Abstract
Background
Which patients with fractures, if any, have a lower mortality with prophylactic inferior vena cava filters has yet to be established. The purpose of this investigation is to determine if patients with low-risk fractures might benefit from a prophylactic inferior vena cava filter.
Methods
Administrative data was analyzed from the National (Nationwide) Inpatient Sample using ICD-9-CM codes. Included patients were aged 18 years or older with a primary diagnosis of non-complex fracture of the pelvis, or fracture of the femuralone, or fracture of the tibia and/or fibula.
Results
From 2003–2012, 1,479,039 patients were hospitalized with low-risk fracture. The vast majority of patients with fracture, 1,461,378 of 1,479,039 (98.8%) did not receive an inferior vena cava filter. Among those who did not receive a filter, 1,446,489 of 1,461,378 (99.0%) did not develop deep venous thrombosis or pulmonary embolism. Pulmonary embolism without a filter occurred in 7207 of 1,461,378 (0.5%) and deep venous thrombosis occurred in 7682 of 1,461,378 (0.5%). Total in-hospital all-cause mortality in those who did not receive a filter was 15,683 of 1,461,378 (1.1%). An inferior vena cava filter was inserted in 17,661 of 1,479,039 (1.2%) of patients with fractures. Most of those who received an inferior vena cava filter, 12,025 of 17,661 (68.1%) did not develop pulmonary embolism or deep venous thrombosis. Total in-hospital all-cause mortality in all patients with an inferior vena cava filter was 516 of 17,661 (2.9%).
Conclusion
The evidence is against the use of a prophylactic inferior cava vena filter in patients with a non-complex pelvic fracture or single fracture of the femur or fracture of the tibia and/or fibula.
Keywords: Pulmonary embolism, Deep venous thrombosis, Mortality, Vena cava filters, Fractures
1. Background
Inferior vena cava filters are inserted prophylactically in a large proportion of patients who receive them.1 One of the challenges of the use of inferior vena cava filters for prophylaxis is to determine categories of patients who may not benefit from prophylactic filters in order to limit unnecessary placements.2 Patients with fractures of the pelvis or long bones, intuitively, would be a group who might benefit from prophylactic inferior vena cava filters because the risk of venous thromboembolism is transient, anticoagulant prophylaxis may be contraindicated, and compression devices may be difficult to apply. Retrievable inferior vena cava filters would be appealing in patients with fractures. The purpose of this investigation is to determine the prevalence of use of prophylactic inferior vena cava filters and mortality with and without filters in patients with non-complex pelvic fractures or single fractures of the femur or fractures of the tibia and/or fibula. Our goal is to determine if such patients with fractures might benefit from a prophylactic inferior vena cava filter.
2. Methods
Administrative data was analyzed from the National (Nationwide) Inpatient Sample (NIS), Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality, 2003 through 2012.3 The NIS provides information on approximately 8 million inpatient stays yearly from about 1000 hospitals. The NIS is designed to approximate a 20% sample of United States non-Federal, short-term, general, and other specialty hospitals.3
Beginning with data from 2012, the NIS was redesigned to improve national estimates. To highlight the design change, beginning with 2012 data, the database was renamed from the “Nationwide Inpatient Sample” to the “National Inpatient Sample." The NIS is now a sample of discharge records from all Healthcare Cost and Utilization Project-participating hospitals, rather than a sample of hospitals from which all discharges were retained.3
We analyzed the prevalence of pulmonary embolism and deep venous thrombosis and in-hospital all-cause mortality according to the prophylactic use of inferior vena cava filters among patients hospitalized with a primary (first-listed) diagnosis of fracture of the pelvis, femur alone or fracture of the tibia and/or fibula.
Included patients were adults (≥aged 18 years) of both genders and all races hospitalized in short-stay hospitals from all regions of the United States. We assume that patients with a first-listed diagnosis of fracture were admitted to the hospital because of the fracture.
