Abstract
BACKGROUND
Several studies have described the burden of trauma care but few have explored the economic burden of trauma inpatient costs from a payer’s perspective or highlighted differences in average costs per person by payer status. This study gives a conservative inpatient National trauma cost estimate, and describes variation in average inpatient trauma cost by payer status.
METHODS
A retrospective analysis of patients who received trauma care at hospitals in the Nationwide Inpatient Sample (NIS) for the years 2005–2010 was conducted. Our sample patients were selected using appropriate ICD-9-CM codes to identify admissions due to traumatic injury. Data were weighted to provide national population estimates and all cost and charges were converted to 2010 US Dollar equivalents. Generalized linear models were used to describe costs by payer status, adjusting for patient characteristics, such as age, sex, race, and hospital characteristics, such as location, teaching status and patient case mix.
RESULTS
A total of 2,542,551 patients were eligible for study, with payer status as follows: 672,960 (26.47%) patients with private insurance, 1,244,817 (48.96%) patients with Medicare, 262,256 (10.31%) with Medicaid, 195,056 (7.67%) of patients with self-pay, 18,506 (0.73%) with no charge, and 150,956 (5.94%) on other types of insurance. The estimated yearly trauma inpatient cost burden was highest for Medicare at $17,551,393,082(46.79%), followed by private insurance $10,772,025,421 (28.72%), Medicaid $3,711,686,012 (9.89%), self-pay $2,831,438,460 (7.55%), other payer types $2,370,187,494 (6.32%), and $274,598,190 (0.73%) for patients who were not charged for their inpatient trauma treatment. Our adjusted national inpatient trauma yearly costs were estimated at $37,511,328,659 US dollars. Privately insured patients had significantly higher mean cost than per person than Medicare, Medicaid, self-pay, or no charge patients.
CONCLUSION
This study demonstrates that the distribution of trauma burden across payers is significantly different from that of the overall healthcare system, and suggests that while the burden of trauma is high, the burden of self-pay/non-reimbursed inpatient services is actually lower than that of overall medical care.
Level of Evidence: Prognostic study with Level II evidence
Keywords: Cost of Trauma Care, Cost Shifting by Payer, National trauma cost
INTRODUCTION
Each year traumatic injuries cost an estimated 300 million years of healthy life, translating to 11% of disability adjusted life years (DALY’s) worldwide.1,2,3 An estimated 37 million trauma emergency visits occur yearly, 2.6 million resulting in hospital admission, and traumatic disorders rank among the five most costly medical conditions.4,5 The lifetime costs of traumatic injuries have been estimated at $406 billion dollars, with $80 billion representing health system costs, and the balance representing lost productivity.6 It has widely been assumed that a large proportion of patients are uninsured, representing lost reimbursement to hospitals; however, the exact distribution of the cost burden to payers is largely unknown. As the US healthcare system faces mounting challenges in curbing costs, with current estimates at 18% of the Gross Domestic Product, disease-specific cost studies are important to guide policy debates, inform health care consumer decisions, and determine the appropriate level of investment needed for injury prevention activities.7,8,9 Prior studies have been subject to limitations as a result of assumptions in data source, exclusion of pediatric trauma patients and an extrapolation of a limited dataset to heterogeneous populations.6,7,8 One barrier to cost analysis is regional variation in cost of treatment estimates.10,11 Consequently, the objective of this study was to use a nationally representative administrative discharge database to quantify the proportion of trauma inpatient care that is borne by different payers, and to estimate the average yearly cost of inpatient care.
METHODS
Data source
The Nationwide Inpatient Sample (NIS) database is a part of the Healthcare Cost and Utilization Project (HCUP), which is sponsored by the Agency for Healthcare Research and Quality. NIS is the largest all-payer inpatient care database that is publicly available in the United States. The data are a 20-percent stratified sample of discharges from US community hospitals, comprising 95% of the US population, and this includes comprehensive abstracted discharge data. The data is then weighted back to make population estimates of various parameters.12 For the present study additional NIS subfiles were merged to the core file, using unique hospital identifiers, to obtain information on cost and hospital characteristics. These sub-files include the hospital weights files and the cost-to-charge ratio files.13 Data from NIS 2005–2010 were queried.
