Abstract
Background
Perinatally HIV-exposed but uninfected (HEU) children have elevated risk of late language emergence at age 1 year, with possible links to in utero antiretroviral (ARV) exposure. We investigated possible risks for speech impairments (SI) and language impairments (LI) in preschool monolingual HEU children in the United States.
Methods
Speech and language assessments were conducted as part of the PHACS Surveillance Monitoring of ART Toxicities (SMARTT) study at ages 3 (N= 208) and 5 (N = 429) years. Domains of speech, overall language, vocabulary and grammar were assessed. SI and LI were defined by standardized scores (SCs) <15th percentile and categorized as primary (normal nonverbal IQ ≥ 85 without hearing loss) and concomitant (low nonverbal IQ and/or presence of hearing loss). Logistic regression models were used to estimate odds of SI and LI for different ARV exposures, adjusted for confounding variables.
Results
The risk for language impairments in HEU children was higher than population norms; risk for speech impairments was not elevated. Risk factors for impairments included male sex, black race, and other socioeconomic measures, although these varied by age, primary (P) vs. concomitant (C) impairment, and by speech or language measure. Adjusted logistic regression models revealed lower as well as increased risk for specific ARVs. Tenofovir exposure was associated with increased risk for SI at age 3 but was associated with decreased risk for CLI at age 5.
Conclusions
Further investigation of cARV exposure and speech/language impairment among pre-school children is needed to confirm associations.
Keywords: HIV-exposed children, antiretroviral, cohort study, language delay, speech delay
Background
Studies of school-aged children with perinatal HIV infection (PHIV) find that they are at elevated risk for language impairments1–4. However, perinatally HIV-exposed and uninfected (HEU) children show similar risk to PHIV children, suggesting factors other than HIV infection may play a role4. Our interest in this study was evaluating whether there may be longer-term adverse effects of perinatal combination ARV (cARV) exposure on speech and language functioning in HEU youth. Studies of early language abilities in HEU children at 1 and 2 years5,6 indicated elevated rates of late language emergence (LLE), 26% at 1 year and 23% at 2 years5, and found that in utero exposure to atazanavir, one of the antiretroviral (ARV) drugs commonly taken by HIV-infected pregnant women, was associated with an increased risk of LLE.
Further study into the causes of elevated risks for language impairment among PHIV and HEU children are needed. Studies are available for infants and for school age children, leaving the preschool period as a gap in our overall understanding. Furthermore, speech development and impairment are not well documented in previous studies. The neuro-motor requirements for speech production are different from those for language development, and the two impairments are relatively independent of each other among 6-year olds in the general population7. Although speech development is essential for intelligibility of communication, there are no reports of speech evaluation in PHIV and HEU preschool-aged children, the developmental period during which speech skills are mastered and a rich linguistic system is established for subsequent academic endeavors. Further, more information is needed regarding individual linguistic dimensions of language acquisition. By early school age, children’s emerging language systems include clearly differentiated dimensions of vocabulary and grammar. Growth in grammar is an especially sensitive index of risk for children with language impairments8. In short, the preschool period warrants targeted investigation of children exposed to ARVs in utero to identify potential risks for language impairment.
Our earlier study4 of school-aged children found that predictors of language impairments for PHIV and HEU children differed based on whether they also had concomitant disorders of cognitive and/or hearing impairment (Concomitant Language Impairment, CLI) as compared to children without these concomitant disorders (Primary Language Impairment, PLI). Population estimates of PLI are approximately 7% of kindergarten children without other neurological disorders; an additional 3% show low levels of language ability with low levels of cognitive ability9,10. Differences in predictive relationships between PLI and CLI groups of PHIV and HEU children suggest that the causal pathways for language impairment may involve language-selective pathways or more general pathways that also affect hearing or cognitive development. Evidence is needed for preschool children with PLI versus CLI to evaluate if predictors of speech and language development differ for the groups earlier in development. Such evidence would be relevant to ongoing concerns regarding possible longer-term effects of in utero ARV exposure, including previously observed associations of specific ARV drugs with risk of language impairment for HEU children11–13.
The specific aims of the current study are to determine among pre-school HEU children: 1) The prevalence of Primary Speech or Language Impairment (PSI/PLI; 2) the prevalence of speech and/or language impairment concomitant with intellectual or hearing impairment (CSI/CLI); and 3) whether risks for speech and/or language impairment are associated with in utero ARV exposures at the level of individual medications, controlling for potential confounders such as demographic and caregiver characteristics and considering infant birth characteristics. Information about the period of speech and language development could inform our understanding of risk for impairment in HEU school-age children and would inform clinical decisions for effective treatment.
Materials and Methods
Participants
This investigation used data collected in the Surveillance Monitoring of ART Toxicities (SMARTT) study, a prospective cohort study conducted by the Pediatric HIV/AIDS Cohort Study (PHACS) network at 22 sites in the United States including Puerto Rico. SMARTT is designed to identify toxicities potentially related to in utero ARV exposures through ongoing follow-up of HEU infants and children11. The study protocol was approved by institutional review boards at participating sites and the Harvard T.H. Chan School of Public Health, and written informed consent was obtained from each child’s parent/legal guardian. Beginning in 2007, women and their newborns or children were enrolled11. Speech and language assessments are conducted at specific ages, as described below.
