Abstract
BACKGROUND
Studies have demonstrated that relative value units (RVUs) do not appropriately reflect cognitive effort or time spent in patient care, but RVU continues to be used as a standardized system to track productivity. It is unknown how well RVU reflects the effort of acute care surgeons. Our objective was to determine if RVUs adequately reflect increased surgeon effort required to treat emergent versus elective patients receiving similar procedures.
METHODS
A retrospective analysis using The American College of Surgeons’ National Surgical Quality Improvement Program 2011 data set was conducted. The control group consisted of patients undergoing elective colectomy, hernia repair, or biliary procedures as identified by Current Procedural Terminology. Comparison was made to emergent cases after being stratified to laparoscopic or open technique. Generalized linear models and logistic regression were used to assess specific outcomes, controlling for demographics and comorbidities of interest. The RVUs, operative time, and length of stay (LOS) were primary variables, with major/minor complications, mortality, and readmissions being evaluated as the relevant outcomes.
RESULTS
A total of 442,149 patients in the National Surgical Quality Improvement Program underwent one of the operative procedures of interest; 27,636 biliary (91% laparoscopic; 8.5% open), 28,722 colorectal (40.3% laparoscopic, 59.7% open), and 31,090 hernia (26.6% laparoscopic, 73.4% open) operations. Emergent procedures were found to have average RVU values that were identical to their elective case counterparts. Complication rates were higher and LOS were increased in emergent cases. Odds ratios for complications and readmissions in emergent cases were twice those of elective procedures. Mortality was skewed toward emergent cases.
CONCLUSION
Our data indicate that the emergent operative management for various procedures is similarly valued despite increased LOS, more complications, higher mortality risk, and subsequently increased physician attention. Our findings suggest that the RVU system for acute care surgeons may need to be reevaluated to better capture the additional work involved in emergent patient care.
Keywords: Relative value unit (RVU), acute care surgery, medical billing, critical care surgery, emergency general surgery
Introduction
Acute care surgeons, many of whom cover trauma, critical care, and emergency general surgery, have found themselves involved in a unique specialty that has taken over the burden of emergent operative management in many hospitals across the country. Preoperative and post-operative counseling and decision making, the technical portion of these emergent operations, and any necessary intensive care required is provided by the Acute Care Surgery (ACS) team. The AAST and affiliates recognized more than 4 million emergent surgical admissions across the United States in 2009, with numbers that are expected to grow1.
Emergencies occur without regard for time and require an on-call team to manage them at all hours2. The emergent diagnoses may not be straightforward due to confounding of co-morbidities that cannot be optimized prior to operation. Consequently complications occur more frequently than in patients who undergo elective surgery3,4. Emergent operations carry higher risk, are known to be associated with greater mortality, and have increased lengths of stay on average when compared to similar planned, elective operations5,6,7,8. As ACS services develop and hospitals trend toward incentivized compensation plans, it is becoming apparent that there is a difference in the work required to facilitate emergent cases9.
All surgical cases are coded into the Current Procedural Terminology (CPT) which is then assigned Relative Value Units for reimbursement value. Establishment of an ACS team maintains profitability for surgical specialty groups, trauma and emergency general surgeons, with relative value units, or RVUs being the standardized comparative value to benchmark surgeon productivity10,11. RVUs are assigned to CPT codes and are calculated to account for physician work, expenses, and malpractice costs. The number of RVUs generated is based on Medicare definitions to reflect standard resources allocated for a typical operations in each category. Operative cases are assigned RVU weights based on CPT coding without ability to designate emergent from elective; complex operations are not readily distinguished from more straight forward, elective procedures within CPT nor consequently within RVU unless a modifier is added to adjust for unusual operative services. Resultantly, RVUs may not give accurate indication to the amount of work performed in ACS per patient inside or outside of the operative theater.
There may be a need to adjust the RVU system for the intricacies of ACS and emergent operations, but the appropriateness of the RVU to reflect surgeon effort in the ACS field has not yet been fully evaluated. We hypothesized that we would find no difference in RVUs for emergent or elective cases. It is our objective to determine if RVUs reflect increased surgeon effort required to treat emergent patients when compared to elective patients receiving similar procedures.
Methods
Data source
This study was a retrospective analysis of patients included in the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) 2011 dataset. The NSQIP was used because it represents an annual report of risk adjusted surgical outcomes where data is collected prospectively and followed for 30 post-operative days using patient records and phone interviews. It additionally contains information on CPT, identifies cases as emergent, and relays risk adjusted data on complications, readmissions, and mortality. The markers that are followed in NSQIP are indirect indicators of surgeon effort; time and attention per patient is assumed for patients requiring increased LOS, having more complications, taking more physician attention for decision making, and needing continuous long-term care and follow-up.
Inclusion Criteria
Adult patients over 18 years of age undergoing elective or emergent colectomy, hernia repair, or biliary procedures were identified using Current Procedural Terminology (CPT) codes listed in addendum 1.
Data Collection and Variables Examined
The database was examined for demographic characteristics such as age, sex, and race, comorbid conditions, operative characteristics, and 30-day postoperative complications and mortality. Table 1 shows basic demographic information, mortality, and grouped complications.
Table 1.
