ABSTRACT
Vietnam is facing a problem of over-crowding in public hospitals. Long waiting time is a major dissatisfaction for patients. Reducing waiting time benefits not only patients but also hospitals in decreasing overall workload. To identify factors contributing to long waiting time in outpatient clinics, a cross-sectional study was conducted at a national hospital in Vietnam. The time for each process of 7,931 patients who visited the outpatient clinics within Thong Nhat Hospital from 5 to 9 September 2016 was collected from the computerized clinical database. Characteristics of patients (age, sex, address, day of visit, registration time, visited department and test) and waiting times were studied at the outcome measures. Multivariate analyses using the linear regression model was carried out to evaluate the contribution of these factors to the total waiting time. Among 7,931 patients, 52.3% were women, 46.3% were 60–80 years, and 64.8% registered between 5:30 and 9:30. The mean total waiting time was 104.1 minutes. The analysis on total waiting time among 4,564 patients who visited one department without any test showed that department group and registration time were significantly associated with a total waiting time. In 1,259 patients who visited one department with one test, early registration and undergoing blood tests were significantly associated with a longer total waiting time. These results showed that old age, visiting internal medicine departments, early registration time, and undergoing blood tests were factors contributing to a longer total waiting time in the outpatient clinics within Thong Nhat Hospital.
Key Words: outpatient clinic, overcrowding, Vietnam, waiting time
INTRODUCTION
Vietnam is one of the countries of Southeast Asia that has a high-level health care system. Commune health stations provide primary care, and hospitals provide high-level curative and preventive care. According to data from the Ministry of Health, at the end of 2013, there were 1,180 hospitals in Vietnam, including 150 managed by the private sector. Public hospitals are categorized by levels of care and technical services, and are divided into three groups: national hospitals under the Ministry of Health, provincial hospitals, and district hospitals.1) Currently, Vietnam is facing a problem of over-crowding in public hospitals. As there are no restrictions on health insurance by the law, many patients visit high-level medical institutions rather than low-level ones for treatment. A study in Vietnam showed that 48% of patients came to central hospitals from other provinces and that only 18% of them received the correct level of health services.2) Thus, the study showed that majority of the patients could be treated at low-level hospitals. The main causes of patients seeking high-level hospitals include larger intake capacity and attractiveness of high-level hospitals due to better techniques and famous doctors.3)
The over-crowding situation of hospitals usually leads to extremely long waiting times, which is one of the causes of patient dissatisfaction.4,5) The Institute of Medicine recommends that at least 90% of patients should meet doctors within 30 minutes of their scheduled appointment times.6) However, patients wait for 2 to 4 hours in the outpatient departments before consulting with doctors.7,8) The duration of waiting times varies depending on health facilities, and many factors affect waiting times, such as quality of medical facilities, quantity and quality of medical equipment, capacity of human resources, speed of a registration process, and patient flow.9) As a waiting time is important for all patients, the health care system should be better managed and organized. A waiting time is not only a factor that affects patient satisfaction but also one of indexes to evaluate the quality of services rendered to outpatients.10,11) Reducing waiting time benefits not only patients but also hospitals in decreasing overall workload.12)
Thong Nhat Hospital is one of the biggest national hospitals in Ho Chi Minh City and managed by the Ministry of Health. The number of inpatient beds is 1,200. The hospital is one of the specialized medical centers for gerontology in southern Vietnam. The number of health insurance cards used in the hospital has increased dramatically from 40,000 in 2014 to 200,000 in early 2016. The number of outpatients has also increased; however, the number of outpatient clinics and medical staffs has remained unchanged. Each department of outpatient clinics has to examine at least 150–200 patients per day and, especially cardiology department has about 250 patients per day. Efforts of the Vietnamese Ministry of Health have resulted in a reduction in the number of patients per doctor per day to 50 in 2015, with a predicted drop to 35 in 2020.13) A long waiting time is a major dissatisfaction for patients and is frequently used as an internal evaluation indicator for hospitals.7,14) What are underlying causes for a long waiting time at Thong Nhat Hospital? Which part of outpatient clinics plays an important role in the process of providing health care services? Based on these research questions, this study was designed to identify factors that contribute to a long waiting time at outpatient clinics, in order to improve the process for making a waiting time shorter.