Outcome Measures
Speech and Language Assessments
Outcomes were age-appropriate speech and language assessments intended to capture individual differences in children’s abilities relative to age expectations. Multiple indicators of speech and language were included to capture speech development, general language ability collapsed across linguistic dimensions (characterized as “language quotient score”), and dimensions of language (vocabulary and grammar). The assessments meet psychometric standards for language assessment validated across racial and ethnic groups, if administered in a child’s native language. For this reason, participants were restricted to monolingual English or Spanish-speaking children, given that all assessments were available in English and some assessments were available in Spanish. Cut-off criteria for speech or language impairment are consistent with widely used levels in research mostly based on standardized scores (SCs)8,9,14,15. These SCs have either population norms of mean=100 and SD=15 or mean=10 and SD=3, and impairment is defined as scores more than 1 SD below the population mean. Thus, depending on the measure, the cut-off levels were a standard score of 85 or below, or a percentile score below 15 which is very close to one SD below the mean in a normal distribution. These criteria may not align with cut-off criteria for clinical services, which vary across settings and are often influenced by availability of resources. Although impairments at this level may be considered “mild” the criteria encompasses the full range that could be enrolled in clinical services and it is also well established that children are not likely to “outgrow” such language impairmentst15. For the purpose of a safety study, our intent is to capture all forms of “impairment.”
At 3 years of age, speech was measured by the Goldman Fristoe Test of Articulation (GFTA-2)16 with impairment defined as a percentile score below 15. Language was measured using the Test of Early Language Development (TELD-3)17 as a general measure of overall language development, with the spoken language quotient as the derived score. Impairment was defined as a SC below 85. A second language test measured vocabulary, the Peabody Picture Vocabulary Test (PPVT-3)18, with impairment defined as a SC below 85. At 5 years of age, speech was measured with the GFTA-2, and speech impairment was again defined as a percentile score below 15. Three measures of language were obtained with the Test of Language Development (TOLD-P:3)19. An omnibus language development index was the spoken language quotient score, an overall measure from the test. In addition, two subtests were of interest: A measure of vocabulary was obtained with the picture vocabulary subtest and a measure of grammar came from the grammatic completion subtest. The definition of impairment for the spoken language quotient score was a SC of 85 or below; for the vocabulary and grammar subtests, impairment was defined as SC below 7 (one SD below the mean). The same criteria for impairment were followed for the parallel assessments in English and Spanish.
For all of the assessments, a child was considered monolingual if a questionnaire administered to the caregiver reported no language exposures beyond their primary language either in the home or outside the home. The TELD-3 and PPVT-3 were available in English and Spanish; the remaining assessments were only available in English. To avoid bias, only monolingual children assessed in the child’s language were included in the analysis.
Concomitant impairment was defined with the additional criteria of either low levels of nonverbal cognitive ability or hearing acuity, or both, using cut-off scores widely used in research9,15,20–22 with the intent to be sensitive to risk for broad causal pathways for speech or language impairment. Nonverbal intellectual impairment was defined as a classification on the Bayley Screener23 cognitive domain as “at risk” at 3 years of age, and a Wechsler Preschool and Primary Scale of Intelligence (WPPSI-III)24 Performance IQ score below 85 at 5 years of age21 placing them in the range of “mild” to “severely delayed”21. At ages 3 and 5, concomitant hearing impairment was defined as the worse ear pure tone average of thresholds at 0.5, 1, 2, and 4 kHz ≥ 20 dB hearing level (HL) based on the audiometric examination22. Audiometric examinations were considered for children at age 3 (or age 5) if they were completed within one year of the third (or the fifth) birthday. Before October 2010, audiometric assessments were performed when a child was considered language impaired according to the trigger design of SMARTT11. After October 2010, all children were required to have an audiometric examination at age 5 in addition to the triggered assessment. In this analysis, if a child had speech or language impairment but lacked an audiometric examination, the child was assumed to lack concomitant hearing impairment. It is noted that this assumption may underestimate the number of children with Concomitant Impairment among the speech/language impaired children.
ARV Exposures
In utero exposures to combination ARV (cARV), ARV drug classes and individual ARV agents were considered. Maternal ARV history during pregnancy was collected through medical record review and from prior studies. Maternal cARV use was defined as use of at least 3 drugs from at least 2 different ARV drug classes during pregnancy. The sample was restricted to those with exposure to in utero cARV or a triple nucleoside/nucleotide analog reverse transcriptase inhibitor (NRTI) regime to control for possible confounding by indication. This restriction excluded 7% of monolingual participants with any language/speech assessments. The two classes of ARVs we evaluated for associations with LI or SI in this analysis included non-nucleoside reverse transcriptase inhibitors (NNRTIs) and protease inhibitors (PIs). We did not include other more recently used classes such as fusion inhibitors, integrase inhibitors and CCR5 inhibitors due to very rare usage during pregnancy. We evaluated risk for individual drugs for which at least 5% of the study sample was exposed. We recognize that the drugs are not administered randomly with preferences among clinicians as well as characteristics of the mother and child likely to play a role in choices, and that conclusions about individual drugs are suggestive, not definitive, when administered as part of a combination regimen. As a safety study, we are interested in indications of any associations that bear further investigation.
Possible Confounders
Possible confounders considered were based on previous studies4,5, and included child, maternal, and household characteristics. The child demographic characteristics were: age at assessment, sex, race (either black race or other), and ethnicity (either Hispanic ethnicity or other), and in school (preschool/kindergarten/grade 1 or not in school). Maternal substance use during pregnancy included alcohol, tobacco, and illicit drugs. Maternal health measures during pregnancy included earliest and latest viral load during pregnancy (>400 vs ≤400 copies/mL), earliest and latest CD4% during pregnancy (<25% vs ≥25%). CD4% was utilized to reflect maternal health rather than absolute CD4 count because percentage values remain relatively stable throughout pregnancy, whereas CD4 counts often decrease during pregnancy due to hemodilution25. Caregiver characteristics considered were relationship to child (biological mother or not), education level (high school diploma or not), household income ≤ $20,000, number of individuals living in the household, number of child’s siblings living in the household, caregiver verbal IQ < 85, caregiver performance IQ < 85, caregiver health problems, caregiver too tired for activities of daily living, and caregiver report of difficulty caring for child. Birth characteristics such as low birth weight were not considered as confounders due to their possible role in the causal pathway of cARV exposure, but their association with impairment outcomes was evaluated.