Patient characteristics and pre-operative risk factors
| Biliary | Colorectal | Hernia | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| laparoscopic | open | laparoscopic | open | laparoscopic | open | |||||||
|
| ||||||||||||
| elective | emergent | elective | emergent | elective | emergent | elective (%) | emergent | elective | emergent | elective | emergent | |
| Age, mean (SD) | 49.07 (17.16) | 48.58 (18.34) | 60.76 (16.01) | 61.03 (17.69) | 60.27 (15.24) | 61.66 (17.30) | 62.08 (15.54) | 64.47 (15.71)* | 54.25 (14.90) | 53.68 (17.24) | 57.60 (15.78) | 62.90 (18.09)* |
| Sex, female, n (%) | 16390 (72.34) | 1744 (65.91)* | 959 (50.18) | 178 (42.28)** | 5836 (52.23) | 224 (56.28) | 6730 (51.65) | 2242 (54.43)** | 1856 (22.91) | 88 (53.01)* | 6205 (28.32) | 358 (39.47)* |
| Race, n (5) | ||||||||||||
| White | 16742 (73.89) | 1771 (66.93)* | 1374 (71.90) | 281 (66.75)** | 9036 (80.87) | 298 (74.87)* | 10072 (77.29) | 3069 (74.51)* | 6609 (81.56) | 128 (77.11)** | 16859 (76.93) | 640 (70.56)* |
| Black | 2124 (9.37) | 246 (9.30) | 254 (13.29) | 44 (10.45) | 854 (7.64) | 33 (8.29) | 1318 (10.11) | 403 (9.78) | 681 (8.40) | 13 (7.83) | 1995 (9.10) | 130 (14.33) |
| Others | 3792 (16.73) | 629 (23.77) | 283 (14.80) | 96 (22.81) | 1284 (11.49) | 67 (16.84) | 1641 (12.60) | 647 (15.71) | 813 (10.03) | 25 (15.06) | 3060 (13.97) | 137 (15.10) |
| Death, N (%) | 59 (0.26) | 11 (0.42) | 27 (1.41) | 27 (6.41)* | 106 (0.95) | 25 (6.28)* | 358 (2.75) | 657 (15.95)* | 14 (0.17) | 6 (3.61)* | 62 (0.28) | 29 (3.20)* |
p < 0.001
p < 0.01
p < 0.05
Demographic data for patients undergoing elective and emergent, laparoscopic and open biliary, colorectal, and hernia cases as found in the NSQIP dataset from 2011
CPT codes for biliary, colectomy, and hernia cases were chosen because they were previously defined by the AAST and affiliates as ACS operations and they represent cases that are known to present in both an emergent and elective fashion12,1. Figure 1 displays the sequence of surgical procedures stratified into study groups (emergent versus elective for laparoscopic and open techniques.)
Figure 1.
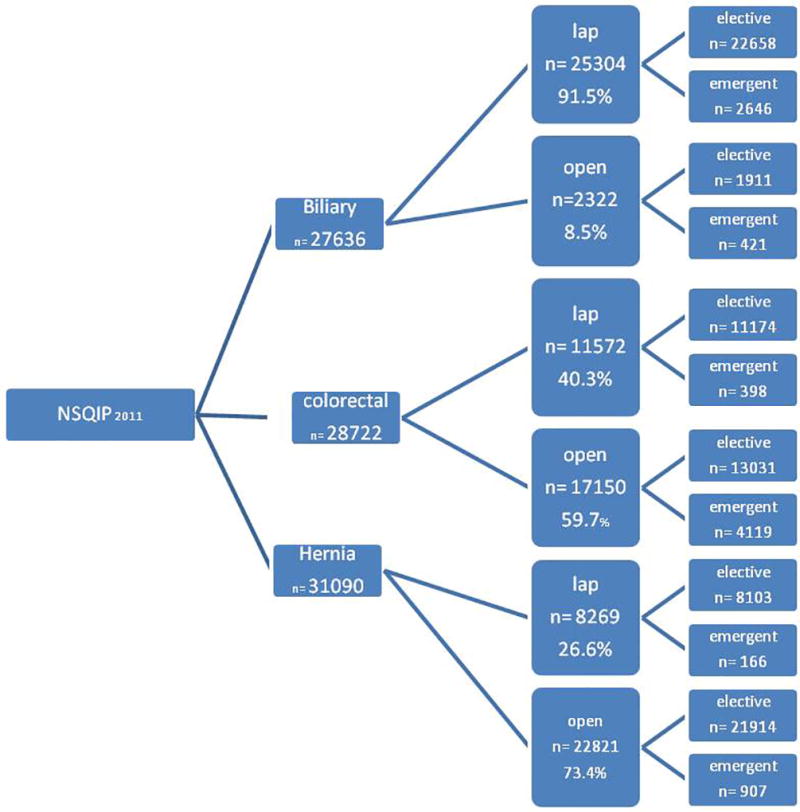
Inclusions from 2011 NSQIP
Codes were chosen for both laparoscopic and open procedures in all three case categories. They were then stratified into emergent or elective based on how they were entered into the NSQIP database. In table 2 frequencies of each CPT were calculated.
Table 2.
