Abstract
Childhood asthma is responsible for significant morbidity and health care expenditures in the United States. The incidence of asthma is greatest in early childhood, and the prevalence is projected to continue rising in the absence of prevention and intervention measures. The prevention of asthma will likely require a multifaceted intervention strategy; however, few randomized controlled trials have assessed such approaches. The purpose of this review was to use previous meta-analyses to identify the most impactful risk factors for asthma development and evaluate the effect of risk factor reduction on future childhood asthma prevalence. Common and modifiable risk factors with large effects included acute viral respiratory infections, antibiotic use, birth by cesarean section, nutritional disorders (overweight, obesity), second hand smoke exposure, allergen sensitization, breastfeeding, and sufficient prenatal vitamin D level. Evaluation and estimates of risk factor modification on populations at risk should guide scientists and policymakers toward high impact areas that are apt for additional study and intervention.
Electronic supplementary material
The online version of this article (10.1186/s40169-018-0195-4) contains supplementary material, which is available to authorized users.
Keywords: Asthma, Risk factors, Pediatrics
Introduction
Asthma is the leading chronic disease among children, affecting 8.4% of children in the United States and up to 14% worldwide [1, 2]. The economic impact and loss of productivity are enormous compared to other childhood illnesses [3]. The overall prevalence of asthma in the US has been increasing over the past 30 years in all demographic groups [4]. A similar increase in prevalence is noted throughout the developing world, although the association with economic development is not uniform [5]. Currently there are no demonstrated effective interventions for the primary prevention of asthma [6].
The rise in asthma and allergy prevalence is happening at a rate that cannot be fully explained by genetic factors. Although a positive family history is a highly predictive risk factor, its positive predictive value for the development of childhood asthma only ranges from 11 to 37%. The marked increase in prevalence over a short time period suggests that multiple environmental risk factors are driving an upward trend in prevalence that cannot be explained by genetic factors alone [7]. In utero or early life risk factors for asthma include maternal health and stress, mode of delivery, exposure to environmental pollutants and allergens, obesity, diet, and exposure to infections and antibiotics, among others. The risk of developing childhood asthma likely depends on a combination of host factors and their interaction with a multitude of environmental factors rather than one single risk factor; however, data on the differential and combined impact of risk factors is lacking [8].
Finland faced a similar public health crisis in 1972 when confronted with very high cardiovascular disease mortality rates. Similar to asthma, the development of cardiovascular disease requires the interaction of multiple genetic and environmental factors, including tobacco use, obesity, physical inactivity, hypercholesterolemia, hypertension, and diabetes. Leaders of the North Karelia Project targeted multiple risk factors and implemented policies on a community and national level, including anti-smoking legislation and strict school meal nutritional requirements. The cardiovascular mortality rate decreased by 65% over the next 2 decades, demonstrating that population-based public health interventions are an effective strategy for prevention of a gene by environment disease [9].
The prevention of asthma will likely require a similar multi-faceted approach, targeting multiple relevant risk factors to prevent disease. The aim of this review is to estimate the impact of modifying risk factor exposure on future childhood asthma development with population level estimates to examine the policy implications of these projections. This paper is the first to use pre-existing data to identify the most impactful risk factors of childhood asthma, and to estimate the effect of risk factor reduction on disease prevalence.
Methods
Search strategy and inclusion criteria
We conducted a search of the PubMed database from 1990 to October 2017 to identify meta-analyses evaluating the association between individual risk factors and asthma development. We used the search term “asthma” and restricted the results to meta-analyses, children or adolescents (0–18 years), and articles published in English. A second search was completed and limited to meta-analyses and female gender to capture maternal pregnancy risk factors. Inclusion of abstracts identified by the initial screen was based on specific criteria: (1) published by a peer-reviewed journal; (2) provided a point estimate such as odds ratio with corresponding 95% confidence intervals (CI); and (3) outcomes were assessed in children or adolescents. The outcome of interest was the risk of developing incident asthma in childhood. For risk factors with more than one meta-analysis available for review, we selected either the most recent analysis or that with the largest study population. The characteristics derived from each selected article included the type of risk factor, study authors, year of publication, size of the study population, definition of asthma diagnosis, and odds ratio estimates with corresponding 95% CI.
Prevalence of risk factors
The prevalence of each risk factor in the US population was identified through a comprehensive literature and database review. Risk factor prevalence estimates were restricted to an age group window for which data was available, and reflect the age ranges in the meta-analyses that we used. The four age exposure windows were prenatal, 0–1, < 5, and 5–13 years. In the absence of risk factor prevalence data for a specific exposure window, prevalence estimates for children 0–18 years of age were applied to the 5–13 years group. The impacted population size of each risk factor was calculated using 2015 Centers for Disease Control National Vital Statistics System (NVSS) birth data and 2010 US Census data [10, 11]. The total number of live births from the 2015 NVSS was used to calculate the impacted population size for prenatal and infant risk factors.
Data analysis: population attributable fraction
The contribution of a specific risk factor to the burden of asthma in the population was quantified using population attributable fraction (PAF). PAF is a useful public health tool because it measures the proportion of cases that could be prevented by eliminating a risk factor through control measures in a target population. The calculation of PAF assumes a causal relationship between a risk factor and a disease; however, asthma is a multifactorial disease likely caused by multiple additive factors [12]. A similar methodology has been used to estimate the impact of risk factor reduction on the prevalence of Alzheimer’s disease and cardiovascular disease [13, 14]. A formula proposed by Levin in 1953 was used to calculate the PAF for each risk factor:
Levin’s formula relies on the prevalence of risk factor exposure in the population (PRF) and the strength of the association between a risk factor and disease (OR, odds ratio) [15]. Although the original formula included relative risk as a measure of association, we used odds ratios as an estimate of relative risk based on the available data in the studies meeting criteria for inclusion.
The total number of cases attributable to each risk factor was obtained by multiplying the PAF for each risk factor by the total number of incident asthma cases in children ages 5–11. This age group was selected for two reasons. First, the onset of asthma occurs before 8 years of age in 80% of cases [16]. Second, the best available asthma prevalence data for children under 8 years is reflected by the prevalence of asthma in the United States between the ages of 5 and 11–9.6% or approximately 2.76 million children [1]. We then projected the impact of a 10 and 25% reduction in the prevalence of individual risk factors on the total number of attributable cases by re-calculating the PAF for each risk factor using reduced prevalence estimates.
