Abstract
The purpose of this study was to determine the efficacy of fluoride varnish (5% sodium fluoride, Duraphat®, Colgate) in reverting white spot lesions (WSLs) after fixed orthodontic treatment. This study was a randomized, parallel group, controlled clinical trial. Using saline solution as control, 110 participants (mean age ± standard deviation: 16.6±3.2 years) ranging from 12 to 22 years old were randomly assigned to either the test group (group 1) or the control group (group 2). Application of fluoride varnish or saline was applied onto tooth surfaces with WSLs every month during the first 6 months after debonding. The labial (buccal) surfaces of the teeth were assessed by the use of a DIAGNOdent pen (DD) at the baseline, 3- and 6-month follow-up visits. After 6 months, 96 subjects with a total of 209 study teeth (47 subjects, 104 teeth in group 1; 49 subjects, 105 teeth in group 2) remained. The WSLs had a mean DD reading at baseline of 17.66±5.36 in group 1 and 16.19±5.70 in group 2, which decreased by 5.78 and 2.44, respectively, at the 3-month follow-up visit and decreased by 7.56 and 3.09, respectively, at the 6-month follow-up visit. The mean baseline DD readings in the two groups were similar (t test, P>0.05). There was statistically significant differences between the mean DD readings of the two groups at the 3-month (P<0.05) and at the 6-month follow-up visits (P<0.01). Topical fluoride varnish application is effective in reversing WSLs after debonding and should be advocated as a routine caries prevention measure after orthodontic treatment.
Keywords: White spot lesion, Orthodontic treatment, Enamel demineralization, Fluoride varnish, DIAGNOdent pen
Introduction
Enamel demineralization or early caries appearing as white spot lesions (WSLs) is a risk factor associated with development of carious cavity which may happened during and even after fixed orthodontic treatment [1, 2]. Directly bonded orthodontic brackets and bands are applied extensively for treatment of malocclusion, but this has led to the prevalent lack or absence of optimal oral hygiene [3]. WSL has been defined as a “subsurface enamel porosity from carious demineralization” that presents itself as “a milky white opacity when located on smooth surfaces” [4]. In orthodontic patients, WSLs are usually present around the periphery of the bracket base, under loose bands, and in areas that are both difficult to access by toothbrush and cannot be detected easily by patients [5]. The incidence of WSLs following orthodontic treatment varies largely from 4.9% [2] to 85% [6] of tooth surfaces. An increase in WSLs in more than 50% of patients with fixed orthodontic therapy has been reported [2, 7, 8]. In a study conducted in China, it was found that 59.4% of 165 debonded patients had one or more orthodontic-related carious lesions, and 12.5% of tooth surfaces in average were affected with WSLs after orthodontic bracket bonding [9]. In general, orthodontic patients had significantly higher incidence of WSLs compared with non-orthodontic patients, and even presented aesthetic problems years after treatment [10]. WSLs may progress into carious cavities when there is a lack of appropriate oral hygiene or remineralization treatment.
The aim of modern dentistry is focused on a prophylactic approach, instead of invasive restoration, of carious defects. Fluoride is the most important agent preventing demineralization, as well as against the development and progression of carious lesions [11–13]. Apart from fluoridated toothpaste, other methods of delivering fluoride to teeth in non-orthodontic patients include mouthrinses [14], gels [15], varnishes [16], and combinations of topical fluorides [17]. Numerous clinical trials have been conducted on the remineralization of WSLs during orthodontic treatment. Information on fluoride treatment for WSLs after orthodontic therapy is relatively scant. Ogaard [18] stated that initial caries induced by orthodontic treatment can be reversed by utilizing fluoride-containing products at posttreatment.
The extensive use of fluoride varnishes has been associated with caries decline in many European countries [19–22]. A recent study concluded that fluoride varnish could be considered an efficient preventive method to enhance enamel resistance against cariogenic challenges during orthodontic therapy [23]. The findings demonstrate that significant calcium fluoride-like material (CaF2) deposition acts as a reaction product of fluoride varnish when applied adjacent to orthodontic brackets. Furthermore, the study reported that the application of fluoride varnish is even more beneficial for less compliant patients compared with those resorting to fluoride mouth rinse on a daily basis.