Frequencies of CPT Codes Used
| Frequency of Emergent Laparoscopic Biliary | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 47562 | 1959 | 74.04 | 74.04 |
| 47563 | 659 | 24.91 | 98.94 |
| 47564 | 28 | 1.06 | 100 |
| Total | 2646 | 100 | |
| Frequency of Elective Laparoscopic Biliary | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 47562 | 16945 | 74.79 | 74.79 |
| 47563 | 5571 | 24.59 | 99.37 |
| 47564 | 142 | 0.63 | 100.00 |
| Total | 22658 | 100 | |
| Frequency of Emergent Open Biliary | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 47600 | 340 | 80.76 | 80.76 |
| 47605 | 61 | 14.49 | 95.25 |
| 47610 | 16 | 3.8 | 99.05 |
| 47612 | 3 | 0.71 | 99.76 |
| 47620 | 1 | 0.24 | 100.00 |
| Total | 421 | 100.00 | |
| Frequency of Elective Open Biliary | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 47600 | 1376 | 72 | 72 |
| 47605 | 359 | 18.79 | 90.79 |
| 47610 | 124 | 6.49 | 97.28 |
| 47612 | 33 | 1.73 | 99.01 |
| 47620 | 19 | 0.99 | 100 |
| Total | 1911 | 100.00 | |
| Frequency of Emergent Laparoscopic Colorectal | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 44204 | 214 | 53.77 | 53.77 |
| 44205 | 65 | 16.33 | 70.10 |
| 44206 | 64 | 16.08 | 86.18 |
| 44207 | 26 | 6.53 | 92.71 |
| 44210 | 18 | 4.52 | 97.24 |
| 44208 | 5 | 1.26 | 98.49 |
| 44211 | 4 | 1.01 | 99.50 |
| 44213 | 2 | 0.50 | 100.00 |
| Total | 398 | 100.00 | |
| Frequency of Elective Laparoscopic Colorectal | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 44204 | 5399 | 48.32 | 48.32 |
| 44207 | 2471 | 22.11 | 70.43 |
| 44205 | 2116 | 18.94 | 89.37 |
| 44210 | 449 | 4.02 | 93.39 |
| 44211 | 280 | 2.51 | 95.89 |
| 44208 | 236 | 2.11 | 98.00 |
| 44206 | 177 | 1.58 | 99.59 |
| 44213 | 46 | 0.41 | 100.00 |
| Total | 11174 | 100.00 | |
| Frequency of Emergent Laparoscopic Colorectal | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 44143 | 1251 | 30.37 | 30.37 |
| 44140 | 1112 | 27.00 | 57.37 |
| 44160 | 731 | 17.75 | 75.12 |
| 44144 | 381 | 9.25 | 84.37 |
| 44141 | 372 | 9.03 | 93.40 |
| 44145 | 106 | 2.57 | 95.97 |
| 44146 | 77 | 1.87 | 97.84 |
| 44155 | 40 | 0.97 | 98.81 |
| 45111 | 15 | 0.36 | 99.17 |
| 44157 | 9 | 0.22 | 99.39 |
| 44158 | 6 | 0.15 | 99.54 |
| 45110 | 5 | 0.12 | 99.66 |
| 44147 | 3 | 0.07 | 99.73 |
| 44156 | 2 | 0.05 | 99.78 |
| 45112 | 2 | 0.05 | 99.83 |
| 45113 | 2 | 0.05 | 99.88 |
| 45119 | 2 | 0.05 | 99.93 |
| 45114 | 1 | 0.02 | 99.95 |
| 45116 | 1 | 0.02 | 99.98 |
| 45123 | 1 | 0.02 | 100.00 |
| Total | 4119 | 100.00 | |
| Frequency of Elective Laparoscopic Colorectal | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 44140 | 4,295 | 32.96 | 32.96 |
| 44145 | 2,112 | 16.21 | 49.17 |
| 44160 | 2,081 | 15.97 | 65.14 |
| 44143 | 910 | 6.98 | 72.12 |
| 45110 | 784 | 6.02 | 78.14 |
| 44141 | 470 | 3.61 | 81.74 |
| 44146 | 446 | 3.42 | 85.17 |
| 44144 | 332 | 2.55 | 87.71 |
| 44155 | 270 | 2.07 | 89.79 |
| 45111 | 239 | 1.83 | 91.62 |
| 45119 | 203 | 1.56 | 93.18 |
| 45113 | 192 | 1.47 | 94.65 |
| 44158 | 190 | 1.46 | 96.11 |
| 45112 | 187 | 1.44 | 97.54 |
| 45123 | 113 | 0.87 | 98.41 |
| 44147 | 85 | 0.65 | 99.06 |
| 44157 | 67 | 0.51 | 99.58 |
| 45114 | 30 | 0.23 | 99.81 |
| 45116 | 10 | 0.08 | 99.88 |
| 45121 | 9 | 0.07 | 99.95 |
| 44156 | 6 | 0.05 | 100.00 |
| Total | 13,031 | 100.00 | |
| Frequency of Emergent Laparoscopic Hernia | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 49653 | 85 | 51.20 | 51.20 |
| 49652 | 46 | 27.71 | 78.92 |
| 49650 | 26 | 15.66 | 94.58 |
| 49651 | 9 | 5.42 | 100.00 |
| Total | 166 | 100.00 | |
| Frequency of Elective Laparoscopic Hernia | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 49650 | 4296 | 53.02 | 53.02 |
| 49652 | 2217 | 27.36 | 80.38 |
| 49653 | 1001 | 12.35 | 92.73 |
| 49651 | 589 | 7.27 | 100.00 |
| Total | 8103 | 100.00 | |
| Frequency of Emergent Open Hernia | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 49507 | 329 | 36.27 | 36.27 |
| 49560 | 168 | 18.52 | 54.80 |
| 49553 | 129 | 14.22 | 69.02 |
| 49505 | 100 | 11.03 | 80.04 |
| 49521 | 71 | 7.83 | 87.87 |
| 49565 | 54 | 5.95 | 93.83 |
| 49520 | 16 | 1.76 | 95.59 |
| 49568 | 13 | 1.43 | 97.02 |
| 49557 | 12 | 1.32 | 98.35 |
| 49550 | 10 | 1.10 | 99.45 |
| 49525 | 4 | 0.44 | 99.89 |
| 49555 | 1 | 0.11 | 100.00 |
| Total | 907 | 100.00 | |
| Frequency of Elective Open Hernia | |||
|---|---|---|---|
|
| |||
| CPT | Frequency | Percentage | Cumulative |
| 49505 | 10,602 | 48.38 | 48.38 |
| 49560 | 6,369 | 29.06 | 77.44 |
| 49565 | 1.877 | 8.57 | 86.01 |
| 49520 | 1,090 | 4.97 | 90.98 |
| 49507 | 984 | 4.49 | 95.47 |
| 49525 | 249 | 1.14 | 96.61 |
| 49550 | 939 | 1.06 | 97.67 |
| 49568 | 175 | 0.80 | 98.47 |
| 49521 | 160 | 0.73 | 99.20 |
| 49553 | 139 | 0.63 | 99.83 |
| 49557 | 21 | 0.10 | 99.93 |
| 49555 | 16 | 0.07 | 100.00 |
| Total | 21,914 | 100.00 | |
Emergent cases were agreed upon by both the attending surgeon and the anesthesiologist and if there was disagreement within the documentation then NSQIP reviewers utilized operative notes and additional charted documentation for best judgment in qualifying cases as emergent. Additionally cases defined as emergent were expected to have operative management within 12 hours of either admission or disease onset based on the criteria outlined within the NSQIP dataset.
