Abstract
Background
The number of black trauma deaths attributable to racial disparities is unknown. The objective of this study is to quantify the excess mortality suffered by black patients given disparities in the risk of mortality.
Materials and Methods
A retrospective analysis of patients aged 16–65 years with blunt and penetrating injuries included in the National Trauma Data Bank (NTDB) from 2007–2010 was performed. Generalized linear modeling estimated the relative risk of death for black patients versus white patients, adjusting for known confounders. This analysis determined the difference in the observed number of black trauma deaths at Level I and II centers and the expected number of deaths if the risk of mortality for black patients had been equivalent to that of white patients.
Results
1.06 million patients were included. Among patients with blunt and penetrating injuries at Level I trauma centers, white males and females had a relative risk of death of 0.82 (95% CI 0.80, 0.85) and 0.78 (95% CI 0.74, 0.83), respectively, compared with black patients. Similarly, at Level II trauma centers white males and females had a relative risk of death of 0.84 (95% CI 0.80, 0.88) and 0.82 (95% CI 0.73, 0.91). Overall, of the estimated 41,613 deaths that occurred at Level I and II centers, 2,206 deaths (5.3%) were excess deaths among black patients.
Conclusions
Over a four year period, approximately five percent of trauma center deaths could be attributed to racial disparities in trauma outcomes. These data underscore the need to better understand and intervene against the mechanisms that lead to trauma outcomes disparities.
Keywords: Trauma outcomes, mortality, disparities
Introduction
Traumatic injury contributes significantly to the burden of unequal health outcomes among minorities in the United States. Trauma is the leading cause of death among all Americans aged 1–44 years,1 and disparities in the risk of mortality after trauma among minority patients have been well documented.2,3 The root causes of unequal outcomes after trauma are complex and not well understood. There are myriad and overlapping factors, such as lack of health insurance, socioeconomic status, and violence, which may potentially contribute to the racial disparity in trauma mortality.2,4–6
There has been a significant effort to establish that racial disparities in mortality after trauma exist. While one study suggests that trauma accounts for 11 percent of the overall racial disparity in potential life years lost in the United States, there has not yet been an attempt to quantify the impact of this risk disparity on the number of deaths among black trauma patients in the United States.7
This study hypothesizes that disparities in the relative risk of mortality between black and white adult trauma patients will be apparent at Level I and Level II trauma centers in the United States and that the impact of these potential mortality disparities can be quantified in terms of “excess” mortality. If previous findings of racial disparities in trauma mortality disparities are confirmed, an analysis of the magnitude of excess mortality will provide policy-makers, providers, and researchers with an indication of how many lives might potentially be saved with the design and implementation of effective interventions targeting the trauma mortality disparity.
Methods
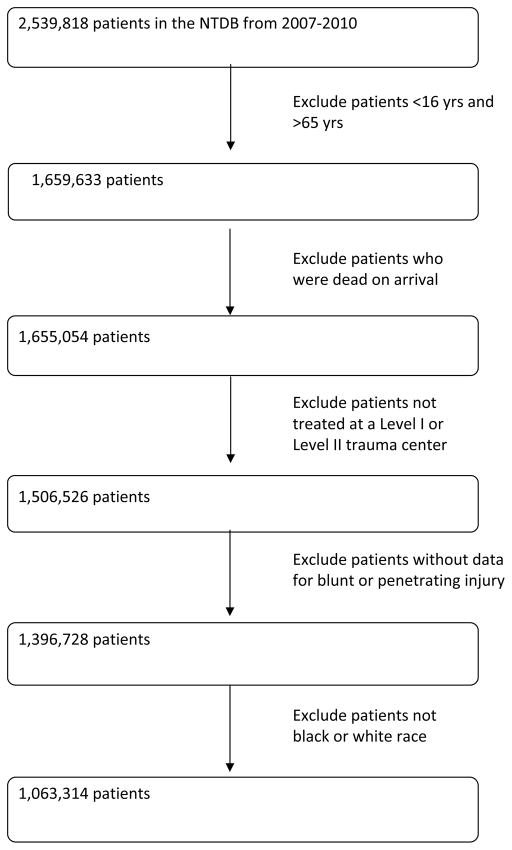
This study was a retrospective analysis of adult trauma patients aged 16–65 years included in the National Trauma Data Bank (NTDB) between 2007 and 2010. The NTDB is the largest repository of trauma registry data in the United States with approximately five million medical records from 900 participating centers. Data from the years 2007–2010 were chosen due to the NTDB’s adoption in 2007 of the National Trauma Data Standard (NTDS), which significantly improved the quality of data. Previous studies have shown that mortality disparities are most significant between black and white patients, thus this study was limited to black and white patients only.8 Patients who were dead on arrival or who were missing data on type of injury (blunt or penetrating) were excluded (Figure 1).
