Abstract
Bacterial meningitis is a global public health concern, with several responsible etiologic agents that vary by age group and geographical area. The aim of this systematic review and meta-analysis was to assess the etiology of bacterial meningitis in different age groups across global regions. PubMed and EMBASE were systematically searched for English language studies on bacterial meningitis, limited to articles published in the last five years. The methodological quality of the studies was assessed using a customized scoring system. Meta-analyses were conducted to determine the frequency (percentages) of seven bacterial types known to cause meningitis: Escherichia coli, Haemophilus influenzae, Neisseria meningitidis, Streptococcus pneumoniae, group B Streptococcus agalactiae, Staphylococcus aureus, and Listeria monocytogenes, with results being stratified by six geographical regions as determined by the World Health Organization, and seven age groups.
Of the 3227 studies retrieved, 56 were eligible for the final analysis. In all age groups, S. pneumoniae and N. meningitidis were the predominant pathogens in all regions, accounting for 25.1–41.2% and 9.1–36.2% of bacterial meningitis cases, respectively. S. pneumoniae infection was the most common cause of bacterial meningitis in the ‘all children’ group, ranging from 22.5% (Europe) to 41.1% (Africa), and in all adults ranging from 9.6% (Western Pacific) to 75.2% (Africa). E. coli and S. pneumoniae were the most common pathogens that caused bacterial meningitis in neonates in Africa (17.7% and 20.4%, respectively). N. meningitidis was the most common in children aged ±1–5 years in Europe (47.0%). Due to paucity of data, meta-analyses could not be performed in all age groups for all regions.
A clear difference in the weighted frequency of bacterial meningitis cases caused by the different etiological agents was observed between age groups and between geographic regions. These findings may facilitate bacterial meningitis prevention and treatment strategies.
1 Introduction
Bacterial meningitis, an infectious disease characterized by infection and inflammation of the meninges, results in significant morbidity and mortality globally. [1] Bacterial meningitis can be fatal in 50% of cases if untreated. Even when diagnosed early and treated adequately, 8–15% of the patients die, typically within 24 and 48 hours of symptom onset. [1] Furthermore, 10–20% of the survivors are prone to permanent sequelae including brain damage, hearing loss, and learning disabilities. [1] In the USA, bacterial meningitis was responsible for an estimated 4100 cases and 500 deaths annually between 2003 and 2007, [2] while developing countries face the highest burden of disease. [3] The African Meningitis Belt, comprising 26 countries in the sub-Saharan region, has the highest meningitis disease rate; in 2009, an estimated 80,000 suspected cases of meningitis, resulting in more than 4000 deaths, were reported. [1, 4]
The etiologic agents responsible for bacterial meningitis vary by age group. Among neonates, most cases of bacterial meningitis are due to group B Streptococcus agalactiae, Escherichia coli, and Listeria monocytogenes, while most cases in children and adults are caused by Streptococcus pneumoniae and Neisseria meningitidis. [3, 5] Although Haemophilus influenzae is implicated in bacterial meningitis in all age groups, it is preponderant in children <5 years of age. [6, 7] Given the variability in bacterial meningitis incidence and causative agents across regions, clear differentiation between them is essential to manage cases of bacterial meningitis. [3, 5]
Bacterial meningitis can be reduced by the use of prevention strategies against these etiological agents, such as vaccination against H. influenzae type B (Hib), S. pneumoniae and N. meningitidis. Hib and pneumococcal conjugate vaccines were introduced in the 1990s and 2000s, and the implementation of additional prevention programs utilizing these vaccines has reduced the occurrence of bacterial meningitis. [8] It has been reported that the widespread use of Hib (against H. influenzae) and PCV7 (against S. pneumoniae) vaccines have together significantly reduced cases of bacterial meningitis worldwide, in both vaccinated and non-vaccinated populations. [6, 9, 10] Reductions were also seen on the introduction of vaccines against N. meningitidis, with a decline in rates in children from 13.5 per 100,000 in 1968–1985 to 5.2 per 100,000 in 1989–2011. [11, 12] Currently there are no vaccines available against E. coli, L. monocytogenes, or group B S. agalactiae. [13, 14] Other prevention strategies include using chemoprophylaxis to prevent secondary disease in high-risk individuals. [13, 15]
The differences in etiology by age and region are yet to be systematically reviewed on a global scale. This systematic review and meta-analysis summarizes available data on the etiology of bacterial meningitis published in the last five years, with the aim of improving current knowledge of bacterial meningitis in different age groups and geographical regions. This could contribute to the management of the disease through development of effective prevention strategies and treatment guidelines.
2 Material and methods
This systematic review was conducted following the Cochrane Collaboration and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. [16, 17] The PRISMA checklist is included in S1 Supporting Information. This study is registered with PROSPERO (CRD42017074949).
2.1 Search strategy for identification of studies
A systematic search of the PubMed and EMBASE databases was conducted (search terms listed in S1 Table), and was limited to articles published in the last five years (i.e. 25 April 2012 to 25 April 2017).
2.2 Inclusion and exclusion criteria
To be included, studies had to report original data on the etiology of bacterial meningitis in English. Studies were excluded if they were another article type (i.e. expert opinions, letters to the editor, editorials, comments, narrative reviews, and case reports), were on a genetic/molecular level, phase I/II trials, diagnostic accuracy studies, or outbreaks. Any studies that only reported data on a specific etiological agent of bacterial meningitis, considered specific types of patients (e.g., HIV-positive or immunocompromised patients), reported data on recurrent bacterial meningitis, did not permit extraction of quantitative data (e.g., if data were presented only in the form of a figure), or when the definition of bacterial meningitis included tuberculous meningitis, were also excluded. If multiple publications reporting findings of the same study were retrieved, only the most recent or most complete publication for each data set for a specific outcome was selected. Reference lists of meta-analyses and systematic reviews were scanned to identify any missing articles that might be relevant. To reduce the risk of bias, studies with a small sample size (<50 subjects) were excluded to be more representative of the population; these were only included if data from large studies were not available for certain countries.
2.3 Data selection
Full-text articles were identified following a preliminary screening of titles and abstracts and were reviewed in detail. As a quality check, two independent researchers individually screened the same first 30% of titles and abstracts and assessed 10% of full-text articles, with a third researcher resolving any disagreements if required. During screening there was less than 5% discrepancy between the two researchers. For each selected article, two researchers extracted the following data to an Excel spreadsheet: study characteristics (country, design, study period, and setting), study population (case definition, exclusion criteria, sample size, age, and sex), and etiological agents.
2.4 Risk of bias assessment
A customized checklist based on the Critical Appraisal Skills Program (CASP) [18] and on criteria relevant to the designs of studies included in the systematic review was used to assess study quality/risk of bias. The checklist included eight questions that could be answered ‘yes’, ‘no’, or ‘cannot tell/not applicable’ and were given a weight of 10 or 15 points based on relevance (S2 Table). Each study was given an overall quality assessment score based on answers to the eight questions; 100 points were scored if all eight responses were positive. Overall study quality was categorized as ‘high’, ‘moderate’, or ‘low’ when studies received scores of ≥80 points, >50 to <80 points, or ≤50 points, respectively.
Data were stratified by six geographic regions in accordance with the World Health Organization (WHO) regional classification of Member States (African region, Region of the Americas, South-East Asian region, European region, Eastern Mediterranean region [including Israel], and Western Pacific region). [19] The data were also stratified by age categories: all ages, all children (<18 years), all adults, neonates (aged <1 month), children aged ±1 month–1 year, children aged ±1–5 years, children aged ±6–18 years, adults aged ±18–29 years, adults aged ±30–49 years, adults aged ±50–64 years, and elderly (±65 years). There was heterogeneity between the studies with regard to the age ranges used and therefore the authors were not too strict on the limits used in order to compare studies in children and adults.
