Abstract
Background
Most of studies suggest the cup inclination angle is controversial. All of the studies previous have not control the prosthesis type and head diameter, it is difficult to determine relative or synergistic effects of cup angle.
Methods
We retrospectively reviewed 54 patients (61 hips) with primary total hip arthroplasties which cup inclination angle bigger than 500 after a mean 11.8 years follow-up. All the prosthesis are noncemented cup with a 28 mm metal head(Trilogy Acetabular Shell, Zimmer). The cup inclination was divided into three groups, 50–550 in 26 hips, 55–600 in 21 hips, and bigger than 600 in 14 hips. An immediate postoperative radiograph was compared with a follow-up radiograph. The polyethylene wear rates and abduction of the acetabular cups was measured in all of the patients.
Results
The preoperative mean Harris hip score improved from 47.36 to 94.3 points at 10 years. The survivorship of the cup was 100% at 10 years. The mean rate of liner wear was 0.144 ± 0.031 mm/y (0.105–0.178 mm/y) in cup inclination angle between 500–550, and 0.260 ± 0.043 mm/y (0.215–0.394 mm/y) in angle between 550–600, 0. 403 ± 0.016 mm/y (0.378–0.423 mm/y) in angle bigger than 600. The different cup inclination groups are different with liner and volumetric wear.
Conclusion
For the metal-on-polyethylene prostheses, the liner wear obvious correlate with cup inclination after angle bigger than 500. It can be concluded that the ideal abduction angle for metal-on-polyethylene prostheses should be less than 55° in hip total replacement.
Keywords: Hip arthroplasty, Cup inclination, Linear wear, Metal-on-polyethylene, Cementless
The ideal cup inclination angle has been studied extensively in THA with metal-on-polyethylene (PE) prostheses. Several studies show that cup inclination should be 45° or less because inclination greater than that is directly related to accelerated wear.1, 2, 3, 4, 5 Other studies recommend the acetabular component should be positioned (for example, some would describe ideal acetabular inclination as 45° ± 10°, while others would say 40° ± 10°). Although authors disagree the absolutely ideal acetabular inclination, it is agreed suboptimal acetabular positioning can lead to construct instability and detrimental wear characteristics.6, 7, 8, 9 However, because previous studies have not controlled head diameter or cup angle independently it is not possible to determine relative or synergistic effects of cup angle.
1. Patients and methods
We retrospectively reviewed 54 patients (61 hips) with primary total hip arthroplasties which cup inclination bigger than 500 during 2001–2004. This was a selected study because we needed radiographs of patients who were alive and active and had current follow-up, also cup inclination is bigger than 500. These operations were performed from 2001 to 2004 using a posterior approach. All patients were implanted with the noncemented cup (Trilogy Acetabular Shell, Zimmer). The technique was to ream the bony acetabulum and implant the hemispherical cup with or without screws. The cup was titanium, with 3.5-mm-thick walls. There were 3 screw holes in the posterior-superior quadrant. All were cobalt-chromium-on-PE bearing surfaces. The locking mechanism was a circumferential polyethylene tab below the rim of the liner, which engaged a recess in the shell. The articulating femoral head was 28 mm cobalt-chrome in all hips. The mean duration of follow-up was 11.8 years (range, 10–13 years). There were 33 men (36 hips) and 21 women (25 hips). The mean age at the time of the operation was 54.5 years (range, 35–71 years), and the mean weight was 71.1 kg (range, 47.6–89.2 kg). The diagnosis at the time of the operation was avascular necrosis of the head in 27, acetabular dysplasia in 22, and posttraumatic arthritis in 12 hips. The cup inclination was divided into three groups, and 500–550 in 26 hips, 550–600 in 21 hips, bigger than 600 in 14 hips (Table 1).
Table 1.
Three groups of different inclination.