Results
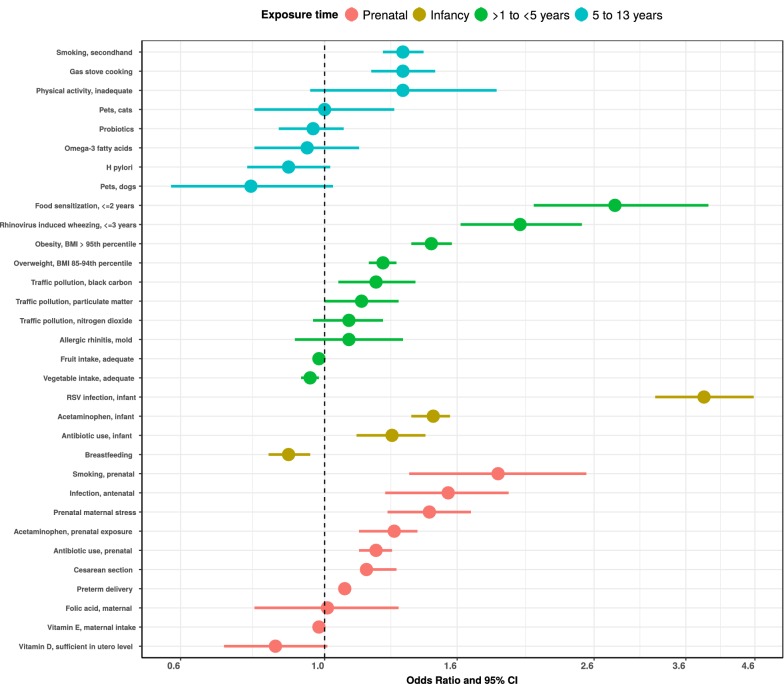
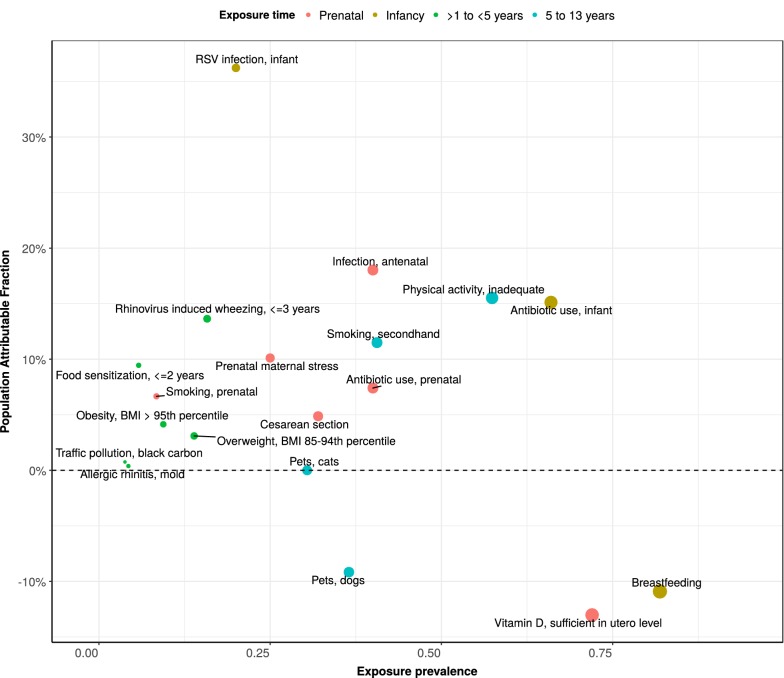
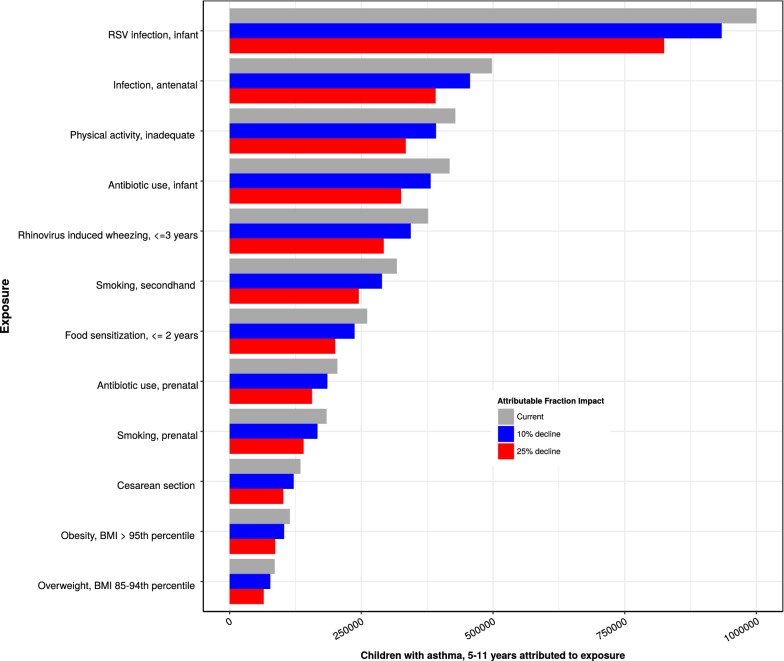
We identified thirty-two meta-analyses examining the association between individual risk factors and asthma development. Additional file 1: Table S1 presents the odds ratios and prevalence data for each risk factor used in the analysis. Figure 1 illustrates the strength and direction of each associated risk factor on asthma development by age exposure window and descending order of effect size. The risk factors with the strongest association, based on the size of the odds ratio, were prenatal maternal smoking, infant RSV infection, food allergen sensitization in early childhood, secondhand smoke exposure, and physical inactivity in late childhood. However, these odds ratios do not take into account the prevalence of risk factor exposure and do not reflect the population attributable fraction (PAF). Figure 2 uses PAF and exposure prevalence to illustrate the impact of each modifiable risk factor on asthma development in the population. PAF provides an indication of the potential percent reduction in incidence of asthma in a given population if the exposure is causal and is eliminated. There is no pre-specified way of evaluating the importance of PAF. Therefore, the magnitude of the PAF and exposure prevalence were evaluated relative to other risk factors in the same age exposure window. Risk factors with a high PAF, high exposure prevalence, and high modifiable impact are the most important public health targets. These risk factors include acute viral respiratory infections, antibiotic use, birth by cesarean section, nutritional disorders (overweight, obesity), second hand smoke exposure, and allergen sensitization. Equally important are risk factors with a protective effect such as breastfeeding and sufficient maternal vitamin D levels. Figure 3 shows the effect of a 10 and 25% reduction in specific, modifiable risk factors on the estimated number of children between 5 and 11 years of age with asthma attributable to the risk factor. Assuming each risk factor plays an independent role, approximately 51% of asthma cases are attributable to two exposures that occur during infancy (RSV lower respiratory tract infection and antibiotic use).
Fig. 1.
Association of risk factors for asthma development within age exposure windows. The four age exposure windows are prenatal, 0–1, < 5, and 5–13 years. Odds ratios and 95% confidence intervals are shown ranked by effect size and directionality. References used to determine point estimates for this figure: smoking, secondhand [69]; gas stove cooking [96]; physical activity, inadequate [64]; pets, cats [57]; probiotics [97]; omega-3 fatty acids [98]; H. pylori [99]; pets, dogs [57]; food sensitization, ≤ 2 years [77]; rhinovirus induced wheezing, ≤ 3 years [24]; obesity [65]; overweight [65]; traffic pollution [100]; allergic rhinitis, mold [101]; fruit intake, adequate [102]; vegetable intake, adequate [102]; RSV infection, infant [23]; acetaminophen, infant [103]; antibiotic use, infant [45]; breastfeeding [88]; smoking, prenatal [70]; infection, antenatal [104]; prenatal maternal stress [105]; acetaminophen, prenatal [103]; antibiotic use, prenatal [44]; cesarean section [37]; preterm delivery [106]; folic acid, maternal [107]; vitamin E, maternal intake [92]; vitamin D, sufficient in utero level [108]
Fig. 2.
Population attributable fraction (PAF) among selected risk factors. PAF, the proportion of cases that are attributable to a risk factor and could be prevented by modifying or eliminating the risk factor, is shown on the y-axis. The x-axis represents the risk factor exposure prevalence. The points on the graph reflect the relationship of exposure prevalence and PAF. The PAF is dependent on the prevalence of exposure and its odds ratio for asthma. The size of the points are proportional to prevalence. Odds ratios from meta-analyses were used to estimate PAF (Additional file 1: Table S1 and Fig. 1). References used to determine exposure prevalence for this figure: smoking, secondhand [71]; gas stove cooking [109]; physical activity, inadequate [110]; pets, cats [111]; probiotics [112]; omega-3 fatty acids [112]; H. pylori [113]; pets, dogs [111]; food sensitization, ≤ 2 years [114]; rhinovirus induced wheezing, ≤ 3 years [29, 30]; obesity [61]; overweight [115]; traffic pollution [116]; allergic rhinitis, mold [117]; fruit intake, adequate [118]; vegetable intake, adequate [118]; RSV infection, infant [28]; acetaminophen, infant [119]; antibiotic use, infant [42]; breastfeeding [87]; smoking, prenatal [72]; infection, antenatal [41]; prenatal maternal stress [120]; acetaminophen, prenatal [121]; antibiotic use, prenatal [41]; cesarean section [72]; preterm delivery [72]; folic acid, maternal [122]; vitamin E, maternal intake [123]; vitamin D, sufficient in utero level [124]
Fig. 3.