The International Classification of Diseases-9-Clinical Modification (ICD-9-CM) Codes for deep venous thrombosis, pulmonary embolism, fractures of the pelvis, femur, tibia and/or fibula and the procedure code for vena cava filter are shown in Table 1. Exclusions were patients with complex fractures of the pelvis (ICD-9-CM codes 808.43, 808.44, 808.53, 808.54), patients with 2 or more long bone fractures, and patients with a pelvic fracture in combination with 1 or more long bone fractures.
Table 1.
ICD-9-CM used.
| Condition | ICD 9 CM Code |
|---|---|
| Fracture of pelvis | |
| Closed fracture of acetabulum | 808.0 |
| Open fracture of acetabulum | 808.1 |
| Closed fracture of pubis | 808.2 |
| Open fracture of pubis | 808.3 |
| Closed fracture of other specified part of pelvis | 808.4 |
| Open fracture of other specified part of pelvis | 808.5 |
| Fracture of femur | |
| Fracture of shaft or unspecified part of femur closed | 821.0 |
| Fracture of shaft or unspecified part of femur open | 821.1 |
| Fracture of lower end of femur closed | 821.2 |
| Fracture of lower end of femur open | 821.3 |
| Fracture of tibia and/or fibula | |
| Fracture of upper end of tibia and/or fibula closed | 823.0 |
| Fracture of upper end of tibia and/or fibula open | 823.1 |
| Fracture of shaft of tibia and /or fibula closed | 823.2 |
| Fracture of shaft of tibia and /or fibula open | 823.3 |
| Fracture of tibia and/or fibula, torus fracture | 823.4 |
| Deep venous thrombosis | |
| Phlebitis and thrombophlebitis of deep veins of lower extremities | 451.1 |
| Phlebitis and thrombophlebitis of lower extremities, unspecified | 451.2 |
| Other venous embolism and thrombosis of inferior vena cava | 453.2 |
| Acute venous embolism and thrombosis of deep vessels of lower extremity | 453.4 |
| Pulmonary embolism | |
| Pulmonary embolism and infarction | 415.1 |
| Inferior vena cava filter | |
| Interruption Of vena cava/Insertion of implant or sieve in vena cava | 38.7 |
2.1. Statistical methods
Descriptive statistics were used. Differences of categorical variables were calculated by Fisher’s two-tailed exact test using GraphPad Software (San Diego, CA). Means and 95% confidence intervals (CI) were calculated using Graphpad Quickcalcs (Graphpad, San Diego, California). Linear regression analyses were performed using SPSS Version 22 for Windows (SPSS Inc., Chicago, IL).
3. Results
From 2003–2012, 1,479,039 patients were hospitalized with fracture of the pelvis, femur or tibia. Age was 62 ± 23 years (mean ± standard deviation). Females were 58.8%. Most, 77.4%, were white, and 9.4% were black.
The distribution of fractures was pelvis (36.1%), femur (28.9%), and tibia (35.0%). The proportion receiving an inferior vena cava filter was pelvis (1.6%), femur (1.4%), and tibia and/or fibula (0.6%) (P < 0.0001 pelvis compared with tibia and/or fibula and, femur compared with tibia and/or fibula; P = 0.01 pelvis compared to femur).
3.1. No inferior vena cava filter
The vast majority of patients with fracture, 1,461,378 of 1,479,039 (98.8%) did not receive an inferior vena cava filter. Among those who did not receive a filter, 1,446,489 of 1,461,378 (99.0%) did not develop deep venous thrombosis or pulmonary embolism (Table 2). Pulmonary embolism in those who did not receive an inferior vena cava filter occurred in 7207 of 1,461,378 (0.5%) and deep venous thrombosis occurred in 7682 of 1,461,378 (0.5%).
Table 2.
