Abstract.
Optical coherence tomography (OCT) manufacturers graphically present circumpapillary retinal nerve fiber layer thickness (cpRNFLT) together with normative limits to support clinicians in diagnosing ophthalmic diseases. The impact of age on cpRNFLT is typically implemented by linear models. cpRNFLT is strongly location-specific, whereas previously published norms are typically restricted to coarse sectors and based on small populations. Furthermore, OCT devices neglect impacts of lens or eye size on the diameter of the cpRNFLT scan circle so that the diameter substantially varies over different eyes. We investigate the impact of age and scan diameter reported by Spectralis spectral-domain OCT on cpRNFLT in 5646 subjects with healthy eyes. We provide cpRNFLT by age and diameter at 768 angular locations. Age/diameter were significantly related to cpRNFLT on 89%/92% of the circle, respectively (pointwise linear regression), and to shifts in cpRNFLT peak locations. For subjects from age 42.1 onward but not below, increasing age significantly decreased scan diameter (, ), which suggests that pathological cpRNFLT thinning over time may be underestimated in elderly compared to younger subjects, as scan diameter decrease correlated with cpRNFLT increase. Our detailed numerical results may help to generate various correction models to improve diagnosing and monitoring optic neuropathies.
Keywords: normative retinal nerve fiber layer profile, age-related thinning, ocular magnification, scan diameter, optical coherence tomography, glaucoma
1. Introduction
The normative profile of circumpapillary retinal nerve fiber layer thickness (cpRNFLT) is important to identify abnormal thinning of cpRNFLT, which is one of the hallmarks for glaucoma diagnosis and progression monitoring.1,2 It is well known that the normative cpRNFLT decreases with increased age.3,4 Moreover, studies have shown that the thinning of normative cpRNFLT with age is highly location-specific.5,6 However, the location specificity of the age-related thinning varies among different studies. For example, Parikh et al.5 have shown the age-related thinning rate of cpRNFLT in superior and inferior quadrants to be the maximum and minimum among the four quadrants, respectively. By contrast, Leung et al.6 have shown the age-related thinning rate of cpRNFLT to be the maximum in inferior and minimum in nasal quadrants, respectively. The varying results of the quadrant specificity of age-related cpRNFLT thinning might be due to the relative small study populations in those studies, as all their results are based on less than 250 eyes. A second limitation of previously published cpRNFLT norms is their restriction on coarsely defined sectors, which neglects the large location specificity of cpRNFLT over the entire scan circle. One of the few studies that presented 12 instead of four to six sectors7 demonstrates this location-specific variability.
Besides the correlation between the normative cpRNFLT and age, studies have also shown the cpRNFLT to be related to factors that represent the eye anatomy, including ocular axial length and the spherical equivalent (SE) of the refractive error.8,9 More specifically, it has been shown that thinner cpRNFLT is associated with larger axial length and more myopia.10–12 Ocular magnification formulas have been proposed to estimate the actual scan diameter from axial length and SE.13,14 However, to our best knowledge, none of the clinical ophthalmic optical coherence tomography (OCT) devices takes the true scan diameter into account. Typically, manufacturers report to apply a fixed size of measurement/scan circle, for instance, for Cirrus HD-OCT (Carl Zeiss Meditec, Jena, Germany), the cpRNFLT on the standard measurement circle with 3.46-mm diameter is extracted from the volume scans without considering the variation of individual eye size.15
To our best knowledge, none of the clinical retinal OCT devices measures the true circle diameter on the retina. Heidelberg Spectralis internally estimates the circle size in mm based on the focus settings adjusted by the device operator prior to the scan.14 This estimated diameter is not part of the printout and therefore not easily accessible to clinicians, but it can be electronically exported from the machine.
In this study, we will leverage a large population-based study to investigate the relationships between age, the scan diameter reported by the employed Spectralis OCT, and the full pointwise cpRNFLT profile in participants with healthy eyes.
2. Methods
This investigation is part of the Leipzig Research Centre for Civilization Diseases (LIFE) adult study.16 The LIFE adult study was approved by the institutional ethics board of the Medical Faculty of Leipzig University and adheres to the Declaration of Helsinki. The written informed consent was obtained from all participants.
2.1. Participants and Data Description
The population-based LIFE adult study16 involved an age and gender stratified random sample of the residents of the city of Leipzig, Germany. In total, 10,000 participants were recruited, with 514 participants in the age group between 18 and 39 years and 9486 participants between 40 and 79 years.