Impact of reducing selected risk factor exposure on asthma cases among children 5–11 years of age. Based on an asthma prevalence of 9.6% from the Centers for Disease Control and Prevention to estimate 2,761,000 children with asthma. Twelve risk factors were selected for ranking based on their effect size, prevalence of exposure, and potential for modification. This figure considers only the main effect of the risk factor (without accounting for potential interactions)
Discussion
The greatest incidence of asthma development occurs during early childhood [17]. The risk of asthma onset is likely influenced by gene-environment interactions. The goal of primary prevention is to prevent the development of disease by identifying and reducing modifiable risk factors within the environment [18]. Given the complexity in identifying candidate genes that predict who will develop asthma, preventive strategies should focus on primary prevention of prenatal and early childhood risk factors with a high population attributable fraction. However, there are a limited number of randomized controlled trials assessing the efficacy of such interventions on asthma incidence. The Canadian Asthma Primary Prevention Study (CAPPS), one of the only multifaceted intervention trials in asthma, showed that multiple interventions before birth and through the 1st year of life could reduce the prevalence of childhood asthma by 7 years of age [19]. Our study is the first to use pre-existing study results to identify the most impactful risk factors for childhood asthma, and to estimate the effect of potential targeted intervention strategies on disease prevalence.
Based on the effect size as a measure of association with outcome, prevalence of exposure, and potential for modification, the following risk factors were found to have the largest impact on childhood asthma development: acute viral respiratory infections, antibiotics, birth by cesarean section, nutritional disorders (overweight, obesity), second hand smoke exposure, and allergen sensitization. These will be discussed below.
Acute viral respiratory infections
Acute respiratory infections (ARI) are the leading cause for ambulatory visits and hospitalizations in infants [20, 21]. Respiratory syncytial virus (RSV) and human rhinovirus (HRV) are the most commonly detected viruses during infant ARIs. RSV is the primary etiology of infant lower respiratory tract infection (LRTI) that may require hospitalization in severe cases while HRV may cause LRTI, but more often leads to a mild upper respiratory infection [22]. In addition to the increased burden in the acute care setting, both RSV and HRV lower respiratory tract infections are strongly associated with the development of early childhood wheezing and asthma [23, 24]. However, it is unclear whether the association is the result of a genetic predisposition or directly attributable to the virus. Two previous studies found that the administration of RSV immunoprophylaxis to preterm infants was associated with a reduction in recurrent wheezing, suggesting a potential causal role of RSV LRTI in the development of asthma [25, 26]. Similar observational or intervention studies do not yet exist to support a definitive relationship associating HRV with asthma [27].
Our analysis indicates that the largest proportion of childhood asthma in the United States is attributable to RSV infection during infancy. Both RSV and HRV are highly prevalent and potentially modifiable risk factors in early childhood. The prevalence of RSV LRTI is 20% in the 1st year of life, whereas the prevalence of HRV-induced wheezing is 15.8% in the first 3 years of life [28–30]. Current strategies to prevent RSV infection include avoidance of exposure, reduction of tobacco smoke exposure, birth timing, and passive immunization with RSV immunoprophylaxis. RSV immunoprophylaxis is effective in reducing morbidity in infants; however, the high total cost and burden of administration limit its use to high-risk children. While there is strong evidence that RSV is a causal factor in asthma development, whether prevention of RSV can significantly reduce the risk of developing asthma is a question best addressed by a randomized controlled trial [31]. Future research should also be directed toward the prevention of RSV through active immunization of infants and/or pregnant women and study of the longer term effects on childhood asthma development. The implementation of influenza and tetanus-diphtheria-acellular pertussis vaccination programs for pregnant women is a successful model for the protection of both the mother and infant [32]. There are currently 10 candidate RSV vaccines in ongoing clinical trials, including 3 maternal vaccines and 7 pediatric vaccines [33]. The development of active and passive immunization strategies against HRV lags behind RSV, and is limited by the sheer number of viral serotypes and lack of cross-protective immunity between serotypes [34].
Perinatal events
The cesarean birth rate has increased from 4.5% in 1965 to 32% in 2015 without a significant improvement in maternal or infant outcomes over the past 10 years [35, 36]. Based on a recent meta-analysis, infants born via cesarean section had an approximately 20% increase in the onset of asthma [37]. These children are also at higher risk for other chronic diseases such as diabetes and obesity, so a reduction in exposure should result in multiple health benefits [38]. The American College of Obstetricians and Gynecologists led the charge to decrease cesarean delivery in 2013 by recommending against elective cesarean delivery prior to 39 weeks of gestation due to the risk of complications [39]. National organizations, health care systems, and individual providers could also re-evaluate current delivery practices to reduce the cesarean birth rate. In addition, all health care systems could proactively release metrics on deliveries to enhance transparency and enable data-driven quality improvement, as is required of hospitals accredited by The Joint Commission [40].
Equally alarming is the rising rate of antibiotic use in the United States. Antibiotic use during pregnancy is reported in 40% of women and in 66% of infants in the 1st year of life [41, 42]. The Centers for Disease Control and Prevention (CDC) reports that at least 30% of all outpatient antibiotics are incorrectly prescribed for the management of viral infections. Inappropriate antibiotic use increases the risk of short-term and long-term complications, including alteration of the infant microbiome [43]. The relative risk of asthma development is increased by 20% in infants exposed to antibiotics in utero and 27% in infants exposed to antibiotics within the 1st year with a very strong dose response relationship [44–46]. Similar to cesarean delivery, infant and prenatal antibiotic use is associated with a multitude of chronic health conditions including inflammatory bowel disease, obesity, and diabetes [47]. All members of the health care team have a role in antibiotic stewardship. Health care systems should provide adequate education and feedback to providers. Providers should use strategies such as watchful waiting and frequent reassessment of need, and patients should be fully engaged in the decision making process [43].
One theory suggests that the effect of cesarean delivery and antibiotics on the development of the immune system is due to alteration of the microbiome. The human microbiome is a collection of symbiotic microorganisms located in the skin, respiratory tract, gastrointestinal tract, and genitourinary tract. Commensal bacteria contribute to human health by performing essential metabolic functions and modulating the emerging immune system [48]. Dysbiosis, or a derangement in the composition of commensal bacteria, can be induced by several environmental factors including cesarean birth, antibiotic use, and dietary changes [49]. The infant microbiome varies predictably depending on the mode of delivery, and recent studies suggest that vaginal microbial transfer may partially restore the microbiome of cesarean-born infants [50, 51]. Another potential mechanism of asthma development due to cesarean delivery is alteration of early air-lung exchange by retention of amniotic fluid in the infant lungs [52]. Pre- and post-natal antibiotic exposure is similarly associated with reduced diversity of the newborn intestinal flora [53]. The clinical relevance of dysbiosis is illustrated by the hygiene hypothesis, which postulates that a lack of early life exposure to a microbe rich environment favors the development of asthma [54]. Growing up in a microbe rich environment, such as a farm, appears to be protective against developing asthma; however, there is no meta-analysis for inclusion into this paper and randomized controlled trials are ongoing [55]. A current clinical trial aims to determine whether administration of an oral bacterial extract to high risk infants can prevent the development of wheezing respiratory illness and asthma [56]. Another microbe rich environment includes pet ownership. A recent meta-analysis failed to find a strong association between pet ownership and a reduction in asthma risk; however, there are studies that suggest a protective effect of dogs [57–59].
