Abstract
Purpose
Increased focus has been put on the use of “‘real-world” data to support randomized clinical trial (RCT) evidence for clinical decision-making. The objective of this study was to assess the performance of an annular closure device (ACD) after stratifying a consecutive series of “real-world” patients by the screening criteria of an ongoing RCT.
Materials and methods
This was a single-center registry analysis of 164 subjects who underwent limited discectomy combined with ACD for symptomatic lumbar disc herniation. Patients were stratified into two groups using the selection criteria of a pivotal RCT on the same device: Trial (met inclusion; n=44) or non-Trial (did not meet inclusion; n=120). Patient-reported outcomes, including Oswestry Disability Index (ODI) and visual analog scale (VAS) for leg and back pain, and adverse events were collected from baseline to last follow-up (mean: Trial – 15.6 months; non-Trial – 14.6 months). Statistical analyses were performed with significance set at p<0.05.
Results
Patient-reported outcomes were not significantly different between groups at last (p≥0.15) and clinical success (≥15-point improvement in ODI score; ≥20-point improvement in VAS scores) was achieved in both the groups. Three non-Trial (2.5%) and three Trial (6.8%) patients experienced symptomatic reherniation (p=0.34). Rates of reoperation, ACD mesh dislocation/separation, and other radiographic findings were similar between groups (p=1.00).
Conclusion
Outcomes with the ACD appeared advantageous in both the groups, particularly in comparison with historical reherniation rates reported in the same high-risk, large annular defect population. Stratification of this “real-world” series on the basis of RCT screening criteria did not result in significant between-group differences. These findings suggest that the efficacy of the ACD extends beyond the strictly defined patient population being studied in the RCT of this device. Furthermore, reducing the reherniation rate following lumbar discectomy has positive clinical and economic implications.
Keywords: annular closure device, annular defect, discectomy, disc herniation, real-world evidence
Introduction
Randomized controlled trials (RCT) have long been considered the gold standard in clinical research design.1 Randomization helps minimize treatment allocation bias, while strict screening criteria diminish the effects of confounding variables. While RCTs aim to provide definitive empirical evidence, concerns remain as to whether these study populations adequately represent patients encountered in routine practice.1,2 Several robust reviews have substantiated this dynamic, concluding that many RCT samples lack sufficient representation of the pertinent diseased-state population.3–6 In some cases, such representation has been found to be as low as 4%–10% of intervention candidates.7–9
Inclusion criteria for RCTs are often stricter than the approved indications for a device, which can bias the RCT population relative to the patient population who will be treated in general practice. Accordingly, physicians may take caution when extrapolating RCT data to the more heterogeneous “real-world” populations whom they treat. Therefore, observational post-market studies are critical to monitor and evaluate the safety and efficacy of new therapeutic techniques. Malchau has emphasized the importance of observational data sets being produced in close proximity with RCT results.10 These post-market studies can be used to confirm the applicability of RCT results to the more generalized “real-world” populations who will be treated by most physicians.
Management of large annular defects associated with lumbar disc herniation is one area in critical need of improved therapies. Large defects in the annulus fibrosis, commonly defined as defects ≥6 mm wide, are a significant risk factor for reherniation and revision surgery, with reherniation rates reported as high as 15%–27%.11–13 In contrast, the rate of reoperation for reherniation among the general discectomy population is around 4% (95% CI: 2%–6%).14 A recent meta-analysis of over 1,500 patients observed significantly greater rates of recurrence (OR =2.5, p=0.004) and reoperation (OR =2.3, p<0.001) in patients with large vs small annular defects.15
Annular closure devices (ACD) aim to occlude or seal the defect in the annular ring and have been a strong topic of research for approximately two decades. Some devices utilize suturing techniques, with or without anchors, in an attempt to seal and reapproximate the defect.16,17 Another strategy has been to occlude the defect with a mesh insert that is anchored to one of the adjacent vertebral bodies.18 Regardless of the technology, the primary goal of an ACD is to minimize reherniation and revision. There is currently one ongoing RCT that is focused on studying the safety and efficacy of a bone-anchored ACD in patients with large annular defects following lumbar discectomy (Clinicaltrials. gov ID: NCT01283438).