The aim of this study was to assess the efficacy of regular topical fluoride varnish applications in reverting WSLs after fixed orthodontic treatment. The null hypothesis to be tested was that there was no difference in the change in status of the WSLs over a 6-month period between subjects who had received applications of a 5% sodium fluoride varnish and those who had not.
Subjects and methods
Ethics
Approval from the ethics committee of the School of Dentistry of the Wuhan University, People’s Republic of China was obtained prior to the start of this study.
Trial design and participants
This study was a randomized, parallel-group, controlled clinical trial on newly debonded orthodontic patients. Patients with a fixed appliance who were being treated at the Orthodontics Department of the Dental Hospital of Wuhan University from June to August 2008 were recruited.
Sample size calculations were based on detecting a difference of 30% reduction in DIAGNOdent pen (DD) reading between the test group and the control group using a two-tailed significance level of 5% with an 80% power. Eligible participants were individuals from both genders, with ages ranging from 12 to 22 years old, in good general health and without systemic diseases, who had received conventional periodontal therapy after fixed orthodontic treatment and with at least two teeth with WSLs. Patients with enamel hypoplasia, dental fluorosis or tetracycline pigmentation, periodontal pocket (≥3 mm), taking antibiotics, and carious cavity were excluded. These aimed at avoiding false-positive results. In accordance with the above mentioned criteria, 110 out of 117 orthodontic patients with WSLs in labial (buccal) tooth surfaces were recruited for this clinical study. The study took place at the Preventive Dentistry Department of the Dental Hospital of Wuhan University in Wuhan, China.
Recruitment and randomization
Using a random number table, the participants were assigned to either the test group (group 1) and received topical application of a 5% sodium fluoride (22,600 mg/L F−) varnish (Duraphat, Colgate Oral Pharmaceuticals, USA), or the placebo group (group 2) who received saline solution. Randomization was performed by a researcher not involved in the study. The patients or their parents from the two groups were informed by letter of the purpose, design, and procedures of the study. Informed written consent was obtained from the patients or their parents prior to study implementation. Applications of the fluoride varnish or saline solution were given to the participants by one trained dentist every month during the first 6 months after debonding. Subjects who missed one or more visits were regarded as dropout.
Intervention
Participants in group 1 (Duraphat; n=55) were treated as follows. Firstly, the subject’s teeth were cleaned with a toothbrush, especially the surfaces with WSLs. Secondly, excessive saliva in one or two quadrants of the mouth was removed by cotton rolls or by using an air syringe. It was not necessary to keep the tooth surface extremely dry because Duraphat could set in the presence of saliva. Thirdly, fluoride varnish was applied onto the tooth surfaces with WSLs using a miniature cotton swab or brush, with the applicator dabbed repeatedly onto the tooth surface without contacting soft tissues. After a few minutes, a thin and clear layer is formed. Then the next quadrants were treated in the same manner.
Participants in group 2 (saline solution; n=55) were treated following the same steps as those in group 1.
Patients in both groups were advised not to brush their teeth or chew food for at least 4 h after treatment; during this time, soft food and liquid might be consumed. No supplemental measure was taken to remove plaque from tooth surfaces, such as using dental floss and mouth rinse. Only standard tooth cleaning and oral hygiene instruction (tooth brushing twice a day with fluoride toothpaste) was provided in the visit in which the orthodontic brackets were debonded.
Measurements
Status of the WSLs were assessed using a DIAGNOdent pen (KaVo, Biberach, Germany) which had been shown to have similar reliability and validity as the conventional DIAGNOdent laser-induced fluorescence detection device when quantifying changes in carious lesion in teeth [24]. In the present study, assessment of the WSLs took place at baseline, at 3 and 6 months after debonding. All teeth were cleaned and dried by air syringe before using the DIAGNOdent pen under cotton roll isolation. The device was calibrated according to the manufacturer’s instructions before every assessment. The assessments in all visits were carried out by the same dentist who was blind as to group allocation of the subjects. The whole labial (buccal) surface of the tooth with a WSL was scanned. While scanning a tooth, the wand was rocked slowly in a pendulous motion using probe tip B. This ensured that the tip would pick up fluorescence from the margin of the WSL where the carious process often began. The peak reading displayed on the panel of the DIAGNOdent pen during the scan was recorded for each tooth surface.