2.5 Statistical analyses
Meta-analyses were performed for the frequency (percentages) of seven pathogens known to cause bacterial meningitis (E. coli, H. influenzae, N. meningitidis, S. pneumoniae, group B S. agalactiae, S. aureus, and L. monocytogenes). Analyses were performed if data stratified by pathogen, age, and region were available from at least three studies. Analyses were also performed on the frequency of the pathogens in the Northern American region (i.e. the USA and Canada), stratified by age and region to determine the impact that vaccine coverage may have. The frequency of the seven pathogens in the ‘all ages’ group was also analyzed, stratified by quality assessment score (low, moderate, or high). Additional analyses were carried out to stratify studies that investigated the frequency of group B S. agalactiae in neonates and in the ‘all ages’ group, ignoring the n≥3 studies criterion. The separate analyses of studies in the Northern American region and the frequency of the pathogens stratified by quality assessment score were carried out when more than two studies provided data for a pathogen.
To combine the study results, two approaches were used; the random-effects model was used for studies with moderate or high heterogeneity, and the fixed-effect model for those with low heterogeneity. [20–22] The inverse-variance method was used for the fixed-effect models to pool summary measures, [23] and the DerSimonian and Laird method for the random-effects models. [24–26] To prevent the exclusion of study estimates that were 0, the Freeman-Tukey transformation was used. [27, 28]
The level of heterogeneity was assessed by the Cochran’s Q test. Heterogeneity was quantified by the Higgins I2 test. [16] Heterogeneity was classed as low (I2 of 0–40%), moderate (30–60%), substantial (50–90%), or high (75–100%). [24, 29] P-values were obtained by comparing the statistic with the Chi2 distribution with k-1 degrees of freedom, with ≤0.10 considered the cut-off for statistically significant heterogeneity. [24] Statistical analyses were performed in STATA version 13.1 (College Station, Texas, USA).
2.6 Sensitivity analyses
Sensitivity analyses were performed to determine the origin of any differences between studies. Studies were omitted from the sensitivity analysis if they: reported results only on isolates or episodes instead of cases, were of low quality, reported on relatively small subgroups, or those with subgroups that excluded neonates in the ‘all ages’ and ‘all children’ groups. Sensitivity analyses were only performed when at least four studies per subgroup could be pooled after study exclusion.
3 Results and discussion
3.1 Study characteristics
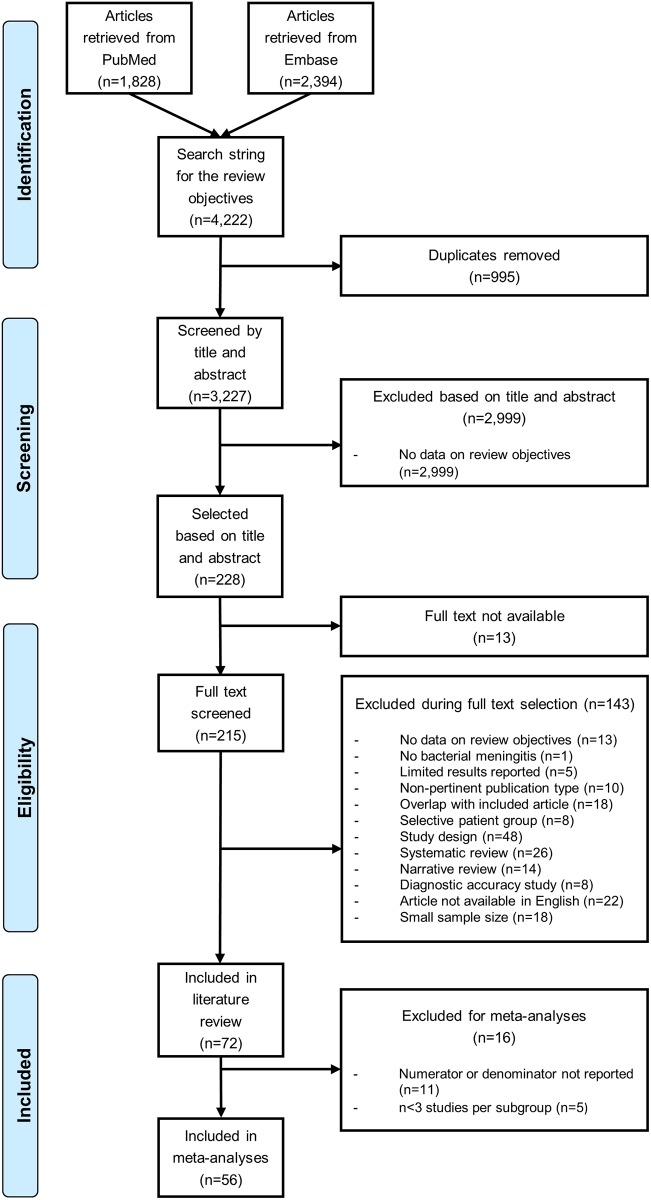
Out of a total of 3227 unique records screened, 72 studies reported data on the etiology of bacterial meningitis by age and region (Fig 1).
Fig 1. Flow chart for study inclusion.
Of the total 72 studies initially identified, 29 were in adults and children, 33 in only children, and 10 in only adults. Between 18 and 110,264 confirmed bacterial meningitis cases were observed in these 72 studies. Five studies of the 72 had a sample size <50 and were included because large studies were not available for those countries: Bosnia and Herzegovina, [30] Nepal, [31] Nigeria, [32] Romania, [33] and Tunisia. [34] The methodological quality assessment of each of the included studies is shown in S3 Table. Approximately 90% of these studies were cross-sectional studies (n = 49/72) or surveillance studies (n = 14/72). The majority of the studies received a ‘moderate’ quality assessment score (n = 40/72), mostly because the study populations were not representative of the source population, and overall quality assessment scores were generally comparable across geographic regions (Table 1). Ten studies received a ‘low’ quality assessment score due to insufficient case definitions and lack of adjustment for potential confounding factors, in addition to lack of representativeness of the study populations.
Table 1. Overall study quality assessment scores in each geographic region.
| Study quality score | |||
|---|---|---|---|
| Geographic region, n (%) | Low | Moderate | High |
| African region | 3 (16.7) | 11 (61.1) | 4 (22.2) |
| Region of the Americas | 1 (16.7) | 2 (33.3) | 3 (50.0) |
| South-East Asia region | 2 (40.0) | 2 (40.0) | 1 (20.0) |
| European region | 1 (5.6) | 11 (61.1) | 6 (33.3) |
| Eastern Mediterranean region | 2 (15.4) | 6 (46.2) | 5 (38.5) |
| Western Pacific region | 1 (8.3) | 8 (66.7) | 3 (25.0) |
| Overall | 10 (13.9) | 40 (55.6) | 22 (30.6) |
3.2 Etiology of bacterial meningitis
Of the 72 studies included in the literature review, 61 studies were eligible for the meta-analysis (11 studies were excluded because the numerator or denominator was missing; 5 studies were excluded as these presented limited data [≤3 studies per subgroup]), resulting in the final inclusion of 56 studies.
The meta-analysis of these studies showed that the most prevalent pathogens that caused bacterial meningitis were N. meningitidis, and S. pneumoniae; with weighted means for frequency across geographical regions and age groups ranging from 3.2–47.0%, and 9.6–75.2%, respectively. The range of weighted means for frequency of H. influenzae was 0.2–15.5% (Table 2, S4 Table). S. pneumoniae was the most frequently implicated cause of bacterial meningitis in the ‘all children’ and ‘all adults’ groups, with weighted means for frequency between 22.5–41.1% and 9.6–75.2%, respectively (Table 2).