MATERIALS AND METHODS
Subjects
A cross-sectional study was conducted at Thong Nhat Hospital, in Ho Chi Minh City, Vietnam. The hospital has 1,200 beds with 35 departments and 1,200 medical staffs. Outpatient clinic includes 20 departments categorized on the basis of type of specialists. Patients who visited outpatient clinic of Thong Nhat Hospital during 1 week, from 5 to 9 September 2016, were considered eligible for enrolment into this study. Exclusion criteria were as follows: (1) patients who did not complete the process of medical consultants from registration to payment, (2) patients who had a severe disease and had to be admitted to the hospital for treatment, (3) patients on priority, such as patients aged above 80 years, pregnant patients or patients with disability, and (4) patients without health insurance coverage.
Data Collection
Data were collected from the computerized clinical database of the hospital. Although a new computer software was introduced in June 2013 to manage patients’ information, the system for recording the time for every patient visit to each department was completely set up in September 2016. Because there was no difference in the number of outpatient visits during different weeks, the study period was selected at random as 1 week from 5 to 9 September 2016 (Monday to Friday). The reception for outpatient clinics was open from 5:30 to 16:30. Doctors worked through Monday to Friday from 6:30 to 17:00, with a 1.5-hour break in the afternoons. The patient flow is shown in Fig. 1. Patients can visit outpatient clinic of the hospital without any appointment. Each Patient is given a number at the registration room and waits for seeing doctors at the consulting room. When doctors order blood tests or imaging tests for patients, patients go to have tests and wait for the results at the laboratory department or the imaging department. Patients see doctors again after getting the results. When patients finish consultation, they pay for medical fees at the cashier and then go to the pharmacy if patients are prescribed with medicine.
Fig. 1.
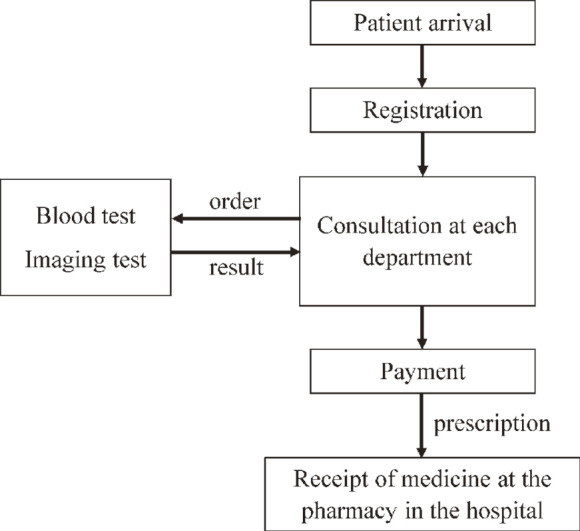
The Patient flow of outpatient clinic
Each Patient is given a number at the registration room. When doctors order blood tests or imaging tests, patients go to have tests and wait for the results at the laboratory department or the imaging department. Patients see doctors again after getting their results. When patients finish consultation, they pay for medical fees at the cashier and then go to the pharmacy if patients are prescribed with medicine. Total waiting time is from registration to payment in this study.
Collected data included age, sex, address, waiting times, departments that each patient visited for doctors’ consultation, and tests such as blood test and imaging tests. The whole process included registration, blood tests, imaging tests, medical consultations, and payments. In each section, time was automatically recorded into the computers when nurses entered the health insurance code of each patient. Twenty departments of the outpatient clinic were divided into four groups: “internal medicine” (cardiology, respiratory, gastroenterology, nephrology, infectious diseases, rheumatology, endocrinology, and neurology); “surgery” (neurosurgery, urology, thoracic and vascular surgery, orthopedic and trauma surgery, and general surgery); “oncology”; and “others” (otolaryngology, ophthalmology, odontology, dermatology, and traditional medicine). Imaging tests included radiography, CT scan, MRI, electrocardiography (ECG), ultrasonography, and endoscopy.
Waiting times of each process were collected for individual patients as follows: waiting time before consulting doctors (T1), waiting time before laboratory tests (T2), waiting time before imaging tests (T3), waiting time to receive results of laboratory tests (T4), and waiting time for payment (T5). Total waiting time (T) was calculated as follows: In case of patients who underwent both blood tests and imaging tests, the total waiting time was the sum of waiting times of all processes (T1 + T2 + T3 + T4 + T5). Total waiting times of patients who underwent no test, underwent blood tests, and underwent imaging tests were calculated as T1 + T5, T1 + T2 + T4 + T5, and T1 + T3 + T5, respectively.