Obesity
Childhood obesity is a modern public health crisis. In children, obesity is defined as a body mass index (BMI) greater than the 95th percentile for age and gender [60]. The prevalence of obesity among children < 5 years of age has doubled from 4.8 to 9.4% over the past 40 years [61]. This increase is most likely due to a combination of complex factors including physical inactivity, altered dietary patterns, and other environmental exposures. Moreover, childhood obesity contributes to the development of asthma, sleep apnea, diabetes mellitus, and cardiovascular disease [62]. The mechanism linking obesity and asthma is poorly understood, but likely related to the pro-inflammatory effects of adipose tissue [63]. Other drivers of obesity, including physical inactivity and overweight status, also have a similar impact on asthma development [64, 65].
Body mass index is the recommended method of screening for obesity beginning at 2 years of age. Current management focuses on mitigating disease severity through secondary and tertiary prevention strategies such as dietary and lifestyle modifications. Pediatricians can play an important role by recommending increased physical activity, avoidance of sweetened beverages, and elimination or reduction of television exposure [66]. However, public health campaigns must also ensure that all children have access to affordable, nutritious food and after school programs that allow at least 60 min of daily exercise in a safe environment. In addition, local school systems should consider implementing multifaceted school-based programs given their effectiveness in the primary prevention of childhood obesity. However, these programs require significant involvement of both parents and educators and may be less cost-effective than other interventions such as lifestyle modifications [67, 68].
Second hand smoke exposure
Pre- and post-natal exposure to tobacco smoke has long been recognized as a risk factor for the development of asthma. The risk of asthma onset is increased by 85% in infants exposed to maternal smoking during pregnancy and by 32% in children exposed to secondhand smoke [69, 70]. These findings are especially troubling given the prevalence of tobacco smoke exposure is 8.4% prenatally and 40.6% between 5 and 13 years of age [71, 72]. Screening caregivers for the use of tobacco products is an obligation of all medical providers [73]. Current therapeutic recommendations focus on proven strategies such as cessation counseling and pharmacotherapy; however, additional policies and funding are needed to increase access and affordability of these services. Reducing the overall prevalence of tobacco use will likely require increased regulation by policymakers such as implementing more robust smoke-free laws, raising cigarette list prices or taxes, and further limiting tobacco advertisements [74]. Parental smoking is a modifiable predictor of smoking initiation during adolescence, so preventing parental smoking is also of critical importance to the long-term behavior of children [75].
Allergen sensitization
The rise of food allergy over the past 20 years parallels the increasing prevalence of childhood asthma in the United States [76]. Recent studies show that food allergen sensitization prior to 2 years of age is a significant risk factor for the development of asthma; however, it is unclear whether this is an independent risk factor or another disease in the atopic march [77]. The recent increase in food allergy may be attributable to previous guidelines that recommended delayed introduction of allergenic foods until after the 1st year of life [78]. More recently, the Learning Early About Peanut Allergy (LEAP) study found that the early introduction of peanut between 4 and 11 months of age in low- and moderate-risk children reduced the onset of peanut allergy [79]. Pediatricians can play a critical role in the prevention of food allergy. The National Institute of Allergy and Infectious Disease recommends early introduction of peanut-containing foods between 4 and 6 months of age to high-risk infants after evaluation for allergy testing and around 6 months for infants with mild-to-moderate eczema [80]. There are ongoing trials studying the efficacy of oral, sublingual, and epicutaneous immunotherapy in the primary prevention of peanut allergy; however, no specific therapy is on the market and it is unknown whether there will be an impact on asthma development [81].
Early sensitization to perennial aeroallergens is associated with an increased risk of asthma development [82]. Exposure to house dust mite (HDM) has been shown to be an important predictor of childhood asthma in multiple studies [83, 84]. Two multifaceted intervention trials that included HDM avoidance were associated with a decreased prevalence of asthma; however, it is less clear whether HDM avoidance alone would have the same effect [19, 85]. In addition, an ongoing clinical trial aims to evaluate whether blocking IgE with omalizumab can prevent progression to asthma in preschool children with wheezing respiratory illness and aeroallergen sensitization [86]. There are no current recommendations for strategies to prevent aeroallergen sensitization; however, patients should be educated on avoidance techniques for seasonal and perennial allergens once diagnosed.
Protective factors
Our review revealed two factors that may be protective against the development of childhood asthma: breastfeeding and sufficient prenatal vitamin D level. These are cost-effective, easily implemented interventions that could offer potential benefit with low risk. Breastfeeding rates vary by duration with 81.9% of infants initiating at birth, 60.6% up to 6 months, and 34.1% up to 1 year [87]. Breastmilk provides early passive immunity through the biologic activity of immunoglobulins; however, the mechanism for protection from asthma and other allergic disorders is unclear [88]. Based on guidelines from the American Academy of Pediatrics, providers should strongly recommend exclusive breastfeeding for at least 6 months with mixed feeding including breastmilk through 12 months [89].
Vitamin D levels are insufficient in approximately 28% of pregnant women between 12 and 44 years of age [90]. Multiple studies suggest a protective effect of higher levels of in utero 25-hydroxy-vitamin D against the development of asthma. Combined analysis of two recent randomized controlled trials showed that prenatal vitamin D supplementation may reduce the risk of childhood asthma [91]. Providers should ensure that women of childbearing age are taking routine prenatal vitamins; however, the need for additional vitamin D supplementation to prevent asthma has yet to be determined. Increased maternal intake of vitamin E (alpha-tocopherol) during pregnancy is associated with protection against early childhood wheezing, but has not been definitively shown to protect against the development of childhood asthma [92]. More than 90% of adults in the United States who do not use supplements fail to meet recommended intake of vitamin E and D, but could with supplementation [93].
Limitations
Several assumptions were made to perform this analysis. First, the use of population attributable fraction (PAF) assumes a causal relationship between risk factor exposure and the development of asthma. Asthma, similar to cardiovascular disease, is likely the result of multiple, interacting risk factors. PAF estimates the proportion of disease that could be eliminated if the risk factor is removed; however, the absence of causality diminishes its value. We have previously reviewed the available levels of causal evidence for many of these risk factors [94, 95]. We are not implying causality is a settled matter for all of the discussed risk factors; however, our intent was to guide policymakers and scientists using a novel analytic plan. Second, the robustness of the PAF calculation is dependent on the strength of the meta-analysis and accuracy of the risk factor prevalence data. Prevalence data can vary based on the population being assessed. We limited our analysis to childhood risk factors for which there was a meta-analysis in order to improve statistical precision. We chose to focus on childhood risk factors because most children experience asthma symptoms by 6 years of age. However, this exclusion criterion eliminated many potentially modifiable risk factors for which no meta-analysis exists. For each risk factor, we selected the meta-analysis that was either the most recent or had the largest study population, knowing that each study may be limited by methodology and subject to confounding. A detailed assessment of each meta-analysis for confounding was not completed given the study was designed to highlight key areas and opportunities for targeted studies to support causal relationships and public health interventions. Therefore, the results should be interpreted with caution given the extent of confounding or reverse causation may vary depending on the risk factor. For example, the association between inadequate physical activity and asthma may be due to exercise limitation from poor symptom control, an example of reverse causation. Prenatal risk factors, such as antibiotic use, cesarean section, and maternal stress, are not subject to reverse causation. However, socioeconomic status as a potential confounder may not have been controlled for in individual studies within a meta-analysis. The upward bias of meta-analyses is an important limitation in using this type of data; however, use of summary data from meta-analyses is a means of incorporating a summary effect size of the available published studies. We are less concerned about an upward bias related to RSV infection because it meets many of the Bradford Hill criteria for causality, compared with a number of risk factors for which there have not been studies conducted to fully support causal relationships. Third, the Levin formula uses unadjusted relative risk to calculate PAF; however, we used odds ratio given it was consistently available across all the included meta-analyses. Odds ratio may overestimate the risk ratio when an outcome is common in a study population. Fourth, risk factor prevalence estimates were based on the best available and most recent data. We were unable to calculate age-standardized rates; therefore, estimates were sorted into the age group for which data was available. This allowed for comparison of PAF within each exposure window since PAF estimates do not take into account the size of the population affected by a risk factor. The impacted population size for prenatal and infant risk factors was calculated using the total number of live births rather than the total number of pregnancies given the focus was on the development of asthma in living children. Fifth, while we provide impact estimates of relevant risk factors based on their strong association and high prevalence, these estimates do not replace the necessity of randomized controlled trials to determine the effect of risk factor modification on future asthma prevalence. Finally, we understand that there are many issues that are likely to affect the success of primary prevention efforts, including a better understanding of the phenotypes of asthma, selecting target risk populations for exposure specific interventions, heterogeneity in treatment effects, mediating effects, etc. For a large list of risk factors, it is not possible to include all of this evidence in a single review. Therefore, we chose to focus on what we believe is the most important in informing the next needed steps in the field—a focus on risk factors that are prevalent, modifiable, and have a large effect size, and to present the data on their potential impact on asthma incidence using PAF. Regarding the overall contribution of PAF, the magnitude of the impact of asthma as a lifelong chronic disease is sufficiently large that even a small reduction in true asthma incidence would have major health implications. Our hope is that the novel compilation of data will inform and prioritize the field toward studies to confirm causality and to conduct public health interventions for primary disease prevention.