Statistical analysis
The DD readings were subjected to statistical analysis and compared between groups at different time points (baseline, 3 and 6 months) and between groups at each time point using repeated measures one-way ANOVA (α=0.05). A two-tail Student’s t test was also used for detecting intergroup difference (α=0.05). Data were processed by the statistical software SPSS (ver. 13.0).
Results
Enrollment and retention
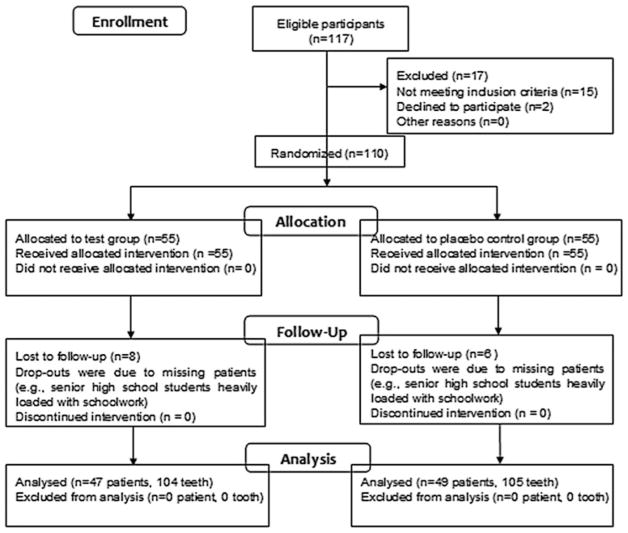
Of the 110 participants recruited, 14 dropped out between the debonding and the six-month recall visit. A total of 47 participants in group 1 (14 males; 33 females) completed the study. In group 2, 49 participants (17 males; 32 females) finished the study. The loss-to-follow-up percentages were 14.5% and 10.9% for the group 1 and group 2, respectively, which were not statistically significant (P=0.51). The dropouts were mainly due to some non-compliant patients (e.g., senior high school students heavily loaded with schoolwork) (see Fig. 1). The mean age of participants was 16.6±3.2 years, ranging from 12 to 22 years. All patients were treated by straight wire fixed orthodontic technique using a non-fluoride bonding agent (3M UniteK, Transbond XT, USA), with 17.8±5.6 months as the mean bonding period.
Fig. 1.
CONSORT flow diagram of participants through the randomized trial
Clinical outcomes
In the 96 remaining subjects (47 in group 1, 49 in group 2), a total of 209 tooth surfaces with WSL were evaluated. The WSLs had a mean DD reading at baseline of 17.66±5.36 in group 1 and 16.19±5.70 in group 2, which decreased by 5.78 and 2.44, respectively, at the 3-month follow-up visit and decreased by 7.56 and 3.09, respectively, at the 6-month follow-up visit. The mean baseline DD readings in the two groups were similar (t test, P>0.05). There were statistically significant differences between the mean DD readings of the two groups at the 3-month (P<0.05) and at the 6-month follow-up visits (P<0.01) (Table 1).
Table 1.
Comparison of scores by DD (x ± SD) between group 1 and group 2 at any two-point measurements, and comparison of scores between any two-point measurements in two groups
| DIAGNOdent pen scores (mean ± SD)
|
P value | ||
|---|---|---|---|
| Group 1 (n=47) | Group 2 (n=49) | ||
| Baseline | 17.66±5.36a | 16.19±5.70c | 0.196 |
| 3 months | 11.88±4.27b | 13.75±4.76d | 0.046 |
| 6 months | 10.10±4.86b | 13.10±5.19d | 0.004 |
Two-tail Student t test intergroup difference was found after 3 months (P=0.046) and 6 months (P=0.004) debonding
Repeated measures one-way ANOVA intragroup difference was found at two-point measurements marked by different alphabet. Group 1: baseline vs. 3 months (P=9.402×10−7 ), baseline vs. 6 months (P=3.794×10−10 ), 3 months vs. 6 months (P=0.0513). Group 2: baseline vs. 3 months (P=0.024), baseline vs. 6 months (P=0.006), 3 months vs. 6 months (P=0.536). No statistical difference was found between two groups
Table 1 also shows comparisons of the DD readings within each group at each time point. There was a significant decrease in the mean DD reading in group 1 during the first 3 months (P<0.001) and a further decrease after 6 months (repeated measures ANOVA P<0.001) compared to baseline. However, the decrease in mean DD reading between the third and the 6 months were not statistically significant (P>0.05). Similar findings were obtained in group 2.