Independent variables of interest included Work Relative Value Unit (RVU), length of total hospital stay (LOS), and total operation time (OR time). RVUs for emergent and elective cases, stratified by laparoscopic or open technique were shown in table 3. Table 4 indicated the primary variables of interest including LOS and OR time.
Table 3.
RVU values for each case type and the difference of the means
| OPEN | OPEN | Laparoscopic | Laparoscopic | |||
|---|---|---|---|---|---|---|
| Average | ELECTIVE | EMERGENT | Difference Mean | ELECTIVE | EMERGENT | Difference Mean |
| RVU BILIARY | 17.54 | 17.45 | −0.09 | 11.86 | 11.87 | 0.01 |
| RVU COLORECTAL | 26.01 | 25.7 | −0.31 | 27.51 | 27.01 | 0.5 |
| RVU HERNIA | 9.73 | 10.29 | 0.56 | 9.5 | 11.43 | 1.93* |
Represents the only statistically significant difference in RVU due to small sample size for laparoscopic hernia cases
Table 4.
The LOS and OR time data for each case type
| OPEN | OPEN | Laparoscopic | Laparoscopic | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| ELECTIVE | EMERGENT | Difference Mean | ELECTIVE | EMERGENT | Difference Mean | |
| BILIARY | ||||||
| LOS (days) | 7.36 | 8.61 | 1.25 | 1.64 | 3.12 | 1.48 |
| OR time (min) | 131.4 | 123.95 | −7.45 | 66.36 | 74.76 | 8.4 |
| COLORECTAL | ||||||
| LOS (days) | 10.07 | 13.33 | 3.26 | 6.16 | 8.52 | 2.36 |
| OR time (min) | 184.27 | 138.8 | −45.47 | 172.31 | 141.95 | −30.36 |
| HERNIA | ||||||
| LOS (days) | 1.34 | 4.5 | 3.16 | 0.58 | 2.21 | 2.63 |
| OR time (min) | 76.53 | 80.73 | 4.2 | 71.31 | 80.08 | 8.77 |
Outcome Parameters
Outcomes that were examined include readmissions, mortality, and 30-day complications. Any complication was distinguished as “yes” if it occurred within 30 days of admission. Complications were defined as deep incisional SSI, wound disruption, unplanned intubation, PE, dialysis, CVA/stroke, cardiac arrest, MI, bleeding transfusion, sepsis, septic shock and return to OR. Additional complications were superficial SSI, pneumonia, progressive renal insufficiency, and DVT. Each complication was analyzed separately in table 5.
Table 5.
Emergent Odds Ratio Compared with Elective Case Controls in Each Category for Complications, Mortality, and Readmission
| Biliary | Colorectal | Hernia | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| laparoscopic | open | laparoscopic | open | laparoscopic | open | |
|
|
|
|
||||
| Superficial SSI | 0.69 | 0.61 | 1.50 | 0.83 | 2.86 | 1.54 |
| Deep Incisional SSI | 1.17 | 1.15 | 1.36 | 0.93 | 3.25 | 1.31 |
| Organ SSI | 1.16 | 1.01 | 1.13 | 1.41 | 7.10 | 1.71 |
| Wound distrupt | 0.53 | 0.66 | 1.47 | 1.31 | 5.91 | 1.91 |
| Pneumonia | 1.92 | 2.45 | 2.93 | 1.87 | 6.71 | 3.36 |
| Unplanned intubation | 2.32 | 1.65 | 2.81 | 2.12 | 7.74 | 1.86 |
| Pulmonary embolism | 1.70 | 1.31 | 1.98 | 0.92 | 2.00 | |
| Renal insufficiency | 1.27 | 0.99 | 0.51 | 1.32 | 2.45 | |
| Dialysis | 2.25 | 2.40 | 3.61 | 2.85 | 2.17 | 3.08 |
| Urinary track infection | 1.28 | 1.11 | 1.18 | 0.86 | 0.72 | 2.51 |
| CVA/shock | 0.44 | 17.73 | 2.08 | 1.23 | 1.03 | |
| Cardiac arrest | 0.58 | 5.93 | 1.61 | 3.19 | 11.51 | 2.44 |
| MI | 1.29 | 4.17 | 0.88 | 1.85 | 10.69 | 2.68 |
| Bleeding transfusion | 1.90 | 1.54 | 1.65 | 1.52 | 3.91 | 1.70 |
| DVT | 2.74 | 2.07 | 1.95 | 1.35 | 2.85 | 1.53 |
| Sepsis | 1.67 | 0.81 | 1.04 | 0.92 | 5.78 | 2.62 |
| Septic shock | 2.32 | 2.21 | 2.86 | 3.12 | 14.68 | 1.78 |
| Return to OR | 1.34 | 1.25 | 1.34 | 1.60 | 2.26 | |
| Mortality | 1.16 | 3.93 | 3.26 | 4.41 | 19.94 | 3.48 |
| Readmission | 1.00 | 0.92 | 1.20 | 0.86 | 1.23 | 0.96 |
Statistically significant results are in bold
Statistical Analysis
For continuous demographic data, comparisons were made using the Welch test, a type of t test that allows comparison amongst two groups with heterogeneity of variance. Univariate comparisons were performed of primary outcome measures in patients with and without pre-operative comorbidities using the Pearson χ2 test. To determine predictors of postoperative outcomes in these patients, a backward stepwise model was constructed with postoperative mortality as the dependent variable and all of the previously mentioned preoperative comorbidities and post-operative complications as independent variables. Generalized linear models were employed to assess outcomes, controlling for 14 preoperative risk factors that included demographics and comorbidities (age, sex, race, BMI, report of smoking within one year of admission, diabetes mellitus controlled with oral agents or insulin, history of severe COPD, history of myocardial infarction 6 months prior to surgery, hypertension requiring medication, acute renal failure, CVA/stroke with neurological deficit, disseminated cancer, steroid use for chronic condition, systemic sepsis). Analyses were then stratified by open versus laparoscopic interventions to compare outcomes for patients undergoing emergent versus elective operations.