Figure 1.
Study Inclusion
Fiscella et al.’s previously published methodology to determine the number of black deaths attributable to the racial disparity in hypertension was adapted for this study of trauma patients.9 Specifically, this analysis incorporated Fiscella’s concept of modeling changes in mortality rates that would result from a reduction of the mean systolic blood pressure of black patients to that of white patients. In this study, the change in the number of deaths that would result from a reduction of the relative risk of death after trauma among black patients to that of white patients was determined.
Patients were stratified by trauma center level and by gender, allowing for a comparison of black vs. white patients within four groups: males treated at Level I trauma centers, females at Level I trauma centers, males at Level II trauma centers, and females at Level II trauma centers. Relative risk of in-hospital mortality for white patients, using black patients as the reference group, was calculated for each of the four patient strata using generalized linear modeling (GLM) with Poisson distributed dependent variable. GLM offers a way to unify basic linear, logit, and Poisson models and is advantageous in analyzing data that is not normally distributed due to the method’s increased flexibility for frequently encountered model violations. Multivariate logistic regression with clustering (to account for interfacility variation), which yields odds ratios, is often used for risk-adjusted analysis. However, to calculate the number of black deaths attributable to racial disparity in a manner consistent with Fiscella et al.’s previously described methodology, this study required the generation of relative risks of mortality for blacks versus white patients. Multiple patient demographic and injury severity variables were controlled for in the analysis, in accordance with previously recommended best practices for analyses using NTDB data.10 The following variables were included in the GLM models with mortality as the outcome: patient age, patient sex,11 anatomic severity [Injury Severity Score (ISS)], physiologic severity (hypotension at presentation),12 type of injury,13 Glasgow Coma Scale, ventilator use, injury intentionality, and insurance status.14
The relative risk of death among white trauma patients was multiplied by the number of black trauma deaths reported in the NTDB in each of the four patient strata to determine how many black trauma deaths would be expected if the risk of mortality had been equivalent to that of white patients. The overall number of “excess” black deaths was determined by subtracting the number of these expected deaths from the observed number of deaths.
Demographic data on patient, injury, and hospital characteristics were assessed for black and white patients separately. A bivariate analysis comparing patients who survived and patients who died according to race was also performed.
As the NTDB contains nearly all U.S. Level I trauma centers, these numbers are directly usable. Since the NTDB only contains 73% of all U.S. Level II trauma centers, the number of Level II patient deaths was multiplied by the constant 1.37 to obtain an estimate of actual deaths.
Given the higher proportion of penetrating trauma among black patients, a subset analysis was performed in blunt injury patients only. Statistical analyses were performed using Stata/MP statistical software version 11 (StataCorp, College Station, Texas). Statistical significance was set at p<0.05.
Results
Of the 2,539,818 patients included in the NTDB from 2007–2010, 1,063,314 patients who were treated at Level I or Level II trauma centers met inclusion criteria for this study (Figure 1). Of these, the majority of patients (77.1%) were white. Black patients were significantly more likely than white patients to be male, younger (16–35 years), and uninsured (Table 1). Intentional injuries were far more common among black trauma patients compared to white patients (43.0% vs. 10.8%), as well as penetrating injuries (35.1% vs. 7.7%). More specifically, black patients were significantly more likely than white patients to present with gunshot wounds (GSWs) (22.5% vs. 3.0%), stab wounds (12.5% vs. 4.7%), or “struck-by” injuries (12.6% vs. 8.3%). Unadjusted mortality was higher among black patients compared to white patients (4.7% vs. 3.2%), with an overall crude mortality rate of 3.5%.
Table 1.