Study population
From a population of 47,882,872 patients in the NIS 2005–2010 sample, using International Classification of Disease Clinical (ICD-9-CM) diagnosis codes we identified 2,542,551 patients with ICD-9CM primary or secondary diagnoses of trauma (800–959). Patients’ records with missing information on cost and other variables of interest were excluded from the study.
Definitions
The primary outcome variable was cost. Other information retrieved included patient demographics, trauma diagnosis (using ICD-9-CM codes), hospital characteristics, total charges, hospital-specific all-payer cost-to-charge ratio (CCR), area wage index, length of stay, comorbidity as measured by Charlson Index, and mortality.
Data on patient demographics retrieved included age, race, gender, median household income quartile for patient’s residential zip code, and primary insurance payer. Hospital characteristics information included bed size, teaching status, private/government ownership, rural/urban location, as well as the region and state where the hospital is located. For the period of data used in the present study, six states (Delaware, North Dakota, Idaho, Mississippi, Alabama, and Alaska) and the District of Columbia did not participate in the NIS.
The individual cost of hospitalization was calculated by multiplying total charge with the hospital-specific CCR. Hospital-specific CCRs are developed using standardized hospital information on all-payer inpatient cost and charge reported by hospitals to the Center for Medicare and Medicaid Services (CMS). Using appropriate Consumer Price Indices, costs in prior years (2005–2009) were then adjusted for inflation and converted to 2010 dollars. The area wage index is computed by the CMS to measure the relative hospital wage level in a geographic area compared to the national average, and was used to control for the influence of local markets on prices. Charlson Index is a measure of comorbidity and risk of mortality, and is derived using a weighted formula, and based on the presence/absence of certain diagnoses in a patient.14,15,16,17
STATISTICAL ANALYSIS
The data were weighted and set to signify survey data. This was necessary to account for the NIS sampling method. We then estimated the weighted unadjusted mean per person cost of trauma inpatient admissions by payer status. Controlling for patient demographic variables and hospital characteristics, which are known to influence mean per person cost, we again assessed the weighted mean per person cost by payer status. Our reference payer variables were private insurance, white race, age <5years, lowest Charlson index, and lowest ISS. Reference variables for hospital characteristics were small bed size, rural location, and private or non-teaching hospitals. Using discharge weights, a generalized linear model was then used to fit our model and the predicted adjusted mean per-person trauma inpatient cost by payer status. Population estimates were used to generate the mean trauma inpatient cost per payer and summed to compute the national trauma cost.
We additionally performed a sensitivity analysis excluding secondary diagnoses of trauma, evaluating only those patients who were admitted with a primary diagnosis of trauma. This was compared to overall cost and mean cost per patient. All statistical analysis was done using STATA/MP Version 11.0 (StataCorp, College Station, Texas USA). Statistical significance was defined as p < 0.05.
RESULTS
The study sample included 2.5 million patients, with nearly half covered by Medicare (48.96%), 26.47% by private insurance, and the balance covered by Medicaid, self-pay, and other payers such as Workers’ Compensation, CHAMPUS, CHAMPV, TITLE V, and other government programs. Demographic data is included in Table 1. Medicare patients had a mean age of 76.98, while patients on Medicaid were the youngest (mean 33.32). The majority of privately insured patients were white (59.86%), followed by unspecified/other races (28.24%), black (6.40%) and Hispanic (5.50%). Patients of white race comprised the greatest number of patients on Medicaid (39.66%), followed by patients with unspecified/other race (29.05%), blacks, (16.58%) and Hispanics (14.71%). Mean length of stay was highest for Medicare and Medicaid patients and lowest for self-pay and private insurance patients, and most had an Injury Severity Score of less than 9. The payers that had the highest proportion of penetrating trauma were self pay and no charge, although overall penetrating trauma comprised less than 4% of the sample. Distribution of each payer type across hospitals by bed size was similar, with large hospitals serving 65.36% of patients, small hospitals serving 10.99%, and the balance being served by medium-sized hospitals. Within each strata by payer status, the proportion of each type of payer was similar. Slightly more Medicare patients were seen at small hospitals, and slightly more self-pay patients were seen at large hospitals, but this was not statisticially significant. As seen in Table 2, adjusted mean per-person cost of trauma injury was significantly lower for Medicare patients compared to privately insured patients. Mean per-person cost of trauma injury was also significantly lower for Medicaid and self-pay patients when compared to patients with private insurance. The adjusted estimated yearly trauma inpatient cost burden was highest for Medicare at $17,551,393,082(46.79%), followed by private insurance $10,772,025,421 (28.72%), Medicaid $3,711,686,012 (9.89%), self-pay $2,831,438,460 (7.55%), other payer types $2,370,187,494 (6.32%), and $274,598,190 (0.73%) for patients who were not charged for their inpatient trauma treatment. These costs were adjusted for patient’s age, sex, race, median income, length of stay, ISS, and number of co-morbidities, and converted to 2010 dollars. Annual national inpatient trauma costs were estimated at $30,741,846,525.
