of acute respiratory distress patients. It helped to start the primary initial management of patient in the emergency room. BLUE protocol avoided the need for urgent transfer of unstable patients for CT scans and other definitive investigations, and it allowed better resuscitation in the emergency room. It can therefore be added as an adjuvant in initial methods of investigation for respiratory distress patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chacko J, Brar G. Bedside ultrasonography-applications in critical care: Part II. Indian J Crit Care Med. 2014;18:376–81. doi: 10.4103/0972-5229.133897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saraogi A. Lung ultrasound: Present and future. Lung India. 2015;32:250–7. doi: 10.4103/0970-2113.156245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest. 2008;134:117–25. doi: 10.1378/chest.07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karim A, Arora VK. Applications of ultrasonography in respiratory intensive care. Indian J Chest Dis Allied Sci. 2014;56:27–31. [PubMed] [Google Scholar]
- 5.Lee FC. Lung ultrasound-a primary survey of the acutely dyspneic patient. J Intensive Care. 2016;4:57. doi: 10.1186/s40560-016-0180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dexheimer Neto FL, Andrade JM, Raupp AC, Townsend Rda S, Beltrami FG, Brisson H, et al. Diagnostic accuracy of the bedside lung ultrasound in emergency protocol for the diagnosis of acute respiratory failure in spontaneously breathing patients. J Bras Pneumol. 2015;41:58–64. doi: 10.1590/S1806-37132015000100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parlamento S, Copetti R, Di Bartolomeo S. Evaluation of lung ultrasound for the diagnosis of pneumonia in the ED. Am J Emerg Med. 2009;27:379–84. doi: 10.1016/j.ajem.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12:844–9. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]