Demographic Characteristics of Black and White Patients
| Black Patients n=243,286 (22.88) |
White Patients n=820,028 (77.12) |
p value | |
|---|---|---|---|
| Male | 186,118 (76.50) | 568,090 (69.28) | <0.001 |
| Female | 57,117 (23.48) | 251,158 (30.63) | |
| Age | |||
| 16–25 | 83,262 (34.22) | 207,983 (25.36) | <0.001 |
| 26–35 | 55,769 (22.92) | 141,773 (17.29) | |
| 36–45 | 43,426 (17.85) | 149,546 (18.24) | |
| 46–55 | 40,338 (16.58) | 178,302 (21.74) | |
| 56–65 | 20,491 (8.42) | 142,424 (17.37) | |
| Insurance Status | |||
| Insured | 127,820 (52.54) | 552,309 (67.35) | <0.001 |
| Uninsured | 76,152 (31.30) | 139,686 (17.03) | |
| Mechanism of Injury | |||
| Motor vehicle collision | 83,783 (34.44) | 364,600 (44.46) | <0.001 |
| Fall | 34,534 (14.19) | 219,528 (26.77) | |
| Struck-by | 30,599 (12.58) | 68,074 (8.30) | |
| Gunshot wound | 54,830 (22.54) | 24,549 (2.99) | |
| Stab wound | 30,485 (12.53) | 38,566 (4.70) | |
| Pedestrian | 2,294 (0.94) | 20,044 (2.44) | |
| Other | 6,761 (2.78) | 84,667 (10.32) | |
| Glasgow Coma Score | |||
| 3–5 | 16,246 (6.68) | 57,735 (7.04) | <0.001 |
| 6–8 | 3,697 (1.52) | 10,751 (1.31) | |
| 9–12 | 6,039 (2.48) | 16,021 (1.95) | |
| 13–15 | 206,222 (84.77) | 684,889 (83.52) | |
| Trauma Center | |||
| Level I | 179,150 (73.64) | 529,180 (64.53) | <0.001 |
| Level II | 64,136 (26.36) | 290,848 (35.47) | |
| Shock –SBP <90 mmHg | |||
| Yes | 13,119 (5.39) | 27,358 (3.34) | <0.001 |
| No | 224,346 (92.21) | 770,562 (93.97) | |
| Injury Severity | |||
| Mild (ISS 1–8) | 126,470 (51.98) | 366,354 (44.68) | <0.001 |
| Moderate (ISS 9–15) | 66,094 (27.17) | 249,260 (30.40) | |
| Severe (ISS 16–24) | 27,054 (11.12) | 118,630 (14.47) | |
| Extremely severe (ISS 25–75) | 21,412 (8.80) | 81,328 (9.92) | |
| Type of Injury | |||
| Blunt | 157,968 (64.93) | 756,891 (92.30) | <0.001 |
| Penetrating | 85,318 (35.07) | 63,137 (7.70) | |
| Intentional | |||
| Yes | 104,616 (43.00) | 88,313 (10.77) | <0.001 |
| No | 136,575 (56.14) | 729,674 (88.98) | |
| Year of Admission | |||
| 2007 | 49,555 (20.37) | 161,901 (19.74) | <0.001 |
| 2008 | 60,374 (24.82) | 205,944 (25.11) | |
| 2009 | 64,667 (26.58) | 217,426 (26.51) | |
| 2010 | 68,690 (28.23) | 234,757 (28.63) | |
| Mortality | 11,449 (4.71) | 26,108 (3.18) | <0.001 |
Gunshot wounds and motor vehicle crashes were the leading causes of death among both white and black patients, followed by falls in white patients and pedestrian injuries in black patients (Table 2). Gunshot wounds were responsible for 55% of the deaths among black trauma patients compared to only 17% of deaths among white patients. Black patients who died tended to be younger than white patients. Nearly forty percent (38.4%) of black trauma patients who died were aged 16–25 years compared to 22% of white patients who died. Although penetrating injuries and intentional injuries were more prevalent among black patients overall, similar proportions of black and white patients with these injury characteristics died (8.4% vs. 8.2%; 6.7% vs. 6.0%, respectively). Among those patients who died, injury severity appeared to be worse among black patients. Significantly more black patients who died arrived at the hospital emergency department in shock (<90mmHg), with a Glasgow Coma Score of 3–5, or with severe or extremely severe injuries (ISS 16–24 or 25–75) compared with white patients who died. Interestingly, although gunshot wounds were far more prevalent among black patients in this study, black patients were actually significantly more likely to survive GSW injuries than white patients (88.3% vs. 81.2%).
Table 2.