Table 1.
Patient Characteristics by Payer Status
| Total N=2,542,551 |
Private 672,960 |
Medicare 1,244,817 |
Medicaid 262,256 |
Self Pay 195,056 |
No Charge 18,506 |
Other* 150,956 |
|---|---|---|---|---|---|---|
| Age mean (SD) | 44.51 (21.70) | 76.98 (13.19) | 33.32 (21.06) | 37.58 (15.69) | 38.93 (15.20) | 42.96 (18.27) |
| Gender % | ||||||
| Female | 43.43 | 63.10 | 42.76 | 26.01 | 24.88 | 26.63 |
| Male | 56.57 | 36.90 | 57.24 | 73.99 | 75.12 | 73.37 |
| Race % | ||||||
| White | 59.86 | 67.69 | 39.66 | 44.30 | 50.91 | 50.40 |
| Black | 6.40 | 4.56 | 16.58 | 14.23 | 17.17 | 9.07 |
| Hispanic | 5.50 | 3.73 | 14.71 | 13.76 | 20.11 | 12.50 |
| Others | 28.24 | 24.02 | 29.05 | 27.71 | 11.81 | 28.03 |
| LOS** mean (SD) | 5.10 (7.72) | 6.12 (6.70) | 6.88 (13.26) | 4.68 (7.71) | 5.39 (9.50) | 5.29 (8.45) |
| Status % | ||||||
| Alive | 98.19 | 96.62 | 98.27 | 97.89 | 98.54 | 98.36 |
| Dead | 1.81 | 3.38 | 1.73 | 2.11 | 1.46 | 1.64 |
| Location % | ||||||
| Rural | 9.13 | 15.24 | 9.38 | 9.31 | 3.30 | 9.77 |
| Urban | 90.87 | 84.76 | 90.62 | 90.69 | 96.70 | 90.23 |
| Bed Size % | ||||||
| Small | 9.47 | 13.05 | 9.46 | 7.54 | 4.97 | 8.60 |
| Medium | 23.55 | 24.15 | 23.83 | 22.99 | 21.85 | 20.65 |
| Large | 66.98 | 62.08 | 66.71 | 69.47 | 73.18 | 70.75 |
| Mechanism % | ||||||
| Penetrating | 6.19 | 1.33 | 16.42 | 19.90 | 23.63 | 12.42 |
| Blunt | 93.81 | 98.67 | 83.58 | 80.10 | 76.37 | 87.58 |
| Injury Severity Score (%) | ||||||
| 1–9 | 75.86 | 87.15 | 79.56 | 71.43 | 74.70 | 73.69 |
| 10–15 | 8.82 | 5.54 | 6.01 | 10.80 | 9.77 | 9.54 |
| 16–24 | 9.37 | 5.39 | 6.94 | 10.48 | 9.28 | 9.40 |
| ≥25 | 5.95 | 1.92 | 7.49 | 7.29 | 6.25 | 7.37 |
Others include Workers’ Compensation, CHAMPUS, CHAMPV, TITLE V, other government programs
LOS = length of stay
Table 2.