Statistical Analysis
The descriptive statistical method was used to analyze the data using frequency, percentage, and mean and standard deviation. Statistical analysis was performed using the one-way ANOVA test to compare the mean of total waiting time with departments, registration time, visiting day, and presence or absence of medical examination. The significance of these factors with total waiting time was examined by multivariate analyses using the linear regression model. SPSS version 22.0 (IBM SPSS Inc.) was used for all data analysis. A P value of less than 0.05 was regarded to be significant.
Ethical Issues
The data were collected from the computerized clinical database of the hospital after obtaining permission from the director of Thong Nhat Hospital. To protect personal information, data were anonymized in a linkable fashion before analysis. This study was conducted as a management activity of the hospital.
RESULTS
Patient Characteristics
A total of 12,299 patients visited the outpatient clinics within Thong Nhat Hospital from 5 to 9 September 2016. The mean number of outpatients per day was 2,460. Data of 7,931 patients were collected in this study as 4,368 patients did not fulfill the inclusion criteria. Of 7,931 patients, women accounted for 52.3%, and 96.8% lived in Ho Chi Minh City (Table 1). Most patients were older than 40 years with the predominant age group being between 60 and 80 years (46.3%). Most patients visited early in the morning, from 5:30 to 9:30, and there was no marked difference in the number of patients visiting on different days of the week (Table 1). Patients who visited only one department without undergoing any tests were 4,564 (Table 2), and the total number of visits of all departments was 9,530 among 7,931 patients. More than half the number of patient visits (59.3%) were the department group of internal medicine (Table 3), and especially 62.8% visits among age group 60 – 80 years old were the internal medicine group.
Table 1.
Patient characteristics (N=7,931)
| Characteristic | Male | Female | Total | |||||
|---|---|---|---|---|---|---|---|---|
| (N=3,783) | (N=4,148) | (N=7,931) | ||||||
| N | (%) | N | (%) | N | (%) | |||
| Age group | ||||||||
| 16–39 | 587 | (15.5) | 924 | (22.3) | 1,511 | (19.1) | ||
| 40–59 | 1,192 | (31.5) | 1,551 | (37.4) | 2,743 | (34.6) | ||
| 60–80 | 2,004 | (53.0) | 1,673 | (40.3) | 3,677 | (46.3) | ||
| Location | ||||||||
| Ho Chi Minh City | 3,642 | (96.3) | 4,034 | (97.3) | 7,676 | (96.8) | ||
| Other areas | 141 | ( 3.7) | 114 | ( 2.7) | 255 | ( 3.2) | ||
| Day of week | ||||||||
| Monday | 780 | (20.6) | 873 | (21.0) | 1,653 | (20.8) | ||
| Tuesday | 887 | (23.4) | 975 | (23.5) | 1,862 | (23.5) | ||
| Wednesday | 711 | (18.8) | 826 | (19.9) | 1,537 | (19.4) | ||
| Thursday | 813 | (21.5) | 814 | (19.6) | 1,627 | (20.5) | ||
| Friday | 592 | (15.6) | 660 | (15.9) | 1,252 | (15.8) | ||
| Registration time | ||||||||
| 5:30–7:30 | 901 | (23.8) | 820 | (19.8) | 1,721 | (21.7) | ||
| 7:31–9:30 | 1,543 | (40.8) | 1,876 | (45.2) | 3,419 | (43.1) | ||
| 9:31–11:00 | 357 | ( 9.4) | 429 | (10.3) | 786 | ( 9.9) | ||
| 11:01–14:00 | 599 | (15.8) | 598 | (14.4) | 1,197 | (15.1) | ||
| 14:01–16:00 | 383 | (10.1) | 425 | (10.2) | 808 | (10.2) | ||
| Blood test | ||||||||
| Yes | 815 | (21.5) | 927 | (22.3) | 1,742 | (22.0) | ||
| No | 2,968 | (78.5) | 3,221 | (77.7) | 6,189 | (78.0) | ||
| Imaging test | ||||||||
| Yes | 612 | (16.2) | 915 | (22.1) | 1,527 | (19.3) | ||
| No | 3,171 | (83.8) | 3,233 | (77.9) | 6,404 | (80.7) | ||
| Number of test | ||||||||
| No | 2,741 | (72.5) | 2752 | (66.3) | 5,493 | (69.3) | ||
| One test | 657 | (17.4) | 950 | (22.9) | 1,607 | (20.3) | ||
| Two tests | 385 | (10.2) | 446 | (10.8) | 831 | (10.5) | ||
| Number of department | ||||||||
| One | 3,146 | (83.2) | 3,314 | (79.9) | 6,460 | (81.5) | ||
| Two | 576 | (15.2) | 767 | (18.5) | 1,343 | (16.9) | ||
| Three | 61 | ( 1.6) | 67 | ( 1.6) | 128 | ( 1.6) | ||
Table 2.