Overall Bivariate Analysis of Demographic Characteristics of Black and White Patients Who Survived and Patients Who Died
| Black Patients | White Patients | ||||
|---|---|---|---|---|---|
| Patients Who Survived n=228,760 (95.23) |
Patients Who Died n=11,449 (4.77) |
Patients Who Survived n=781,599 (96.77) |
Patients Who Died n=26,108 (3.23) |
p value | |
| Male | 173,915 (94.7) | 9,814 (5.3) | 540,182 (96.5) | 19,540 (3.5) | <0.001 |
| Female | 54,796 (97.1) | 1,633 (2.9) | 240,665 (97.4) | 6,541 (2.7) | |
| Trauma Level I | 167,716 (95.0) | 8,929 (5.1) | 502,923 (96.6) | 17,661 (3.4) | <0.001 |
| Trauma Level II | 61,044 (96.0) | 2,520 (4.0) | 278,676 (97.1) | 8,447 (2.9) | |
| Age | |||||
| 16–25 | 77,824 (94.7) | 4,392 (5.3) | 199,359 (97.2) | 5,762 (2.8) | <0.001 |
| 26–35 | 52,121 (94.7) | 2,943 (5.3) | 135,860 (97.2) | 3,963 (2.8) | |
| 36–45 | 41,164 (96.0) | 1,700 (4.0) | 142,874 (97.0) | 4,353 (3.0) | |
| 46–55 | 38,321 (96.2) | 1,499 (3.8) | 169,289 (96.5) | 6,193 (3.5) | |
| 56–65 | 19,330 (95.5) | 915 (4.5) | 134,217 (95.8) | 5,864 (4.2) | |
| Insured | |||||
| Yes | 121,965 (96.5) | 4,375 (3.5) | 529,988 (97.2) | 15,227 (2.8) | <0.001 |
| No | 69,963 (93.1) | 5,159 (6.9) | 131,546 (95.5) | 6,260 (4.5) | |
| Glasgow Coma | |||||
| 3–5 | 7,550 (47.2) | 8,440 (52.8) | 37,369 (65.8) | 19,429 (34.2) | <0.001 |
| 6–8 | 3,166 (87.0) | 472 (13.0) | 9,655 (90.8) | 973 (9.2) | |
| 9–12 | 5,509 (92.8) | 427 (7.2) | 15,035 (95.3) | 738 (4.7) | |
| 13–15 | 202,035 (99.2) | 1,681 (0.8) | 670,690 (99.4) | 3,865 (0.6) | |
| Shock | |||||
| Yes | 7,0709 (54.8) | 5,840 (45.2) | 18,074 (67.1) | 8,875 (32.9) | <0.001 |
| No | 216,919 (97.9) | 4,652 (2.1) | 743,188 (97.9) | 15,861 (2.1) | |
| ISS | |||||
| 1–8 | 123,975 (99.2) | 1,053 (0.8) | 359,184 (99.6) | 1,298 (0.4) | <0.001 |
| 9–15 | 64,006 (98.2) | 1,197 (1.8) | 243,374 (99.0) | 2,377 (1.0) | |
| 16–24 | 24,825 (93.0) | 1,863 (7.0) | 113,316 (96.9) | 3,664 (3.1) | |
| 25–75 | 13,903 (65.9) | 7,211 (34.2) | 61,757 (77.0) | 18,468 (23.0) | |
| Mechanism | |||||
| Stab | 29,386 (97.7) | 682 (2.3) | 37,300 (98.6) | 528 (1.4) | <0.001 |
| Fall | 33,336 (98.0) | 696 (2.1) | 210,775 (97.8) | 4,764 (2.2) | |
| GSW | 47,786 (88.3) | 6,364 (11.8) | 19,628 (81.2) | 4,545 (18.8) | |
| MVC | 79,618 (96.1) | 3,210 (3.9) | 346,143 (96.2) | 13,644 (3.8) | |
| Pedestrian | 2,180 (96.7) | 74 (3.3) | 19,505 (98.4) | 312 (1.6) | |
| Struck-by | 29,934 (99.1) | 268 (0.9) | 66,321 (98.8) | 792 (1.2) | |
| Other | 6,520 (97.7) | 155 (2.3) | 81,927 (98.2) | 1,523 (1.8) | |
| Intentional | 96,311 (93.3) | 6,921 (6.7) | 81,588 (94.0) | 5,243 (6.0) | <0.001 |
| Unintentional | 130,640 (96.8) | 4,269 (3.2) | 698,298 (97.1) | 20,572 (2.9) | |
| Year of Admission | |||||