Mean per person cost of injury per year by payer type
| Unadjusted:
| ||||
|---|---|---|---|---|
| PAYER | Mean Cost | 95% Confidence Interval | Weighted Population Estimate | Mean Cost per Year (USD 2010)* |
| Private | $13,314 | ($13,264, $13,364) | 4,083,605 | $9,061,675,607.00 |
| Medicare | $12,036 | ($12,010, $12,062) | 7,559,401 | $15,164,587,669.00 |
| Medicaid | $14,224 | ($14,317, $14,527) | 1,592,638 | $3,828,187,503.00 |
| Self Pay | $11,854 | ($11,770, $11,937) | 1,164,718 | $2,301,041,181.00 |
| No Charge | $12,876 | ($12,559, $13,194) | 112,359 | $241,126,670.00 |
| Others | $13,782 | ($13,672, $13,892) | 904,868 | $2,078,471,576.00 |
| Unadjusted Total Yearly National Trauma Inpatient Cost: $32,675,090,206.00 | ||||
|
Adjusted**:
| ||||
| Private | $15,827 | ($15,345, $16,309) | 4,083,605 | $10,772,025,421.00 |
| Medicare | $13,931 | ($13,396, $14,465) | 7,559,401 | $17,551,393,082.00 |
| Medicaid | $13,983 | ($13,423, $14,543) | 1,592,638 | $3,711,686,012.00 |
| Self Pay | $14,586 | ($14,038, $15,134) | 1,164,718 | $2,831,438,460.00 |
| No Charge | $14,664 | ($13,982, $15,345) | 112,359 | $274,598,190.00 |
| Others | $15,716 | ($15,153, $16,279) | 904,868 | $2,370,187,494.00 |
| Adjusted Total Yearly National Trauma Inpatient Cost: $37,511,328,659.00 | ||||
All costs in 2010 dollars
Adjusted for patient’s age, sex, race, median income in residential zip code, length of stay, ISS, co-morbidity.
When examining blunt and penetrating mechanisms separately, similar differences were noted for patients with blunt injury, with higher mean per-person cost for privately insured and other insured versus Medicare or Medicaid patients. For patients with penetrating injury, however, cost was not different across payer type, as shown in Table 3.
Table 3.
Adjusted** mean per person cost of injury per year by payer type and mechanism
| Penetrating:
| ||
|---|---|---|
| PAYER | Mean Cost | 95% Confidence Interval |
| Private | $7642 | ($4433, $10851) |
| Medicare | $5503 | ($1929, $10128) |
| Medicaid | $7349 | ($3849, $10849) |
| Self Pay | $7544 | ($4126, $10963) |
| No Charge | $8852 | ($5001, $12703) |
| Others | $8568 | ($5084, $12052) |
|
Blunt:
| ||
| Private | $15,040 | ($14492,$15589) |
| Medicare | $13,491 | ($12883,$14099) |
| Medicaid | $13,769 | ($13117,$14421) |
| Self Pay | $14,064 | ($13435,$14693) |
| No Charge | $14,217 | ($13423,$15011) |
| Others | $15,228 | ($14584,$15872) |
All costs in 2010 dollars
Adjusted for patient’s age, sex, race, length of stay, living status, hospital location, hospital bedsize, ISS.
Sensitivity analysis excluding patients with secondary diagnoses of trauma and including only those who were admitted with a primary diagnosis of trauma yielded 1,559,786 patients, with no significant difference in distribution across payer status. Additionally, there was no change in mean cost by group, as seen in Table 4.
Table 4.