For 17,974 eyes of 9069 participants, Heidelberg Spectralis cpRNFLT OCT scans with a resolution of 768 measurement points around the optic nerve head (ONH) were available. In all of those eyes, nonmydriatic fundus imaging (Nidek AFC-230) and further OCT scans of the macular and papillary areas were additionally obtained.16 On all images, degenerative changes and abnormalities were classified according to current ophthalmic standards.
Three sources of information were available for this step prior to analysis: (a) self-reported questionnaire including full list of diagnosed eye diseases, (b) all medications of the subject taken at time of test (all details/packages were brought in by the subject, the full list was coded and entered into the LIFE database using international classifications), and (c) ophthalmic examination of fundus and OCT images and resulting clinically significant diseases found. For the ophthalmic examination, two ophthalmologically trained readers graded all eyes separately based on macular and papillary OCT images and 45 deg color fundus photography and formed a consensus decision. The following categories were employed: “clinical” (i.e., eye disease present), “subclinical” and “free of subclinical or clinical signs” as well as “nongradable” (i.e., poor image quality). The exclusion criteria include manifestation of retina-related diseases defined by the following: (a) self-reported data on glaucoma diagnosis or status of prescribed glaucoma medication and (b) clinical findings at the papillary area, clinical findings at the macula, and clinical findings within the periphery (retinal area outside papillary and macular areas). This resulted in exclusion of any retinal or optic nerve disease objectively present. Cataract and anterior eye segment problems (granting the image was obtained in the first place) were not excluded. It is important for the current analysis to be strict on exclusion of retinal or optic nerve lesion as they potentially affect the cpRNFLT, and we aim to establish our model free from disease-based bias.
For the current analyses, subjects with manifestation of retina-related diseases or nongradable images in any of the two eyes were excluded. Furthermore, to ensure the reliability of the cpRNFLT measurements, only circle scans with image quality , average number of B-scans , and no more than 5% missing or unreliable cpRNFLT segmentations among the 768 A-scans were included. Unreliable cpRNFLT segmentations were defined as measurements above 99.5% or below 0.5% quantiles among the cpRNFLT distribution for all measurement locations of all OCT scans. If both eyes of a participant met the aforementioned selection criteria, only one eye was randomly selected.
2.2. Description of Scan Diameter
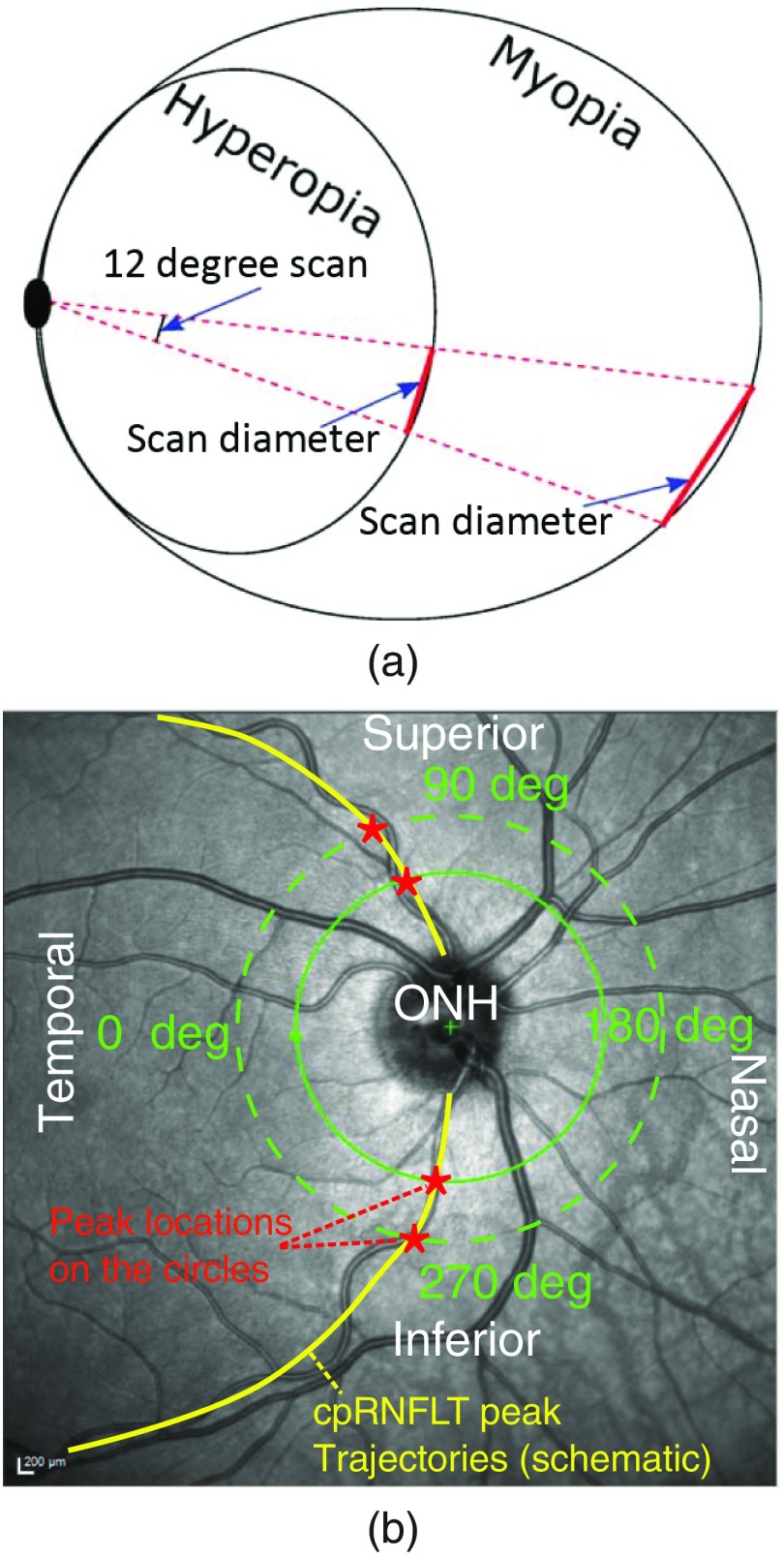
The Heidelberg Spectralis OCT (Heidelberg Engineering, Heidelberg, Germany) device used in this study specifies a fixed circle diameter of 12 deg in the device settings, projected onto the retinal plane, as shown in Fig. 1(a), which corresponds to approximately a 3.5-mm diameter scan circle size on the retinal plane based on the standard eye model employed in the machine.14,17 While the Spectralis machine always projects a fixed measurement circle into the eye, the size of the scan diameter on the retina varies with individual ocular parameters, particularly axial length and corneal curvature. For example, the actual scan diameter can be larger for eyes with larger axial length and smaller for eyes with shorter axial length, as illustrated in Fig. 1(a). Within the Spectralis OCT, conversion of this 12 deg circle scan into mm is achieved by calculations based on defocus correction and corneal curvature, as detailed in the work by Garway-Heath et al.14