Adverse events
No adverse response or safety concerns in the use of Duraphat were reported by any of the subjects.
Discussion
This study was a randomized, parallel-group, controlled clinical trial which followed changes of WSLs in debonded tooth surfaces after monthly application of a 5% NaF varnish over a period of 6 months. The tooth surfaces with WSLs of the subjects were assessed by a DIAGNOdent pen, and the readings which estimated the organic content and bacterial metabolites in enamel caries lesions were used to indicate the changes of the WSLs after fluoride varnish application [25]. The positive results found in this study may be due to the high sensitivity and acceptable specificity of DIAGNOdent in detecting changes in early caries lesions. Shi et al. [26] reported that DIAGNOdent had acceptable sensitivity (75%) and high specificity (96%) (i.e., correlation of 0.85) for their enamel depth analysis in smooth surface caries, as compared with quantitative light-induced fluorescence. Similarly, high sensitivity and acceptable specificity were also observed in other studies, such as those by Rocha et al. [27] and Anttonen et al. [28]. The greater decrease in DD readings for the WSLs in group 1 compared to that of group 2 may be taken to indicate a larger reversal of the early caries process due to the repeated fluoride varnish application. Longer observation is recommended to confirm whether the greater change in WSLs is maintained.
Gwinnett et al. [29] showed that fixed orthodontic appliances induced a rapid increase in the volume of dental plaque. The composition of the bacterial flora of plaques shifts rapidly after introducing orthodontic appliances. Scheie et al. [30] observed significantly elevated plaque and salivary levels of acidogenic bacteria, such as Streptococcus mutans and lactobacilli in orthodontic patients. The low pH of plaques adjacent to the orthodontic appliances and areas without optimal oral hygiene favors caries development; thus, decalcification of enamel and even carious cavity occurs. Moreover, because of low concentrations of calcium, phosphate, and fluoride in the saliva, natural remineralization after orthodontic treatment is difficult to achieve. Thus, intervention is needed to promote reversal of the caries process in the enamel lesions.
Fluoride varnishes have been proven to be safe and feasible in topical application. They contain high concentrations of fluoride compared with the daily used tooth-pastes and mouth rinse. The varnish can remain on tooth surfaces for several hours after application, and release sufficiently high level of fluoride ion to maintain surface fluoridation [31]. Based on the results of a recent study, it appears that the application of a fluoride varnish can help to reduce WSLs occurring adjacent to orthodontic appliances. Apart from minimal clinical chair time, it eliminates the need for patient compliance, enables better control of fluoride exposure, and can be accomplished by a trained hygienist.
Numerous studies have been conducted on prevention of WSLs during orthodontic treatments. Stecksén-Blicks et al. [32] evaluated the efficacy of topical fluoride vanish (Fluor Protector, containing 1,000 ppm F−) applications on WSL formation in adolescents during fixed orthodontic treatment. The results showed the incidence of WSL was 7.4% in the fluoride varnish compared to 25.3% in the placebo group (P<0.001), and the mean progression score was significantly lower in the fluoride varnish group than in the placebo group (P<0.001). An in vivo study conducted by Nasrin et al. [33] revealed an approximately 40% reduction in depth of demineralization around brackets after application of high concentration fluoride varnish (Bifluorid 12, 6% calcium fluoride, and 6% sodium fluoride). Vivaldi-Rodrigues et al. [34] examined the effectiveness of fluoride varnish in reducing enamel demineralization during 12 months of orthodontic treatment, which showed a significantly smaller change in mean enamel decalcification index for the experimental group (0.34) compared to the control group (0.51).