Sensitivity analysis of mean per person cost of injury per year by payer type using only primary diagnosis code for trauma.
| Unadjusted:
| ||||
|---|---|---|---|---|
| PAYER | Mean Cost | 95% Confidence Interval | Weighted Population Estimate | Mean Cost per Year (USD 2010)* |
| Private | $13,714 | ($13,651, $13,777) | 2,250,028 | $5,142,813,999.00 |
| Medicare | $11,980 | ($11,948, $12,013) | 3,476,550 | $6,941,511,500.00 |
| Medicaid | $15,835 | ($15,679, $15,991) | 700,185 | $1,847,904,913.00 |
| Self Pay | $12,855 | ($12,752, $12,958) | 688,914 | $1,475,998,245.00 |
| No Charge | $14,201 | ($13,792, $14,610) | 63,218 | $149,626,470.00 |
| Others | $14,460 | ($14,324, $14,596) | 528,809 | $1,274,429,690.00 |
| Unadjusted Total Yearly National Trauma Inpatient Cost: $16,832,284,816.00 | ||||
|
Adjusted**:
| ||||
| Private | $15,939 | ($15,330, $16,548) | 2,250,028 | $5,977,200,072.00 |
| Medicare | $14,177 | ($13,508, $14,846) | 3,476,550 | $8,214,411,368.00 |
| Medicaid | $14,578 | ($13,865, $15,292) | 700,185 | $1,701,256,980.00 |
| Self Pay | $14,821 | ($14,138, $15,505) | 688,914 | $1,701,785,197.00 |
| No Charge | $15,015 | ($14,168, $15,863) | 63,218 | $158,208,039.00 |
| Others | $15,876 | ($15,176, $16,577) | 528,809 | $1,399,242,256.00 |
| Adjusted Total Yearly National Trauma Inpatient Cost: $19,152,103,912.00 | ||||
All costs in 2010 dollars
Adjusted for patient’s age, sex, race, length of stay, living status, hospital location, hospital bedsize, ISS, co-morbidity.
DISCUSSION
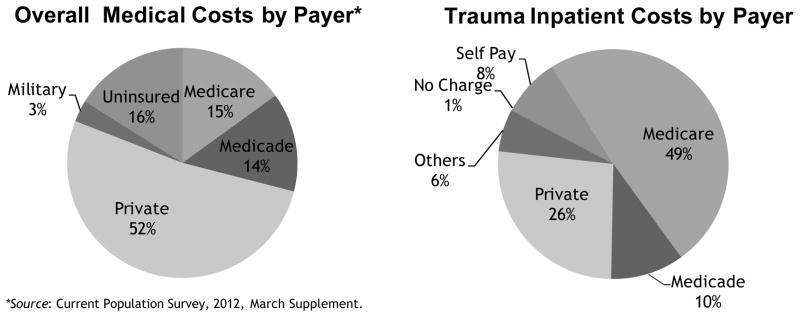
This study demonstrates that the distribution of trauma burden across payers is significantly different from that of the overall healthcare system, although not in the direction that we have previously expected (Figure 1). Whereas costs to Medicare comprise only about 15% of total payments across all types of healthcare in comparison to private insurers at 52%, the major payer in trauma care is actually Medicare at 49%, with private following at 27%. Of particular interest is the self-pay and no charge proportion, which represents uninsured patients. While they comprise 16% of overall healthcare costs, and are often thought to be greater in number in the trauma population, our study demonstrates that they represent only 9% of inpatient trauma costs.
Figure 1.
Distribution of payers for overall medical costs compared to inpatient trauma costs, showing that burden of uninsured patients is less in trauma, while trauma bears an increased share of Medicare cost.
We also find that mean cost estimates, both crude and adjusted for age, sex, race, income, LOS, ISS and comorbidities, are higher in private and other types of insurance compared to Medicare, Medicaid, self-pay, and no charge patients When stratified by mechanism, this difference disappeared for penetrating trauma patients. The reason for this is not clear and represents an area for further study. Because these estimates are based on charges adjusted by CCR rather than hospital revenue, difference in reimbursement rate by payer cannot explain this cost differential.
This study suggests that while the burden of trauma is high, the burden of self-pay/non-reimbursed inpatient services is actually lower than that of overall medical care. This has important implications for policy at the local, regional, and national level, particularly in discussions of the funding of Medicare and Medicaid, the perceived burden of uninsured patients, and funding of trauma research and prevention programs. Because there are regional differences in payer mix, algorithms should be developed to adjust reimbursement and funding for hospitals that bear a disproportionate burden of non-reimbursable trauma services.