Conclusion
In the United States, a significant proportion of childhood asthma may be attributable to modifiable risk factors including acute viral respiratory infections, antibiotic use, birth by cesarean section, obesity, second hand smoke exposure, and allergen sensitization. Breastfeeding and sufficient prenatal vitamin D concentrations may be protective against asthma onset. In the absence of effective primary prevention strategies, current management focuses on reducing the impairment and risk associated with asthma. However, this study shows that multifactorial prevention of early childhood risk factors could reduce the future prevalence of asthma. Additional randomized controlled trials are needed to provide evidence of causality of the risk factor-disease relationship and to identify effective preventive strategies. Causal evidence and controlled trials of known asthma risk factors will be essential in driving policymakers to create more effective community-based programs and public health strategies targeting high prevalence risk factors with high population attributable fraction.
Additional file
Additional file 1: Table S1. Meta-analyses and exposure prevalence data of risk factors for childhood asthma development.
Authors’ contributions
TH conceptualized the manuscript. AA collected the relevant articles and drafted the manuscript. TG conducted the analyses and contributed to manuscript development. TH made significant revisions to the manuscript. CS contributed to development of the initial methodology and edited the manuscript. All authors edited the final manuscript prior to submission. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data used in this review is from published meta-analyses.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
This work was supported in part by the National Institutes of Health: NIH K24 AI 077930 (TH). Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Institutes of Health.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- CI
confidence interval
- NVSS
National Vital Statistics System
- PAF
population attributable fraction
- PRF
prevalence of risk factor exposure in the population
- OR
odds ratio
- CAPPS
Canadian Asthma Primary Prevention Study
- ARI
acute respiratory infection
- RSV
respiratory syncytial virus
- HRV
human rhinovirus
- LRTI
lower respiratory tract infection
- CDC
Centers for Disease Control and Prevention
- BMI
body mass index
- LEAP
Learning Early About Peanut Allergy
- HDM
house dust mite
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s40169-018-0195-4) contains supplementary material, which is available to authorized users.
Contributor Information
Andrew Abreo, Email: andrew.abreo@vanderbilt.edu.
Tebeb Gebretsadik, Email: tebeb.gebretsadik@Vanderbilt.edu.
Cosby A. Stone, Email: cosby.a.stone@vanderbilt.edu
Tina V. Hartert, Email: tina.hartert@vanderbilt.edu
References
- 1.Centers for Disease Control and Prevention. Most recent asthma data. https://www.cdc.gov/asthma/most_recent_data.htm. Accessed 11 Oct 2017
- 2.Lai CK, Beasley R, Crane J, Foliaki S, Shah J, Weiland S, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the international study of asthma and allergies in childhood (ISAAC) Thorax. 2009;64(6):476–483. doi: 10.1136/thx.2008.106609. [DOI] [PubMed] [Google Scholar]
- 3.Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009;9:24. doi: 10.1186/1471-2466-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012;35:1–58. [PubMed] [Google Scholar]
- 5.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services National Heart, Lung, and Blood Institute. Expert panel report 3: guidelines for the diagnosis and management of asthma. 2007. https://www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines/full-report. Accessed 24 Oct 2017
- 7.Burke W, Fesinmeyer M, Reed K, Hampson L, Carlsten C. Family history as a predictor of asthma risk. Am J Prev Med. 2003;24(2):160–169. doi: 10.1016/S0749-3797(02)00589-5. [DOI] [PubMed] [Google Scholar]
- 8.Wong GW, Chow CM. Childhood asthma epidemiology: insights from comparative studies of rural and urban populations. Pediatr Pulmonol. 2008;43(2):107–116. doi: 10.1002/ppul.20755. [DOI] [PubMed] [Google Scholar]
- 9.Puska P, Vartiainen E, Tuomilehto J, Salomaa V, Nissinen A. Changes in premature deaths in Finland: successful long-term prevention of cardiovascular diseases. Bull World Health Organ. 1998;76(4):419–425. [PMC free article] [PubMed] [Google Scholar]
- 10.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep. 2017;66(1):1. [PubMed] [Google Scholar]
- 11.United States Census Bureau. Annual estimates of the resident population for selected age groups by sex for the United States April. 2010. https://factfinder.census.gov. Accessed 14 Nov 2017
- 12.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15–19. doi: 10.2105/AJPH.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10(9):819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sacco RL, Roth GA, Reddy KS, Arnett DK, Bonita R, Gaziano TA, et al. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American heart association and world heart federation. Circulation. 2016;133(23):e674–e690. doi: 10.1161/CIR.0000000000000395. [DOI] [PubMed] [Google Scholar]
- 15.Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 1953;9(3):531–541. [PubMed] [Google Scholar]
- 16.Morgan WJ, Stern DA, Sherrill DL, Guerra S, Holberg CJ, Guilbert TW, et al. Outcome of asthma and wheezing in the first 6 years of life: follow-up through adolescence. Am J Respir Crit Care Med. 2005;172(10):1253–1258. doi: 10.1164/rccm.200504-525OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The group health medical associates. N Engl J Med. 1995;332(3):133–138. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 18.Joseph CL, Williams LK, Ownby DR, Saltzgaber J, Johnson CC. Applying epidemiologic concepts of primary, secondary, and tertiary prevention to the elimination of racial disparities in asthma. J Allergy Clin Immunol. 2006;117(2):233–240. doi: 10.1016/j.jaci.2005.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan-Yeung M, Ferguson A, Watson W, Dimich-Ward H, Rousseau R, Lilley M, et al. The Canadian childhood asthma primary prevention study: outcomes at 7 years of age. J Allergy Clin Immunol. 2005;116(1):49–55. doi: 10.1016/j.jaci.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 20.Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008;121(2):244–252. doi: 10.1542/peds.2007-1392. [DOI] [PubMed] [Google Scholar]
- 21.Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001–02. Vital Health Stat 13. 2006;159:1–66. [PubMed] [Google Scholar]
- 22.Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. 2010;23(1):74–98. doi: 10.1128/CMR.00032-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Regnier SA, Huels J. Association between respiratory syncytial virus hospitalizations in infants and respiratory sequelae: systematic review and meta-analysis. Pediatr Infect Dis J. 2013;32(8):820–826. doi: 10.1097/INF.0b013e31829061e8. [DOI] [PubMed] [Google Scholar]
- 24.Liu L, Pan Y, Zhu Y, Song Y, Su X, Yang L, et al. Association between rhinovirus wheezing illness and the development of childhood asthma: a meta-analysis. BMJ Open. 2017;7(4):e013034. doi: 10.1136/bmjopen-2016-013034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wenzel SE, Gibbs RL, Lehr MV, Simoes EA. Respiratory outcomes in high-risk children 7 to 10 years after prophylaxis with respiratory syncytial virus immune globulin. Am J Med. 2002;112(8):627–633. doi: 10.1016/S0002-9343(02)01095-1. [DOI] [PubMed] [Google Scholar]