Number of patients by number of visiting departments and tests
| Number of tests | Number of departments | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| None | 4,564 | 867 | 72 | 5,503 |
| One test | 1,259 | 309 | 34 | 1,602 |
| Two tests | 637 | 167 | 22 | 826 |
| Total | 6,460 | 1,343 | 128 | 7,931 |
Table 3.
Visited departments among age groups
| Department | Age group | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 16–39 years old | 40–59 years old | 60–80 years old | ||||||
| N | % | N | % | N | % | N | % | |
| Internal medicine | 806 | 47.3 | 1,948 | 60.6 | 2,897 | 62.8 | 5,651 | 59.3 |
| Surgery | 300 | 17.6 | 457 | 14.2 | 401 | 8.7 | 1,158 | 12.2 |
| Oncology | 12 | 0.7 | 28 | 0.9 | 85 | 1.8 | 125 | 1.3 |
| Others | 587 | 34.4 | 779 | 24.3 | 1,230 | 26.7 | 2,596 | 27.2 |
| Total | 1,705 | 100 | 3,212 | 100 | 4,613 | 100 | 9,530 | 100 |
This table shows the number of visits of the department groups and the total number of visits was 9,530, because 1,343 and 128 patients visited two and three departments.
Waiting Time
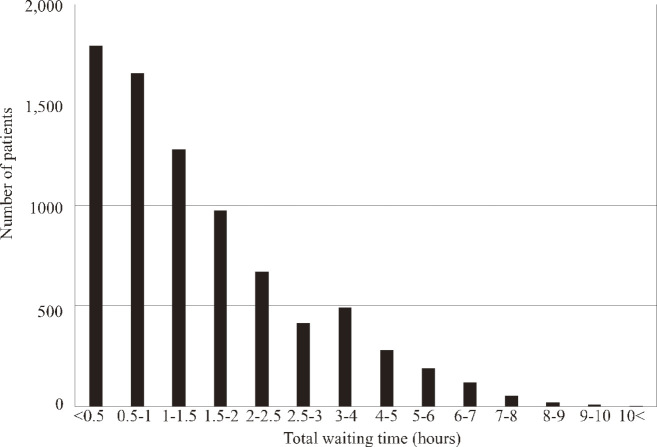
Fig. 2 shows the distribution of total waiting times of all 7,931 patients. The number of patients whose total waiting times were <0.5 hour, 0.5–1 hour, and 1–1.5 hours were 1,793 (22.6%), 1,655 (20.9%), and 1,278 (16.1%), respectively. The number of patients decreased as their total waiting time became longer. However, 383 patients (4.8%) had total waiting time longer than 5 hours. Total waiting time ranged from 4 to 623 minutes, with a mean of 104.1 minutes. Among the five processes, the mean waiting time was the longest for receiving results of blood tests (124.3 minutes) and the second longest was for undergoing imaging tests (78.4 minutes) (Table 4). Among patients whose total waiting time was <0.5 hour, most patients (83.3%) visited only one department, and only one and 14 patients had blood test and imaging tests, respectively. There were 16 patients who waited for 9 hours or more. Among the 16 patients, 5 patients (31.2%) visited two or three departments and all patients had both blood and imaging tests. Their registration time was between 7:35 and 9:04.
Fig. 2.
Distribution of the total waiting time of 7,931 patients
The number of patients whose total waiting times were <0.5 hour, 0.5–1 hour, and 1–1.5 hours were 1,793 (22.6%), 1,655 (20.9%), and 1,278 (16.1%), respectively. The number of patients decreased as their total waiting time became longer. However, 383 patients (4.8%) had total waiting time longer than 5 hours.
Table 4.
Waiting time for processes
| Waiting time | N | Min
(minute) |
Max
(minute) |
Mean ± SD
(minute) |
|---|---|---|---|---|
| Waiting time before consulting doctors (T1) | 7,931 | 1 | 401 | 50.3 ± 55.1 |
| Waiting time before blood tests (T2) | 1,742 | 1 | 236 | 50.4 ± 28.2 |
| Waiting time before imaging tests (T3) | 1,527 | 2 | 444 | 78.4 ± 59.9 |
| Waiting time to receive results of test (T4) | 1,742 | 2 | 449 | 124.3 ± 85.9 |
| Waiting time for payment (T5) | 7,931 | 1 | 188 | 9.4 ± 11.8 |
| Total waiting time (T) | 7,931 | 4 | 623 | 104.1 ± 96.4 |
SD, standard deviation
Correlation of Total Waiting Time with Variables of Patients
The total waiting time was significantly associated with the number of tests, the number of visited departments, day of the week, registration time, and department groups (P<0.001), as shown in Table 5. Patients who either registered earlier or visited more departments had a longer total waiting time. Among the analyzed parameters considering the registration time and department groups, time from 14:01 to 16:00 and the group of “others” showed the shortest total waiting time.