| 2007 | 45,484 (94.8) | 2,492 (5.2) | 148,929 (96.4) | 5,624 (3.6) | <0.001 |
| 2008 | 56,211 (95.0) | 2,979 (5.0) | 195,062 (96.7) | 6,673 (3.3) | |
| 2009 | 61,546 (95.4) | 2,974 (4.6) | 210,238 (96.9) | 6,790 (3.1) | |
| 2010 | 65,519 (95.6) | 3,004 (4.4) | 227,370 (97.0) | 7,021 (3.0) | |
| Type of Injury | |||||
| Blunt | 151,585 (97.2) | 4,403 (2.8) | 724,649 (97.2) | 21,035 (2.8) | <0.001 |
| Penetrating | 77,175 (91.6) | 7,046 (8.4) | 56,950 (91.8) | 5,073 (8.2) | |
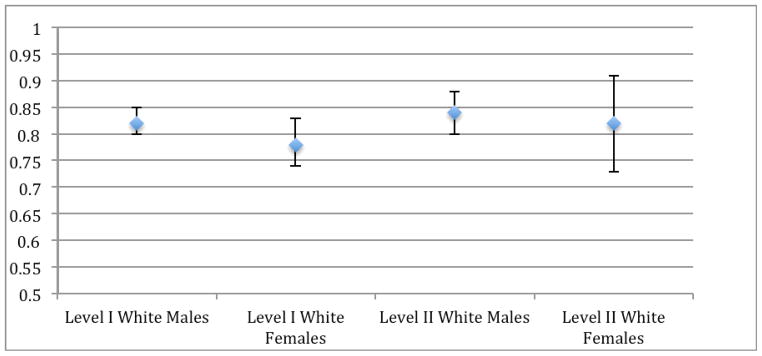
Of the more than one million patients included in this study, the adjusted relative risk of mortality was significantly lower for white compared to black patients (Figure 2). At Level I trauma centers white males and females had a relative risk of death of 0.82 (95% CI 0.80, 0.85) and 0.78 (95% CI 0.74, 0.83), respectively (Figure 2). There was no significant difference between Level I and Level II trauma centers in the disparity in relative risk of mortality. At Level II trauma centers white males and females had a relative risk of death of 0.84 (95% CI 0.80, 0.88) and 0.82 (95% CI 0.73, 0.91).
Figure 2.
Relative Risk of Mortality among White Adult Trauma Patients with Blunt and Penetrating Injuries
Reference group is black patients of equivalent stratum. All relative risks were significant. Level I white males: (RR 0.82, 95% CI 0.80, 0.85); Level I white females: (RR 0.78, 95% CI 0.74, 0.83); Level II white males (RR 0.84, 95% CI 0.80, 0.88); Level II white females (RR 0.82, 95% CI 0.73, 0.91).
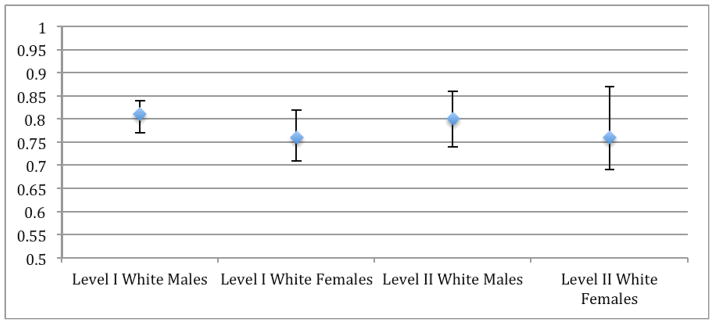
Given the confidence intervals of the relative risks of death shown in the analysis of patients with all injuries, it is unlikely that there would be a significant difference in results among blunt injury patients only. However, due to the high prevalence of penetrating injuries among black patients, a subset analysis was conducted in patients with blunt injury only (Figure 3). The racial disparity in relative risk of mortality did not diminish with the exclusion of penetrating trauma patients; there was no statistically significant difference in the risk of mortality between patients with only blunt trauma compared with all injury types at Level I trauma centers among white males [RR 0.81 (95% CI 0.77, 0.84) vs. RR 0.82 (95% CI 0.80, 0.85)] or among white females [RR 0.76 (95% CI 0.71, 0.82) vs. RR 0.78 (95% CI 0.74, 0.83)].
Figure 3.
Relative Risk of Mortality among White Adult Trauma Patients with Blunt Injury Only
Reference group is black patients of equivalent stratum. All relative risks were significant. Level I white males: (RR 0.81, 95% CI 0.77, 0.84), Level I white females (RR 0.76, 95% CI 0.71, 0.82), Level II white males (RR 0.80, 95% CI 0.74, 0.86), Level II white females (RR 0.76, 95% CI 0.69, 0.87).