| Angle of cup inclination | Hip number |
|---|---|
| 50–550 | 26 |
| 550–600 | 21 |
| >600 | 14 |
Clinical and radiographic data were collected on standardized hip evaluation at immediately postoperatively, at 6 months, and at yearly follow-up visits. The radiographs were digitized. The clinical assessment included an evaluation of pain as well as of functional parameters such as walking, stair climbing, and use of external support, limp, and ability to perform daily activities involving the hip. A composite Harris hip score was calculated on the hip basis of these data.10 Migration, lucent lines, the abduction angle, heterotopic ossification, osteolysis, and wear of PE were assessed on radiographs with a computer assisted design (ACD) system (Canvas 15.0; ACD Systems International Inc; Victoria, British Columbia, Canada) (Fig. 1). Radiolucent lines were evaluated in the 3 zones described by DeLee and Charnley.11 Osteolysis was defined as a circular or oval area of distinct bone loss. Evidence of migration was measured on the follow-up radiographs. The acetabular component was considered loose if there was 2 mm of migration from either the interteardrop or vertical lines or a change of 4° in the abduction angle.12 Heterotopic ossification was measured with the method of Brooker et al.13 Liner polyethylene wear was measured using a digital hip analysis suite.14, 15 Five measurements were taken for each patient, and a mean value was calculated. The analysis was performed on digitized radiographs. The underlying approach of the computer-assisted vector analysis of wear was to find the circles that best fitted the prosthetic femoral head and the acetabular component. The magnitude and direction of the displacement of the femoral head vector from the acetabular center were calculated on the latest follow-up radiographs.
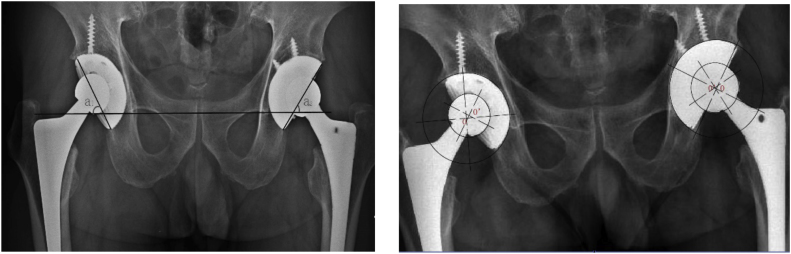
Fig. 1.
Radiograph showing measurements made. A horizontal line was drawn across the bottom of the acetabular teardrops, and a line that connected the superior and inferior edges of the acetabular component was connected to this horizontal line to measure the angle of inclination. The polyethylene wear rates were calculated by measuring the shortest radius from the center of the prosthetic femoral head to a point on the outer surface of the acetabular cup. In this figure. Cup inclination in left hip (a1) is 61.50, and right (a2) is 54.50. Liner wear of left side(o-ó) is 4.191 mm, and right side is 2.921 mm.
1.1. Statistics
The end point for survival was defined as revision or loosening in radiographs. Aseptic loosening was considered as a separate end point because “revision for any reason” included nonimplant-related operations. Kaplan-Meier survival data were used to construct the survival probabilities of implants at 10 years. Paired t-tests were used to investigate liner wear differences among different cup inclination groups. The SPSS 11.5 software package (SPSS Inc, Chicago, IL, USA) was used for the calculations with the significance level of p < 0.05.
2. Results
2.1. Clinical result
The overall clinical result was satisfactory with a mean preoperative Harris hip score at 47.36 points (range, 8–72 points) and a mean postoperative score at 94.3 points(range, 70–100 points) at the most recent examination. There was no pain in 48 hips (54 patients). When the patients with pain were questioned about location, only three (slight pain, no medication taken) stated it was “thigh” pain, and the others stated it was in the “hip” (2) or “buttock” (2).