Table 5.
Correlation of total waiting time with variables of patients (N=7,931)
| Total waiting time (minute) | |||||
|---|---|---|---|---|---|
| Mean ± SD | Range | P-value | |||
| Number of tests | |||||
| 0 | 65.9 ± 61.1 | 4–406 | <0.001 | ||
| 1 | 148.4 ± 87.4 | 9–504 | |||
| 2 | 218.9 ± 114.0 | 25–606 | |||
| Number of departments | |||||
| 1 | 96.4 ± 87.9 | 4–606 | <0.001 | ||
| 2 | 107.1 ± 100.2 | 5–595 | |||
| 3 | 127.5 ± 118.4 | 10–540 | |||
| Day of week | |||||
| Monday | 86.6 ± 76.9 | 4–563 | <0.001 | ||
| Tuesday | 101.4 ± 97.4 | 5–561 | |||
| Wednesday | 92.8 ± 89.4 | 4–540 | |||
| Thursday | 104.9 ± 90.7 | 4–595 | |||
| Friday | 109.5 ± 97.4 | 5–606 | |||
| Registration time | |||||
| 5:30–7:30 | 126.0 ± 88.3 | 5–606 | <0.001 | ||
| 7:31–9:30 | 109.3 ± 100.4 | 4–595 | |||
| 9:31–11:00 | 96.9 ± 104.3 | 5–473 | |||
| 11:01–14:00 | 66.9 ± 47.4 | 4–302 | |||
| 14:01–16:00 | 44.3 ± 37.1 | 4–431 | |||
| Department group | |||||
| Internal medicine | 41.4 ± 56.8 | 4–440 | <0.001 | ||
| Surgery | 81.7 ± 59.8 | 6–437 | |||
| Oncology | 79.0 ± 59.5 | 7–433 | |||
| Others | 74. 6 ± 69.4 | 4–389 | |||
SD, standard deviation
Analysis among Patients Who Visited One Department Without any Test
There were 4,564 patients who visited only one department without undergoing any test. Table 6 shows the contribution of age group, department group, registration time, and day of the week to a total waiting time. Department group and registration time were the main factors contributing to a longer total waiting time. The total waiting time was significantly longer for patients above 40 years old. Those registered in 5:30–7:30 had a longer total waiting time. The group of “internal medicine” showed the longest waiting time among the department groups. Total waiting times on Tuesday, Thursday, and Friday were significantly longer compared with Monday (Table 6).
Table 6.
Analysis of total waiting time among patients who visited one department with no test (N= 4,564)
| Characteristics | Unadjusted | Adjusteda | |||
|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | ||
| Age group | |||||
| 16–39 years old | 0 | (Reference) | 0 | (Reference) | |
| 40–59 years old | 11.6 | 6.4–16.8** | 5.9 | 0.9–11.0* | |
| 60–80 years old | 22.6 | 17.6–27.5** | 10.8 | 5.8–15.9** | |
| Department group | |||||
| Internal medicine | 0 | (Reference) | 0 | (Reference) | |
| Surgery | -37.2 | -42.3– -32.2** | -33.5 | -38.5– -28.5** | |
| Oncology | -31.6 | -47.8– -15.4** | -33.3 | -49.2– -17.5** | |
| Others | -26.6 | -30.9– -22.4** | -22.9 | -27.2– -18.6** | |
| Registration time | |||||
| 5:30–7:30 | 0 | (Reference) | 0 | (Reference) | |
| 7:31–9:30 | -12.9 | -18.3– -7.7** | -5.8 | -11.1– -0.6* | |
| 9:31–11:00 | -10.1 | -16.9– -3.3** | 1.7 | -5.1–8.5 | |
| 11:01–14:00 | -23.5 | -29.6– -17.5** | -15.4 | -21.4– -9.4** | |
| 14:01–16:00 | -44.4 | -50.9– -37.7** | -32.3 | -39.0– -25.6** | |
| Day of week | |||||
| Monday | 0 | (Reference) | 0 | (Reference) | |
| Tuesday | 9.4 | 3.9–14.9** | 8.2 | 2.9–13.5** | |
| Wednesday | -1.2 | -6.9–4.5 | -2.4 | -7.9–3.0 | |
| Thursday | 15.2 | 9.6–20.9** | 13.9 | 8.6–19.4** | |
| Friday | 19.4 | 13.3–25.6** | 12.5 | 6.5–18.5** | |
* P<0.05, ** P<0.001
CI, confidence interval
aAdjusted for age group, department group, registration time and day of week.