Various inclusion criteria for this ongoing RCT, such as minimum pain and disability scores, result in the exclusion of many patients from the trial. Based on the indications of this ACD, many of these patients would still be eligible for treatment. The goal of the current study was to determine if the clinical outcomes would differ between patients who meet the strict RCT inclusion criteria and those who do not. This is a retrospective registry analysis of all patients who were treated with this ACD at a single site. Considering the immense diversity that exists among lumbar discectomy patients and surgical techniques, addressing the questions of safety and efficacy of this ACD in a wider spine care population is highly advantageous.19
Materials and methods
Study design and data collection
This was a single-center retrospective registry study of 164 subjects who underwent limited lumbar discectomy augmented with an ACD (ResearchRegistry.com UIN: 3392). This study was designed to include patients enrolled in an ongoing RCT (Clinicaltrials.gov ID: NCT01283438) as well as patients who did not meet inclusion criteria for the RCT but received the same ACD intervention. Clinical data collection was cleared by the local medical ethics committee (Ethics Committee of the Bavarian Medical Association), and all patient data were anonymized. All clinical outcomes and patient imaging had been collected previously in accordance with institutional standard-of-care. All procedures were performed in an academic medical center between July 2009 and November 2015 across 15 surgeons, all of whom were experienced in both limited discectomy and the ACD techniques.
Patient selection and stratification
All patients presented with posterior or posterolateral symptomatic disc herniations at one level between L1 and S1 with radiographic confirmation of neural compression via magnetic resonance imaging (MRI). All patients were subsequently treated with limited lumbar discectomy and ACD instrumentation. Patient stratification for this registry study was then performed by using the selection criteria of the ongoing RCT (Clinicaltrials.gov ID: NCT01283438) evaluating the same ACD intervention. Patients meeting RCT inclusion were classified as “Trial” patients, while those who did not were considered “non-Trial” patients.
Preoperative inclusion criteria:
Failed at least 6 weeks of conservative therapy
Leg pain graded on the visual analog scale (VAS) higher than 40/100
Dysfunction graded on the Oswestry Disability Index (ODI) greater than 40/100
Age of 21–75 years
No prior herniation at the index level
Intraoperative inclusion criteria:
Minimum posterior disc height of 5 mm
Minimum/maximum annular defect height of 4/6 mm
Minimum/maximum annular defect width of 6/12 mm (patients with defects wider than 10 mm were assigned to the non-Trial group, as the 12 mm ACD was not available for clinical use when the RCT was initiated)
Hypothesis
The authors hypothesized that both patient-reported and radiographic outcomes at last follow-up would not be significantly different between groups given the conservative nature of limited discectomy and the mechanical occlusion properties of the ACD.
Surgical technique
A standard posterior lumbar-limited discectomy was performed in all cases. All patients received prophylactic antibiotics shortly before skin incision. In some patients, the discectomy could be performed through the interlaminar space alone, especially in L5/S1. A small unilateral laminotomy was performed in the remaining patients. Medial facetectomy was avoided unless the medial facet was impinging on the nerve root after discectomy. Standard limited discectomy with the removal of all loose fragments outside the disc space was performed without entering the disc space with any instrumentation.
Following discectomy, the extent of the annular defect was measured and the appropriately sized ACD was implanted under fluoroscopic guidance in accordance with the manufacturer’s surgical technique manual. Upon discharge, patients were given standardized post-surgery care instructions per institutional standard-of-care, without any additional bracing or other activity restrictions. Patients with persisting neurological deficits were recommended to do physical therapy or sent to rehabilitation centers, while all other patients were allowed to perform activities as tolerated.