2.2. Radiologic analysis
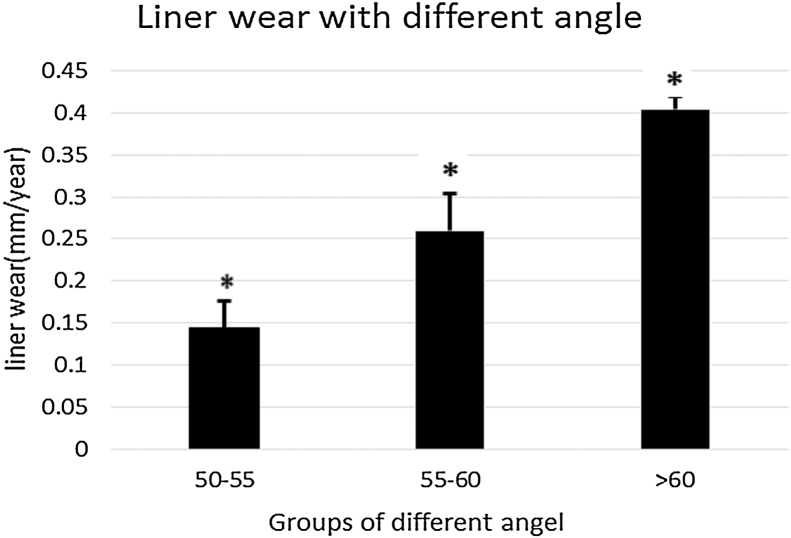
Two hips had a lucency of 2 mm, and 10 hips had a lucency less than 2 mm around the component on the initial postoperative radiograph. Of these, 6 hips had a lucency in 2 zones, 4 hips had a lucency in 1 zone, and 2 had a lucency in 3 zones. At the last follow-up, only 2 hips had a lucency in 1 zone. Acetabular osteolysis was not found in all the hips. The horizontal migration of cup is from −1.612 to 2.386 mm, and the vertical migration is from −0.932 to 2.019 mm after 10 years. No hip had a more than 4 °change in acetabular abduction after 10 years. The mean rate of liner wear was 0.144 ± 0.031 mm/y (0.105–0.178 mm/y) in cup inclination angle between 500–550, and 0.260 ± 0.043 mm/y (0.215–0.394 mm/y) in angle between 550–600, 0. 403 ± 0.016 mm/y (0.378–0.423 mm/y) in angle bigger than 600.The mean volumetric wear was 89.033 mm3/y (64.621–131.088 mm3/y), 160.190 mm3/y(132.319–219.096 mm3/y), 248.443 mm3/y (232.636–260.331 mm3/y) accordingly. The liner and volumetric wear were no relationship to sex, weight, or height. The different cup inclination groups are different with liner and volumetric wear (Fig. 2). Acetabular heterotopic ossification was seen in 2 hips (18.7%): 1 were Brooker grade 1, 1 were grade 2.
Fig. 2.
The mean rate of liner wear was 0.144 ± 0.031 mm/y (0.105–0.178 mm/y) in cup inclination angle between 500–550, and 0.260 ± 0.043 mm/y (0.215–0.394 mm/y) in angle between 550–600, 0.403 ± 0.016 mm/y (0.378–0.423 mm/y) in angle bigger than 600. There are significant difference between three groups after paired T-test (P < 0.05).
2.3. Survival of the component
No acetabular component was revised for aseptic loosening. The rate of survival at 10 years for loosening is 100%.
3. Discussion
This study confirmed that polyethylene wear, one of the principal, if not the most important, reasons for failure in THA today, was related to the inclination angle of the cup. A vertical angle of inclination of the acetabular component of more than 45° has been shown to increase the load per unit area in the superior aspect of the polyethylene.16, 17, 18 Several studies have correlated cup inclination of more than 45° to the occurrence of increased wear 19, 20, 21, 22, 23 while other studies showed have no correlation.24, 25 The reasons of the different results may due to different prosthesis, head and liner.
Several studies had showed that cup inclination should be 45° or less because inclination greater than that is directly related to accelerated wear. The principle that inclination must be kept below 45° creates a technical dilemma in acetabular preparation for cup implantation for total hip arthroplasty. Our study showed average liner wear of the inclination angle between 50°–55° is 0.144 ± 0.031 mm/y, this result was similar with most of studies.26, 27 For inclination angle bigger than 55°, the liner wear increase significantly, especially for inclination angle bigger than 60°. From our study there was increased wear in the group of patients who had a higher acetabular inclination angle although there was no effect on the clinical outcomes for patients.
There were several limitations of this study. First, this was a retrospective selected analysis with a specific criterion of a primary total hip arthroplasty in situ at least 10 years. The most accurate method of assessing the effect of any variable on clinical wear behavior is with a prospective, randomized study. In the absence of such data, however, we believe that the examination of retrospective data with T-test analysis in different inclination angle groups provides information that is clinically important to the orthopedic surgeon. A second limitation for some would be that the amount of the sample is too small. In fact, it is unusually in our primary hip arthroplasty with a cup inclination bigger than 550. Additionally, the effect of anteversion was not accounted for in this study. This omission may be considered minor with respect to results.
Of interest also are the effects of creep on wear rates. This study did not attempt to distinguish between real wear and creep, focusing instead on radiographic assessment of wear. Given that this is a clinical study and not a specific biomaterials study, we felt this omission was justified.
Given the growing clinical wisdom that wear and polyethylene deformation may contribute significantly to long-term failure, it is more important than ever to identify all factors contributing to wear in THA. Our study sought to establish a correlation between acetabular abduction of all-polyethylene cementless acetabular components and increased contact forces resulting in greater wear rates. In this study, we successes to demonstrate a correlation between abduction bigger than 500 of the acetabular components and polyethylene wear and we suggest the ideal abduction angle should be less than 55°.