Statistical Analyses
For each speech or language outcome, each participant was classified into one of the following groups: primary Impairment (PSI or PLI), concomitant impairment (CSI or CLI), or No Impairment (NI). The proportion of children within each category manifesting each speech and language outcome was summarized. Potential confounders were examined by impairment status for each of the seven speech or language impairment outcomes. Comparisons were made between children with Primary versus NI and between children with Concomitant versus NI. Associations of potential confounders with speech or language impairments were tested using a Wilcoxon test for continuous measures and Fisher’s Exact test for discrete measures.
Crude associations of in utero ARV exposures with speech or language impairment (Primary versus NI, and Concomitant versus NI) were examined using Fisher’s Exact test. Logistic regression models were used to model Primary versus NI and then Concomitant versus NI for each speech or language outcome. Covariates with p-value < 0.3 based on Wilcoxon or Fisher’s Exact tests were included in a logistic regression stepwise selection procedure, with entry criteria p-value < 0.2 and inclusion criteria p-value < 0.1. All child demographic characteristics were forced into the models. After potential confounders were identified through the stepwise selection procedure, the final core model was re-fitted to the set of subjects with complete data for the factors in the model.
The association between each speech or language impairment outcome and each ARV exposure was evaluated by both unadjusted and adjusted logistic regression. Each adjusted model was adjusted for demographic characteristics and the core covariates specific to each speech or language impairment. Exact logistic regression models were used for situations with lower exposure rates and low impairment rates.
Results
Study Population and Language Outcomes
As of May, 2014, 492 monolingual HEU children had at least one valid speech or language assessment: 208 at age 3 years, and 429 at age 5 years; 145 had an assessment at both ages. As shown in Table 1, the 3- and 5-year age groups had similar demographic characteristics. Additional child, maternal, and household demographic factors are reported in Supplemental Digital Content 1 (Table).
Table 1.
Child, maternal, and household demographic factors for monolingual HIV-exposed uninfected participants with language assessments at age 3 or 5 years in the PHACS SMARTT Study, by age.
| Characteristics | Age 3 (n=208) |
Age 5 (n=429) |
Age 3 or 5 Totala (n=492) |
|---|---|---|---|
| Child characteristics | |||
| Median age (min, max) | 3.1 (2.8, 3.9) | 5.1 (4.8, 5.9) | – |
| Female sex | 118 (57%) | 229 (53%) | 262 (53%) |
| Black race | 152 (73%) | 361 (84%) | 398 (81%) |
| Hispanic ethnicity | 34 (16%) | 26 (6%) | 51 (10%) |
| Primary language | |||
| English | 189 (91%) | 429 (100%) | – |
| Spanish | 19 (9%) | 0 (0%) | – |
| Birthweight (grams) | |||
| <2,000 | 11 (5%) | 30 (7%) | 34 (7%) |
| 2,000 to <2,500 | 27 (13%) | 55 (13%) | 65 (13%) |
| ≥2,500 | 169 (82%) | 336 (80%) | 385 (80%) |
| Maternal characteristics during pregnancy | |||
| Maternal alcohol use | 11 (6%) | 31 (8%) | 36 (8%) |
| Maternal tobacco use | 46 (24%) | 98 (25%) | 109 (24%) |
| Latest maternal CD4% <25 | 62 (32%) | 117 (30%) | 141 (31%) |
| Caregiver characteristics | |||
| Lacks high school degree | 72 (35%) | 128 (30%) | 152 (31%) |
| Verbal IQ <85 | 81 (45%) | 180 (45%) | 194 (44%) |
| Self-reported health problems | 187 (91%) | 369 (87%) | 426 (87%) |
| Self-reported difficulty caring for child | 30 (15%) | 74 (17%) | 80 (16%) |
| Household characteristics | |||
| Household income ≤ $20,000 | 134 (69%) | 266 (67%) | 310 (63%) |
| Median number in household (IQR) | 4 (3, 5) | 4 (3, 5) | 4 (3, 5) |
IQR=interquartile range (25th, 75th percentiles)
Total column includes participants evaluated at age three or age five; 145 participants had an assessment that was included in the analysis at both ages.
Missing data on 8 participants for birthweight, 43 for maternal alcohol use during pregnancy and maternal tobacco use during pregnancy, 40 for latest maternal CD4%, 6 for caregiver lacks high school degree, 51 for caregiver verbal IQ, 4 for caregiver health problems and difficulty caring for child, 35 for household income, and 6 for number in household.
Speech and language impairment classifications—Primary or concomitant
At age 3, of the 186 children (89%) who completed the Bayley Screen, 5 (3%) were classified as “at risk” with a low cognitive score. One of 208 3-year old children (0.5%) was identified to have hearing impairment. At age 5, of the 425 children (99%) who completed the WPPSI-III, 104 (24%) were classified as having low cognitive functioning. Nineteen of 429 children (4%) were identified to have hearing impairment.
The number and percentage of HEU children in each category for each speech or language impairment is displayed in Table 2 and Figure 1. The proportion of children with impairments varied according to age, primary vs concomitant groups, and type of impairments. Highest rates were observed for vocabulary at 3 years for the Primary group (19%) and lowest for speech impairments at 3 and 5 years for the Concomitant group (2%). Overall, the proportion of children with speech impairments was lower (2-7%) than for language impairments (2-19%).
Table 2.