ACD
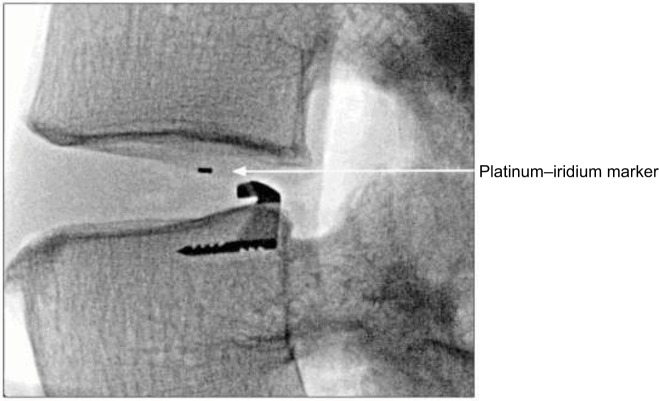
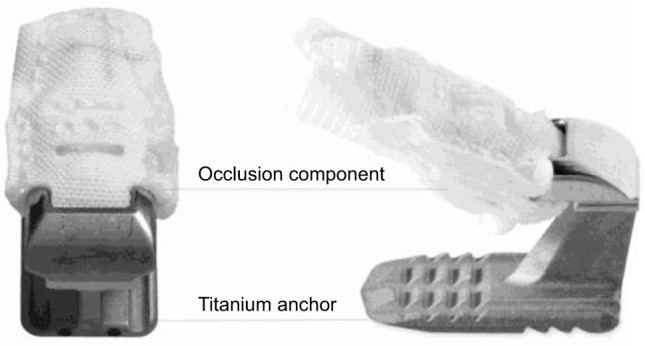
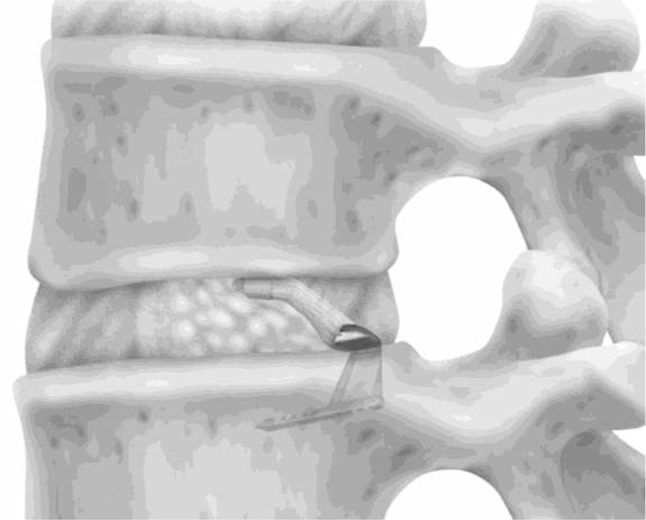
The ACD under consideration in this study (Barricaid®; Intrinsic Therapeutics, Woburn, MA, USA) is intended for use as an adjunct to lumbar discectomy surgery (Figures 1 and 2). It is designed to block large annular defects following a sequestrectomy or limited discectomy, preventing extrusion of the nucleus material from within the disc space. The device consists of two components, a flexible mesh component that blocks the defect and inhibits nucleus extrusion (the mesh overlies the residual nucleus) and a bone anchor that secures the mesh component to one of the adjacent vertebral bodies. The mesh material is woven polyester (Dacron). A platinum–iridium marker within the polymer mesh allows visualization on plain radiographs (Figure 3). The bone anchor is composed of Ti6AL-4V ELI. The anchor is placed into one of the adjacent vertebral bodies via tamp and mallet. The implant is available in three mesh widths (8, 10, and 12 mm) and is provided pre-loaded on a disposable delivery tool.
Figure 1.
Annular closure device possessing a mesh occlusion component and titanium anchor.
Figure 2.
Rendering of annular closure device following implantation.
Figure 3.
Postoperative plain radiograph showing platinum–iridium marker within the annular closure device polymer mesh.
Study follow-up and outcome measures
Data were collected at baseline (preoperative) and at all follow-up visits, with the last follow-up visit serving as the comparison to baseline measures. ODI scores and VAS leg and VAS back scores were collected at all time points. Plain radiographs (lateral, anterior/posterior, and flexion/extension) and functional imaging (magnetic resonance images [MRIs] or computed tomography [CT] scans) were obtained preoperatively, with plain radiographs collected again at follow-up to confirm implant position. Postoperative functional imaging was used in any instance in which the patient reported pain. Reasons for CT instead of MRI included contraindications or long waiting lists for MRI, with the majority receiving MRI.
Clinical success was defined as a 15-point improvement in ODI score and a 20-point improvement in VAS leg and back scores, as defined by prior lumbar device studies.20,21 Ipsilateral and contralateral reherniations were confirmed via functional imaging and reported as adverse events. Reherniation was considered to be any protrusion, extrusion, or sequestration of disc material and classified as symptomatic or asymptomatic. All functional imaging was reviewed by a single spine surgeon. Additional reoperations and complications occurring within follow-up were also reported. The disc height was measured 2–3 mm from the posterior aspect of the vertebral bodies by using lateral radiographs that were collected pre- or peri-operatively and at last follow-up.