Statistical analyses were performed using Stata/MP statistical software version 12 (StataCorp, College Station, Texas). Statistical significance was set at p<0.05.
Results
Of the 442,149 patients in NSQIP for the year 2011, there were 27,636 biliary, 28,722 colorectal, and 31,090 hernia procedures by CPT code. Figure 1 shows how the cases were distributed.
Table 1 shows basic demographic data and data on frequency of preoperative comorbidities. Comorbid conditions were seen more frequently in emergent level cases.
Addendum 1 and table 2 show CPT codes used and frequencies when examined by case type. The RVUs for groupings of emergent and elective cases in all three categories, stratified by laparoscopic or open, were not significantly different from each other as shown in table 3.
As seen in tables 4 and 5, when emergent and elective cases were compared within the same case category type, the average length of stay and the complication rates for the emergent procedures were universally longer and higher. Odds of mortality, SSI, PNA, unplanned re-intubations, need for dialysis with new onset renal failure, need for transfusion post operatively, DVTs, septic shock and return to OR were all significantly higher in emergent cases when compared to elective ones. This was despite emergent and elective case types generating nearly identical RVUs. The operative times were, in several cases, considerably shorter in emergent procedures. Mortality in emergent cases was higher indicating a more complex patient population. Mortality odds demonstrated higher likelihood of death in the emergent case types, although significantly skewed results were seen in the laparoscopic emergent hernia category due to low sample size. Higher complications and longer lengths of stay in the emergent sector translated into more surgeon attention and more dedicated time for this population during the hospitalization.
Discussion
This analysis of over 90,000 patients demonstrates that, for three common surgical conditions, the RVU system does not distinguish the extra work required for emergent patient care. In most cases emergency and elective operations were rewarded the same amount of RVUs, even though emergent cases were found to be associated with longer LOS, more complications, and higher readmission and mortality rates. The RVU does not reliably reflect complexity or care required for emergent operations, but continues to be used by administration and payer entities to evaluate and compare surgeon productivity. A potential solution is to create a modifier for emergent operations, which demand more surgeon attention, time, and ultimately, effort. Schneider et al. have previously shown that emergent colectomies have longer LOS, higher mortality, and more complications, but they did not examine the RVU valuation compared to the elective population RVUs. Our study emphasizes that complexities of the emergent patient population extrapolate to surgeon attention and time taken from other duties that could generate additional RVUs13. We are the first to show that despite worse outcomes for ACS emergencies, there has been no change in compensation standards or recognition for the work being done.
RVUs are defined by The Center for Medicare and Medicaid Services (CMS) as a standardized measurement for productivity of multiple entities, including the individual and the institution; they reflect the preoperative evaluation, the operation itself, and the global coverage period, even when used by entities other than Medicare14. RVU is now inappropriately extrapolated for this purpose by third party payers, insurance companies, and government programs, but is not a complete translation of productivity in surgical fields where time is spent in additional endeavors outside the operative theater. For example the ACS surgeon is additionally responsible for complex counseling, end of life care, ICU coverage, consult responsibility, and trauma amongst other aspects of care. Arguments against RVUs for productivity measurement come from academic physicians and surgeons, whose time is spent in the education of trainees, research pursuits, or innovation, none of which can be captured or acknowledged in a system that only recognizes RVU-defined productivity15,16. This RVU dichotomy simply does not reflect ACS work.
Medicare enforces a global period, which means that once decision for surgery has been made, the operative diagnosis cannot be double billed. Any additional credit for work done on post-operative patients comes in the form of E/M coding or with modification of the operative CPT. E/M coding must be supported with extensive documentation and is still subject to denial in post-operative patients; modifiers are attached to CPT codes to identify unusual circumstances pertaining to operative cases and are not used for post-operative complexities. For an elective general surgeon a global period seems reasonable since the care can be standardized amongst patients. It is harder to standardize emergent care because the preoperative and post-operative variables are often unpredictable and complicated17. In our study we found complications occurred more frequently in the emergent population. Those same patients also had more preoperative comorbidities on average. The significance of these findings is that within the global period, diagnoses related to operative intervention, whether as contributors or consequences can only be billed once unless specifically modified and supported with documentation. In caring for the emergent population, surgeon time is directed toward these complexities and subsequently away from new patients where additional RVUs could be generated.