Prevalence of Use of Prophylactic Inferior Vena Filters and Mortality Among 1,479,039 Patients with Fractures.
| Condition | Prevalencea n (%) | 95% CI | Deaths (n/N) | Mortality% (95% CI) | |
|---|---|---|---|---|---|
| No IVCF | No PE, No DVT |
1,446,489/1,461,378 (99.0) | 99.0–99.0 | 14,719/1,446,489 | 1.0 (1.0–1.0) |
| PE | 7207/1,461,378 (0.5) | 0.5–0.5 | 860/7207 | 11.9 (11.2–12.7) | |
| DVT | 7682/1,461,378 (0.5) | 0.5–0.5 | 104/7682 | 1.4 (1.1–1.6) | |
| IVCF | No PE, No DVT |
12,025/17,661 (68.1) | 67.4–68.8 | 322/12,025 | 2.7 (2.4–3.0) |
| PE | 2599/17,661 (14.7) | 14.2–15.3 | 116/2599 | 4.5 (3.7–5.3) | |
| DVT | 3037/17,661 (17.2) | 16.7–17.8 | 78/3037 | 2.6 (2.1–3.2) | |
IVCF, inferior vena cava filter; CI, Confidence Interval.
P < 0.0001 comparing patients with IVCF and no IVCF.
Prevalence was calculated based on all patients with fractures (N = 1,479,040).
All-cause in–hospital mortality among patients who did not receive an inferior vena cava filter was 15,683 of 1,461,378 (1.1%)(95% CI 1.1–1.1). Among those who did not receive an inferior vena cava filter and did not develop pulmonary embolism or deep venous thrombosis, all-cause in-hospital mortality was 14,719 of 1,446,489 (1.0%) (Table 2). Among those who did not receive an inferior vena cava filter and developed pulmonary embolism, all-cause in-hospital mortality was 860 of 7207 (11.9%). Among those who did not receive an inferior vena cava filter and developed deep venous thrombosis all-cause in-hospital mortality was 104 of 7682 (1.4%).
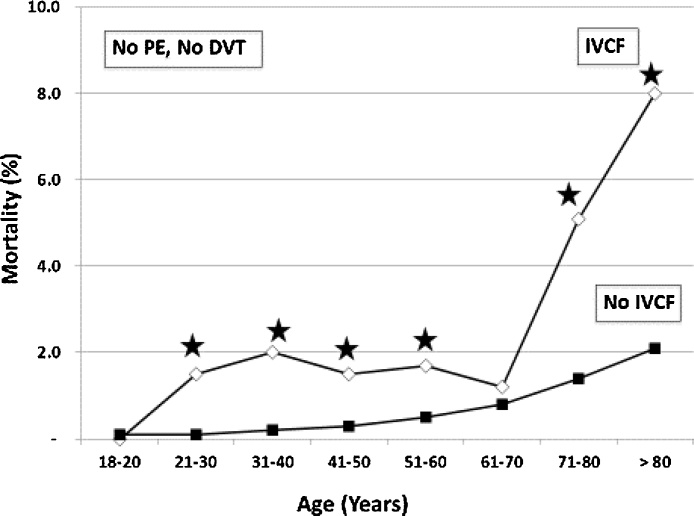