Statistical analysis
Fisher’s exact test was used for between-group comparisons of categorical demographic and surgical variables. The same analysis was performed for comparing clinical success rates as well as clinical and radiographic complication rates. An unpaired t-test was used for normally distributed variables and the Wilcoxon rank-sum test was used for all other variables, such as defect area, operative time, latest follow-up, and outcome scores. In addition to Trial vs non-Trial comparisons, a subgroup analysis was conducted between primary discectomy and repeat discectomy patients by using the same analysis techniques. Statistical significance was set at p<0.05 for all comparisons.
Ethics approval and informed consent
Clinical data collection was cleared by the local medical ethics committee. All clinical outcomes and patient imaging had been collected previously in accordance with institutional standard-of-care.
Results
Patient demographics
During the study review period, 221 patients received limited discectomy with the ACD. Of the 221, 19 were participants of the aforementioned RCT and were excluded from this analysis since the RCT protocol prohibited subjects from participation in other studies. Of the remaining sample (n=202), follow-up data were available for 164 consecutive patients, of which all were subsequently screened against the RCT inclusion/exclusion criteria. Inclusion criteria and metrics that constituted failure to meet inclusion criteria are outlined in Table 1. Forty-four patients (27%) met the RCT inclusion criteria (Trial group) and 120 patients (73%) did not (non-Trial group). Only three patients (3/164; 1.8%) had an annular defect measuring <6 mm in width. Average time to last follow-up was 15.6 months (range: 1–64.5 months) in the Trial group and 14.6 months (range: 1–71.8 months) in the non-Trial group.
Table 1.
Summary of exclusion criteria resulting in subject conversion to non-trial group
| Inclusion criteria | Proportion excluded: % (n/164) |
|---|---|
| 6 weeks conservative care | <6 weeks conservative care: 51.2% (84/164) |
| ODI and/or VAS leg ≥40 | ODI <40: 25.6% (42/164) VAS leg <40: 7.9% (13/164) |
| Primary discectomy | Subsequent discectomy/recurrence: 14.0% (23/164) |
| Defect width ≥6 mm and ≤10 mm | <6 mm: 1.8% (3/164) >10 mm: 9.1% (15/164) |
| Defect height ≥4 mm and ≤6 mm | <4 mm or >6 mm: 6.7% (11/164) |
| Posterior disc height ≥5 mm | <5 mm: 4.9% (8/164) |
| Age ≥21 years and ≤75 years | <21 years: 2.4% (4/164) >75 years: 0.6% (1/164) |
Abbreviations: ODI, Oswestry disability Index; VAS, visual analog scale.
Contributors for patients being categorized as non-Trial included <6 weeks conservative treatment (84/164 or 51%), preoperative ODI scores <40 (42/164 or 26%), and discectomies for recurrent herniation (23/164 or 14%), with some patients having more than one contributor (Table 1).
Demographic and surgical characteristics were compared between Trial and non-Trial groups. No statistically significant differences were identified, indicating that the groups were well-matched (p>0.05, Table 2).
Table 2.
Patient demographics stratified by group
| Demographic | Trial group (n=44) | Non-Trial group (n=120) | p-value |
|---|---|---|---|
| Gender (male: female) | 25 M: 19 F | 66 M: 54 F | 0.86 |
| Operative level | |||
| L2–3 | 1 | 0 | 0.67 |
| L3–4 | 1 | 4 | |
| L4–5 | 25 | 69 | |
| L5–6 | 0 | 1 | |
| L5–S1 | 17 | 45 | |
| Defect area (mm2) | 39.2±8.9 | 44.2±13.9 | 0.08 |
| Age (years) | 46.7±12.8 | 45.6±14.3 | 0.56 |
| Operative time (min) | 97.5±36.8 | 93.5±34.0 | 0.54 |
| Operative side (left: right) | 21 L : 23 R | 64 L : 56 R | 0.60 |
| Mean latest follow-up (months) | 15.6±13.7 | 14.6±11.1 | 0.99 |
Note: Average values are presented as “mean±SD.”
Outcome measures
Mean preoperative ODI, VAS leg, and VAS back scores were significantly different between the two groups, with worse scores in the Trial group (p≤0.04). This is likely attributable to the inclusion criteria of ODI and VAS scores >40 for the Trial group. However, these scores were not significantly different between the Trial and non-Trial groups at last follow-up (p≥0.15) (Table 3).