Table 2. Overview of studies with data on percentages of pathogens that caused bacterial meningitis stratified by age group and region*.
| E. coli | H. influenzae | L. monocytogenes | N. meningitidis | S. aureus | Group B S. agalactiae | S. pneumoniae | |
|---|---|---|---|---|---|---|---|
| All ages | |||||||
| African region, n | 8 [35–42] | 10 [35–44] | 7 [35–41] | 10 [35–44] | 8 [35–42] | 7 [35–41] | 10 [35–44] |
| Weighted mean, % | 0.99 | 5.59 | 0.00 | 36.18 | 0.89 | 0.23 | 41.17 |
| (95% CI) | (0.00–3.18) | (3.50–8.09) | (0.00–0.11) | (26.58–46.36) | (0.00–2.85) | (0.00–1.17) | (34.10–48.43) |
| I2, % (p-value) | 94.9 (p<0.001) | 93.5 (p<0.001) | 36.4 (p = 0.15) | 98.7 (p<0.001) | 94.2 (p<0.001) | 88.0 (p<0.001) | 97.3 (p<0.001) |
| Eastern Mediterranean, n | 2 | 3 [45–47] | 2 | 4 [45–48] | 2 | 0 | 4 [45, 47–49] |
| Weighted mean, % | 6.41 | 9.09 | 25.13 | ||||
| (95% CI) | (0.29–19.02) | (6.19–13.17) | (14.23–37.91) | ||||
| I2, % (p-value) | NA | 99.3 (p<0.001) | 96.2 (p<0.001) | ||||
| Europe, n | 2 | 3 [50–52] | 3 [50–52] | 3 [50–52] | 3 [50–52] | 3 [50–52] | 3 [50–52] |
| Weighted mean, % | 2.36 | 1.63 | 36.18 | 4.36 | 1.93 | 27.0 | |
| (95% CI) | (0.88–4.43) | (0.58–3.10) | (17.91–56.78) | (0.25–12.33) | (0.00–6.14) | (7.93–52.06) | |
| I2, % (p-value) | NA | NA | NA | NA | NA | NA | |
| South-East Asia, n | 1 | 2 | 2 | 2 | 1 | 1 | 2 |
| The Americas, n | 0 | 4 [53–56] | 2 | 4 [53–56] | 0 | 0 | 4 [53–56] |
| Weighted mean, % | 7.84 | 26.94 | 26.23 | ||||
| (95% CI) | (3.84–13.09) | (22.57–31.54) | (8.21–50.12) | ||||
| I2, % (p-value) | 99.9 (p<0.001) | 99.6 (p<0.001) | 99.8 (p<0.001) | ||||
| Western Pacific, n | 1 | 2 | 1 | 2 | 0 | 0 | 2 |
| All children | |||||||
| African region, n | 4 [32, 39, 57, 58] | 4 [32, 39, 57, 58] | 4 [32, 39, 57, 58] | 4 [32, 39, 57, 58] | 4 [32, 39, 57, 58] | 4 [32, 39, 57, 58] | 5 [32, 39, 42, 57, 58] |
| Weighted mean, % | 2.45 | 13.14 | 0.00 | 7.46 | 2.00 | 2.93 | 41.06 |
| (95% CI) | (0.00–10.14) | (0.39–37.17) | (0.00–6.80) | (1.91–15.75) | (0.00–6.50) | (0.00–10.67) | (24.66–58.52) |
| I2, % (p-value) | 84.8 (p<0.001) | 95.3 (p<0.001) | 0.0 (p = 1.00) | 77.0 (p<0.001) | 67.1 (p = 0.03) | 83.8 (p<0.001) | 91.2 (p<0.001) |
| Eastern Mediterranean, n | 1 | 2 | 1 | 2 | 1 | 1 | 1 |
| Europe, n | 2 | 8 [30, 33, 52, 59–63] | 3 [30, 33, 52] | 9 [30, 33, 50, 52, 59–63] | 3 [30, 50, 52] | 5 [30, 33, 50, 52, 59] | 9 [30, 33, 50, 52, 59–63] |
| Weighted mean, % | 13.59 | 0.00 | 46.87 | 2.22 | 2.25 | 22.47 | |
| (95% CI) | (6.70–22.26) | (0.00–1.35) | (35.27–58.64) | (0.03–6.57) | (0.00–7.83) | (14.13–32.05) | |
| I2, % (p-value) | 93.9 (p<0.001) | NA | 97.3 (p<0.001) | NA | 94.2 (p<0.001) | 96.7 (p<0.001) | |
| South-East Asia, n | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| The Americas, n | 1 | 2 | 2 | 2 | 1 | 2 | 2 |
| Western Pacific, n | 5 [64–68] | 5 [64–68] | 2 | 5 [64–68] | 3 [64, 66, 69] | 5 [64–68] | 5 [64–68] |
| Weighted mean, % | 10.32 | 13.87 | 3.15 | 4.15 | 13.65 | 26.18 | |
| (95% CI) | (6.55–14.80) | (6.70–22.26) | (0.69–7.06) | (0.00–13.83) | (4.60–26.35) | (17.73–35.61) | |
| I2, % (p-value) | 74.0 (p<0.001) | 95.5 (p<0.001) | 84.9 (p<0.001) | NA | 95.5 (p<0.001) | 88.9 (p<0.001) | |
| All adults | |||||||
| African region, n | 2 | 2 | 2 | 2 | 2 | 2 | 3 [39, 42, 70] |
| Weighted mean, % | 75.18 | ||||||
| (95% CI) | (56.19–90.22) | ||||||
| I2, % (p-value) | NA | ||||||
| Eastern Mediterranean, n | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Europe, n | 6 [50, 71–75] | 5 [52, 71, 72, 74, 75] | 6 [52, 71–75] | 7 [50, 52, 71–75] | 7 [50, 52, 71–75] | 4 [52, 73–75] | 7 [50, 52, 71–75] |
| Weighted mean, % | 2.86 | 2.55 | 5.84 | 24.31 | 5.48 | 0.95 | 38.02 |
| (95% CI) | (1.08–5.38) | (1.08–5.38) | (3.24–9.07) | (15.30–34.61) | (1.06–12.55) | (0.49–1.52) | (17.09–61.55) |
| I2, % (p-value) | 93.2 (p<0.001) | 0.0 (p = 0.75) | 80.0 (p<0.001) | 97.9 (p<0.001) | 98.2 (p<0.001) | 0.0 (p = 0.94) | 99.6 (p<0.001) |
| South-East Asia, n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| The Americas, n | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Western Pacific, n | 3 [68, 76, 77] | 4 [68, 76–78] | 4 [68, 76–78] | 4 [68, 76–78] | 3 [76–78] | 3 [76–78] | 4 [68, 76–78] |
| Weighted mean, % | 1.82 | 0.20 | 1.10 | 4.59 | 12.16 | 1.28 | 9.55 |
| (95% CI) | (0.35–4.15) | (0.00–1.43) | (0.00–4.03) | (0.00–22.01) | (9.00–15.70) | (0.28–2.81) | (0.92–25.01) |
| I2, % (p-value) | NA | 55.3 (p = 0.08) | 78.7 (p<0.001) | 97.6 (p<0.001) | NA | NA | 96.0 (p<0.001) |
*Meta-analyses were only conducted only if there were ≥3 studies.