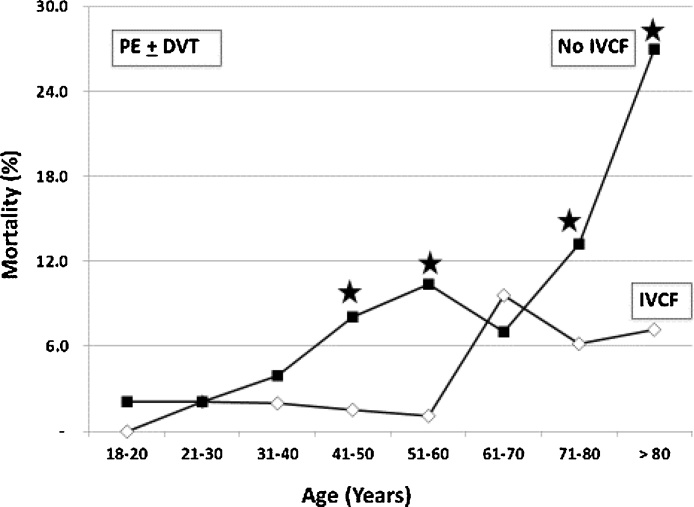
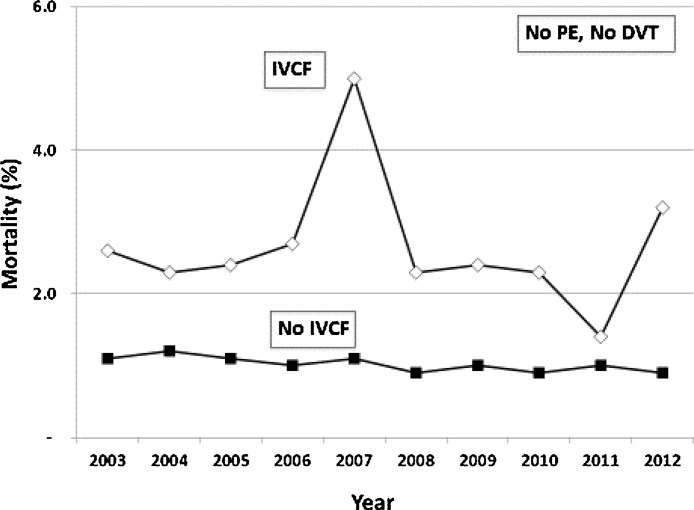
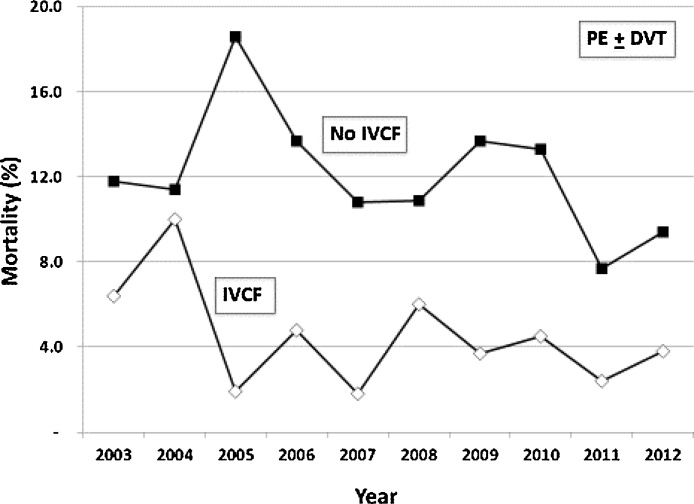
Mortality in those who did not receive an inferior vena cava filter increased with age in those with neither pulmonary embolism nor deep venous thrombosis (Fig. 1) and it increased with age in those with pulmonary embolism (Fig. 2). Mortality decreased from 1.1% in 2003 to 0.9% in 2012 in those with no inferior vena cava filter and no pulmonary embolism or deep venous thrombosis (P = 0.008) (Fig. 3). Mortality did not change from 2003 to 2012 in those with pulmonary embolism and no inferior vena cava filter (Fig. 4).
Fig. 1.
In-hospital all-cause mortality according to age and use of inferior vena cava filter (IVCF) in patients with no pulmonary embolism (PE) and no deep venous thrombosis (DVT). Mortality increased with increasing age in those who received a filter (P = 0.02) and in those who did not receive a filter (P = 0.002). Stars indicate P <0.0001 comparing mortality in those with IVCF and those with no IVCF.
Fig. 2.
In-hospital all-cause mortality according to age and use of inferior vena cava filter (IVCF) in patients with pulmonary embolism (PE) ± deep venous thrombosis (DVT). Mortality increased with increasing age in those who received a filter (P = 0.02) and in those who did not receive a filter (P = 0.006). Stars indicate P < 0.0001 comparing mortality in those with IVCF and those with no IVCF. In patients with an IVCF, it cannot be determined if the IVCF was inserted for treatment or prophylaxis.
Fig. 3.