Table 3.
ODI, VAS leg, and VAS back scores at baseline and last follow-up, stratified by group
| Outcome metric | Trial group (n=44) | Non-Trial group (n=120) | p-value |
|---|---|---|---|
| Baseline (preoperative) | |||
| ODI | 59.5±13.8 | 50.5±22.5 | 0.03* |
| VAS leg | 87.7±12.6 | 76.1±25.5 | 0.02* |
| VAS back | 67.0±28.2 | 55.7±31.7 | 0.04* |
| Last follow-up | |||
| ODI | 24.2±20.8 | 18.7±17.4 | 0.15 |
| VAS leg | 28.2±29.9 | 27.6±27.6 | 0.97 |
| VAS back | 38.4±32.7 | 30.5±24.8 | 0.28 |
Notes:
p<0.05.
Average values are presented as “mean±SD.”
Abbreviations: ODI, Oswestry Disability Index; VAS, visual analog scale.
Clinical success, defined as 15-point improvement in ODI score and 20-point improvement in VAS scores, was achieved in both the groups. No statistically significant differences were observed at last follow-up between groups for any index (p≥0.11) (Table 4). In addition, the change in disc height was not significantly different between the Trial (−0.38±0.69 mm) and non-Trial (−0.39±0.59 mm) groups (p=0.66).
Table 4.
Rate of clinical success* based on ODI, VAS leg, and VAS back scores
| Outcome metric | Trial group (n=44) | Non-Trial group (n=120) | p-value |
|---|---|---|---|
| ODI | 84% (37/44) | 71% (85/120) | 0.11 |
| VAS leg | 84% (37/44) | 79% (94/119) | 0.52 |
| VAS back | 68% (30/44) | 62% (74/119) | 0.58 |
Note:
Defined as 15-point improvement in ODI score and 20-point improvement in VAS scores.
Abbreviations: ODI, Oswestery Disability Index; VAS, visual analog scale.
Reherniations
Three patients (2.5%) in the non-Trial group and three patients (6.8%) in the Trial group had symptomatic reherniations (p=0.34). Asymptomatic reherniations occurred in three non-Trial patients (2.5%) and two (4.5%) Trial patients (p=0.61).
Reoperations and other adverse events
Reoperation rates and radiographic findings were statistically similar between the two groups (p=1.00). In total, there were three (6.8%) subsequent surgical interventions in the Trial group and 11 (9.2%) in the non-Trial group as summarized in Table 5. In each group, two of the aforementioned, symptomatic, reherniations were treated with repeat discectomies. In the non-Trial group, four reoperations were performed in a single patient to treat a wound infection. Details of two reoperations could not be confirmed as each patient went to a different institution.
Table 5.
Rates of subsequent surgical interventions
| Intervention type | Trial group (n=44) | Non-Trial group (n=120) |
|---|---|---|
| Fusion | 1 (2.3%) | 2 (1.7%) |
| Discectomy | 2 (4.5%) | 3 (2.5%) |
| Wound | 0 (0.0%) | 4 (3.3%) |
| Decompression | 0 (0.0%) | 3 (2.5%) |
| Unknown* | 0 (0.0%) | 2 (1.7%) |
Note:
Performed outside of institution.
Migration or loosening of the bone anchor was not observed in any case. There were 15 patients (9.1%) with mesh migrations and/or separations from the implant with 10 (8.3%) in the non-Trial group and 5 (11.4%) in the Trial group. Of these 15 patients, two had undergone reoperation prior to the last follow-up. Migrations included dorsal or medial movements of the mesh from its immediate postoperative position (n=6 in non-Trial, n=4 in Trial) without separation from the anchor. Separations of the mesh from the anchor (n=4 in non-Trial, n=1 in Trial) were usually preceded by radiographically identified migrations that were observed as early as 1.8 months postoperative with an average time to separation of 25.9 months (range: 3.5–57.7 months). Both the overall rate of mesh dislocations and the rate of mesh separations were statistically similar between the two groups (p=1.00). At last follow-up, two of the 15 patients with mesh migrations had radicular pain, but did not have significant neurological deterioration or motor deficits. One of those patients was treated with a subsequent fusion and the other did not require additional therapy.