References
- 1.Udomkiat P., Dorr L.D., Wan Z. Cementless hemispheric porous-coated sockets implanted with pressfit technique without screws: average ten-year follow-up. J Bone Joint Surg Am. 2002;84-A:1195. doi: 10.2106/00004623-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Schmalzried T.P., Guttmann D., Grecula M. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy J.G., Rogers W.B., Soffe K.E. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530. doi: 10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 4.Patil S., Bergula A., Chen P.C. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85-A(Suppl. 4):56–A. doi: 10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 5.Hirakawa K., Mitsugi N., Koshino T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001:135. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Barrack R.L. Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg. 2003;11:89–99. doi: 10.5435/00124635-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 7.D’Lima D.D., Urquhart A.G., Buehler K.O., Walker R.H., Colwell C.W., Jr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different headneck ratios. J Bone Joint Surg Am. 2000;82:315–321. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Jolles B.M., Zangger P., Leyvraz P.F. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 9.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 10.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty, an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737. [PubMed] [Google Scholar]
- 11.DeLee J.G., Charnley J. Radiological demarcation of cemented sockets in total hip replacements. Clin Orthop. 1976;20 [PubMed] [Google Scholar]
- 12.Massin P., Schmidt L., Engh C.A. Evaluation of cementless acetabular componen migrationt: an experimental study. J Arthroplasty. 1989;4:245. doi: 10.1016/s0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 13.Brooker A.F., Bowerman J.W., Robinson R.A. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629. [PubMed] [Google Scholar]
- 14.Hui A., McCalden R., Martell J. Validation of two and three-dimensional radiographic techniques for measuring polyethylene wear after total hip arthroplasty. J Bone Joint Surg (Am) 2003;85-A:505. doi: 10.2106/00004623-200303000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Martell J., Berdia S. Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am. 1997;79:1635. doi: 10.2106/00004623-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 16.D'Lima D.D., Chen P.C., Colwell C.W., Jr. Optimizing acetabular component position to minimize impingement and reduce contact stress. J Bone Joint Surg Am. 2001;83-A(Suppl. 2 Pt 2):87. doi: 10.2106/00004623-200100022-00005. [DOI] [PubMed] [Google Scholar]
- 17.‘Lima D.D., Urquhart A.G., Buehler K.O. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Robinson R.P., Simonian P.T., Gradisar I.M. Joint motion and surface contact area related to component position in total hip arthroplasty. J Bone Joint Surg Br. 1997;79:140. doi: 10.1302/0301-620x.79b1.6842. [DOI] [PubMed] [Google Scholar]
- 19.Udomkiat P., Dorr L.D., Wan Z. Cementless hemispheric porous-coated sockets implanted with pressfit technique without screws: average ten-year follow- up. J Bone Joint Surg Am. 2002;8-A:1195. doi: 10.2106/00004623-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Schmalzried T.P., Guttmann D., Grecula M. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy J.G., Rogers W.B., Soffe K.E. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530. doi: 10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 22.Patil S., Bergula A., Chen P.C. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85-A(Suppl. 4):56. doi: 10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 23.Hirakawa K., Mitsugi N., Koshino T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001:135. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Goosen J.H., Verheyen C.C., Tulp N.J. Mid-term wearcharacteristics of an uncemented acetabular component. J Bone Joint Surg Br. 2005;87(1475):25. doi: 10.1302/0301-620X.87B11.16101. [DOI] [PubMed] [Google Scholar]
- 25.Del Schutte H., Jr., Lipman A.J., Bannar S.M. Effects of acetabular abduction on cup wear ratesin total hip arthroplasty. J Arthroplasty. 1998;13:621. doi: 10.1016/s0883-5403(98)80003-x. [DOI] [PubMed] [Google Scholar]
- 26.Karidakis G.K. Oxidized zirconium head on crosslinked polyethylene liner in total hip arthroplasty: a 7- to 12-year In vivo comparative wear study. Clin Orthop Relat Res. 2015 Dec;473(12):3836–3845. doi: 10.1007/s11999-015-4503-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bragdon Charles R. The 2012 John Charnley Award: clinical multicenter studies of the wear performance of highly crosslinked remelted polyethylene in THA. Clin Orthop Rel Res. 2013;471(Issue 2):393–402. doi: 10.1007/s11999-012-2604-0. [DOI] [PMC free article] [PubMed] [Google Scholar]