- 26.Simoes EA, Groothuis JR, Carbonell-Estrany X, Rieger CH, Mitchell I, Fredrick LM, et al. Palivizumab prophylaxis, respiratory syncytial virus, and subsequent recurrent wheezing. J Pediatr. 2007;151(1):34–42. doi: 10.1016/j.jpeds.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 27.Stone CA, Jr, Miller EK. Understanding the association of human rhinovirus with asthma. Clin Vaccine Immunol. 2015;23(1):6–10. doi: 10.1128/CVI.00414-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics . Respiratory syncytial virus. In: Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Red book: 2015 report of the committee on infectious diseases. 30. Elk Grove Village: American Academy of Pediatrics; 2015. pp. 667–676. [Google Scholar]
- 29.Busse WW, Lemanske RF, Jr, Gern JE. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376(9743):826–834. doi: 10.1016/S0140-6736(10)61380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Aalderen WM. Childhood asthma: diagnosis and treatment. Scientifica (Cairo) 2012;2012:674204. doi: 10.6064/2012/674204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu P, Hartert TV. Evidence for a causal relationship between respiratory syncytial virus infection and asthma. Expert Rev Anti Infect Ther. 2011;9(9):731–745. doi: 10.1586/eri.11.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neuzil KM. Progress toward a respiratory syncytial virus vaccine. Clin Vaccine Immunol. 2016;23(3):186–188. doi: 10.1128/CVI.00037-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mazur NI, Martinon-Torres F, Baraldi E, Fauroux B, Greenough A, Heikkinen T, et al. Lower respiratory tract infection caused by respiratory syncytial virus: current management and new therapeutics. Lancet Respir Med. 2015;3(11):888–900. doi: 10.1016/S2213-2600(15)00255-6. [DOI] [PubMed] [Google Scholar]
- 34.McLean GR. Developing a vaccine for human rhinoviruses. J Vaccines Immun. 2014;2(3):16–20. doi: 10.14312/2053-1273.2014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taffel SM, Placek PJ, Liss T. Trends in the United States cesarean section rate and reasons for the 1980–85 rise. Am J Public Health. 1987;77(8):955–959. doi: 10.2105/AJPH.77.8.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American College of O, Gynecologists, Society for Maternal-Fetal M Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123(3):693–711. doi: 10.1097/01.AOG.0000444441.04111.1d. [DOI] [PubMed] [Google Scholar]
- 37.Huang L, Chen Q, Zhao Y, Wang W, Fang F, Bao Y. Is elective cesarean section associated with a higher risk of asthma? A meta-analysis. J Asthma. 2015;52(1):16–25. doi: 10.3109/02770903.2014.952435. [DOI] [PubMed] [Google Scholar]
- 38.Blustein J, Liu J. Time to consider the risks of caesarean delivery for long term child health. BMJ. 2015;350:h2410. doi: 10.1136/bmj.h2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American College of O, Gynecologists ACOG committee opinion no. 559: cesarean delivery on maternal request. Obstet Gynecol. 2013;121(4):904–907. doi: 10.1097/01.AOG.0000428647.67925.d3. [DOI] [PubMed] [Google Scholar]
- 40.Joint Commission on Accreditation of Healthcare Organizations. Specifications manual for joint commission national quality measures (v2017A1). 2017. https://manual.jointcommission.org/releases/TJC2017A1/index.html. Accessed 28 Dec 2017
- 41.Ledger WJ, Blaser MJ. Are we using too many antibiotics during pregnancy? BJOG. 2013;120(12):1450–1452. doi: 10.1111/1471-0528.12371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinlaw AC, Sturmer T, Lund JL, Pedersen L, Kappelman MD, Daniels JL, et al. Trends in antibiotic use by birth season and birth year. Pediatrics. 2017;140(3):e20170441. doi: 10.1542/peds.2017-0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fleming-Dutra KE, Hersh AL, Shapiro DJ, Bartoces M, Enns EA, File TM, Jr, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864–1873. doi: 10.1001/jama.2016.4151. [DOI] [PubMed] [Google Scholar]
- 44.Zhao D, Su H, Cheng J, Wang X, Xie M, Li K, et al. Prenatal antibiotic use and risk of childhood wheeze/asthma: a meta-analysis. Pediatr Allergy Immunol. 2015;26(8):756–764. doi: 10.1111/pai.12436. [DOI] [PubMed] [Google Scholar]
- 45.Penders J, Kummeling I, Thijs C. Infant antibiotic use and wheeze and asthma risk: a systematic review and meta-analysis. Eur Respir J. 2011;38(2):295–302. doi: 10.1183/09031936.00105010. [DOI] [PubMed] [Google Scholar]
- 46.Wu P, Feldman AS, Rosas-Salazar C, James K, Escobar G, Gebretsadik T, et al. Relative importance and additive effects of maternal and infant risk factors on childhood asthma. PLoS ONE. 2016;11(3):e0151705. doi: 10.1371/journal.pone.0151705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vangay P, Ward T, Gerber JS, Knights D. Antibiotics, pediatric dysbiosis, and disease. Cell Host Microbe. 2015;17(5):553–564. doi: 10.1016/j.chom.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375(24):2369–2379. doi: 10.1056/NEJMra1600266. [DOI] [PubMed] [Google Scholar]
- 49.Feehley T, Stefka AT, Cao S, Nagler CR. Microbial regulation of allergic responses to food. Semin Immunopathol. 2012;34(5):671–688. doi: 10.1007/s00281-012-0337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci USA. 2010;107(26):11971–11975. doi: 10.1073/pnas.1002601107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dominguez-Bello MG, De Jesus-Laboy KM, Shen N, Cox LM, Amir A, Gonzalez A, et al. Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med. 2016;22(3):250–253. doi: 10.1038/nm.4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tollanes MC, Moster D, Daltveit AK, Irgens LM. Cesarean section and risk of severe childhood asthma: a population-based cohort study. J Pediatr. 2008;153(1):112–116. doi: 10.1016/j.jpeds.2008.01.029. [DOI] [PubMed] [Google Scholar]
- 53.Fricke WF. The more the merrier? Reduced fecal microbiota diversity in preterm infants treated with antibiotics. J Pediatr. 2014;165(1):8–10. doi: 10.1016/j.jpeds.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 54.Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrlander C, et al. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364(8):701–709. doi: 10.1056/NEJMoa1007302. [DOI] [PubMed] [Google Scholar]
- 55.Martinez FD, Guerra S. Early origins of asthma: role of microbial dysbiosis and metabolic dysfunction. Am J Respir Crit Care Med. 2018;197(5):573–579. doi: 10.1164/rccm.201706-1091PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.University of Arizona. Oral bacterial extract for the prevention of wheezing lower respiratory tract illness (ORBEX): ClinicalTrials.gov ID: NCT02148796. https://clinicaltrials.gov/ct2/show/NCT02148796. Accessed 14 Jan 2018
- 57.Lodrup Carlsen KC, Roll S, Carlsen KH, Mowinckel P, Wijga AH, Brunekreef B, et al. Does pet ownership in infancy lead to asthma or allergy at school age? Pooled analysis of individual participant data from 11 European birth cohorts. PLoS ONE. 2012;7(8):e43214. doi: 10.1371/journal.pone.0043214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Remes ST, Castro-Rodriguez JA, Holberg CJ, Martinez FD, Wright AL. Dog exposure in infancy decreases the subsequent risk of frequent wheeze but not of atopy. J Allergy Clin Immunol. 2001;108(4):509–515. doi: 10.1067/mai.2001.117797. [DOI] [PubMed] [Google Scholar]