Similarly, there was no significant difference in mortality risk between blunt injury only and all injury types at Level II trauma centers among white males (RR 0.80 (95% CI 0.74, 0.86) vs. RR 0.84 (95% CI 0.80, 0.88) or among white females RR 0.76 (95% CI 0.69, 0.87) vs. RR 0.82 (95% CI 0.73, 0.91).
Of the 8,927 deaths that occurred among black patients at Level I trauma centers, an estimated 1,633 (18.3%) may have survived in the absence of the race-based disparity in mortality outcomes (Table 3). While there were 2,520 actual deaths among black patients reported at Level II trauma centers, after accounting for the approximately 27% of Level II trauma centers not accounted for in NTDB data, it is estimated that 3,452 deaths occurred. Of these estimated 3,452 black patients who died at Level II trauma centers, 573 (16.6%) are estimated to have survived in the absence of the disparity in relative risk of mortality. Overall, of the estimated 41,613 deaths among black and white patients that occurred at both Level I and Level II trauma centers from 2007–2010, 2,206 deaths (5.3%) were among black patients who may have survived without a race-based disparity in the relative risk of mortality.
Table 3.
Excess Deaths Among Black Patients At Level I and Level II Trauma Centers
| Observed Deaths | Estimated Deaths (Actual Deaths Divided by 0.73)* | RR of Mortality for White Patients (95% CI) | Expected Deaths with No Racial Disparity | Excess Deaths (Observed-Expected) | |
|---|---|---|---|---|---|
| Level I Blacks | |||||
| Males | 7,664 | N/A | 0.82 (0.80,0.85) | 6,306 | 1,358 |
| Females | 1,263 | N/A | 0.78 (0.74, 0.83) | 989 | 275 |
| Total | 8,927 | N/A | -- | 7,295 | 1,633 |
| Level II* Blacks | |||||
| Males | 2,150 | 2,945 | 0.84 (0.80, 0.88) | 2,466 | 479 |
| Females | 370 | 507 | 0.82 (0.73, 0.91) | 413 | 94 |
| Total | 2,520 | 3,452 | -- | 2,669 | 573 |
| Overall Total | 9,964 | 2,206 |
Discussion
This study again confirms previously described racial disparities in the risk of mortality after trauma in both Level I and Level II trauma centers and goes beyond this prior work to estimate the number of patients who may have survived in the absence of this disparity. Approximately 2,200 deaths occurred among adult trauma patients at Level I and Level II trauma centers from 2007–2010 who may have survived had they had the same relative risk of mortality as white patients. Overall, these excess deaths represent approximately five percent of the deaths among trauma patients at Level I and Level II trauma centers.
Black patients were significantly more likely to suffer from penetrating injuries and intentional injuries. More than half of black patients who died suffered from a gunshot wound. It is clear that the disproportionate number of gunshot wounds – which have a high case fatality rate15 – contribute significantly to trauma mortality among black patients. Even among survivors of violence, penetrating injuries are associated with trauma recidivism, with each subsequent penetrating injury carrying more than twice the risk of mortality.16 To ensure that penetrating injuries were not a confounding driver of the differences in risk of mortality seen between black and white trauma patients, a subset analysis of blunt injury patients only was performed and showed that the disparity in risk of death persisted.
Few other studies have attempted to quantify “excess” deaths resulting from racial disparities,9,17–18 and to our knowledge, none have done so specifically for trauma. This analysis aims to quantify, rather than explain, the divergent risk of death among trauma patients by race. However, there are some possible mechanisms through which these disparities originate and are translated into a disproportionate number of deaths among black patients. For instance, black patients in this study were more likely to lack health insurance, a known risk factor for trauma mortality.6 Race is an independent predictor of trauma mortality even when controlling for insurance status.2 Furthermore, trauma patients are guaranteed emergent care regardless of ability to pay under the federal Emergency Treatment and Active Labor Act (EMTALA).2 However, black patients in the United States are disproportionately uninsured and may be in worse overall health at the time of their injury due to prior lack of access to care. Expanding health insurance coverage may improve the overall health status of the minority population, perhaps allowing them to better sustain an injury.