Recurrent herniation patients
In the non-Trial group, 23 patients (14%) had a prior discectomy. At mean last follow-up (12 months; range: 1–24 months), no symptomatic or asymptomatic reherniations occurred in this subgroup. Furthermore, patient-reported outcomes for this prior discectomy group were not significantly different from patients who received a primary discectomy (p>0.3). Of the two patients in this subgroup who received a subsequent surgery, one patient was treated with fusion for degenerative disc disease and one was treated at a different institution with no available details.
Discussion
Comparison of RCT data to observational registry data is increasingly performed within spine research.22,23 Malchau has led this trend across musculoskeletal research, offering a stepwise approach to medical device introduction that seeks to substantiate RCTs by the collection of real-world evidence.10 One such example is Staub et al, a retrospective analysis of registry data, which examined patient-reported outcomes after total disc arthroplasty vs anterior interbody fusion and compared the results with the corresponding RCTs.24 These comparisons provide external validity for the extrapolation of RCT data for treatment decision-making when real-world patients are outside of the strict study inclusion criteria.
In this analysis, the authors examined 164 consecutive patients who had undergone limited discectomy with an ACD, mirroring the same intervention of an ongoing RCT. The observational group was screened against the RCT selection criteria and patients were stratified into Trial and non-Trial segments for comparative purposes. Preoperative and intraoperative demographics were not significantly different between the groups, except when comparing patient-reported outcomes. The Trial group had significantly worse preoperative ODI, VAS leg, and VAS back scores (p≤0.04). These differences were not unexpected, however, since the RCT was designed to include a high-risk discectomy population with ODI and VAS scores >40. Patients with better preoperative scores were more likely to be included in the non-Trial group, with 34% of non-Trial patients qualifying under this criterion alone.
Clinical success rates between the groups tended to favor Trial patients but did not reach a statistically significant difference. The favoring of Trial patients was most likely due to this group beginning with a mean preoperative ODI score that was nearly 10 points worse than that of non-Trial patients. Therefore, Trial patients had more room to improve than non-Trial patients. It is important to note that improvements in ODI and VAS scores are attributable to the successful nerve decompression that is achieved during the discectomy procedure, independent of the ACD. The efficacy of the ACD is primarily realized by minimizing the risk of reherniation, which is often associated with symptom recurrence.18
Symptomatic reherniation, a primary concern with limited lumbar discectomy, was marginalized in both the groups, with the Trial group exhibiting a higher recurrence rate (6.8% vs 2.5%) (p=0.34). These rates compare favorably to the literature on recurrence rates in limited discectomy patients with large annular defects (15%–27%).11–13 Each of those studies examined patients by using screening criteria similar to those of the RCT and Trial group presented here, specifically targeting large annular defect (≥6 mm) patients. Given the large annular defect area of non-Trial and Trial patients (44.3±13.9 and 39.2±8.9 mm2, respectively), the rates of recurrent herniation in the present study (2.5%–6.8%) suggest increased efficacy of limited discectomy when augmented with an ACD, relative to the literature rates of limited discectomy alone (15%–27%). Furthermore, within the non-Trial group, no reherniations (with or without radicular symptoms) were observed in those patients who had undergone previous discectomy, demonstrating similar outcome scores to those patients who had undergone primary discectomy (p>0.3). These trends compare favorably to the literature in which Osterman et al reported that patients with one reoperation after lumbar discectomy had a 25.1% cumulative risk of subsequent surgical intervention within 10-year follow-up.25
The mesh occlusion component partially or completely migrated from the bone anchor in 15 patients (9.1%). The non-Trial and Trial patients were similarly susceptible to these migrations, indicating that an increased risk does not exist among the more generalized treatment population. Only two of those patients reported radicular pain, without any significant neurological dysfunction or motor deficits. Based on this study, a clear relationship between mesh migration and clinical outcomes could not be identified. A 2-year sub analysis on the RCT data of this device examined the association of vertebral endplate changes (VEPC) with device complications and clinical outcomes.26 There were less mesh migrations in the subgroup with VEPC vs those without VEPC (1% vs 11%). Furthermore, VEPC and mesh subsidence were not correlated with any clinical outcomes in the ACD group. Those findings suggest that the mesh migrations may be a minor complication with respect to clinical outcomes. Continual follow-up with patients to monitor these mesh migrations will be important to better understand the effects of such complications.