In-hospital all-cause mortality according to use of inferior vena cava filter (IVCF) and year in patients with no pulmonary embolism (PE) and no deep venous thrombosis (DVT). Mortality did not change from 2003 to 2012 in patients with an IVCF. Mortality decreased 2003–2012 in those who did not receive a filter (P = 0.01).
Fig. 4.
In-hospital all-cause mortality according to use of inferior vena cava filter (IVCF) and year in patients with pulmonary embolism (PE) ± deep venous thrombosis (DVT). Mortality did not change from 2003 to 2012 in either group. In patients with an IVCF, it cannot be determined if the IVCF was inserted for treatment or prophylaxis.
3.2. Inferior vena cava filter
An inferior vena cava filter was inserted in 17,661 of 1,479,039 (1.2%) of patients with fractures. Most of those who received an inferior vena cava filter, 12,025 of 17,661 (68.1%) did not develop pulmonary embolism or deep venous thrombosis. It is clear, therefore, that inferior vena cava filters in these patients were inserted for prophylaxis. In 5636 of 17,661 (31.9%), we cannot determine if the filters were inserted for prophylaxis or for treatment. Among these, 2599 inferior vena cava filters were inserted in patients who had pulmonary embolism and 3037 were inserted in patients who had deep venous thrombosis.
Mortality among all fracture patients who received an inferior vena cava filter was 516 of 17,661 (2.9%)(95% CI 2.7-3.2). Among patients who received an inferior vena cava filter and did not develop pulmonary embolism or deep venous thrombosis, mortality was 322 of 12,025 (2.7%)(Table 2). Mortality among fracture patients with pulmonary embolism who received an inferior vena cava filter was 116 of 2599 (4.5%), and mortality among fracture patients with deep venous thrombosis who received an inferior vena cava filter was 78 of 3037 (2.6%).
Among patients who had pulmonary embolism, in-hospital all-cause mortality was lower in those who received an inferior vena cava filter than in those who did not, 116 of 2599 (4.5%) with filter compared with 860 of 7207 (11.9%) without filter (P < 0.0001). We do not know if these patients received a filter for prophylaxis and had a breakthrough pulmonary embolism or if they received no prophylactic filter, subsequently developed pulmonary embolism, and received a filter for treatment.
Mortality in those with an inferior vena cava filter was age-dependent in those with no pulmonary embolism or deep venous thrombosis (Fig. 1) and in those with pulmonary embolism (Fig. 2). Mortality in those with an inferior vena cava filter was comparable during all years of observation in those with no pulmonary embolism or deep venous thrombosis (Fig. 3) and in those with pulmonary embolism (Fig. 4).
3.3. Sensitivity analysis
If all patients who had pulmonary embolism or deep venous thrombosis with inferior vena cava filters received the filters for prophylaxis, and pulmonary embolism or deep venous thrombosis developed despite the filters, then in-hospital all-cause mortality with prophylactic inferior vena cava filters would have been 516 of 17,661 (2.9%)(95% CI = 2.7-3.2) compared with 15,683 of 1,461,378 (1.1%) (95% CI = 1.1–1.1) without filters.
If all patients who had pulmonary embolism or deep venous thrombosis received the inferior vena cava filter for treatment of thromboembolic disease that developed in those who did not receive a prophylactic filter, then in-hospital all-cause mortality would have been 322 of 12,025 (2.7%)(95%CI = 2.4–3.0) with filters compared with 15,877 of 1,467,014 (1.1%)(95% CI = 1.1–1.1) without filters. Therefore, irrespective of whether the inferior vena cava filters were inserted for prophylaxis or for treatment in patients with pulmonary embolism or deep venous thrombosis, the filters did not reduce overall mortality in patients with non-complex pelvic fractures, fracture of the femur alone or fracture of the tibia and/or fibula.