While it has been shown that RVU generation is higher for surgeons who spend time providing critical care than those who do not, this was only found to be true in groups where the remaining members are clinically productive and billing diagnoses are vast beyond the operative diagnosis where critical care billing or E/M can be applied18. This model implies that there should be pooling of the group’s RVUs to increase overall reflection of productivity, but this model takes away each individual’s contribution and makes the individual dependent on group effort.
We found little RVU distinction in comparing emergent laparoscopic to elective laparoscopic cases for biliary, hernia, and colectomy procedures, but there were significantly less RVUs generated for biliary laparoscopic than for open biliary cases. This is a stark contrast to what has been noted in other surgical specialties. For example plastic surgeons have noted that increasing complexity and therefore increased RVU’s corresponded to higher complication rates for patients19. In vascular surgery longer open procedures are reimbursed by fewer RVU’s than shorter endovascular cases, without consideration of the complexity of open technique20. In a generation where only the most difficult aortas are operated on in an open, often staged fashion, this discrepancy suggests that RVU may inappropriately value other subspecialists. Moreover, endovascular approaches are subject to fewer wound complications in the immediate post-operative period than are open procedures of the same type. Vascular surgeons have noted that the RVU system may not define their true work load either, specifically in terms of efficiency, obligations to academia, or patient satisfaction measures and that potentially the RVU should not be a sole indicator of surgeon productivity21.
We also demonstrated an increased odds ratio of reoperation in our emergent sector in every emergent case category. The planned and unexpected reoperation rates in ACS and trauma are higher and abdomens are left purposefully open more often than seen in elective cases22,23. While RVUs can be calculated for each portion of the case, there is additional effort and time associated with repeated trips to the operating room, often for low RVU level washouts or straightforward closures.
When compared to an elective general surgery practice, it seems that the acute care surgeon may be getting short changed-their operations occur at unscheduled times, have consequently more frequent complications, and require more overall surgeon effort. Our data specifically demonstrates that emergent cases have higher odds of complication and mortality with longer length of stay, but the credit, as measured by RVU, per case is identical to non-emergent cases of same type. Plus, the patients’ preoperative comorbidities cannot be optimized prior to emergent operations24. When cases are scheduled electively there is time for complete workup, imaging adlib, full laboratory data, and discussion with the patient and family regarding each intricacy of the case. Patients with comorbidities may even be managed non-operatively when operative management is otherwise elective, but the acute care surgeon does not have the luxury of patient selection, time to plan, or complete workup in many cases25.
The governing agency, Centers for Medicare and Medicaid Services, or CMS, of approximately 30 appointed members, revises the RVU pay scale no less than every 5 years26. Multiple physician groups have requested modifications to reflect a cognitive portion and other important clinical endeavors that are not notable in RVU, suggesting a potential modifier or even an overall critique of RVU as a fair and reasonable reflection of daily work27,28,29.
The RVU system’s main weakness is that procedures and services are bundled, which creates over and under estimation of work30. We believe that there is potentially a justification for reconsideration of the RVU system or for the addition of a modifier that reflects this more complex population. As hospitals focus on cost analysis and on pay-for-performance plans, it seems reasonable that specialty services be appropriately recognized for effort and time spent. Without appropriate recognition or incentive for the additional work involved in ACS, it is possible that in time the field will lose recruitment power. General surgeons are in shortage, previously attributed to hours, call obligation, and workload without adequate compensation31,32,33,34,35. As acute care services have emerged there have been many studies looking the feasibility of established teams, particularly trauma, to handle the obligations of an ACS team36,37,38. When we examine the short changing of the RVU system in defining our true productivity and time spent, the ACS field is not competitive on paper when compared to specialties that are appropriately recognized for their work, and we are at risk of losing surgeons to other fields39.
Limitations to this study include that elective procedures heavily outweighed the emergent procedures in every category evaluated, which is expected, but comparisons of average RVU values were better represented by the elective case categories. Physician services not related to the primary operative diagnosis may be billed separately but were not considered in this analysis. Additional E/M billing was also not considered. This analysis sought to evaluate the RVU value in the context of elective versus emergent operative procedures only.
Emergency general surgeon work is evaluated based on a standardized coding system even though there is an unfavorable difference in complication rate and length of stay for emergent procedures. The increased physician attention required for dealing with complications and the complexities of emergency care, not to mention the unpredictable nature of ACS, deserves consideration of a modifier in the coding system that might better capture the additional work involved in caring for this population.