Study limitations
The authors acknowledge that there were limitations in this analysis. Nonstandardized follow-up, with no minimal last follow-up is inconsistent with the RCT design. However, since mean last follow-up was consistent between groups, any effect of this variation is diminished for the purpose of this analysis. An additional limitation was the study being conducted at a single-center on a sample size that may render insufficient statistical power for some analyses. Future analyses with longer follow-up on larger sample sizes can be done to further substantiate the present findings.
Conclusion
This study supports the conclusion that data from an ongoing RCT can be extrapolated to certain patients falling outside its selection criteria. However, more definitive extrapolation can only be fully considered in the context of whether other real-world outcomes align with those reported from the RCT. Outcomes observed with the technique of combining limited discectomy with an ACD in this study were favorable in comparison with historical reherniation rates in the same large annular defect population. Long-term outcomes from the RCT will better address the efficacy of this ACD, but the current study supports that similar outcomes can be expected in a more generalized patient population.
Acknowledgments
This study was investigator initiated and performed without outside funding support. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors would like to thank Telos Partners, LLC, for their logistical contributions and organizational efforts.
Footnotes
Disclosure
Both the authors (AK and SAR) have previously received research support fees from Intrinsic Therapeutics, Inc. in accordance with being site investigators for an industry (Intrinsic)-sponsored clinical trial. AK has received consulting fees (unrelated to this study) from Intrinsic Therapeutics, Inc.
Author contributions
Both the authors contributed to study design, data collection, analysis, interpretation, drafting and revising manuscript, final approval, accountability for accuracy, and integrity.
References
- 1.Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ. 1996;312(7040):1215–1218. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price D, Bateman ED, Chisholm A, et al. Complementing the randomized controlled trial evidence base. Evolution not revolution. Ann Am Thorac Soc. 2014;11(Suppl 2):S92–S98. doi: 10.1513/AnnalsATS.201308-276RM. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy-Martin T, Curtis S, Faries D, Robinson S, Johnston J. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials. 2015;16:495. doi: 10.1186/s13063-015-1023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lisspers K, Teixeira P, Blom C, et al. Are pharmacological randomised controlled clinical trials relevant to real-life asthma populations? A protocol for an UNLOCK study from the IPCRG. NPJ Prim Care Respir Med. 2016;26:16016. doi: 10.1038/npjpcrm.2016.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruokoniemi P, Sund R, Arffman M, et al. Are statin trials in diabetes representative of real-world diabetes care: a population-based study on statin initiators in Finland. BMJ Open. 2014;4(6):e005402. doi: 10.1136/bmjopen-2014-005402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ziemssen F, Feltgen N, Holz FG, et al. Demographics of patients receiving Intravitreal anti-VEGF treatment in real-world practice: healthcare research data versus randomized controlled trials. BMC Ophthalmol. 2017;17(1):7. doi: 10.1186/s12886-017-0401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa DJ, Amouyal M, Lambert P, et al. How representative are clinical study patients with allergic rhinitis in primary care? J Allergy Clin Immunol. 2011;127(4):920–926.e921. doi: 10.1016/j.jaci.2010.10.058. [DOI] [PubMed] [Google Scholar]
- 8.Hlatky MA, Califf RM, Harrell FE, Jr, Lee KL, Mark DB, Pryor DB. Comparison of predictions based on observational data with the results of randomized controlled clinical trials of coronary artery bypass surgery. J Am Coll Cardiol. 1988;11(2):237–245. doi: 10.1016/0735-1097(88)90086-1. [DOI] [PubMed] [Google Scholar]
- 9.Wong GW, Miravitlles M, Chisholm A, Krishnan JA. Respiratory guidelines – which real world? Ann Am Thorac Soc. 2014;11(Suppl 2):S85–S91. doi: 10.1513/AnnalsATS.201309-298RM. [DOI] [PubMed] [Google Scholar]