Another area that merits further review is quality of care in regard to cost. Some studies suggest that outcomes are better for privately insured patients, who have higher per-person costs, while other studies such as the RAND Health Insurance Experiment show little difference in quality regardless of payment paradigm. Cost sharing and cost shifting have not yet been shown to make a definitive difference.19,20 There is also concern that decreasing reimbursements will lead to fewer physicians providing charity care, thus further reducing the quality of this type of care.21,22
Using a nationally representative cross sectional dataset, this study estimates the trauma cost burden by payer status and also provides an estimate for the national trauma inpatient yearly costs. Our finding of a National Trauma cost estimates of $37 billion is close to the $27 billion estimate by Weir S et al., accounting for inflation.7 Finkinstel et al8, utilizing the Medical Expenditure Panel Survey (MEPS) and HCUP-NIS Cost to Charge Ratio files, similarly estimated trauma inpatient costs at $33.7 billion. In our study, Medicare bore the highest cost burden, followed by Private insurance, Medicaid, other insurance types, self-pay patients and patients with no charges respectively. Of note, the analysis controlled for differences in comorbidities and other potential differences among the groups. Hospitals contemplating the addition of trauma services should be reassured that the burden of non-compensated care is likely much lower than previously expected, although there is certainly regional variation.
Use of the NIS database does have some limitations. Coding errors that lead to misdiagnosis are possible, as well as potential overcoding that would inflate the costs. To verify that relevant trauma diagnoses are not excluded due to inappropriate ordering within the database, we included secondary diagnosis codes as well. Although trauma patients are occasionally admitted for other reasons, we are not able to directly determine this from the data, and because cost data are not itemized for diagnosis or procedure, we are not able to assure that all costs are attributable to trauma diagnoses alone. Of note, however, the Medicare group, which is an older cohort with more comorbidities, did not incur greater inpatient costs over the younger groups, as might have been expected if non-trauma diagnoses were heavily implicated. Importantly, sensitivity analysis including only those patients with a primary diagnosis of trauma did not change the mean cost as might have been expected when all diagnoses are included.
As an additional limitation, there are certainly unmeasured confounders as only a set number of variables are collected, and we are unable in a retrospective database review to establish any causal relationships. We also do not have data on additional cost that might be associated with outpatient needs after discharge, such as rehabilitation or wound care, nor can we account for regional variation with this dataset.
Future study should be developed to further gauge the impact of indirect costs and societal burden of traumatic injury, including rehabilitation, follow-up, and extended care needs affected by personal resources such as income, transportation, child care, and loss of productivity, as well as to explore potential mechanisms for disparities.
The anticipated aging of the US population has the potential to place a huge demand for trauma care in the elderly, which in turn will place a significant cost burden on the health system, particularly Medicare.23 Injury prevention activities and treatment modalities targeted at this patient population will go a long way, not only in the improvement of quality of life, and reduction of mortality, but also in significant cost savings for the US health system.
Footnotes
Author Contributions.
All authors contributed to the study conception and design. Drs. Enwerem, Schneider, Velopulos, Hui and Haider contributed to the acquisition of data. Analysis and interpretation of data was completed by Drs. Enwerem, Velopulos, Obirieze, Hui, Hashmi, Schneider, Cornwell and Haider. The manuscript was drafted by Dr. Enwerem, Dr. Velopulos, Dr Obirieze, Dr. Haider and Ms Scott. Critical revision of the manuscript was undertaken by Drs. Velopulos, Schneider, Cornwell, Hui and Haider.
References
- 1.Murray CJ, Vos T, Lozano R, et al. Disability adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013 Dec 15;380(9859):2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.WISQARS Leading Causes of Death Reports, 1999–2007. Office of Statistics and Programming, National Center for Injury Prevention and Control, Center for Disease Control and Prevention; [Accessed 1/3/13.]. http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html. [Google Scholar]
- 3.Shakur H, Robert I, et al. A promise to save 100,000 trauma patients. Lancet. 2013 Dec 15;380(9859):2062–2063. doi: 10.1016/S0140-6736(12)62037-6. [DOI] [PubMed] [Google Scholar]
- 4.The case for Funding Trauma Research. A Report from the National Trauma Institute. [Accessed 1/3/13.]; http://www.nationaltraumainstitue.org/pdf/case_trauma_funding.pdf.