Prevalence of speech and language impairments among monolingual HIV-exposed uninfected participants.
| Impairment Type | |||||
|---|---|---|---|---|---|
| Age | Domain | Primary | Concomitanta | None | Total |
| 3b | Speech | 13 (7%) | 3 (2%) | 159 (91%) | 175 |
| Language | 25 (13%) | 3 (2%) | 164 (84%) | 195d | |
| Vocabulary | 35 (19%) | 4 (2%) | 146 (78%) | 186e | |
| 5c | Speech | 13 (7%) | 3 (2%) | 163 (91%) | 179 |
| Language | 66 (16%) | 71 (17%) | 276 (67%) | 414e | |
| Vocabulary | 30 (7%) | 36 (9%) | 350 (84%) | 416 | |
| Grammar | 59 (14%) | 49 (12%) | 306 (74%) | 415e | |
Concomitant Impairment indicates speech or language impairment concurrent with hearing or cognitive impairment (determined within one year of the 3rd or 5th birthday)
Age three impairments based on the Goldman Fristoe Test of Articulation (speech), Test of Early Language Development (language), and Peabody Picture Vocabulary Test (vocabulary).
Age five impairments based on the Goldman Fristoe Test of Articulation (speech), and Test of Language Development (language, vocabulary, grammar).
3 children with language impairment that could not be classified as primary or concomitant because they did not complete the cognitive assessment were excluded
1 child with language impairment that could not be classified as primary or concomitant because they did not complete the cognitive assessment was excluded
Figure 1.
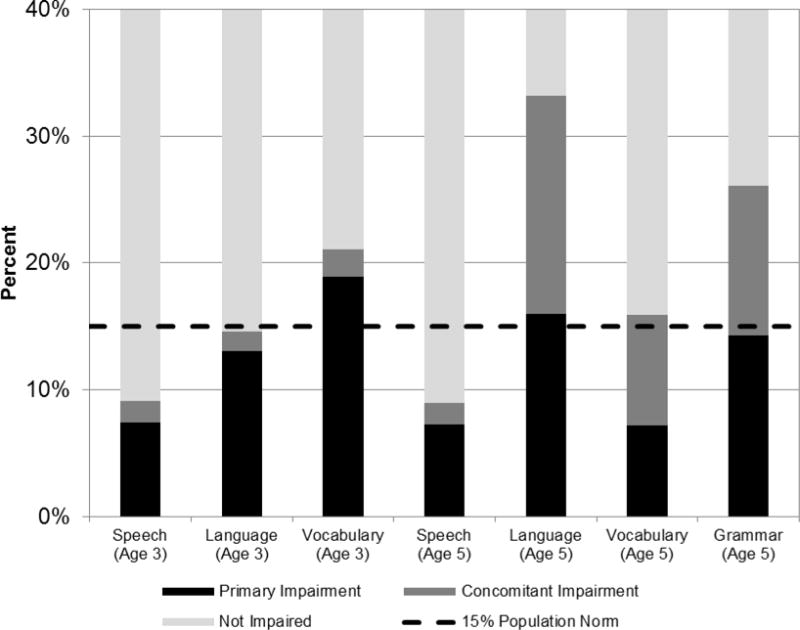
Study Prevalence of Primary and Concomitant Speech, Language, Vocabulary and Grammar Impairment at Ages 3 and 5 Years.
In response to a reviewer, we examined whether monolingual Spanish-speaking children (N = 16) were at a disadvantage for language assessment. The mean standard scores and SDs for the TELD-3 at age 3 were as follows, where 100 is the expected mean and 15 is the expected SD: Receptive language, English, 99.99 (15.4), Spanish, 104.63 (12.4); Expressive language, English, 101.4 (13.7), Spanish, 103.9 (13.6); Spoken language quotient, English 100.8 (16.2), Spanish, 105.00 (14.6). While the monolingual Spanish group was small, there were no statistical differences in mean scores between the groups. The proportion of children identified as language impaired was actually slightly higher for the English-speaking group compared to the Spanish-speaking group (16% vs 13%), suggesting no disadvantage for the Spanish-speaking children. The monolingual English-speaking group and the monolingual Spanish-speaking group performed as expected relative to the population norms of TELD-3.
The general population estimates for language impairments using these criteria would be about 15%9. HEU children had lower scores compared to population norms (PN) at ages 3 for vocabulary (mean SC (mSC) = 94.4, 95% CI: 92.4, 96.4; PN = 100) and 5 years for overall language (mSC = 90.4, CI: 89.1, 91.8; PN = 100), vocabulary (mSC = 9.4, CI: 9.2, 9.7; PN = 10) and grammar (mSC=8.4, CI: 8.1, 8.6; PN = 10), but did not underperform on the speech assessment at either age.
Speech/Language Impairment and ARV Exposure
A summary of the associations of ARV exposure with speech or language impairment groups is provided in Table 3, where the reference group is NI. The associations are adjusted for demographic characteristics and various child, maternal, and caregiver factors as reported below. The summary shows that certain in utero ARV exposures were associated with reduced risk while others were associated with increased risk for speech and language impairments, with effects of cARV and individual drugs varying by age and type of impairment. Measures of association were more robust at 5 years than at 3 years; all indications of reduced risk effects were at 5 years, and all but one of those were for the CLI group only. For example, tenofovir was associated with reduced risk effects across different dimensions of language at age 5 years for the CLI group, and was associated with increased risk for speech impairment at 3 years for the PSI group. Although the associations are statistically significant, the effect size, indexed by ORs, were generally modest. We observed no association between low birth weight (<2500gm, LBW) and impairment in speech, language, vocabulary, or grammar outcomes at age 3 or 5 years, with the exception of higher risk of PSI at age 5 for children with LBW. However, for this outcome, further adjustment for LBW had little impact on observed associations with in utero ARV exposures.
Table 3.