- 59.O’Connor GT, Lynch SV, Bloomberg GR, Kattan M, Wood RA, Gergen PJ, et al. Early-life home environment and risk of asthma among inner-city children. J Allergy Clin Immunol. 2018;141(4):1468–1475. doi: 10.1016/j.jaci.2017.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barlow SE, Expert C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 61.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gungor NK. Overweight and obesity in children and adolescents. J Clin Res Pediatr Endocrinol. 2014;6(3):129–143. doi: 10.4274/jcrpe.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lessard A, Turcotte H, Cormier Y, Boulet LP. Obesity and asthma: a specific phenotype? Chest. 2008;134(2):317–323. doi: 10.1378/chest.07-2959. [DOI] [PubMed] [Google Scholar]
- 64.Lochte L, Nielsen KG, Petersen PE, Platts-Mills TA. Childhood asthma and physical activity: a systematic review with meta-analysis and graphic appraisal tool for epidemiology assessment. BMC Pediatr. 2016;16:50. doi: 10.1186/s12887-016-0571-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mebrahtu TF, Feltbower RG, Greenwood DC, Parslow RC. Childhood body mass index and wheezing disorders: a systematic review and meta-analysis. Pediatr Allergy Immunol. 2015;26(1):62–72. doi: 10.1111/pai.12321. [DOI] [PubMed] [Google Scholar]
- 66.Daniels SR, Hassink SG, Committee On N. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1):e275–e292. doi: 10.1542/peds.2015-1558. [DOI] [PubMed] [Google Scholar]
- 67.Wang Y, Cai L, Wu Y, Wilson RF, Weston C, Fawole O, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16(7):547–565. doi: 10.1111/obr.12277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity (Silver Spring) 2013;21(12):2422–2428. doi: 10.1002/oby.20515. [DOI] [PubMed] [Google Scholar]
- 69.Tinuoye O, Pell JP, Mackay DF. Meta-analysis of the association between secondhand smoke exposure and physician-diagnosed childhood asthma. Nicotine Tob Res. 2013;15(9):1475–1483. doi: 10.1093/ntr/ntt033. [DOI] [PubMed] [Google Scholar]
- 70.Burke H, Leonardi-Bee J, Hashim A, Pine-Abata H, Chen Y, Cook DG, et al. Prenatal and passive smoke exposure and incidence of asthma and wheeze: systematic review and meta-analysis. Pediatrics. 2012;129(4):735–744. doi: 10.1542/peds.2011-2196. [DOI] [PubMed] [Google Scholar]
- 71.Homa DM, Neff LJ, King BA, Caraballo RS, Bunnell RE, Babb SD, et al. Vital signs: disparities in nonsmokers’ exposure to secondhand smoke–United States, 1999–2012. MMWR Morb Mortal Wkly Rep. 2015;64(4):103–108. [PMC free article] [PubMed] [Google Scholar]
- 72.Curtin SC, Abma JC, Ventura SJ, Henshaw SK. Pregnancy rates for US women continue to drop. NCHS Data Brief. 2013;136:1–8. [PubMed] [Google Scholar]
- 73.Farber HJ, Walley SC, Groner JA, Nelson KE, Section on Tobacco C Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5):1008–1017. doi: 10.1542/peds.2015-3110. [DOI] [PubMed] [Google Scholar]
- 74.Koplan JP, Satcher D. Reducing tobacco use. A report of the Surgeon General. Executive summary. MMWR Recomm Rep. 2000;49(RR-16):1–27. [PubMed] [Google Scholar]
- 75.Gilman SE, Rende R, Boergers J, Abrams DB, Buka SL, Clark MA, et al. Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics. 2009;123(2):e274–e281. doi: 10.1542/peds.2008-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Platts-Mills TA. The allergy epidemics: 1870–2010. J Allergy Clin Immunol. 2015;136(1):3–13. doi: 10.1016/j.jaci.2015.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alduraywish SA, Lodge CJ, Campbell B, Allen KJ, Erbas B, Lowe AJ, et al. The march from early life food sensitization to allergic disease: a systematic review and meta-analyses of birth cohort studies. Allergy. 2016;71(1):77–89. doi: 10.1111/all.12784. [DOI] [PubMed] [Google Scholar]
- 78.Tran MM, Lefebvre DL, Dai D, Dharma C, Subbarao P, Lou W, et al. Timing of food introduction and development of food sensitization in a prospective birth cohort. Pediatr Allergy Immunol. 2017;28(5):471–477. doi: 10.1111/pai.12739. [DOI] [PubMed] [Google Scholar]
- 79.Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372(9):803–813. doi: 10.1056/NEJMoa1414850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Togias A, Cooper SF, Acebal ML, Assa’ad A, Baker JR, Jr, Beck LA, et al. Addendum guidelines for the prevention of peanut allergy in the United States: report of the national institute of allergy and infectious diseases-sponsored expert panel. J Allergy Clin Immunol. 2017;139(1):29–44. doi: 10.1016/j.jaci.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jhamnani RD, Frischmeyer-Guerrerio P. Desensitization for peanut allergies in children. Curr Treat Options Allergy. 2016;3(3):282–291. doi: 10.1007/s40521-016-0091-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Stoltz DJ, Jackson DJ, Evans MD, Gangnon RE, Tisler CJ, Gern JE, et al. Specific patterns of allergic sensitization in early childhood and asthma & rhinitis risk. Clin Exp Allergy. 2013;43(2):233–241. doi: 10.1111/cea.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sporik R, Holgate ST, Platts-Mills TA, Cogswell JJ. Exposure to house-dust mite allergen (Der p I) and the development of asthma in childhood. A prospective study. N Engl J Med. 1990;323(8):502–507. doi: 10.1056/NEJM199008233230802. [DOI] [PubMed] [Google Scholar]
- 84.Celedon JC, Milton DK, Ramsey CD, Litonjua AA, Ryan L, Platts-Mills TA, et al. Exposure to dust mite allergen and endotoxin in early life and asthma and atopy in childhood. J Allergy Clin Immunol. 2007;120(1):144–149. doi: 10.1016/j.jaci.2007.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Arshad SH, Bateman B, Sadeghnejad A, Gant C, Matthews SM. Prevention of allergic disease during childhood by allergen avoidance: the Isle of Wight prevention study. J Allergy Clin Immunol. 2007;119(2):307–313. doi: 10.1016/j.jaci.2006.12.621. [DOI] [PubMed] [Google Scholar]
- 86.Boston Children’s Hospital. Preventing asthma in high risk kids (PARK): ClinicalTrials.gov ID: NCT02570984. https://clinicaltrials.gov/ct2/show/NCT02570984. Accessed 14 Jan 2018
- 87.Centers for Disease Control and Prevention. Breastfeeding report card. 2016. https://www.cdc.gov/breastfeeding/pdf/2016breastfeedingreportcard.pdf. Accessed 28 Dec 2017
- 88.Lodge CJ, Tan DJ, Lau MX, Dai X, Tham R, Lowe AJ, et al. Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):38–53. doi: 10.1111/apa.13132. [DOI] [PubMed] [Google Scholar]
- 89.Gartner LM, Morton J, Lawrence RA, Naylor AJ, O’Hare D, Schanler RJ, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 90.Looker AC, Johnson CL, Lacher DA, Pfeiffer CM, Schleicher RL, Sempos CT. Vitamin D status: United States, 2001–2006. NCHS Data Brief. 2011;59:1–8. [PubMed] [Google Scholar]