Acknowledgments
Conflicts of Interest and Source of Funding:
National Institutes of Health/ NIGMS K23GM093112-01
American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care
Footnotes
This study was presented at the 72nd annual meeting of the American Association for the Surgery of Trauma, September 18–21, 2013, in San Francisco, California
Author Contribution:
Literature search (DS, AH), study design (DS, AH, ES, XH, CV, DL), data collection (ES, XH, CV), data analysis (AH, ES, XH), data interpretation (DS, AH, ES, XH, CV, SS), writing (DS, AH, XH), critical revision (DS, AH, XH, EH, DE, SS)
References
- 1.Shafi S, Aboutanos MB, Agarwal S, Jr, Brown CV, Crandall M, Feliciano DV, Guillamondegui O, Haider A, Inaba K, Osler TM, Ross S, Rozycki GS, Tominaga GT. AAST Committee on Severity Assessment and Patient Outcomes. Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg. 2013 Apr;74(4):1092–7. doi: 10.1097/TA.0b013e31827e1bc7. [DOI] [PubMed] [Google Scholar]
- 2.Vaziri K, Roland JC, Robinson L, Fakhry SM. Optimizing physician staffing and resource allocation: sine-wave variation in hourly trauma admission volume. J Trauma. 2007 Mar;62(3):610–4. doi: 10.1097/TA.0b013e31803245c7. [DOI] [PubMed] [Google Scholar]
- 3.Fakhry SM, Martin B, Al Harakeh H, Norcross ED, Ferguson PL. Proportional costs in trauma and acute care surgery patients: dominant role of intensive care unit costs. J Am Coll Surg. 2013 Apr;216(4):607–14. doi: 10.1016/j.jamcollsurg.2012.12.031. discussion 614-6. [DOI] [PubMed] [Google Scholar]
- 4.Wood L, Buczkowski A, Panton OM, Sidhu RS, Hameed SM. Effects of implementation of an urgent surgical care service on subspecialty general surgery training. Can J Surg. 2010 Apr;53(2):119–25. [PMC free article] [PubMed] [Google Scholar]
- 5.Diaz JJ, Jr, Norris PR, Gunter OL, Collier BR, Riordan WP, Morris JA., Jr Does regionalization of acute care surgery decrease mortality? J Trauma. 2011 Aug;71(2):442–6. doi: 10.1097/TA.0b013e3182281fa2. [DOI] [PubMed] [Google Scholar]
- 6.Altom LK, Snyder CW, Gray SH, Graham LA, Vick CC, Hawn MT. Outcomes of emergent incisional hernia repair. Am Surg. 2011 Aug;77(8):971–6. [PubMed] [Google Scholar]
- 7.Klima DA, Brintzenhoff RA, Agee N, Walters A, Heniford BT, Mostafa G. A review of factors that affect mortality following colectomy. J Surg Res. 2012 May 15;174(2):192–9. doi: 10.1016/j.jss.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Smith M, Hussain A, Xiao J, Scheidler W, Reddy H, Olugbade K, Jr, Cummings D, Terjimanian M, Krapohl G, Waits SA, Campbell D, Jr, Englesbe MJ. The importance of improving the quality of emergency surgery for a regional quality collaborative. Ann Surg. 2013 Apr;257(4):596–602. doi: 10.1097/SLA.0b013e3182863750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parent MB, McArthur K, Sava J. Are emergency general surgery patients more work than trauma patients? Characterizing surgeon work in an acute care surgery practice. J Trauma Acute Care Surg. 2013 Jan;74(1):289–93. doi: 10.1097/TA.0b013e318278935f. [DOI] [PubMed] [Google Scholar]
- 10.Preston RM, Wildman E, Chang MC, Meredith JW. Acute Care Surgery: Impact on Practice and Economics of Elective Surgeons. J Am Coll Surg. 2012 Apr;214:531–8. doi: 10.1016/j.jamcollsurg.2011.12.045. [DOI] [PubMed] [Google Scholar]
- 11.Austin MT, Diaz JJ, Jr, Feurer ID, Miller RS, May AK, Guillamondegui OD, Pinson CW, Morris JA. Creating an emergency general surgery service enhances the productivity of trauma surgeons, general surgeons and the hospital. J Trauma. 2005 May;58(5):906–10. doi: 10.1097/01.ta.0000162139.36447.fa. [DOI] [PubMed] [Google Scholar]
- 12.Nelson BV, Talboy GE., Jr Acute care surgery: redefining the general surgeon. Mo Med. 2010 Sep-Oct;107(5):313–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Schneider EB, Haider AH, Lidor AO, Efron JE, Villegas CV, Stevens KA, Hirani SA, Haut ER, Efron DT. Global Surgical Package Reimbursement and the Acute Care Surgeon: A Threat to Optimal Care. J Trauma. 2011 Mar;70(3):583–9. doi: 10.1097/TA.0b013e3182098a30. [DOI] [PubMed] [Google Scholar]
- 14.Glass KP, Anderson JR. Relative value units: from A to Z. J Med Pract Manage. 2002;17:225–8. [PubMed] [Google Scholar]
- 15.Berger JR, Maher RF. An Innovative approach for calculating the work relative value units of clinical activities otherwise concealed. Acad Med. 2011 Jul;86(7):853–7. doi: 10.1097/ACM.0b013e31821deade. [DOI] [PubMed] [Google Scholar]
- 16.Akl EA, Meerpohl JJ, Raad D, Piaggio G, Mattioni M, Paggi MG, Gurtner A, Mattarocci S, Tahir R, Muti P, Schunemann HJ. Effects of assessing the productivity of faculty in academic medical centres: a systematic review. CMAJ. 2012 Aug 7;184(11):E602–12. doi: 10.1503/cmaj.111123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg. 2011 Jan;212(1):20–28. doi: 10.1016/j.jamcollsurg.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 18.Van der Wilden GM, Schmidt U, Chang Y, Bittner EA, Cobb JP, Velmahos GC, Alam HB, de Moya MA, King DR. Implementation of 24/7 intensivist presence in the SICU: effect on processes of care. J Trauma Acute Care Surg. 2013 Feb;74(2):563–7. doi: 10.1097/TA.0b013e31827880a8. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen KT, Gart MS, Smetona JT, Aggarwal A, Bilimoria KY, Kim JY. The relationship between relative value units and outcomes: a multivariate analysis of plastic surgery procedures. Eplasty. 2012;12:e60. Epub 2012 Dec 27. [PMC free article] [PubMed] [Google Scholar]