The frequencies of these pathogens in the other age groups; neonates, children aged ±1 month– 1 year, ±1–5 years, and ±6–18 years across geographical regions, are given in S4 Table.
n, number of studies; NA, not applicable
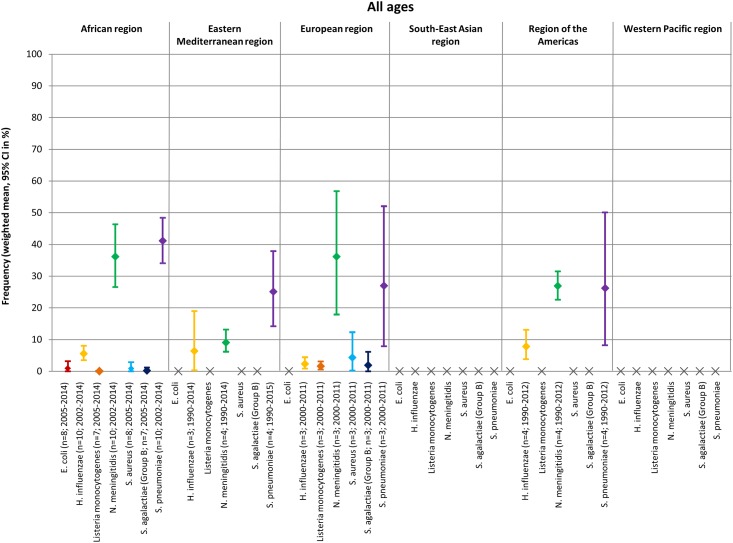
A visual depiction of the frequency of the seven pathogens that caused bacterial meningitis stratified by age group and geographic region is provided in Fig 2 and S1 Fig.
Fig 2. Frequency of seven pathogens that caused bacterial meningitis in all ages by geographic region.
The most common pathogens in the ‘all ages’ group, for most regions, were N. meningitidis and S. pneumoniae, with weighted means for frequency ranging from 9.1–36.2%, and from 25.1–41.2%, respectively (Fig 2); meta-analysis could not be performed for the South-east Asia or Western Pacific regions for ‘all ages’. Additional meta-analyses of two studies conducted in Northern America demonstrated that S. pneumoniae was the most common pathogen that caused bacterial meningitis in ‘all ages’, with a weighted mean of 43.1% (S5 Table; [55, 56]).
Data for meta-analyses of individual age groups by region (neonates, children aged ±1 month–1 year, aged ±1–5 years, aged ±6–18 years, adults aged ±18–29 years, aged ±30–49 years, aged ±50–64 years, and the elderly) was limited (S1 Fig). N. meningitidis was the most prevalent pathogen that caused bacterial meningitis in children aged ±1–5 years, and S. pneumoniae was the most prevalent pathogen in children aged ±6–18 years (S1 Fig). In neonates, E. coli and S. pneumoniae were the most common bacterial meningitis-causing pathogens (weighted means of 17.7% and 20.4%, respectively; S1 Fig); however, meta-analyses could only be performed in the African region. Due to the importance of investigating bacterial meningitis caused by group B S. agalactiae in neonates, additional analyses were performed for all regions and ignored the n ≥3 studies criterion for meta-analysis. The frequency of group B S. agalactiae in neonates was highest in Europe and lowest in the Eastern Mediterranean region, with weighted means of 58.2% and 4.9%, respectively (S6 Table), but frequency could not be determined in the region of the Americas.
When the prevalence of pathogens that caused bacterial meningitis in all ages was stratified by quality assessment score, N. meningitidis and S. pneumoniae remain the most prevalent pathogens in all geographic regions (data not shown).
3.3 Sensitivity analyses
Large heterogeneity was found between the included studies. However, most sensitivity analyses resulted in very small changes in the observed heterogeneity, indicating that these analyses did not point out specific causes for this. Clear sources of the observed heterogeneity were identified for a limited number of sensitivity analyses, although these sources did not appear to be consistent when compared with other sensitivity analyses on specific bacteria, even though the included studies were essentially the same. It is therefore unlikely that these sources of heterogeneity fully explain the observed heterogeneity between the included studies.
3.4 Discussion
To our knowledge, this is the first systematic review and meta-analysis of the frequency of key pathogens that cause bacterial meningitis across a wide variety of age groups and geographical regions. The present systematic review showed that N. meningitidis, S. pneumoniae, and H. influenzae were the predominant pathogens that caused bacterial meningitis in most ages within the majority of regions in studies published in the last five years.
In children aged ±6–18 years and neonates in all regions, S. pneumoniae was the predominant pathogen, and it remains an important cause of bacterial meningitis in regions with high vaccine coverage such as Northern America. [55, 56] N. meningitidis was the predominant pathogen for bacterial meningitis among children in the age group ±1–5 years in Europe. Previous studies have identified that in recent years serogroup B N. meningitidis is responsible for the majority of meningococcal disease in Europe, [79, 80] while serogroup C is the most common in the US. [80] The high frequency of bacterial meningitis cases due to N. meningitidis and S. pneumoniae come against the backdrop of the availability of vaccines for both pathogens. A decrease of ≥90% of invasive Hib disease was noted across industrialized countries following the introduction of Hib vaccination programs. [6] Administration of multiple pneumococcal conjugate vaccines resulted in a 66% reduction in the average annual rate of pneumococcal meningitis in children aged <2 years old, and a 33% reduction in adults aged ≥65 years old in the USA. [9, 10] Vaccines targeted against N. meningitidis serogroups A or C, or a tetravalent A, C, Y, and W135 vaccine have been incorporated into vaccine programs in many countries over recent years, and have led to a documented decrease in cases due to these serogroups. [11, 12] More recently a N. meningitidis serogroup B protein-based vaccine has been developed and use has been shown to limit outbreaks. [81, 82] Together these findings suggest that prevention strategies against these pathogens should be more robust, and the utilization of data on specific incidences in specific regions can help to formulate vaccination policies.
In our study, E.coli and S. pneumoniae were the most frequent pathogens that caused bacterial meningitis in neonates but this assumption was limited to meta-analyses in the African region. A retrospective analysis of bacterial meningitis in neonates and young infants between 2004 and 2014 contradicted this and found that group B S. agalactiae was the predominant pathogen, however, this was in a small population of 56 volunteers and retrospective analyses may have questionable validity. [83] An additional analysis was carried out in our study for data in neonates on the frequency of group B S. agalactiae for all regions and found that the frequency was highest in the European region (but limited to one study only [84]), and lowest in the Eastern Mediterranean region (based on two studies only [34, 85]). It has been estimated that group B S. agalactiae could cause between 114,000–204,000 invasive cases and 147,000 still births and infant deaths every year worldwide [86]. Neonatal mortality rates are estimated at 10–15% and 40–58% in developed and developing countries, respectively [87], and highlights the public health concern for group B S. agalactiae. There are no licensed vaccines against E. coli or group B S. agalactiae, despite these two pathogens being the major causes of bacterial meningitis in neonates. The availability of effective vaccines with a good tolerability profile is considered a strategic priority for the WHO to reduce the burden of invasive disease in neonates and young infants. [1, 88]
Significant heterogeneity was observed between the included studies. Sensitivity analyses omitting specific types of studies based on the types of data reported or based on study quality resulted in small changes in heterogeneity, and had little impact on the pooled estimates. It was not possible to identify the sources that fully explained the observed heterogeneity between the included studies. However, this was expected because most of the included studies were observational surveillance studies.