- 10.Malchau H. Introducing new technology: a stepwise algorithm. Spine (Phila Pa 1976) 2000;25(3):285. doi: 10.1097/00007632-200002010-00004. [DOI] [PubMed] [Google Scholar]
- 11.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85-A(1):102–108. [PubMed] [Google Scholar]
- 12.Kim KT, Lee DH, Cho DC, Sung JK, Kim YB. Preoperative risk factors for recurrent lumbar disk herniation in L5–S1. J Spinal Disord Tech. 2015;28(10):E571–E577. doi: 10.1097/BSD.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 13.Zhou B, Kun W, Hong X, et al. Adjacent level disc degeneration: a prognostic factor for recurrent lumbar disc herniation after transforaminal endoscopic lumbar discectomy in 409 cases. Int J Clin Exp Med. 2016;9(11):21854–21859. [Google Scholar]
- 14.Virk SS, Diwan A, Phillips FM, Sandhu H, Khan SN. What is the rate of revision discectomies after primary discectomy on a national scale? Clin Orthop Relat Res. 2017;475(11):2752–2762. doi: 10.1007/s11999-017-5467-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller LE, McGirt MJ, Garfin SR, Bono CM. Association of annular defect width after lumbar discectomy with risk of symptom recurrence and reoperation: systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976) 2018;43(5):E308–E315. doi: 10.1097/BRS.0000000000002501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey A, Araghi A, Blumenthal S, Huffmon GV; Anular Repair Clinical Study Group. Prospective, multicenter, randomized, controlled study of anular repair in lumbar discectomy: two-year follow-up. Spine (Phila Pa 1976) 2013;38(14):1161–1169. doi: 10.1097/BRS.0b013e31828b2e2f. [DOI] [PubMed] [Google Scholar]
- 17.Qi L, Li M, Si H, et al. The clinical application of “jetting suture” technique in annular repair under microendoscopic discectomy: a prospective single-cohort observational study. Medicine (Baltimore) 2016;95(31):e4503. doi: 10.1097/MD.0000000000004503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klassen PD, Bernstein DT, Kohler HP, et al. Bone-anchored annular closure following lumbar discectomy reduces risk of complications and reoperations within 90 days of discharge. J Pain Res. 2017;10:2047–2055. doi: 10.2147/JPR.S144500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilke HJ, Ressel L, Heuer F, Graf N, Rath S. Can prevention of a reherniation be investigated? Establishment of a herniation model and experiments with an anular closure device. Spine (Phila Pa 1976) 2013;38(10):E587–E593. doi: 10.1097/BRS.0b013e31828ca4bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller LE, Block JE. Interspinous spacer implant in patients with lumbar spinal stenosis: preliminary results of a multicenter, randomized, controlled trial. Pain Res Treat. 2012;2012:823509. doi: 10.1155/2012/823509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zigler JE, Glenn J, Delamarter RB. Five-year adjacent-level degenerative changes in patients with single-level disease treated using lumbar total disc replacement with ProDisc-L versus circumferential fusion. J Neurosurg Spine. 2012;17(6):504–511. doi: 10.3171/2012.9.SPINE11717. [DOI] [PubMed] [Google Scholar]
- 22.Berg S, Tropp H. Results from a randomized controlled study between total disc replacement and fusion compared with results from a spine register. SAS J. 2010;4(3):68–74. doi: 10.1016/j.esas.2010.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jee YM, Bak JS, Weinlander E, Anderson PA. Comparing nonrandomized observational studies with randomized controlled trials in cervical disc arthroplasty: a meta-analysis. Spine (Phila Pa 1976) 2016;41(5):419–428. doi: 10.1097/BRS.0000000000001377. [DOI] [PubMed] [Google Scholar]
- 24.Staub LP, Ryser C, Roder C, et al. Total disc arthroplasty versus anterior cervical interbody fusion: use of the Spine Tango registry to supplement the evidence from randomized control trials. Spine J. 2016;16(2):136–145. doi: 10.1016/j.spinee.2015.11.056. [DOI] [PubMed] [Google Scholar]
- 25.Osterman H, Sund R, Seitsalo S, Keskimaki I. Risk of multiple reoperations after lumbar discectomy: a population-based study. Spine (Phila Pa 1976) 2003;28(6):621–627. doi: 10.1097/01.BRS.0000049908.15854.ED. [DOI] [PubMed] [Google Scholar]
- 26.Kursumovic A, Kienzler JC, Bouma GJ, et al. Morphology and clinical relevance of vertebral endplate changes following limited lumbar discectomy with or without bone-anchored annular closure. Spine (Phila Pa 1976) 2018 Mar 13; doi: 10.1097/BRS.0000000000002632. Epub. [DOI] [PubMed] [Google Scholar]