Analysis among Patients Who Visited One Department with One Test
Linear regression analysis using data of patients who visited one department and underwent one test (N=1,259) showed that blood tests and imaging tests were the main factors that influenced a total waiting time, as shown in Table 7. Undergoing a blood test was associated with a significantly longer waiting time than an imaging test. When patients underwent a blood test, their waiting time was prolonged by more than 13.9 times. The group of patients registered between 9:30 and 11:00 waited 28 times longer than those registered between 5:30 and 7:30.
Table 7.
Analysis of total waiting time among patients who visited one department and underwent one test (N=1,259)
| Characteristic | Unadjusted | Adjusteda | |||
|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | ||
| Age Group | |||||
| 16–39 years old | 0 | (Reference) | 0 | (Reference) | |
| 40–59 years old | -2.6 | -14.6–9.4 | -5.9 | -17.6–5.9 | |
| 60–80 years old | 2.7 | -9.6–15.0 | -3.1 | -15.8–9.7 | |
| Department group | |||||
| Internal medicine | 0 | (Reference) | 0 | (Reference) | |
| Surgery | 6.3 | -4.9–17.6 | 10.5 | -0.9–21.9 | |
| Oncology | 26.9 | -14.1–67.9 | 28.1 | -11.5–67.6 | |
| Others | 8.6 | -13.3–30.4 | 15.0 | -6.2–36.3 | |
| Registration time | |||||
| 5:30–7:30 | 0 | (Reference) | 0 | (Reference) | |
| 7:31–9:30 | -8.5 | -19.5–2.4 | -8.9 | -20.5–2.7 | |
| 9:31–11:00 | 28.0 | 9.3–46.7* | 27.2 | 7.3–47.0* | |
| 11:01–14:00 | -64.8 | -80.8– -48.7** | -64.2 | -81.1– -47.4** | |
| 14:01–16:00 | -89.0 | -115.8– -62.1** | -88.6 | -116.1– -61.1** | |
| Day of week | |||||
| Monday | 0 | (Reference) | 0 | (Reference) | |
| Tuesday | 15.1 | 1.0–29.1* | 7.6 | -5.9–21.2 | |
| Wednesday | 9.4 | -5.4–24.3 | 3.2 | -11.1–17.5 | |
| Thursday | 9.1 | -5.5–23.7 | 2.6 | -11.5–16.6 | |
| Friday | 9.2 | -6.1–24.4 | -4.7 | -19.5–10.1 | |
| Test | |||||
| Imaging test | 0 | (Reference) | 0 | (Reference) | |
| Blood test | 13.9 | 4.3–23.4 * | 11.2 | 1.0–21.3* | |
*P< 0.05, ** P< 0.001
CI, confidence interval
aAdjusted for age group, department group, registration time, day of week and test.
DISCUSSION
In this study, we found that age, visited department, registration time, day of the week, and undergoing tests were the factors significantly associated with total waiting time among outpatients at Thong Nhat Hospital. The earlier registration procedure would result in a longer waiting time and this association was significant in two groups of patients (patients who visited one department without undergoing any test and patients who visited one department and underwent one test), suggesting that this association with a long waiting time was independent of having availed tests. This was particularly applicable to most of the patients (64.8%) registered before 9:30 and the reason behind could be that many patients assumed that they would be able to get treatment earlier if they registered early-on. Results of previous studies conducted in Saudi Arabia, Indonesia and China corresponded with the result of this study.5,13,15) However, the result of a study in Bach Mai Hospital, the largest hospital in Ha Noi, the capital of Vietnam, was different. In Bach Mai Hospital, patients who arrived before 8:00 had the shortest waiting time (44 minutes) while patients who came after 11:00 and in the afternoon had the longest (more than 3 hours).16) This difference might be due to the type of systems in hospitals, the number of doctors and clinics, availability of specialists, and/or characteristics of patients. Bach Mai Hospital has 1,800 beds and more medical staffs than Thong Nhat Hospital. The outpatient clinic in Bach Mai Hospital has 70 departments, opens 6 days per week, and begins doctors’ consultations at 6 o’clock, while Thong Nhat Hospital has 20 departments, opens 5 days per week, and begins at 6:30 hours. The larger capacity to intake patients at Bach Mai Hospital might be the reason why patients did not have to wait for a long time early in the morning.