Adjusted associations of in utero ARV exposure with speech or language impairment including all ARV exposures with p<0.10
| ARV | Age / Groupa | Impairment | Adjusted OR (95% CI) | P-Value |
|---|---|---|---|---|
| Decreased Risk | ||||
| cARV vs 3NRTI | 5 / PSI | Speech | 0.24 (0.05, 1.10)a | 0.07a |
| Didanosine | 5 / CLI | Language | 0.16 (0.02, 1.27) | 0.08 |
| 5 / CLI | Grammar | 0.17 (<0.01, 0.81) | 0.05 | |
| Tenofovir | 5 / CLI | Language | 0.53 (0.27, 1.04) | 0.06 |
| 5 / CLI | Vocabulary | 0.42 (0.16, 1.12) | 0.08 | |
| 5 / CLI | Grammar | 0.32 (0.13, 0.77) | 0.01 | |
| Nelfinavir | 5 / CLI | Language | 0.52 (0.27, 1.00) | 0.05 |
| Increased Risk | ||||
| cARV vs 3NRTI | 3 / PLI | Language | 5.17 (1.02, Infinity) | 0.09 |
| Didanosine | 5 / PLI | Vocabulary | 3.46 (1.18, 10.21) | 0.02 |
| Lamivudine | 5 / CLI | Language | 2.10 (0.90, 4.93) | 0.09 |
| Tenofovir | 3 / PSI | Speech | 5.28 (1.09, 30.39) | 0.04 |
| Zidovudine | 5 / CLI | Language | 2.35 (1.00, 5.50) | 0.05 |
| 5 / CLI | Grammar | 2.50 (0.84, 7.43) | 0.10 | |
CLI = Concomitant Language Impairment; PSI = Primary Speech Impairment; PLI = Primary Language Impairment; reference group for each was “no impairment”
OR = odds ratio; CI=confidence interval, cARV=combination antiretroviral, 3NRTI=three or more nucleoside/nucleotide analog reverse transcriptase inhibitors regimen. All models adjusted for age, sex, race, and ethnicity. Model of age 3 PSI also adjusted for caregiver health problems and caregiver difficulty caring for the child; model of age 3 PLI/language: maternal alcohol use during pregnancy and caregiver lack high school degree. Model of age 5 CLI/grammar also adjusted for caregiver health problems.
aOR (95% CI) = 0.28 (0.06, 1.37), p-value = 0.12 when further adjusted for low birth weight (< 2500 gm).
In the adjusted logistic regression models of ARV exposure, for language impairment, zidovudine was associated with higher odds of CLI (aOR 2.35, p = 0.05) and nelfinavir was associated with lower odds (aOR 0.52, p = 0.05). Additionally, didanosine and tenofivir were associated with lower odds (aOR 0.16, p = 0.08, and aOR 0.53, p = 0.06, respectively) and lamivudine was associated with higher odds (aOR 2.10, p = 0.09), although not attaining statistical significance. For vocabulary impairment, after adjustment, tenofovir was associated with marginally lower odds (aOR .42, p = 0.08). For grammar impairment, after adjustment, tenofovir and didanosine were associated with lower odds (aOR 0.32, p = 0.01 and aOR 0.17, p=0.05, respectively); and zidovudine was marginally associated with higher odds (aOR 2.50, p = 0.10).
Details of the logistic regression models for primary and concomitant impairments at each age for each speech or language outcome including both ARV exposures and covariates are displayed in Supplemental Digital Content 2–4 (table). There is some variation in associations of speech and language outcomes with age, sex, race, ethnicity and household/caregiver across groups and times of measurement, with the exception of the 5-year-old CLI group. Female sex was associated with lower odds of CLI (aOR 0.54, p = 0.03) and grammar impairment (aOR 0.39, p = 0.007); black race was associated with higher odds of language impairment (aOR 2.93, p = 0.04), vocabulary impairment (aOR 5.22, p = 0.06) and grammar impairment (aOR 8.94, p = 0.01).
Discussion
This is a descriptive study on a number of children who were all exposed to ARVs in utero given that they were born to HIV infected women. This first investigation of speech and language acquisition of HEU preschool children revealed interesting differences and similarities for speech and language impairments, with or without concomitant cognitive impairment and/or hearing loss. Consistent with the outcomes of our earlier studies of infants and school age children4–6, there was elevated risk for language impairments for HEU children at 3 and more so at 5 years when compared to population norms, although there was no elevated risk for speech impairments. Overall, 33% of children had language impairments at 5 years, more than double what is expected.
One unexpected finding was the relatively small number of children identified as CLI at 3 years. This was attributable to a small number of children who met the criterion for low levels of nonverbal cognitive abilities as measured by the Bailey-III Screener “at risk” category. Among 208 children of age 3 included in this study, 186 (89%) were assessed by Bailey-III Screener and only 5 (3%) of them were categorized as “at risk”, regardless of their language impairment status. This suggests a possible under-identification of children with low nonverbal cognitive abilities on this brief screening version of the Bayley III assessment21–22. We found consistency in the proportions of children with speech and language impairments in the PLI groups at 3 and 5 years, and at 5 years comparing the PLI and CLI groups, even though the proportions of speech impairments were consistently lower than language impairments (see Table 2). However, not all of the children were measured at both 3 and 5 years, depending on the measures. Overall, 145 children had any assessment at age 3 years and any assessment at age 5 years, which contribute to 70% (145/208) of age 3 study group and 34% (145/429) of age 5 study group. Further detail is provided in Supplemental Digital Content 5 (table), which reports the breakdown by speech or language domain. Of the 139 children assessed for language, 76.5% were stable in classification across ages 3 and 5 (None/none, 95/139, 68%; Primary/primary,10/139, 7%; Concomitant/concomitant, 2/139,1.4%. Three children shifted from primary at 3 years to concomitant at 5 years; 2 were concomitant at 3 and 5. The biggest shift was for children who did not score as language impaired at 3 years but did so at 5 years, evenly distributed as Primary (12) or Concomitant (11). Only 3 children moved from Primary at 3 years to Concomitant at 5 years, suggesting that a possibly insensitive Bayley score at 3 years was not a major contributor to the distribution of children across groups. The general picture is that the risk of language impairment increases with age, as more complex language abilities emerge, which may or may not be accompanied by a general cognitive impairment.