Our study successfully analyzed a large number of studies over a five year publication timeframe, giving a comprehensive overview of the current status of the pathogens causing bacterial meningitis worldwide. Although the search was limited to articles published in the last five years, the study periods in the included studies often covered a longer period than 2012–2017. In addition, the studies analyzed had certain limitations which might have impacted this meta-analysis. There were a small number of studies available for sub-analysis, with limited data available for some pathogens in different age groups, such as group B S. agalactiae, L. monocytogenes, E. coli, and S. aureus, highlighting the need for greater surveillance. Some studies only focused on the three most common pathogens (H. influenzae, N. meningitidis, and S. pneumoniae), while others only presented the frequency of the most common or important etiologic agent within their study population and combined the other etiologic agents in the ‘other’ category. More than half of the studies were conducted at a single institution, with a study population that may not be representative. As only studies that were published in English were included, this may have caused language bias and missed relevant studies, and may also have resulted in under-representation of the regions in our study. Some of the studies used surveillance data (n = 14/72), which is frequently incomplete and subject to systematic and random errors. Studies that provided data for specific subgroups were sometimes too small, thus meta-analyses could not be performed for all subgroups. The frequency of N. meningitidis and S. pneumoniae in all ages may be underrepresented as limited countries within the Meningitis Belt were included in this analysis. Finally, the criteria for the methodological quality assessment as well as the overall quality assessment score were customized by the authors and have not been validated.
4 Conclusions
This systematic review and meta-analysis demonstrated notable differences in the frequency of bacterial meningitis pathogens in a wide range of age groups across geographic regions in studies published in the last five years. Further studies are required to monitor bacterial meningitis cases and facilitate the further development of prevention and treatment strategies worldwide.
Supporting information
(DOC)
Only analyses for frequency of pathogens in neonates, children aged ±1–5 and ±6–18 years are shown. No data were obtained in children aged ±1 month–1 year.
(PDF)
(DOCX)
(DOCX)
CSF, cerebrospinal fluid; IQR, interquartile range; LAT, latex agglutination test; NA, not applicable; NR, not reported; PCR, polymerase chain reaction; SD, standard deviation.
(DOCX)
*The frequency of pathogens in age groups that were not presented in Table 2.
(DOCX)
n, number of studies; NA, not applicable; NR, not reported.
(DOCX)
n, number of studies; NA, not applicable.
(DOCX)
Acknowledgments
Professional medical writing assistance was provided by Jonathon Ackroyd, inScience Communications, London, UK which was funded by Sanofi Pasteur Inc., Swiftwater, Pennsylvania, USA. Bret Wing, PhD of Sanofi Pasteur provided editorial assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was conducted by Pallas Health Research and Consultancy, Rotterdam, The Netherlands under contract and funded by Sanofi Pasteur Inc., Swiftwater, Pennsylvania, USA. The funder provided support in the form of salaries for authors [AB, MHK], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.World Health Organization (WHO). Meningococcal meningitis: Fact sheet 2017 [updated December 2017; cited 2017 November 9]. http://www.who.int/mediacentre/factsheets/fs141/en/.
- 2.Thigpen MC, Whitney CG, Messonnier NE, Zell ER, Lynfield R, Hadler JL, et al. Bacterial meningitis in the United States, 1998–2007. The New England journal of medicine. 2011;364(21):2016–25. Epub 2011/05/27. doi: 10.1056/NEJMoa1005384 . [DOI] [PubMed] [Google Scholar]
- 3.Brouwer MC, Tunkel AR, van de Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clinical microbiology reviews. 2010;23(3):467–92. Epub 2010/07/09. doi: 10.1128/CMR.00070-09 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO). Number of suspected meningitis cases and deaths reported, 2010 epidemiological season 2017 [cited 2017 November 9]. http://www.who.int/gho/epidemic_diseases/meningitis/suspected_cases_deaths_text/en/.
- 5.Centers for Disease Control and Prevention (CDC). Bacterial Meningitis 2017 [updated January 25, 2017]. https://www.cdc.gov/meningitis/bacterial.html.
- 6.World Health Organization (WHO). Haemophilus influenzae type b (Hib) Vaccination Position Paper—July 2013. Releve epidemiologique hebdomadaire. 2013;88(39):413–26. Epub 2013/10/23. . [PubMed] [Google Scholar]
- 7.Hamborsky J, Kroger A, Wolfe C, editors. Centers for Disease Control and Prevention: Epidemiology and Prevention of Vaccine-Preventable Diseases. 13th ed Washington D.C.: Public Health Foundation; 2015. [Google Scholar]
- 8.Davis S, Feikin D, HL J. The effect of Haemophilus influenzae type B and pneumococcal conjugate vaccines on childhood meningitis mortality: a systematic review. BMC Public Health. 2013;13(Suppl 3):S21 doi: 10.1186/1471-2458-13-S3-S21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai CJ, Griffin MR, Nuorti JP, Grijalva CG. Changing epidemiology of pneumococcal meningitis after the introduction of pneumococcal conjugate vaccine in the United States. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;46(11):1664–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tin Tin Htar M, Madhava H, Balmer P, Christopoulou D, Menegas D, Bonnet E. A review of the impact of pneumococcal polysaccharide conjugate vaccine (7-valent) on pneumococcal meningitis. Adv Ther. 2013;30(8):748–62. doi: 10.1007/s12325-013-0051-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin NG, Sadarangani M, Pollard AJ, Goldacre MJ. Hospital admission rates for meningitis and septicaemia caused by Haemophilus influenzae, Neisseria meningitidis, and Streptococcus pneumoniae in children in England over five decades: a population-based observational study. The Lancet Infectious Diseases. 14(5):397–405. doi: 10.1016/S1473-3099(14)70027-1 [DOI] [PubMed] [Google Scholar]
- 12.Cohn AC, MacNeil JR, Harrison LH, Hatcher C, Theodore J, Schmidt M, et al. Changes in Neisseria meningitidis disease epidemiology in the United States, 1998–2007: implications for prevention of meningococcal disease. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2010;50(2):184–91. Epub 2009/12/17. doi: 10.1086/649209 . [DOI] [PubMed] [Google Scholar]
- 13.Heath PT. Status of vaccine research and development of vaccines for GBS. Vaccine. 2016;34(26):2876–9. doi: 10.1016/j.vaccine.2015.12.072 [DOI] [PubMed] [Google Scholar]
- 14.Poolman JT, Wacker M. Extraintestinal Pathogenic Escherichia coli, a Common Human Pathogen: Challenges for Vaccine Development and Progress in the Field. J Infect Dis. 2016;213(1):6–13. doi: 10.1093/infdis/jiv429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lieberman JM, Greenberg DP, Ward JI. Prevention of bacterial meningitis. Vaccines and chemoprophylaxis. Infect Dis Clin North Am. 1990;4(4):703–29. [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. London, United Kingdom: Cochrane Collaboration; 2011. [Google Scholar]
- 17.PRISMA. PRISMA Checklist [14 December 2017]. http://prisma-statement.org/.
- 18.CASP UK. CASP Checklists Oxford, United Kingdom: CASP UK; 2017. http://www.casp-uk.net/casp-tools-checklists.
- 19.World Health Organization (WHO). WHO regional offices. 2017 [10 May 2018]. http://www.who.int/about/regions/en/.