Two of the longest processes were receiving results of blood tests and undergoing imaging tests. This finding was similar to results of the studies conducted at National Dermatology Hospital and Bach Mai Hospital in Vietnam,16,17) although the waiting time to have tests in this study was three times longer than that of the Bach Mai Hospital. The reason is assumed to be a lack of equipment and machines when many patients needed to have the tests. As elderly patients aged 60 to 80 years accounted for 46.3% of the patients, it was assumed that most patients had multiple diseases and needed to undergo tests. Although the reports of laboratory tests were automatically uploaded into the computer system, patients did not know the time when they would have to come back to know the results of blood tests. Making an announcement or displaying the patient’s number on a monitor when their results are available would help to shorten a waiting time to get results of blood tests.
A waiting time was different among various departments with regard to doctors’ consultations. This study showed that the department group of “internal medicine” had the longest waiting time as well as the highest number of patients among patients who visited one department without any test. This was a new finding that a visited department was a factor associated to a longer waiting time. There has been no previous study that has focused on the association between departments and a waiting time. This observation can be explained by the probable existence of an insufficiently running system in which a limited number of medical staff has to accept a large number of patients early in the morning and this might lead to a longer waiting time as compared to the department group of others. These results suggest that the best way to reduce the overload would be increasing the number of rooms and staff of the internal medicine departments.
A previous study has reported that three major factors associated with a long wait time are registration time, insufficient number of physicians, and insufficient number of counter staff.9) Early arrival was found to be one of three challenges related to patient flow in this study as well as in another previous studies.5,18) An appointment system could be recommended that does not permit patients to come earlier than 30 minutes before the scheduled appointment time.5,13) Chen et al. found that a flexible schedule for doctors, which increased the number of doctors early in the morning and reduced in the afternoon, helped in decreasing a waiting time.12) Future studies should evaluate a waiting time before and after interventions and consider total waiting time in various hospitals at different levels of the healthcare system in Vietnam.
This study used the computer system of automatic time recording for evaluating waiting time in all processes of outpatients at a national hospital in Vietnam. To the best of our knowledge, this is the first study in Ho Chi Minh City to use data recorded by the computer system for the evaluation of a waiting time of outpatients in all departments. The data were collected from 7,931 patients and was large enough to evaluate a waiting time. Several previous studies on waiting time were conducted at only outpatient clinics or emergency departments with a limited number of patients’ data or surveys using questionnaires.4,7,17) The limitations of this study, however, are as follows. First, our computer system could not identify a waiting time across different imaging tests and laboratory tests, or record a waiting time at the pharmacy. However, the computer system is useful enough to save lots of time for both medical staffs and patients in recording of data and to reduce human bias. It also helps researchers to extract data and analyze it easily. The existing electronic database systems should be updated to record a waiting time as hospital staff hope. Second, this study was conducted at only one national hospital. The results cannot be generalized to the whole health system of Vietnam, because the distribution of waiting times may be different among hospitals at different levels of the healthcare system. However, most national hospitals have the same over-crowding situation. The methods of this study will help other hospitals to find factors associated to a long waiting time.
In conclusion, this study showed that the mean total waiting time was 104.1 minutes at the outpatient clinic of Thong Nhat Hospital. Older age, visiting internal medicine departments, early registration time, and undergoing tests were significantly associated with a longer total waiting time. Registration time, especially, was found to strongly affect a total waiting time. Based on these results, introduction of an appointment system and announcement of the time to get results of blood test as well as a flexible schedule for doctors may be recommended in order to reduce a waiting time.
CONFLICT OF INTEREST
The author declares no conflict of interest.
ACKNOWLEDGEMENTS
We would like to express sincere gratitude to Young Leaders’ Program, Nagoya University which is supported by Ministry of Education, Culture, Sports, Science and Technology, Japan. We would like to thank Editage (www.editage.jp) for English language editing.
REFERENCES
- 1).Ministry of Health and Joint Partnership Group. Towards Universal Health Coverage. 2013 (in Vietnamese). Available at: http://jahr.org.vn/downloads/JAHR2013/JAHR2013_Final_EN.pdf. Accessed August 1, 2017.