Fluoride varnishes are widely available in the USA. Among these, Duraphat was the first to be approved by the FDA in 1994 [22]. Numerous clinical trials have been conducted to examine the efficacy of Duraphat in preventing dental caries. Helfenstein and Steinen [35] after conducting a meta-analysis on the results of eight clinical studies concluded that caries incidence could be decreased by 38% if Duraphat is used at 6-month intervals. Enamel decalcifications in the form of WSLs resulting from use of orthodontic appliance have become problematic from the prospective of aesthetics. If the appropriate oral hygiene or remineralization measures are not implemented on time, WSLs may progress into carious cavitations. However, up to now, information on fluoride treatment for extant caries after orthodontic therapy remains relatively scant.
The distinct advantages of Duraphat are as follows: regardless of its high fluoride concentration, rapid setting time can be performed once upon contact with saliva, hence preventing risk of ingestion. Moreover, only a small dosage is used, and less the use of a tray, thus shortening the amount of clinical chair time and maximizing application safety [36].
The dropout rate in this study is relatively higher than desirable, due to some non-compliant patients (e.g., senior high school students heavily loaded with schoolwork). A total of 14 patients dropped out during the first 6 months of treatment. DIAGNOdent could only detect depth of lesions, but the amount of lesion areas is impossible to test. Due to lack of other form of fluoride or non-fluoride-containing varnish, we used a saline solution in the control arm instead. More well-designed clinical trials are necessary for further studies on the 5% NaF varnish and related testing on enamel lesion reduction, particularly, with the use of DIAGNOdent pen. Longer periods of follow-up are necessary.
Conclusions
The efficacy of repeated applications of a 5% NaF varnish in reducing WSLs after orthodontic treatment was investigated in this randomized controlled clinical trial. A greater decrease in DIAGNOdent pen readings was found in the test group during the first 6 months after debonding. This may be taken to imply an improvement in the WSLs. Thus, topical fluoride varnish application appears to be a good method to treat WSLs and should be advocated as a routine measure after orthodontic treatment.
Acknowledgments
The study was supported by the 11th five-year plan of Chinese Science and Technology R&D Program (No: 2007BA118B01) and the Dental Hospital of Wuhan University (China). The authors wish to thank Dr. Xiong Hui who offered great help to make this study possible.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest. The authors alone are responsible for the performance and evaluation of the clinical study, as well as for the writing and content of this paper.
Contributor Information
Minquan Du, Department of Preventive Dentistry, School & Hospital of Stomatology, Wuhan University, 237 Luoyu Road, Wuhan, China 430079.
Ning Cheng, Department of Preventive Dentistry, School & Hospital of Stomatology, Wuhan University, 237 Luoyu Road, Wuhan, China 430079.
Baojun Tai, Department of Preventive Dentistry, School & Hospital of Stomatology, Wuhan University, 237 Luoyu Road, Wuhan, China 430079.
Han Jiang, Department of Preventive Dentistry, School & Hospital of Stomatology, Wuhan University, 237 Luoyu Road, Wuhan, China 430079.
Jing Li, Department of Preventive Dentistry, School & Hospital of Stomatology, Wuhan University, 237 Luoyu Road, Wuhan, China 430079.
Zhuan Bian, Key Laboratory of Oral Biomedicine Ministry of Education, Wuhan University, Wuhan, China.