- 20.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–45. doi: 10.1016/j.cct.2015.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. Epub 2010/04/01. doi: 10.1002/jrsm.12 . [DOI] [PubMed] [Google Scholar]
- 22.Harris R, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. Metan: fixed- and random-effects meta-analysis. The Stata Journal. 2008;8(1):3–28. [Google Scholar]
- 23.Lee CH, Cook S, Lee JS, Han B. Comparison of Two Meta-Analysis Methods: Inverse-Variance-Weighted Average and Weighted Sum of Z-Scores. Genomics Inform. 2016;14(4):173–80. doi: 10.5808/GI.2016.14.4.173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deeks J HJ, and Altman D. Chapter 9: Analysing data and undertaking meta-anlysis In: Higgins JPT G S, editor. Cochrane Handbook for Systematic Reviews of Interventions Version 501: The Cochrane Collaboration; Updated September 2008. [Google Scholar]
- 25.Borenstein M, Hedges L., and Rothstein H. Introduction to meta-analysis. 2007. [Google Scholar]
- 26.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974–8. doi: 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 27.Freeman MF, Tukey JW. Transformations Related to the Angular and the Square Root. Ann Math Statist. 1950;21(4):607–11. doi: 10.1214/aoms/1177729756 [Google Scholar]
- 28.StataCorp. Stata Statistical Software: Release 13. 2013, TX: StataCorp LP: College Station. [Google Scholar]
- 29.Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. Epub 2006/06/21. doi: 10.1037/1082-989X.11.2.193 . [DOI] [PubMed] [Google Scholar]
- 30.Porobic-Jahic H, Piljic D, Jahic R, Ahmetagic S, Numanovic F. Etiology of bacterial meningitis in children in Tuzla Canton. Medical archives (Sarajevo, Bosnia and Herzegovina). 2013;67(1):13–6. Epub 2013/05/18. . [DOI] [PubMed] [Google Scholar]
- 31.Shrestha RG, Tandukar S, Ansari S, Subedi A, Shrestha A, Poudel R, et al. Bacterial meningitis in children under 15 years of age in Nepal. BMC pediatrics. 2015;15:94 Epub 2015/08/20. doi: 10.1186/s12887-015-0416-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nwadioha SI, Nwokedi EO, Onwuezube I, Egesie JO, Kashibu E. Bacterial isolates from cerebrospinal fluid of children with suspected acute meningitis in a Nigerian tertiary hospital. The Nigerian postgraduate medical journal. 2013;20(1):9–13. Epub 2013/05/11. . [PubMed] [Google Scholar]
- 33.Juganariu G, Miftode E, Teodor D, Leca D, Dorobat CM. Clinical features and course of bacterial meningitis in children. Revista medico-chirurgicala a Societatii de Medici si Naturalisti din Iasi. 2012;116(3):722–6. Epub 2013/01/01. . [PubMed] [Google Scholar]
- 34.Kamoun F, Dowlut MB, Ameur SB, Sfaihi L, Mezghani S, Chabchoub I, et al. Neonatal purulent meningitis in southern Tunisia: Epidemiology, bacteriology, risk factors and prognosis. Fetal and pediatric pathology. 2015;34(4):233–40. Epub 2015/06/18. doi: 10.3109/15513815.2015.1051252 . [DOI] [PubMed] [Google Scholar]
- 35.Ky-Ba A, Sanou M, Tranchot JD, Christiasen PA, Ouedraogo AS, Tamboura M, et al. Dynamics of germs responsible for acute bacterial meningitis in Burkina faso in the last ten years (2005–2014). African Journal of Clinical and Experimental Microbiology. 2016;17(1):10–7. doi: 10.4314/ajcem.v17i1.2 [Google Scholar]
- 36.Massenet D, Birguel J, Azowe F, Ebong C, Gake B, Lombart JP, et al. Epidemiologic pattern of meningococcal meningitis in northern Cameroon in 2007–2010: contribution of PCR-enhanced surveillance. Pathogens and global health. 2013;107(1):15–20. Epub 2013/02/26. doi: 10.1179/2047773212Y.0000000070 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tegene B, Gebreselassie S, Fikrie N. Bacterial Meningitis: a five-year retrospective study among patients who had attended at University of Gondar Teaching Hospital, Northwest Ethiopia. Biomedical Research and Therapy. 2015;2(5). doi: 10.7603/s40730-015-0012-2 [Google Scholar]
- 38.Nuoh RD, Nyarko KM, Nortey P, Sackey SO, Lwanga NC, Ameme DK, et al. Review of meningitis surveillance data, upper West Region, Ghana 2009–2013. The Pan African medical journal. 2016;25(Suppl 1):9 Epub 2017/02/18. doi: 10.11604/pamj.supp.2016.25.1.6180 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Owusu M, Nguah SB, Boaitey YA, Badu-Boateng E, Abubakr AR, Lartey RA, et al. Aetiological agents of cerebrospinal meningitis: a retrospective study from a teaching hospital in Ghana. Annals of clinical microbiology and antimicrobials. 2012;11:28 Epub 2012/10/06. doi: 10.1186/1476-0711-11-28 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mengistu A, Gaeseb J, Uaaka G, Ndjavera C, Kambyambya K, Indongo L, et al. Antimicrobial sensitivity patterns of cerebrospinal fluid (CSF) isolates in Namibia: implications for empirical antibiotic treatment of meningitis. Journal of pharmaceutical policy and practice. 2013;6:4 Epub 2013/01/01. doi: 10.1186/2052-3211-6-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karou SD, Balaka A, Bamoke M, Tchelougou D, Assih M, Anani K, et al. Epidemiology and antibiotic resistance of bacterial meningitis in Dapaong, northern Togo. Asian Pacific journal of tropical medicine. 2012;5(11):848–52. Epub 2012/11/14. doi: 10.1016/S1995-7645(12)60158-8 . [DOI] [PubMed] [Google Scholar]
- 42.Tall H, Njanpop-Lafourcade BM, Mounkoro D, Tidjani L, Agbenoko K, Alassani I, et al. Identification of Streptococcus suis Meningitis through Population-Based Surveillance, Togo, 2010–2014. Emerging infectious diseases. 2016;22(7):1262–4. Epub 2016/06/18. doi: 10.3201/eid2207.151511 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Storz C, Schutz C, Tluway A, Matuja W, Schmutzhard E, Winkler AS. Clinical findings and management of patients with meningitis with an emphasis on Haemophilus influenzae meningitis in rural Tanzania. Journal of the neurological sciences. 2016;366:52–8. Epub 2016/06/12. doi: 10.1016/j.jns.2016.04.044 . [DOI] [PubMed] [Google Scholar]
- 44.Kambire D, Soeters HM, Ouedraogo-Traore R, Medah I, Sangare L, Yameogo I, et al. Nationwide Trends in Bacterial Meningitis before the Introduction of 13-Valent Pneumococcal Conjugate Vaccine-Burkina Faso, 2011–2013. PloS one. 2016;11(11):e0166384 Epub 2016/11/11. doi: 10.1371/journal.pone.0166384 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saeed N, AlAnsari H, AlKhawaja S, Jawad JS, Nasser K, AlYousef E. Trend of bacterial meningitis in Bahrain from 1990 to 2013 and effect of introduction of new vaccines. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2016;22(3):175–82. Epub 2016/06/24. . [DOI] [PubMed] [Google Scholar]
- 46.Motamedifar M, Ebrahim-Saraie HS, Mansury D, Nikokar I, Hashemizadeh Z. Prevalence of etiological agents and antimicrobial resistance patterns of bacterial meningitis in Nemazee Hospital, Shiraz, Iran. Archives of Clinical Infectious Diseases. 2015;10(2). doi: 10.5812/archcid.22703 [Google Scholar]