- 2).Oanh TTM, Tuan KA, Phuong H, Phuong NK, Due OT, Hort K. Public hospital governance in Viet Nam: a case study in two provinces. In: Public Hospital Governance in Asia and the Pacific, edited by Huntington D and Hort K. pp. 98–136, 2015, World Health Organization, Geneva. Available at: http://www.wpro.who.int/asia_pacific_observatory/country_comparative_studies/ccs_public_hospital_4_vnm.pdf?ua=1. Accessed August 1, 2017.
- 3).Ministry of Health and Joint Partnership Group. Improving quality of medical services. 2010 (in Vietnamese). Available at: http://jahr.org.vn/downloads/JAHR2012/JAHR2012_Eng_Full.pdf?phpMyAdmin=5b051da883f5a46f0982cec60527c597. Accessed August 1, 2017.
- 4).Cowan RM, Trzeciak S. Clinical review: Emergency department overcrowding and the potential impact on the critically ill. Crit Care, 2005; 9: 291–295. [DOI] [PMC free article] [PubMed]
- 5).Almomani I, AlSarheed A. Enhancing outpatient clinics management software by reducing patients’ waiting time. J Infect Public Health, 2016; 9: 734–743. [DOI] [PubMed]
- 6).Oche M, Adamu H. Determinants of patient waiting time in the general outpatient department of a tertiary health institution in north Western Nigeria. Ann Med Health Sci Res, 2013; 3: 588–592. [DOI] [PMC free article] [PubMed]
- 7).Medway AM, de Riese WT, de Riese CS, Cordero J. Why patients should arrive late: The impact of arrival time on patient satisfaction in an academic clinic. Healthc (Amst), 2016; 4: 188–191. [DOI] [PubMed]
- 8).Khatoon KF, Reddy BK, Guvva S. Reducing Patient Waiting Time in Dental Clinic According to Treatment Type. Int J Com Health and Med Res, 2016; 2: 3–7.
- 9).Babalola D, Meng YX, Nichols M, Omole F, Sow C, Perkins V. Improving the patient flow at an academic primary care teaching clinic serving African American patients. Clin Exp Med Sci, 2013; 1: 241–250.
- 10).Mohebbifar R, Hasanpoor E, Mohseni M, Sokhanvar M, Khosravizadeh O, Mousavi Isfahani H. Outpatient waiting time in health services and teaching hospitals: a case study in Iran. Glob J Health Sci, 2013; 6: 172–180. [DOI] [PMC free article] [PubMed]
- 11).Schachter ME, Romann A, Djurdev O, Levin A, Beaulieu M. The British Columbia Nephrologists’ Access Study (BCNAS) — a prospective, health services interventional study to develop waiting time benchmarks and reduce wait times for out-patient nephrology consultations. BMC Nephrol, 2013; 14: 182. [DOI] [PMC free article] [PubMed]
- 12).Chen BL, Li ED, Yamawuchi K, Kato K, Naganawa S, Miao WJ. Impact of adjustment measures on reducing outpatient waiting time in a community hospital: application of a computer simulation. Chin Med J, 2010; 123: 574–580. [PubMed]
- 13).Sakano N. Introduction of Regional Health Information Network in Vietnam. Fujitsu Sci Tech J, 2015; 51: 84–89.
- 14).Stoop AP, Vrangbaek K, Berg M. Theory and practice of waiting time data as a performance indicator in health care. A case study from The Netherlands. Health Policy, 2005; 73: 41–51. [DOI] [PubMed]
- 15).Mardiah FP, Basri MH. The analysis of appointment system to reduce outpatient waiting time at Indonesia’s public hospital. Human Resour Manage Res, 2013; 3: 27–33.
- 16).Hieu DTN. Waiting time in outpatient clinic in Bach Mai hospital in 2013: Thang Long University; 2013 (in Vietnamese). Available at: https://www.slideshare.net/garmentspace/kho-st-s-hi-lng-ca-bnh-nhn-v-dch-v-khm-cha-bnh-ti-phng-khm-gia-nh-h-ni-nm-2011-69551633. Accessed August 1, 2017.
- 17).Thao NTP, Thang NH. Medical examination time of patients at diagnosis department, national dermatology hospital in 2015. J Practical Med. 2016 (in Vietnamese); 6: 102–109.
- 18).Zhu Z, Heng BH, Teow KL. Analysis of factors causing long patient waiting time and clinic overtime in outpatient clinics. J Med Syst. 2012; 36: 707–713. [DOI] [PubMed]