References
- 1.O’Reilly MM, Featherstone JDB. Decalcification and remineralization around orthodontic appliances: an in vivo study. Am J Orthod Dentofacial Orthop. 1985;92(1):33–40. doi: 10.1016/0889-5406(87)90293-9. [DOI] [PubMed] [Google Scholar]
- 2.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 3.Zachrisson BU. A posttreatment evaluation of direct bonding in orthodontics. Am J Orthod Dentofacial Orthop. 1977;71:173–189. doi: 10.1016/s0002-9416(77)90394-3. [DOI] [PubMed] [Google Scholar]
- 4.Summitt JB, Robbins JW, Schwartz RS. Fundamentals of operative dentistry: a contemporary approach. 3. Quintessence; Illinois: 2006. pp. 2–4. [Google Scholar]
- 5.Samir E. White spot lesions: formation, prevention, and treatment. Semin Orthod. 2008;14:174–182. [Google Scholar]
- 6.Mitchell L. Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod. 1992;19:199–205. doi: 10.1179/bjo.19.3.199. [DOI] [PubMed] [Google Scholar]
- 7.Mizrahi E. Surface distribution of enamel opacities following orthodontic treatment. Am J Orthod. 1983;84:323–331. doi: 10.1016/s0002-9416(83)90348-2. [DOI] [PubMed] [Google Scholar]
- 8.Artun J, Brobakken BO. Prevalence of carious white spots after orthodontic treatment with multibonded appliances. Eur J Orthod. 1986;8:229–234. doi: 10.1093/ejo/8.4.229. [DOI] [PubMed] [Google Scholar]
- 9.Wei H, Qing W, Mingkui F, Yiyue X, Zhuoyue C. An evaluation of enamel decalcification in orthodontic treatment with fixed appliance. Chinese Journal of Orthodontics. 2001;8:51–54. [Google Scholar]
- 10.Ogaard B. Prevalence of white spot lesions in 19-year-olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–427. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 11.Schmit JL, Staley RN, Wefel JS, Kanellis M, Jakobsen JR, Keenan PJ. Effect of fluoride varnish on demineralization adjacent to brackets bonded with RMGI cement. Am J Orthod Dentofacial Orthop. 2002;122:125–134. doi: 10.1067/mod.2002.126595. [DOI] [PubMed] [Google Scholar]
- 12.American Dental Association Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. J Am Dent Assoc. 2006;137:1151–1159. doi: 10.14219/jada.archive.2006.0356. [DOI] [PubMed] [Google Scholar]
- 13.Trairatvorakul C, Kladkaew S, Songsiripradabboon S. Active management of incipient caries and choice of materials. J Dent Res. 2008;87:228–232. doi: 10.1177/154405910808700301. [DOI] [PubMed] [Google Scholar]
- 14.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews. 2003:CD002284. doi: 10.1002/14651858.CD002284. [DOI] [PubMed] [Google Scholar]
- 15.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews. 2002:CD002280. doi: 10.1002/14651858.CD002280. [DOI] [PubMed] [Google Scholar]
- 16.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews. 2002:CD002279. doi: 10.1002/14651858.CD002279. [DOI] [PubMed] [Google Scholar]
- 17.Marinho VC, Higgins JP, Sheiham A, Logan S. Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews. 2004:CD002781. doi: 10.1002/14651858.CD002781.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogaard B, Larsson E, Henriksson T, Birkhed D, Bishara SE. Effects of combined application of antimicrobial and fluoride varnishes in orthodontic patients. Am J Orthod Dentofacial Orthop. 2001;120:28–35. doi: 10.1067/mod.2001.114644. [DOI] [PubMed] [Google Scholar]
- 19.Einarsdottir KG, Bratthall D. Restoring oral health: on the rise and fall of dental caries in Iceland. Eur J Oral Sci. 1996;104:459–469. doi: 10.1111/j.1600-0722.1996.tb00113.x. [DOI] [PubMed] [Google Scholar]
- 20.Splieth C, Meyer G. Factors for changes of caries prevalence among adolescents in Germany. Eur J Oral Sci. 1996;104:441–451. doi: 10.1111/j.1600-0722.1996.tb00111.x. [DOI] [PubMed] [Google Scholar]