We examined possible associations of demographic and caregiver characteristics and infant birth characteristics on speech and language impairments at ages 3 and 5 years in HEU children. Predictors of speech and language acquisition varied across measures and time points, but black race was consistently associated with increased odds of impairment of all studied groups (aOR range 2.32 – 8.94). Effects were strongest at age five, suggesting possible cumulative age effects, more discriminating testing at older ages or possible severity effects such that children of black race are more at risk as they age, especially if their language impairments co-exist with other developmental impairments. A study of 336 rural 4-year-old Pennsylvania Head Start children, using the same language test as used for 5-year-olds in this study, provides a useful comparison26. Nearly two-thirds of the low income sample in the Pennsylvania study evidenced clinically significant language delay using criteria similar to this study. Overall language levels did not differ by minority (African-American or Hispanic) and White European Majority groups, and there was no interaction with nonverbal IQ levels, suggesting that the test is not biased. The absence of a mean difference between minority and majority groups in the Head Start study differs from the finding of racial differences in our study. These differences may be attributable to methodological differences: Our models adjusted for household income and thus identify potential risk indicators among HEU children after adjusting for household income. Another relevant recent study27 from the nationally representative sample of the Early Childhood Longitudinal Study, Birth Cohort (ECLS-B) (N=9600) suggests that the PPVT assessment we used is not biased for low performance for African American children. Using the PPVT as a vocabulary outcome at 48 months, in their model for low PPVT scores as outcome, defined as 10% or below, African American race was not a statistically significant sociodemographic predictor. Further, the Hammer et al study found no statistical significance for African American race as a predictor in their model for low language outcomes at 24 months of age, using a different language assessment, providing further support for the validity of the PPVT at 48 months.
Overall, the outcomes are reassuring regarding possible in utero ARV exposure risks for SI or LI; the signals are not highly significant in the face of multiple tests, and the domains affected or directions of the effects are diverse. Yet some signals bear evaluation in other cohorts and attention to research methods. Interpretation of the patterns of effects for ARV exposure may require consideration of differences between speech and language impairments, Primary vs Concomitant groups, and age differences. For example, cARV relative to triple NRTI regimens did not add risks for speech impairments at 5 years but added risk for language impairment at 3 years for children without concomitant low nonverbal cognitive abilities or hearing impairment. Given that behavioral data show that speech impairments are independent of language impairments28, it is possible that the relationships between cortical infrastructure and drug effects are different for speech compared to language development. It is also possible that the effects of drugs differ on speech or language impairment at particular developmental levels during the dynamic time of change between 3 and 5 years of age, as suggested by the different patterns of outcome across ages. Another possible timing effect is when during pregnancy the exposure started. Consideration of individual drugs also suggests differential effects at different developmental levels for speech vs. language. Tenofovir was associated with reduced risk of all three measures of language impairment (overall, vocabulary, and grammar) at 5 years for the CLI group, but was linked to increased risk for speech acquisition for children in the PSI group at 3 years; thus, at 3 years the added risk for speech impairments is apparently selective for speech as compared to the reduced risk at 5 for the broad language acquisition mechanisms for children with CLI. These observations are consistent with the distinct trajectories of speech and language impairments for children without neurological disorders or exposure to cARV28. Speech impairments and language impairments in the general population of 6-year-old children overlap only 2%28 although children with SI and LI are more likely than LI children to be enrolled in clinical treatment.
In studies of adults with HIV, HIV-associated neurocognitive disorders (HAND) is attributed to poor control of HIV in the central nervous system, with limited CNS penetration by ARV drugs in cerebrospinal fluid associated with HAND29,30. A recent analysis of ARV drug concentrations in brain tissue collected from adults dying with HIV disease found that tenofovir, unlike other evaluated drugs, had higher concentrations than expected from previous levels found in cerebrospinal fluid31. The suggestion of reduced risk for language impairment outcomes as well as increased risk for speech with tenofovir exposure in HEU children may be consistent with new findings of tenofovir concentrations in brain tissue from adults with HIV and ARV drug exposure.
In keeping with the safety monitoring goal of SMARTT, these analyses examined a large number of in utero ARV exposures for associations with speech and language impairment. The limitations of the study include those of interpretation of possible effects of single drugs. Given clinical practice over the last decade, individual ARV drugs were prescribed as part of a combination regimen, creating complexity in statistical outcomes. Another limitation of the data source is that clinical practices in the U.S. are not representative of worldwide clinical practices. Also, in the U.S., some drugs, including didanosine and nelfinavir, are no longer used during pregnancy. This study evaluated children at two different ages; longitudinal analyses to evaluate consistency of impairments across time will be reported in a subsequent study. Further exploration of the relationship between ARV exposure and speech/language impairment among pre-school children is warranted to confirm the observed associations, with a particular need for longitudinal data.
Supplementary Material
Acknowledgments
We thank the children and families for their participation in PHACS, and the individuals and institutions involved in the conduct of PHACS. The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development with co-funding from the National Institute on Drug Abuse, the National Institute of Allergy and Infectious Diseases, the Office of AIDS Research, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, the National Institute on Deafness and Other Communication Disorders, the National Heart Lung and Blood Institute, the National Institute of Dental and Craniofacial Research, and the National Institute on Alcohol Abuse and Alcoholism, through cooperative agreements with the Harvard T.H. Chan School of Public Health (HD052102) (Principal Investigator: George Seage; Project Director: Julie Alperen) and the Tulane University School of Medicine (HD052104) (Principal Investigator: Russell Van Dyke; Co-Principal Investigators: Kenneth Rich, Ellen Chadwick; Project Director: Patrick Davis). Data management services were provided by Frontier Science and Technology Research Foundation (PI: Suzanne Siminski), and regulatory services and logistical support were provided by Westat, Inc (PI: Julie Davidson).