Deaths among black patients in this study were concentrated among young men suffering from gunshot wounds. The racial disparity in risk of mortality after trauma cannot be explained away by the prevalence of penetrating trauma among black patients; however, gunshot wounds are responsible for a staggering proportion of black trauma deaths (56%). Although this study controlled for potential confounding factors such as insurance status, it is possible that there was residual confounding that maybe have contributed to the disproportionately higher risk of mortality among black trauma patients. Given the ongoing epidemic of violence in American cities and the high case fatality rate of gunshot injuries, violence prevention initiatives are critically important to reduce the incidence of trauma among black patients.19 The Ceasefire Campaign in Chicago has successfully reduced gun violence through interventions designed to mediate disputes and challenge social acceptance of violence and is now being successfully replicated in other U.S. cities with programs such as Safe Streets in Baltimore.20,21 Mitigating the impact of violence, particularly in urban areas, provides an opportunity to reduce disparities by preventing violent trauma that disproportionately affects black patients.
It is unclear whether or not implicit racial bias among providers contributes to the increased risk of death among black trauma patients. Several studies have shown that implicit bias against black patients has a negative impact on the quality of care, as well as physician-patient communication and patient satisfaction with care in a primary care setting.22–24 However, a recent study found no association between implicit bias and vignette-based clinical decision-making among medical students.25 Further study is warranted to determine what, if any, role implicit bias plays in mediating the quality of care provided to minority trauma patients.
Improving quality at low performing, disproportionately minority trauma centers may also be a key intervention to reduce racial disparities. Low performing hospitals tend to serve more minority, uninsured, and low-income patients.26,27 Haider et al. found that trauma centers caring for between 25–50% minority patients or more than 50% minority patients have an increased adjusted odds of mortality of 1.16 (95% CI 1.01–1.34) and 1.37 (95% CI 1.16–1.61), respectively.4 Given the high proportion of uninsured patients seen at these disproportionately minority trauma centers, interventions to augment resource-poor hospitals to improve quality of care may reduce racial disparities in mortality.
To our knowledge, this is the first study to quantify the contribution of the racial mortality disparity to the number of deaths recorded among black trauma patients. Using a dataset of more than one million patients and following recommended best practices for robust analyses of NTDB data, this study reaffirms the wide gap in risk of death after trauma among black patients, even among those with blunt injuries only. However, there are several important limitations to consider in this study. First, co-morbidities have not been controlled for due to the prevalence of missing data in the NTDB. To address this concern the analysis was restricted to patients under age 65 years, as co-morbidities in older patients are more prevalent. However, it is unknown if there are racial disparities in patients over age 65 years, as most outcomes studies have excluded this population and disparities appear to lessen after age 65.28 Second, our estimates for Level II trauma centers have been extrapolated from the 73% of centers reporting to the NTDB and thus are not directly usable. It is possible that the Level II trauma centers not included in the NTDB may have differed from those centers reporting to the NTDB. However, the mortality estimates for Level II centers were proportionally similar to Level I centers. Furthermore, the NTDB is not a nationally representative sample and this study does not include data on trauma patients not treated at a Level I or Level II trauma center. Finally, while patient and hospital characteristics were controlled for in the analysis, there may have been some residual confounding due to a lack of important clinical information.
Creating interventions designed to identify and target the root causes of the racial mortality disparity could have a significant impact on overall trauma survival. Nearly one in five black trauma patients who died from 2007–2010 in this study may have survived had they experienced the same risk of mortality as white patients. Overall, these excess deaths represent approximately five percent of the deaths among trauma patients at Level I and Level II trauma centers. While the underlying drivers of this disparity remain unclear, the magnitude of the impact on mortality demands that policy-makers, providers, and researchers renew their efforts to better understand and intervene to mitigate racial disparities in trauma.
Acknowledgments
Financial support for this work was provided by: National Institutes of Health/ NIGMS K23GM093112-01; American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care (Dr. Haider).