- 47.Teleb N, Pilishvili T, Van Beneden C, Ghoneim A, Amjad K, Mostafa A, et al. Bacterial meningitis surveillance in the Eastern Mediterranean region, 2005–2010: successes and challenges of a regional network. The Journal of pediatrics. 2013;163(1 Suppl):S25–31. Epub 2013/06/21. doi: 10.1016/j.jpeds.2013.03.027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rezaeizadeh G, Pourakbari B, Ashtiani MH, Asgari F, Mahmoudi S, Mamishi S. Antimicrobial susceptibility of bacteria isolated from cerebrospinal fluids in an Iranian referral pediatric center, 1998–2008. Maedica. 2012;7(2):131–7. Epub 2013/02/13. . [PMC free article] [PubMed] [Google Scholar]
- 49.Abdelkader MM, Aboshanab KM, El-Ashry MA, Aboulwafa MM. Prevalence of MDR pathogens of bacterial meningitis in Egypt and new synergistic antibiotic combinations. PloS one. 2017;12(2):e0171349 Epub 2017/02/17. doi: 10.1371/journal.pone.0171349 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Okike IO, Ribeiro S, Ramsay ME, Heath PT, Sharland M, Ladhani SN. Trends in bacterial, mycobacterial, and fungal meningitis in England and Wales 2004–11: an observational study. The Lancet Infectious diseases. 2014;14(4):301–7. Epub 2014/02/11. doi: 10.1016/S1473-3099(13)70332-3 . [DOI] [PubMed] [Google Scholar]
- 51.Bretonniere C, Jozwiak M, Girault C, Beuret P, Trouillet JL, Anguel N, et al. Rifampin use in acute community-acquired meningitis in intensive care units: the French retrospective cohort ACAM-ICU study. Critical care (London, England). 2015;19:303 Epub 2015/08/27. doi: 10.1186/s13054-015-1021-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Namani SA, Koci RA, Qehaja-Bucaj E, Ajazaj-Berisha L, Mehmeti M. The epidemiology of bacterial meningitis in Kosovo. Journal of infection in developing countries. 2014;8(7):823–30. Epub 2014/07/16. doi: 10.3855/jidc.3553 . [DOI] [PubMed] [Google Scholar]
- 53.Azevedo LC, Toscano CM, Bierrenbach AL. Bacterial Meningitis in Brazil: Baseline Epidemiologic Assessment of the Decade Prior to the Introduction of Pneumococcal and Meningococcal Vaccines. PloS one. 2013;8(6):e64524 Epub 2013/07/05. doi: 10.1371/journal.pone.0064524 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saraiva M, Santos EC, Saraceni V, Rocha LL, Monte RL, Albuquerque BC, et al. Epidemiology of infectious meningitis in the State of Amazonas, Brazil. Revista da Sociedade Brasileira de Medicina Tropical. 2015;48 Suppl 1:79–86. Epub 2015/06/11. doi: 10.1590/0037-8682-0116-2014 . [DOI] [PubMed] [Google Scholar]
- 55.Castelblanco RL, Lee M, Hasbun R. Epidemiology of bacterial meningitis in the USA from 1997 to 2010: a population-based observational study. The Lancet Infectious diseases. 2014;14(9):813–9. Epub 2014/08/12. doi: 10.1016/S1473-3099(14)70805-9 . [DOI] [PubMed] [Google Scholar]
- 56.Gounder PP, Zulz T, Desai S, Stenz F, Rudolph K, Tsang R, et al. Epidemiology of bacterial meningitis in the North American Arctic, 2000–2010. The Journal of infection. 2015;71(2):179–87. Epub 2015/04/14. doi: 10.1016/j.jinf.2015.04.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kuti BP, Bello EO, Jegede TO, Olubosede O. Epidemiological, clinical and prognostic profile of childhood acute bacterial meningitis in a resource poor setting. Journal of neurosciences in rural practice. 2015;6(4):549–57. Epub 2016/01/12. doi: 10.4103/0976-3147.165424 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wolzak NK, Cooke ML, Orth H, van Toorn R. The changing profile of pediatric meningitis at a referral centre in Cape Town, South Africa. Journal of tropical pediatrics. 2012;58(6):491–5. Epub 2012/07/14. doi: 10.1093/tropej/fms031 . [DOI] [PubMed] [Google Scholar]
- 59.Snaebjarnardottir K, Erlendsdottir H, Reynisson IK, Kristinsson K, Halldorsdottir S, Hardardottir H, et al. Bacterial meningitis in children in Iceland, 1975–2010: a nationwide epidemiological study. Scandinavian journal of infectious diseases. 2013;45(11):819–24. Epub 2013/08/24. doi: 10.3109/00365548.2013.817680 . [DOI] [PubMed] [Google Scholar]
- 60.Ciofi degli Atti M, Esposito S, Parola L, Rava L, Gargantini G, Longhi R. In-hospital management of children with bacterial meningitis in Italy. Italian journal of pediatrics. 2014;40:87 Epub 2015/01/15. doi: 10.1186/s13052-014-0087-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ceyhan M, Gurler N, Ozsurekci Y, Keser M, Aycan AE, Gurbuz V, et al. Meningitis caused by Neisseria Meningitidis, Hemophilus Influenzae Type B and Streptococcus Pneumoniae during 2005–2012 in Turkey. A multicenter prospective surveillance study. Human vaccines & immunotherapeutics. 2014;10(9):2706–12. Epub 2014/12/09. doi: 10.4161/hv.29678 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ceyhan M, Ozsurekci Y, Gurler N, Karadag Oncel E, Camcioglu Y, Salman N, et al. Bacterial agents causing meningitis during 2013–2014 in Turkey: A multi-center hospital-based prospective surveillance study. Human vaccines & immunotherapeutics. 2016;12(11):2940–5. Epub 2016/07/28. doi: 10.1080/21645515.2016.1209278 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Toprak D, Soysal A, Torunoglu MA, Turgut M, Turkoglu S, Pimenta FC, et al. PCR-based national bacterial meningitis surveillance in Turkey: years 2006 to 2009. The Pediatric infectious disease journal. 2014;33(10):1087–9. Epub 2014/11/02. doi: 10.1097/INF.0000000000000378 . [DOI] [PubMed] [Google Scholar]
- 64.Guo LY, Zhang ZX, Wang X, Zhang PP, Shi W, Yao KH, et al. Clinical and pathogenic analysis of 507 children with bacterial meningitis in Beijing, 2010–2014. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases. 2016;50:38–43. Epub 2016/07/28. doi: 10.1016/j.ijid.2016.07.010 . [DOI] [PubMed] [Google Scholar]
- 65.Shinjoh M, Iwata S, Yagihashi T, Sato Y, Akita H, Takahashi T, et al. Recent trends in pediatric bacterial meningitis in Japan—a country where Haemophilus influenzae type b and Streptococcus pneumoniae conjugated vaccines have just been introduced. Journal of infection and chemotherapy: official journal of the Japan Society of Chemotherapy. 2014;20(8):477–83. Epub 2014/05/27. doi: 10.1016/j.jiac.2014.04.007 . [DOI] [PubMed] [Google Scholar]
- 66.Wee LY, Tanugroho RR, Thoon KC, Chong CY, Choong CT, Krishnamoorthy S, et al. A 15-year retrospective analysis of prognostic factors in childhood bacterial meningitis. Acta paediatrica (Oslo, Norway: 1992). 2016;105(1):e22–9. Epub 2015/10/02. doi: 10.1111/apa.13228 . [DOI] [PubMed] [Google Scholar]
- 67.Lin MC, Chiu NC, Chi H, Ho CS, Huang FY. Evolving trends of neonatal and childhood bacterial meningitis in northern Taiwan. Journal of microbiology, immunology, and infection = Wei mian yu gan ran za zhi. 2015;48(3):296–301. Epub 2013/11/05. doi: 10.1016/j.jmii.2013.08.012 . [DOI] [PubMed] [Google Scholar]