The following institutions, clinical site investigators and staff participated in conducting PHACS SMARTT in 2015, in alphabetical order: Ann & Robert H. Lurie Children’s Hospital of Chicago: Ram Yogev, Margaret Ann Sanders, Kathleen Malee, Scott Hunter; Baylor College of Medicine: William Shearer, Mary Paul, Norma Cooper, Lynnette Harris; Bronx Lebanon Hospital Center: Murli Purswani, Emma Stuard, Anna Cintron; Children’s Diagnostic & Treatment Center: Ana Puga, Dia Cooley, Patricia A. Garvie, James Blood; New York University School of Medicine: William Borkowsky, Sandra Deygoo,Marsha Vasserman; Rutgers - New Jersey Medical School: Arry Dieudonne, Linda Bettica; St. Jude Children’s Research Hospital: Katherine Knapp, Kim Allison, Megan Wilkins; San Juan Hospital/Department of Pediatrics: Midnela Acevedo-Flores, Lourdes Angeli-Nieves, Vivian Olivera; SUNY Downstate Medical Center: Stephan Kohlhoff, Ava Dennie, Susan Bewley; Tulane University School of Medicine: Russell Van Dyke, Karen Craig, Patricia Sirois; University of Alabama, Birmingham: Marilyn Crain, Paige Hickman, Dan Marullo; University of California, San Diego: Stephen A. Spector, Kim Norris, Sharon Nichols; University of Colorado, Denver: Elizabeth McFarland, Carrie Chambers, Jenna Wallace, Emily Barr; University of Florida, Center for HIV/AIDS Research, Education and Service: Mobeen Rathore, Kristi Stowers, Saniyyah Mahmoudi, Ann Usitalo; University of Illinois, Chicago: Karen Hayani, Kenneth Rich, Lourdes Richardson, Renee Smith; University of Miami: Gwendolyn Scott, Sady Dominguez, Anai Cuadra; University of Southern California: Toni Frederick, Mariam Davtyan, Guadalupe Morales-Avendano; University of Puerto Rico School of Medicine, Medical Science Campus: Zoe M. Rodriguez, Ibet Heyer, Nydia Scalley Trifilio.
SOURCES OF SUPPORT: The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development with co-funding from the National Institute on Drug Abuse, the National Institute of Allergy and Infectious Diseases, the Office of AIDS Research, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, the National Institute on Deafness and Other Communication Disorders, the National Heart Lung and Blood Institute, the National Institute of Dental and Craniofacial Research, and the National Institute on Alcohol Abuse and Alcoholism, through cooperative agreements with the Harvard T.H. Chan School of Public Health (HD052102) (Principal Investigator: George Seage; Project Director: Julie Alperen) and the Tulane University School of Medicine (HD052104) (Principal Investigator: Russell Van Dyke; Co-Principal Investigators: Kenneth Rich, Ellen Chadwick; Project Director: Patrick Davis). Data management services were provided by Frontier Science and Technology Research Foundation (PI: Suzanne Siminski), and regulatory services and logistical support were provided by Westat, Inc (PI: Julie Davidson).
Footnotes
Note: The conclusions and opinions expressed in this article are those of the authors and do not necessarily reflect those of the National Institutes of Health or U.S. Department of Health and Human Services.
References
- 1.Brackis-Cott E, Kang E, Dolezal C, Abrams EJ, Mellins CA. The impact of perinatal HIV infection on older school-aged children’s and adolescents’ receptive language and word recognition skills. AIDS Patient Care STDS. 2009;23(6):415–421. doi: 10.1089/apc.2008.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brackis-Cott E, Kang E, Dolezal C, Abrams EJ, Mellins CA. Brief Report: Language ability and school functioning of youth perinatally infected with HIV. J Pediatr Health Care. 2009;23(3):158–164. doi: 10.1016/j.pedhc.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coplan J, Contello KA, Cunningham CK, et al. Early language development in children exposed to or infected with Human Immunodeficiency Virus. Pediatrics. 1998;102(1):e8. doi: 10.1542/peds.102.1.e8. [DOI] [PubMed] [Google Scholar]
- 4.Rice ML, Buchanan AL, Siberry GK, et al. Language impairment in children perinatally infected with HIV compared to children who were HIV-exposed and uninfected. J Dev Behav Pediatr. 2012;33(2):112–123. doi: 10.1097/DBP.0b013e318241ed23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rice ML, Zeldow B, Siberry GK, et al. Evaluation of risk for late language emergence after in utero antiretroviral drug exposure in HIV-exposed uninfected infants. Pediatr Infect Dis J. 2013;32(10):e406–e413. doi: 10.1097/INF.0b013e31829b80ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sirois PA, Huo Y, Williams PL, et al. Safety of perinatal exposure to antiretroviral mediations: Developmental outcomes in infants. Pediatr Infect Dis J. 2013;32(6):648–655. doi: 10.1097/INF.0b013e318284129a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shriberg LD, Tomblin JB, McSweeny JL. Prevalence of Speech Delay in 6-Year-Old Children and Comorbidity With Language Impairment. J Speech Lang Hear Res. 1999;42(6):1461–1481. doi: 10.1044/jslhr.4206.1461. [DOI] [PubMed] [Google Scholar]
- 8.Rice ML, Taylor CL, Zubrick SR. Language outcomes of 7-year-old children with or without a history of Late Language Emergence at 24 months. Journal of Speech, Language, and Hearing Research. 2008;51(2):394–407. doi: 10.1044/1092-4388(2008/029). [DOI] [PubMed] [Google Scholar]