4. Discussion
Most patients with fractures did not receive an inferior vena cava filter, and only a small proportion of those who did not receive a filter developed pulmonary embolism or deep venous thrombosis. Mortality was not reduced by the prophylactic use of inferior vena cava filters. To the contrary, mortality was higher in those who received an inferior vena cava filter than in those who did not. This may have reflected the use of filters in more severely injured patients.
Mechanical or pharmacological prophylaxis is essential in trauma patients with severe fractures. Among trauma patients who did not receive mechanical or pharmacological antithrombotic prophylaxis, deep venous thrombosis occurred in 61 of 100 (61%) with pelvic fracture, 59 of 74 (80%) with femoral fracture, and 66 of 86 (77%) with tibial fracture.4
The prevalence of pulmonary embolism and of deep venous thrombosis was low in our population of patients who did not receive an inferior vena cava filter. We assume that patients received mechanical prophylaxis, and possibly prophylaxis with anticoagulants, but we do not have data on this.
Mortality was lower in those with pulmonary embolism who received an inferior vena cava filter than in those with pulmonary embolism who did not receive an inferior vena cava filter. If the filters were inserted for treatment of pulmonary embolism, it would suggest that inferior vena cava filters reduce mortality in patients with long bone or pelvic fractures who develop pulmonary embolism. This needs further assessment.
The placement of an inferior vena cava filter for prophylaxis in a patient without evidence of venous thromboembolism is controversial,5 and appropriate use of prophylactic inferior vena cava filters in trauma patients has yet to be definitively determined.6 Some demonstrated a significant reduction in the incidence of pulmonary embolism in trauma patients treated with prophylactic inferior vena cava filters compared with historical controls.7, 8, 9 Some, however, did not demonstrate an overall reduction of pulmonary embolism with prophylactic inferior vena cava filters in trauma patients.10 The real issue is to define who should receive a prophylactic inferior vena cava filter.11 No prospective randomized controlled trial exists to support insertion of a prophylactic inferior vena cava filter in trauma patients.11 Clinical studies with prospectively collected data and retrospective analyses support use of a prophylactic inferior vena cava filter in ‘high-risk’ trauma patients.11 The Eastern Association for the Surgery of Trauma (EAST) and the Inflammation and the Host Response to Injury Collaborative Project recommend consideration of a prophylactic filter in patients who meet high-risk criteria and cannot be anticoagulated.5, 11 This high-risk patient population includes patients with a complex (comminuted) pelvic fracture and associated long bone fracture and patients with multiple long bone fractures.11 In the present investigation we evaluate the use of prophylactic inferior vena cava filters in patients who are not at high-risk according to the EAST criteria in order to determine if lower risk trauma patients might benefit from a prophylactic inferior vena cava filter.
The ease and safety of insertion of inferior vena cava filters has encouraged physicians to consider liberalization of the indications for their use.12 In case series of less than 50 patients, investigators explored extended indications for insertion of a vena cava filter. These included 1) patients undergoing surgery for acetabular fracture with 2 or more risk factors including aged >60 years, contraindication to anticoagulants, oral contraceptives, hypercoagulable state, immobilization, malignancy, obesity, prior venous thromboembolism,13 and 2) patients undergoing joint replacement with history of venous thromboembolism.14
A strength of this investigation is the large number of patients of both genders, all ages ≥ 18 years, and all races from all regions of the United States. A weakness is the inability to determine if inferior vena cava filters in patients with pulmonary embolism or deep venous thrombosis were inserted for prophylaxis or for therapy. Patients with pulmonary embolism or deep venous thrombosis, however, were a small proportion (1.4%) of patients with fractures. We showed that the vast majority of patients with fractures did well without an inferior vena cava filter. Overall mortality was not reduced with prophylactic filters, irrespective of whether the inferior vena cava filters in those with pulmonary embolism or deep venous thrombosis were inserted for prophylaxis or treatment. Other weaknesses are no information on associated organ trauma and no information on use of anticoagulants or mechanical prophylaxis. Also we have no follow-up information after discharge.
5. Conclusion
The evidence is against the use of a prophylactic inferior vena cava filter in patients with non-complex fractures of the pelvis, fracture of the femur alone or fracture of the tibia and /or fibula.