- 5.Soni A. The Five Most Costly Conditions, 2000 and 2004: Estimates for the US Civilian Noninstitutionalized Population. Statistical Brief #167. Agency for Healthcare Research and Quality; Rockville, Md: Mar, 2007. [Accessed 1/3/13]. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st167/stat167.shtml. [Google Scholar]
- 6.Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006 Aug;12(4):212–8. doi: 10.1136/ip.2005.010983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weir S, Salkever DS, Rivara FP, et al. One-year treatment costs of trauma care in the USA. Expert Rev Pharmacoecon Outcomes Res. 2010 Apr;10(2):187–97. doi: 10.1586/erp.10.8. [DOI] [PubMed] [Google Scholar]
- 8.Finkelstein EA, Corso PS, Miller TR. The incidence and Economic Burden of Injuries in the United States. Oxford University Press; NY USA: 2006. [Google Scholar]
- 9.World Health Statistics 2009. World Health Organization; May, 2009. [Accessed 1/3/13.]. Available at http://www.who.int/whosis/whostat/EN_WHS09_Full.pdf. [Google Scholar]
- 10.Obirieze CA, Gaskin DJ, Villegas CV, et al. Regional variations in cost of trauma care in the United States: who is paying more. J Trauma Acute Care Surg. 2012 Aug;73(2):516–522. doi: 10.1097/ta.0b013e31825132a0. [DOI] [PubMed] [Google Scholar]
- 11.The dartmouth atlas of health care 1998. Darmouth: The Center for the Evaluative Clinical Sciences, Dartmouth Medical School; 1998. [Accessed 1/3/13.]. http://www.dartmouthatlas.org/publications/reports.aspx. [Google Scholar]
- 12.HCUP Nationwide Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP) 2008. Agency for Healthcare Research and Quality; Rockville, MD: [Accessed 1/3/13.]. http://www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- 13.HCUP Cost-to-Charge Ratio Files (CCR) Healthcare Cost and Utilization Project (HCUP) 2006–2009. Agency for Healthcare Research and Quality; Rockville, MD: [Accessed 1/3/13.]. http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD–9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 16.Quan H, Parsons GA, Ghali WA. Validity of information on comorbidity derived from ICD-9-CCM administrative data. Med Care. 2002 Aug;40(8):675–85. doi: 10.1097/00005650-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 18.Department of Health and Human Services. [Accessed 1/3/13.];Administration on Aging data file. 2009 http://www.aoa.gov/aoaroot/aging_statistics/index.aspx.
- 19.Gisburg PB. Can Hospitals and Physicians Shift the Effects of Cuts in Medicare Reimbursement to Private Payers? Health Aff (Millwood) 2003 Jul-Dec;(Suppl Web Exclusives):W3-472-9. doi: 10.1377/hlthaff.w3.472. [DOI] [PubMed] [Google Scholar]
- 20.Meyer JA, Johnson WR. Cost shifting in health care: an economic analysis. Health Aff (Millwood) 1983 Summer;2(2):20–35. doi: 10.1377/hlthaff.2.2.20. [DOI] [PubMed] [Google Scholar]
- 21.Gruber J, Rodriguez How much uncompensated care do doctors provide? J of Health Econ. 2007 Dec 1;26(6):1151–1169. doi: 10.1016/j.jhealeco.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Cunningham PJ, May JH. A growing hole in the safety net: physician charity care declines again. [Accessed 1/3/13.];Center for Health Systems Change Tracking Study. (13) http://hschange.org/CONTENT/826/826.pdf. [PubMed]
- 23.Blumenthal J, Plummer E, Gambert SR. [Accessed 1/3/13.];Trauma in the Elderly: Causes and Prevention. Clinical Geriatrics. http://www.clinicalgeriatrics.com/articles/Trauma-Elderly-Causes-and-Prevention.