- 9.Tomblin JB, Records NL, Buckwalter P, Zhang X, Smith E, O’Brien M. The prevalence of specific language impairment in kindergarten children. J Speech Hear Res. 1997;40:1245–1260. doi: 10.1044/jslhr.4006.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norbury CF, Gooch D, Wray C, et al. The impact of nonverbal ability on prevalence and clinical presentation of language disorder: evidence from a population study. Journal of Child Psychology & Psychiatry. 2016;57(11):1247–1257. doi: 10.1111/jcpp.12573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams PL, Seage GRr, Van Dyke RB, et al. A trigger-based design for evaluating the safety of in utero antiretroviral exposure in uninfected children of human immunodeficiency virus-infected mothers. Am J Epidemiol. 2012;175(9):950–961. doi: 10.1093/aje/kwr401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams PL, Hazra R, Van Dyke RB, et al. Antiretroviral exposure during pregnancy and adverse outcomes in HIV-exposed uninfected infants and children using a trigger-based design. AIDS. 2016;30(1):133–144. doi: 10.1097/QAD.0000000000000916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caniglia EC, Patel K, Huo Y, et al. Atazanivir exposure in utero and neurodevelopment in infants: A comparative safety study. AIDS. 2016;30(8):1267–1278. doi: 10.1097/QAD.0000000000001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Redmond SM. Language Impairment in the Attention-Deficit/Hyperactivity Disorder Context. Journal of Speech, Language, and Hearing Research. 2016;59:133–142. doi: 10.1044/2015_JSLHR-L-15-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rice ML, Hoffman L. Predicting vocabulary growth in children with and without Specific Language Impairment (SLI): A longitudinal study from 2 1/2 to 21 years of age. Journal of Speech, Language & Hearing Research. 2015;58:345–359. doi: 10.1044/2015_JSLHR-L-14-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldman R, Fristoe M. Goldman Fristoe Test of Articulation-2. 2nd. Circle Pines, MN: American Guidance Service; 2000. [Google Scholar]
- 17.Hresko WP, Reid DK, Hammill DD. Test of Early Language Development-3. Austin, TX: Pro-Ed; 1999. [Google Scholar]
- 18.Dunn LM, Dunn DM. Peabody Picture vocabulary Test. Fourth. San Antonio, Texas: PsychCorp; 2007. [Google Scholar]
- 19.Newcomer PL, Hammill DD. Test of Language Development 2-Primary. 2nd. Auxtin, TX: Pro-Ed; 1988. [Google Scholar]
- 20.Redmond SM, Thompson HL, Goldstein S. Psycholinguistic Profiling Differentiates Specific Language Impairment from Typical Development and From Attention-Deficit/Hyperactivity Disorder. Journal of Speech, Language, and Hearing Research. 2011;54:99–117. doi: 10.1044/1092-4388(2010/10-0010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bode MM, D’Eugenio DB, Mettelman BB, Gross SJ. Predictive Validity of the Bayley, at 2 years for Intelligence Quotient at 4 years in Preterm Infants. J Dev Behav Pediatr. 2014;35(9):570–575. doi: 10.1097/DBP.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 22.Torre P, Zeldow B, Hoffman HJ, et al. Hearing loss in perinatally HIV-infected and HIV-exposed but uninfected children and adolescents. The Pediatric Infectious Disease Journal. 2012;31(8):835–841. doi: 10.1097/INF.0b013e31825b9524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bayley N. Bayley Scales of Infant and Toddler Development. Third. San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- 24.Weschler D. Wechsler Preschool and Primary Scale of Intelligence–III. San Antonio, Texas: Pearson; 2002. [Google Scholar]
- 25.Ekouevi DK, Inwoley A, Tonwe-gold B, et al. Variation of CD4 count and percentage during pregnancy and after delivery: implications for HAART initiation in resource-limited settings. AIDS Res Hum Retroviruses. 2007;23(12):1469–1474. doi: 10.1089/aid.2007.0059. [DOI] [PubMed] [Google Scholar]
- 26.Nelson KE, Welsh JA, Trup EMV, Greenberg MT. Language delays of impoverished preschool children in relation to early academic and emotion recognition skills. First Language. 2011;31:164–194. [Google Scholar]
- 27.Hammer CS, Morgan PL, Farkas G, Hillemeier MM, Bitetti D, Maczuga S. Late Talkers: A population-based study of risk factors and school rediness consequences. J Speech Lang Hear Res. 2017;60:607–626. doi: 10.1044/2016_JSLHR-L-15-0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shriberg LD, Tomblin JB, McSweeny JL. Prevalence of speech delay in 6-year-old children and comorbidity with language impairment. J Speech Lang Hear Res. 1999;42:1461–1481. doi: 10.1044/jslhr.4206.1461. [DOI] [PubMed] [Google Scholar]
- 29.Best BM, Letendre SL, Koopmans P, et al. Low cerebrospinal fluid concentrations of the nucleotide HIV reverse transcriptase inhibitor, Tenofovir. Acquired Immune Deficiency Syndrome. 2012;59(4):376–381. doi: 10.1097/QAI.0b013e318247ec54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lahiri CD, Reed-Walker K, Sheth AN, Acosta EP, Vunnava A, Ofotokun I. Cerebrospinal fluid concentratoins of Tenofovir and Emtricitabine in the setting of HIV-I protease inhibitor-based regimens. The Journal of Clinical Pharmacology. 2015;56(4):492–496. doi: 10.1002/jcph.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bumpus N, Ma Q, Best BM, et al. Antiretroviral concentrations in brain tissue are similar to or exceed those in CSF. J Neurovirol. 2015;21:S10–S10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