Authors contribution
All authors had access to the data and participated in preparation of the manuscript.
Funding
None
Conflict of interest
None.
Contributor Information
Paul D. Stein, Email: steinp@msu.edu.
Fadi Matta, Email: mattaf@msu.edu.
Mary J. Hughes, Email: Mary.Hughes@hc.msu.edu.
References
- 1.Stein P.D., Matta F., Hull R.D. Increasing use of vena cava filters for prevention of pulmonary embolism. Am J Med. 2011;124:655–661. doi: 10.1016/j.amjmed.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 2.Greenfield L.J., Proctor M.C., Michaels A.J. Prophylactic vena caval filters in trauma: the rest of the story. J Vasc Surg. 2000;32:490–497. doi: 10.1067/mva.2000.108636. [DOI] [PubMed] [Google Scholar]
- 3.HCUP Databases. Healthcare Cost and Utilization Project (HCUP). February 2016. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/nisoverview.jsp. (Accessed 10 December, 2016).
- 4.Geerts W.H., Code K.I., Jay R.M., Chen E., Szalai J.P. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331(24):1601–1606. doi: 10.1056/NEJM199412153312401. [DOI] [PubMed] [Google Scholar]
- 5.Cuschieri J., Freeman B., O'Keefe G. Inflammation and the host response to injury a large-scale collaborative project: patient-oriented research core standard operating procedure for clinical care X. Guidelines for venous thromboembolism prophylaxis in the trauma patient. J Trauma. 2008;65:944–950. doi: 10.1097/TA.0b013e3181826df7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wehrenberg-Klee E., Stavropoulos S.W. Inferior vena cava filters for primary prophylaxis: when are they indicated. Semin Intervent Radiol. 2012;29:29–35. doi: 10.1055/s-0032-1302449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers F.B., Shackford S.R., Wilson J. Prophylactic vena cava filter insertion in severely injured trauma patients: indications and preliminary results. J Trauma. 1993;35:637–641. doi: 10.1097/00005373-199310000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Rogers F.B., Shackford S.R., Ricci M.A. Routine prophylactic vena cava filter insertion in severely injured trauma patients decreases the incidence of pulmonary embolism. J Am Coll Surg. 1995;180:641–647. [PubMed] [Google Scholar]
- 9.Carlin A.M., Tyburski J.G., Wilson R.F., Steffes C. Prophylactic and therapeutic inferior vena cava filters to prevent pulmonary emboli in trauma patients. Arch Surg. 2002;137:521–525. doi: 10.1001/archsurg.137.5.521. [discussion 525–527. [DOI] [PubMed] [Google Scholar]
- 10.McMurtry A.L., Owings J.T., Anderson J.T. Increased use of prophylactic vena cava filters in trauma patients failed to decrease overall incidence of pulmonary embolism. J Am Coll Surg. 1999;189:314–320. doi: 10.1016/s1072-7515(99)00137-4. [DOI] [PubMed] [Google Scholar]
- 11.Rogers F.B., Cipolle M.D., Velmahos G. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002;53:142–164. doi: 10.1097/00005373-200207000-00032. [DOI] [PubMed] [Google Scholar]
- 12.Rohrer M.J., Scheidler M.G., Wheeler H.B., Cutler B.S. Extended indications for placement of an inferior vena cava filter. J Vasc Surg. 1989;10:44–49. [discussion 49–50. [PubMed] [Google Scholar]
- 13.Webb L.X., Rush P.T., Fuller S.B., Meredith J.W. Greenfield filter prophylaxis of pulmonary embolism in patients undergoing surgery for acetabular fracture. J Orthop Trauma. 1992;6:139–145. doi: 10.1097/00005131-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Golueke P.J., Garrett W.V., Thompson J.E. Interruption of the vena cava by means of the Greenfield filter: expanding the indications. Surgery. 1988;103:111–117. [PubMed] [Google Scholar]