- 21.Seppä L. Studies of fluoride varnishes in Finland. Proc Finn Dent Soc. 1991;87:541–547. [PubMed] [Google Scholar]
- 22.Beltrán-Aguilar ED, Goldstein JW, Lockwood SA. Fluoride varnishes: a review of their clinical use, cariostatic mechanism, efficacy and safety. J Am Dent Assoc. 2000;131:589–596. doi: 10.14219/jada.archive.2000.0232. [DOI] [PubMed] [Google Scholar]
- 23.Gontijo L, de Cruz RA, Brandão PR. Dental enamel around fixed orthodontic appliances after fluoride varnish application. Braz Dent J. 2007;18:49–53. doi: 10.1590/s0103-64402007000100011. [DOI] [PubMed] [Google Scholar]
- 24.De Benedetto MS, Morais CC, Novaes TF, de Almeida RJ, Braga MM, Mendes FM. Comparing the reliability of a new fluorescence camera with conventional laser fluorescence devices in detecting caries lesions in occlusal and smooth surfaces of primary teeth. Lasers Med Sci. 2010;26(2):157–162. doi: 10.1007/s10103-010-0757-1. [DOI] [PubMed] [Google Scholar]
- 25.Astvaldsdóttir A, Tranæus S, Karlsson L, Peter Holbrook W. DIAGNOdent measurements of cultures of selected oral bacteria and demineralized enamel. Acta Odontol Scand. 2011 doi: 10.3109/00016350903567176. (in press) [DOI] [PubMed] [Google Scholar]
- 26.Shi XQ, Tranaeus S, Angmar-Månsson B. Comparison of QLF and DIAGNOdent for quantification of smooth surface caries. Caries Res. 2001;35:21–26. doi: 10.1159/000047426. [DOI] [PubMed] [Google Scholar]
- 27.Rocha RO, Ardengi TM, Oliveria LB, Rodrigues CR, Ciamponi AL. In vivo effectiveness of laser fluorescence compared to visual inspection and radiography for the detection of occlusal caries in primary teeth. Caries Res. 2003;37:437–441. doi: 10.1159/000073396. [DOI] [PubMed] [Google Scholar]
- 28.Anttonen V, Seppa L, Hausen H. Clinical study of the use of the laser fluorescence device DIAGNOdent for detection of occlusal caries in children. Caries Res. 2003;37:17–23. doi: 10.1159/000068227. [DOI] [PubMed] [Google Scholar]
- 29.Gwinnett AJ, Ceen RF. Plaque distribution on bonded brackets: a scanning microscope study. Am J Orthod. 1979;75:67–77. doi: 10.1016/0002-9416(79)90098-8. [DOI] [PubMed] [Google Scholar]
- 30.Scheie AA, Arneberg P, Krogstad O. Effect of orthodontic treatment on prevalence of Streptococcus mutans in plaque and saliva. Scand J Dent Res. 1984;92:211–217. doi: 10.1111/j.1600-0722.1984.tb00881.x. [DOI] [PubMed] [Google Scholar]
- 31.Seppä L. Effect of dental plaque on fluoride uptake by enamel from a sodium fluoride varnish in vivo. Caries Res. 1983;17:71–75. doi: 10.1159/000260651. [DOI] [PubMed] [Google Scholar]
- 32.Stecksén-Blicks C, Renfors G, Oscarson ND, Bergstrand F, Twetman S. Caries-preventive effectiveness of a fluoride varnish: a randomized controlled trial in adolescents with fixed orthodontic appliances. Caries Res. 2007;41(6):455–459. doi: 10.1159/000107932. [DOI] [PubMed] [Google Scholar]
- 33.Farhadian N, Miresmaeili A, Eslami B, Mehrabi S. Effect of fluoride varnish on enamel demineralization around brackets: an in-vivo study. Am J Orthod Dentofacial Orthop. 2008;133:S95–98. doi: 10.1016/j.ajodo.2006.09.050. [DOI] [PubMed] [Google Scholar]
- 34.Vivaldi-Rodrigues G, Demito CF, Bowman SJ, Ramos AL. The effectiveness of a fluoride varnish in preventing the development of white spot lesions. World J Orthod. 2006;7(2):138–144. [PubMed] [Google Scholar]
- 35.Helfenstein U, Steiner M. Fluoride varnishes (Duraphat): a meta-analysis. Community Dent Oral Epidemiol. 1994;22:1–5. doi: 10.1111/j.1600-0528.1994.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 36.Warren DP, Henson HA, Chan JT. Dental hygienist and patient comparisons of fluoride gels. J Dent Hyg. 2000;74:94–101. [PubMed] [Google Scholar]