References
- 1.Centers for Disease Control and Prevention. Office of Statistics and Programming, National Center for Injury Prevention and Control. 10 leading causes of death by age group. United States: 2010. [Accessed April 15, 2013]. http://www.cdc.gov/injury/wisqars/pdf/10LCID_All_Deaths_By_Age_Group_2010-a.pdf. Updated Oct 15, 2012. [Google Scholar]
- 2.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., 3rd Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 3.Crompton JG, Pollack KM, Oyetunji T, et al. Racial disparities in motorcycle-related mortality: An analysis of the National Trauma Data Bank. Am J Surg. 2010;200(2):191–196. doi: 10.1016/j.amjsurg.2009.07.047. [DOI] [PubMed] [Google Scholar]
- 4.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: A nationwide analysis of 434 hospitals. Arch Surg. 2012;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haider AH, Bentley JM, Monn MF, et al. Disparities in trauma care and outcomes in the United States: A systematic review and meta-analysis. J Trauma Acute Care Surg. 2012 doi: 10.1097/TA.0b013e31828c331d. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosen H, Saleh F, Lipsitz S, Rogers SO, Gawande AA. Downwardly mobile: The accidental cost of being uninsured. Arch Surg. 2009;144(11):1006–1011. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 7.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. NEJM. 2002;347(20):1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 8.Haider AH, Rehman KA, Velopulos CG, Bentley JM, Cornwell EE, 3rd, Al-Refaie W. Racial disparities in surgical care and outcomes in the United States: A comprehensive review of patient, provider and systemic factors. J Amer Coll Surg. 2012 doi: 10.1016/j.jamcollsurg.2012.11.014. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiscella HK. Racial disparity in hypertension control: Tallying the death toll. Ann Fam Med. 2008;6(6):497–502. doi: 10.1370/afm.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214(5):756–68. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haider AH, Crompton JG, Oyetunji T, et al. Females have fewer complications and lower mortality following trauma than similarly injured males: A risk adjusted analysis of adults in the National Trauma Data Bank. Surgery. 2009;146(2):308–315. doi: 10.1016/j.surg.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Oyetunji T, Crompton JG, Efron DT, et al. Simplifying physiologic injury severity measurement for predicting trauma outcomes. J Surg Res. 2010;159(2):627–632. doi: 10.1016/j.jss.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 13.Maybury RS, Bolorunduro OB, Villegas C, et al. Pedestrians struck by motor vehicles further worsen race- and insurance-based disparities in trauma outcomes: The case for inner-city pedestrian injury prevention programs. Surgery Aug. 2010;148(2):202–208. doi: 10.1016/j.surg.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am J Surg. 2010;199(4):554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Haider AH, Crompton JG, Oyetunji T, et al. Mechanism of injury predicts case fatality and functional outcomes in pediatric trauma patients: The case for its use in trauma outcomes studies. J Pediatr Surg. 2011;46(8):1557–1563. doi: 10.1016/j.jpedsurg.2011.04.055. [DOI] [PubMed] [Google Scholar]
- 16.Brooke BS, Efron DT, Chang DC, Haut ER, Cornwell EE., 3rd Patterns and outcomes among penetrating trauma recidivists: It only gets worse. J Trauma. 2006;61(1):16–19. doi: 10.1097/01.ta.0000224143.15498.bb. [DOI] [PubMed] [Google Scholar]
- 17.LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv. 2011;41(2):231–238. doi: 10.2190/HS.41.2.c. [DOI] [PubMed] [Google Scholar]
- 18.Fiscella K, Dressler R, Meldrum S, Holt K. Impact of influenza vaccination disparities on elderly mortality in the United States. Prev Med. 2007;45(1):83–87. doi: 10.1016/j.ypmed.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Efron DT, Haider A, Chang D, Haut ER, Brooke B, Cornwell EE., 3rd Alarming surge in nonsurvivable urban trauma and the case for violence prevention. Arch Surg. 2006;141(8):800–805. doi: 10.1001/archsurg.141.8.800. [DOI] [PubMed] [Google Scholar]
- 20. [Accessed Dec 5, 2012];Ceasefire-The Campaign to Stop the Shooting Web site. http://ceasefirechicago.org/
- 21.Webster DW, Whitehill JM, Vernick JS, Curriero FC. Effects of Baltimore’s Safe Streets Program on gun violence: A replication of Chicago’s CeaseFire Program. J Urban Health. 2012;90(1):27–40. doi: 10.1007/s11524-012-9731-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J of Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J of Public Health. 2012;102(5):988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306(9):942–951. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: Examination of the hospital quality alliance measures. Arch Intern Med. 2007;167(12):1233–1239. doi: 10.1001/archinte.167.12.1233. [DOI] [PubMed] [Google Scholar]
- 27.Baicker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspect Biol Med. 2005;48(1 Suppl):S42–53. [PubMed] [Google Scholar]
- 28.Singer MB, Liou DZ, Clond MA, et al. Insurance-and race-related disparities decrease in elderly trauma patients. J Trauma Acute Care Surg. 2013;74(1):312–316. doi: 10.1097/TA.0b013e31826fc899. [DOI] [PubMed] [Google Scholar]