- 91.Wolsk HM, Chawes BL, Litonjua AA, Hollis BW, Waage J, Stokholm J, et al. Prenatal vitamin D supplementation reduces risk of asthma/recurrent wheeze in early childhood: a combined analysis of two randomized controlled trials. PLoS ONE. 2017;12(10):e0186657. doi: 10.1371/journal.pone.0186657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wu H, Zhang C, Wang Y, Li Y. Does vitamin E prevent asthma or wheeze in children: a systematic review and meta-analysis. Paediatr Respir Rev. 2017 doi: 10.1016/j.prrv.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 93.Bailey RL, Fulgoni VL, 3rd, Keast DR, Dwyer JT. Examination of vitamin intakes among US adults by dietary supplement use. J Acad Nutr Diet. 2012;112(5):657.e4–663.e4. doi: 10.1016/j.jand.2012.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Feldman AS, He Y, Moore ML, Hershenson MB, Hartert TV. Toward primary prevention of asthma. Reviewing the evidence for early-life respiratory viral infections as modifiable risk factors to prevent childhood asthma. Am J Respir Crit Care Med. 2015;191(1):34–44. doi: 10.1164/rccm.201405-0901PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rosas-Salazar C, Hartert TV. Prenatal exposures and the development of childhood wheezing illnesses. Curr Opin Allergy Clin Immunol. 2017;17(2):110–115. doi: 10.1097/ACI.0000000000000342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lin W, Brunekreef B, Gehring U. Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheeze in children. Int J Epidemiol. 2013;42(6):1724–1737. doi: 10.1093/ije/dyt150. [DOI] [PubMed] [Google Scholar]
- 97.Elazab N, Mendy A, Gasana J, Vieira ER, Quizon A, Forno E. Probiotic administration in early life, atopy, and asthma: a meta-analysis of clinical trials. Pediatrics. 2013;132(3):e666–e676. doi: 10.1542/peds.2013-0246. [DOI] [PubMed] [Google Scholar]
- 98.Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;7:CD010085. doi: 10.1002/14651858.CD010085.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen C, Xun P, Tsinovoi C, He K. Accumulated evidence on Helicobacter pylori infection and the risk of asthma: a meta-analysis. Ann Allergy Asthma Immunol. 2017;119(2):137.e2–145.e2. doi: 10.1016/j.anai.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 100.Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy. 2015;70(3):245–256. doi: 10.1111/all.12561. [DOI] [PubMed] [Google Scholar]
- 101.Tischer CG, Hohmann C, Thiering E, Herbarth O, Muller A, Henderson J, et al. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy. 2011;66(12):1570–1579. doi: 10.1111/j.1398-9995.2011.02712.x. [DOI] [PubMed] [Google Scholar]
- 102.Hosseini B, Berthon BS, Wark P, Wood LG. Effects of fruit and vegetable consumption on risk of asthma, wheezing and immune responses: a systematic review and meta-analysis. Nutrients. 2017;9(4):341. doi: 10.3390/nu9040341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Etminan M, Sadatsafavi M, Jafari S, Doyle-Waters M, Aminzadeh K, FitzGerald JM. Acetaminophen use and the risk of asthma in children and adults: a systematic review and metaanalysis. Chest. 2009;136(5):1316–1323. doi: 10.1378/chest.09-0865. [DOI] [PubMed] [Google Scholar]
- 104.Zhu T, Zhang L, Qu Y, Mu D. Meta-analysis of antenatal infection and risk of asthma and eczema. Medicine (Baltimore) 2016;95(35):e4671. doi: 10.1097/MD.0000000000004671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.van de Loo KF, van Gelder MM, Roukema J, Roeleveld N, Merkus PJ, Verhaak CM. Prenatal maternal psychological stress and childhood asthma and wheezing: a meta-analysis. Eur Respir J. 2016;47(1):133–146. doi: 10.1183/13993003.00299-2015. [DOI] [PubMed] [Google Scholar]
- 106.Jaakkola JJ, Ahmed P, Ieromnimon A, Goepfert P, Laiou E, Quansah R, et al. Preterm delivery and asthma: a systematic review and meta-analysis. J Allergy Clin Immunol. 2006;118(4):823–830. doi: 10.1016/j.jaci.2006.06.043. [DOI] [PubMed] [Google Scholar]
- 107.Crider KS, Cordero AM, Qi YP, Mulinare J, Dowling NF, Berry RJ. Prenatal folic acid and risk of asthma in children: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(5):1272–1281. doi: 10.3945/ajcn.113.065623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Feng H, Xun P, Pike K, Wills AK, Chawes BL, Bisgaard H, et al. In utero exposure to 25-hydroxyvitamin D and risk of childhood asthma, wheeze, and respiratory tract infections: a meta-analysis of birth cohort studies. J Allergy Clin Immunol. 2017;139(5):1508–1517. doi: 10.1016/j.jaci.2016.06.065. [DOI] [PubMed] [Google Scholar]
- 109.Centers for Disease C, Prevention Use of unvented residential heating appliances–United States, 1988–1994. MMWR Morb Mortal Wkly Rep. 1997;46(51):1221–1224. [PubMed] [Google Scholar]
- 110.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 111.Association American Veterinary Medical. US pet ownership and demographics sourcebook. Schaumburg: American Veterinary Medical Association; 2012. [Google Scholar]
- 112.Black LI, Clarke TC, Barnes PM, Stussman BJ, Nahin RL. Use of complementary health approaches among children aged 4–17 years in the United States: national health interview survey, 2007–2012. Natl Health Stat Rep. 2015;78:1–19. [PMC free article] [PubMed] [Google Scholar]
- 113.Staat MA, Kruszon-Moran D, McQuillan GM, Kaslow RA. A population-based serologic survey of Helicobacter pylori infection in children and adolescents in the United States. J Infect Dis. 1996;174(5):1120–1123. doi: 10.1093/infdis/174.5.1120. [DOI] [PubMed] [Google Scholar]
- 114.Centers for Disease Control and Prevention. Summary health statistics: national health interview survey. 2015. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_C-2.pdf. Accessed 22 Dec 2017
- 115.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 116.Boehmer TK, Foster SL, Henry JR, Woghiren-Akinnifesi EL, Yip FY, Centers for Disease C et al. Residential proximity to major highways—United States, 2010. MMWR Suppl. 2013;62(3):46–50. [PubMed] [Google Scholar]
- 117.Jackson KD, Howie LD, Akinbami LJ. Trends in allergic conditions among children: United States, 1997–2011. NCHS Data Brief. 2013;121:1–8. [PubMed] [Google Scholar]
- 118.Lorson BA, Melgar-Quinonez HR, Taylor CA. Correlates of fruit and vegetable intakes in US children. J Am Diet Assoc. 2009;109(3):474–478. doi: 10.1016/j.jada.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 119.Lundgren M, Steed LJ, Tamura R, Jonsdottir B, Gesualdo P, Crouch C, et al. Analgesic antipyretic use among young children in the TEDDY study: no association with islet autoimmunity. BMC Pediatr. 2017;17(1):127. doi: 10.1186/s12887-017-0884-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yali AM, Lobel M. Coping and distress in pregnancy: an investigation of medically high risk women. J Psychosom Obstet Gynaecol. 1999;20(1):39–52. doi: 10.3109/01674829909075575. [DOI] [PubMed] [Google Scholar]
- 121.Werler MM, Mitchell AA, Hernandez-Diaz S, Honein MA. Use of over-the-counter medications during pregnancy. Am J Obstet Gynecol. 2005;193(3 Pt 1):771–777. doi: 10.1016/j.ajog.2005.02.100. [DOI] [PubMed] [Google Scholar]
- 122.Daniels K, Daugherty J, Jones J. Current contraceptive status among women aged 15–44: United States, 2011–2013. NCHS Data Brief. 2014;173:1–8. [PubMed] [Google Scholar]
- 123.Kim HJ, Giovannucci E, Rosner B, Willett WC, Cho E. Longitudinal and secular trends in dietary supplement use: nurses’ health study and health professionals follow-up study, 1986–2006. J Acad Nutr Diet. 2014;114(3):436–443. doi: 10.1016/j.jand.2013.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mansbach JM, Ginde AA, Camargo CA., Jr Serum 25-hydroxyvitamin D levels among US children aged 1 to 11 years: do children need more vitamin D? Pediatrics. 2009;124(5):1404–1410. doi: 10.1542/peds.2008-2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Meta-analyses and exposure prevalence data of risk factors for childhood asthma development.
Data Availability Statement
All data used in this review is from published meta-analyses.