- 20.Martin JD, Warble PB, Hupp JA, Mapes JE, Stanziale SF, Weiss LL, Schiller TB, Hanson LA. A real world analysis of payment per unit time in a Maryland Vascular Practice. J Vasc Surg. 2010 Oct;52(4):1094–8. doi: 10.1016/j.jvs.2010.04.072. discussion 1098-9. [DOI] [PubMed] [Google Scholar]
- 21.Satinani B. Use, misuse, and underuse of work relative value units in a vascular surgery practice. J Vasc Surg. 2012 Jul;56(1):267–72. doi: 10.1016/j.jvs.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 22.Lamme B, Boermeester MA, Reitsma JB, Mahler CW, Obertop H, Gouma DJ. Meta analysis of relaparotomy for secondary peritonitis. Br J Surg. 2002 Dec;89(12):1516–24. doi: 10.1046/j.1365-2168.2002.02293.x. [DOI] [PubMed] [Google Scholar]
- 23.Van Ruler O, et al. Dutch Peritonitis Study Group. Comparison of on demand vs planned relaparotomy strategy in patients with severe peritonitis: A Randomized Trial. JAMA. 2007 Aug 22;298(8):865–72. doi: 10.1001/jama.298.8.865. [DOI] [PubMed] [Google Scholar]
- 24.Rivera RA, Nguyen MT, Martinez-Osorio JI, McNeill MF, Ali SK, Mansi IA. Preoperative medical consultation: maximizing its benefits. Am J Surg. 2012 Nov;204(5):787–97. doi: 10.1016/j.amjsurg.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 25.Stefan M, Iglesia Lino L, Fernandez G. Medical consultation and best practices for preoperative evaluation of elderly patients. Hosp Pract (1995) 2011 Feb;39(1):41–51. doi: 10.3810/hp.2011.02.373. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Medicare and Medicaid Services (CMS), HHS. Medicare program; revisions to payment policies and five year review of and adjustments to the relative value units under the physician fee schedule for calendar year 2002. Final rule with comment period. Fed Regist. 2001 Nov 1;66(212):55245–503. [PubMed] [Google Scholar]
- 27.Manchikanti L, Giordano J. Physician payment 2008 for interventionalists: current state of health care policy. Pain Physician. 2007 Sep;10(5):607–26. [PubMed] [Google Scholar]
- 28.Committee on Coding and Nomenclature. Application of the resource based relative value scale system to pediatrics. Pediatrics. 2008 Dec;122(6):1395–400. doi: 10.1542/peds.2008-2578. [DOI] [PubMed] [Google Scholar]
- 29.Sinsky CA, Dugdale DC. Medicare Payment for Cognitive vs Procedural Care: Minding the Gap. JAMA Intern Med. 2013 Aug 12; doi: 10.1001/jamainternmed.2013.9257. [DOI] [PubMed] [Google Scholar]
- 30.Reed RL, 2nd, Luchette FA, Esposito TJ, Pyrz K, Gamelli RL. Medicare's "Global" terrorism: where is the pay for performance? J Trauma. 2008 Feb;64(2):374–83. doi: 10.1097/TA.0b013e31815f6f11. discussion 383-4. [DOI] [PubMed] [Google Scholar]
- 31.Richardson JD. Workforce and lifestyle issues in general surgery training and practice. Arch Surg. 2002 May;137(5):515–20. doi: 10.1001/archsurg.137.5.515. [DOI] [PubMed] [Google Scholar]
- 32.Napolitano LM, Fulda GJ, Davis KA, Ashley DW, Friese R, Van Way CW, 3rd, Meredith JW, Fabian TC, Jurkovich GJ, Peitzman AB. Challenging issues in surgical critical care, trauma, and acute care surgery: a report from the Critical Care Committee of the American Association for the Surgery of Trauma. J Trauma. 2010 Dec;69(6):1619–33. doi: 10.1097/TA.0b013e3182011089. [DOI] [PubMed] [Google Scholar]
- 33.Debas HT. Surgery: a noble profession in a changing world. Ann Surg. 2002;236:263–269. doi: 10.1097/00000658-200209000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Polk HC, Vitale DS, Qadan M. The very busy urban surgeon: another face of the evermore obvious shortage of general surgeons. J Am Coll Surg. 2009 Jul;209(1):144–7. doi: 10.1016/j.jamcollsurg.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 35.Cohn SM, Price MA, Villarreal CL. Trauma and surgical critical care workforce in the United States: a severe surgeon shortage appears imminent. J Am Coll Surg. 2009 Oct;209(4):446–52. doi: 10.1016/j.jamcollsurg.2009.06.369. [DOI] [PubMed] [Google Scholar]
- 36.Endorf FW, Jurkovich GJ. Should the trauma surgeon do the emergency surgery? Adv Surg. 2007;41:155–63. doi: 10.1016/j.yasu.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 37.Cothren CC, Moore EE, Hoyt DB. The US trauma surgeon’s current scope of practice: can we deliver acute care surgery? J trauma. 2008 Apr;64(4):955–65. doi: 10.1097/TA.0b013e3181692148. [DOI] [PubMed] [Google Scholar]
- 38.Galante JM, Phan HH, Wisner DH. Trauma surgery to acute care surgery: defining the paradigm shift. J Trauma. 2010 May;68(5):1024–31. doi: 10.1097/TA.0b013e3181d76bf6. [DOI] [PubMed] [Google Scholar]
- 39.Fakhry SM, Watts DD, Michetti C, Hunt JP EAST Multi-Institutional Blunt Hollow Viscous Injury Research Group. The resident experience on trauma: declining surgical opportunities and career incentives? Analysis of data from a large multi-institutional study. J Trauma. 2003 Jan;54(1):1–7. doi: 10.1097/00005373-200301000-00001. [DOI] [PubMed] [Google Scholar]