- 68.Ho Dang Trung N, Le Thi Phuong T, Wolbers M, Nguyen Van Minh H, Nguyen Thanh V, Van MP, et al. Aetiologies of central nervous system infection in Viet Nam: a prospective provincial hospital-based descriptive surveillance study. PloS one. 2012;7(5):e37825 Epub 2012/06/05. doi: 10.1371/journal.pone.0037825 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Basri R, Zueter AR, Mohamed Z, Alam MK, Norsa’adah B, Hasan SA, et al. Burden of bacterial meningitis: a retrospective review on laboratory parameters and factors associated with death in meningitis, kelantan malaysia. Nagoya journal of medical science. 2015;77(1–2):59–68. Epub 2015/03/24. . [PMC free article] [PubMed] [Google Scholar]
- 70.Britz E, Perovic O, von Mollendorf C, von Gottberg A, Iyaloo S, Quan V, et al. The Epidemiology of Meningitis among Adults in a South African Province with a High HIV Prevalence, 2009–2012. PloS one. 2016;11(9):e0163036 Epub 2016/09/27. doi: 10.1371/journal.pone.0163036 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bodilsen J, Dalager-Pedersen M, Schonheyder HC, Nielsen H. Time to antibiotic therapy and outcome in bacterial meningitis: a Danish population-based cohort study. BMC infectious diseases. 2016;16:392 Epub 2016/08/11. doi: 10.1186/s12879-016-1711-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lummel N, Koch M, Klein M, Pfister HW, Bruckmann H, Linn J. Spectrum and Prevalence of Pathological Intracranial Magnetic Resonance Imaging Findings in Acute Bacterial Meningitis. Clinical neuroradiology. 2016;26(2):159–67. Epub 2014/09/24. doi: 10.1007/s00062-014-0339-x . [DOI] [PubMed] [Google Scholar]
- 73.Thornorethardottir A, Erlendsdottir H, Sigurethardottir B, Harethardottir H, Reynisson IK, Gottfreethsson M, et al. Bacterial meningitis in adults in Iceland, 1995–2010. Scandinavian journal of infectious diseases. 2014;46(5):354–60. Epub 2014/02/27. doi: 10.3109/00365548.2014.880184 . [DOI] [PubMed] [Google Scholar]
- 74.Domingo P, Pomar V, de Benito N, Coll P. The spectrum of acute bacterial meningitis in elderly patients. BMC infectious diseases. 2013;13:108 Epub 2013/03/01. doi: 10.1186/1471-2334-13-108 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bijlsma MW, Brouwer MC, Kasanmoentalib ES, Kloek AT, Lucas MJ, Tanck MW, et al. Community-acquired bacterial meningitis in adults in the Netherlands, 2006–14: a prospective cohort study. The Lancet Infectious diseases. 2016;16(3):339–47. Epub 2015/12/15. doi: 10.1016/S1473-3099(15)00430-2 . [DOI] [PubMed] [Google Scholar]
- 76.McBride S, Fulke J, Giles H, Hobbs M, Suh J, Sathyendran V, et al. Epidemiology and diagnostic testing for meningitis in adults as the meningococcal epidemic declined at Middlemore Hospital. The New Zealand medical journal. 2015;128(1410):17–24. Epub 2015/04/02. . [PubMed] [Google Scholar]
- 77.Lien CY, Huang CR, Tsai WC, Hsu CW, Tsai NW, Chang CC, et al. Epidemiologic trend of adult bacterial meningitis in southern Taiwan (2006–2015). Journal of clinical neuroscience: official journal of the Neurosurgical Society of Australasia. 2017. Epub 2017/03/28. doi: 10.1016/j.jocn.2017.03.017 . [DOI] [PubMed] [Google Scholar]
- 78.Kim HI, Kim SW, Park GY, Kwon EG, Kim HH, Jeong JY, et al. The causes and treatment outcomes of 91 patients with adult nosocomial meningitis. The Korean journal of internal medicine. 2012;27(2):171–9. Epub 2012/06/19. doi: 10.3904/kjim.2012.27.2.171 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Whittaker R, Dias JG, Ramliden M, Kodmon C, Economopoulou A, Beer N, et al. The epidemiology of invasive meningococcal disease in EU/EEA countries, 2004–2014. Vaccine. 2017;35(16):2034–41. doi: 10.1016/j.vaccine.2017.03.007 [DOI] [PubMed] [Google Scholar]
- 80.Pelton SI. The Global Evolution of Meningococcal Epidemiology Following the Introduction of Meningococcal Vaccines. J Adolesc Health. 2016;59(2 Suppl):S3–S11. Epub 2016/07/28. [DOI] [PubMed] [Google Scholar]
- 81.Toneatto D, Pizza M, Masignani V, Rappuoli R. Emerging experience with meningococcal serogroup B protein vaccines. Expert Rev Vaccines. 2017;16(5):433–51. doi: 10.1080/14760584.2017.1308828 [DOI] [PubMed] [Google Scholar]
- 82.McNamara LA, Thomas JD, MacNeil J, Chang HY, Day M, Fisher E, et al. Meningococcal Carriage Following a Vaccination Campaign With MenB-4C and MenB-FHbp in Response to a University Serogroup B Meningococcal Disease Outbreak-Oregon, 2015–2016. J Infect Dis. 2017;216(9):1130–40. doi: 10.1093/infdis/jix446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kotzbauer D, Travers C, Shapiro C, Charbonnet M, Cooley A, Andresen D, et al. Etiology and Laboratory Abnormalities in Bacterial Meningitis in Neonates and Young Infants. Clin Pract. 2017;7(2):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Okike IO, Johnson AP, Henderson KL, Blackburn RM, Muller-Pebody B, Ladhani SN, et al. Incidence, etiology, and outcome of bacterial meningitis in infants aged <90 days in the United kingdom and Republic of Ireland: prospective, enhanced, national population-based surveillance. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2014;59(10):e150–7. Epub 2014/07/06. doi: 10.1093/cid/ciu514 . [DOI] [PubMed] [Google Scholar]
- 85.Ergaz Z, Benenson S, Cohen MJ, Braunstein R, Bar-Oz B. No change in antibiotic susceptibility patterns in the neonatal ICU over two decades. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2013;14(2):164–70. Epub 2012/12/21. doi: 10.1097/PCC.0b013e31824fbc19 . [DOI] [PubMed] [Google Scholar]
- 86.Seale AC, Bianchi-Jassir F, Russell NJ, Kohli-Lynch M, Tann CJ, Hall J, et al. Estimates of the Burden of Group B Streptococcal Disease Worldwide for Pregnant Women, Stillbirths, and Children. Clinical Infectious Diseases. 2017;65(suppl_2):S200–S19. doi: 10.1093/cid/cix664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ku LC, Boggess KA, Cohen-Wolkowiez M. Bacterial meningitis in infants. Clin Perinatol. 2015;42(1):29–45. doi: 10.1016/j.clp.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.World Health Organization (WHO). Meningococcal A conjugate vaccine: updated guidance, February 2015. 2015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Only analyses for frequency of pathogens in neonates, children aged ±1–5 and ±6–18 years are shown. No data were obtained in children aged ±1 month–1 year.
(PDF)
(DOCX)
(DOCX)
CSF, cerebrospinal fluid; IQR, interquartile range; LAT, latex agglutination test; NA, not applicable; NR, not reported; PCR, polymerase chain reaction; SD, standard deviation.
(DOCX)
*The frequency of pathogens in age groups that were not presented in Table 2.
(DOCX)
n, number of studies; NA, not applicable; NR, not reported.
(DOCX)
n, number of studies; NA, not applicable.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.