Fig. 1.
(a) Schematic illustration of scan diameter variation with respect to axial length of the eye and (b) schematic illustration of the cpRNFLT measurement circle around the ONH including the effect of varying circle diameters.
Figure 1(b) illustrates the cpRNFLT circle, the coordinate system used in this study, and the effect of varying circle diameters. Superimposed on the ONH-centered infrared fundus image of the right eye of a 42-year old participant, a typical cpRNFLT measurement circle (solid circle) is depicted and an illustrative larger circle (dashed circle) is overlaid. In addition, the schematic trajectories of the cpRNFLT peaks are illustrated (curves in superior/inferior temporal direction). These trajectories are correlated to the major temporal-superior/temporal-inferior arteries. As illustrated, the nonlinear curvy trajectories of the main nerve fiber bundles cause relative shifts of the angular positions of the cpRNFLT peak locations (illustrated by asterisks) if the measurement circle diameter changes. In addition, cpRNFLT is naturally thinner with increasing diameter for myopes due to ocular elongation.10,11
In this study, we employed the scan diameter as a measure of ocular magnification. The scan diameter in mm measured by Spectralis OCT is based on the scan focus parameters as a surrogate measure of refractive error and standard corneal curvature, as detailed in the work by Garway-Heath et al.14 Within the current investigation, we deliberately employed only parameters routinely available from the Spectralis OCT device to ensure that our results can immediately be applied to all Spectralis OCT data without requiring additional tools or machines.
2.3. Statistical Analyses
All statistical analyses were performed by R platform.18 First, the inter-relationships between age, scan diameter, and global cpRNFLT were evaluated. Segmented regression was performed to examine whether there are different relationships between age and scan diameter for different age groups. Second, multiple linear regressions were performed from age and scan diameter to global, quadrantal, and clock-hour cpRNFLTs, respectively, in comparison to the univariate regressions from age to global, quadrantal, and clock-hour cpRNFLTs. Third, we compared the spatial profiles of cpRNFLT between groups with younger and older ages with enforced no significant group difference of scan diameter, as well as between groups with smaller and larger scan diameters with enforced no significant group difference of age, in order to decouple the potential underlying interactive effects between age and scan diameter. Last, multivariate linear regressions were performed from age and scan diameter to pointwise cpRNFLT over all 768 measurement locations on the scan circle. The values were adjusted for multiple comparisons.19
The context for our extensive linear regression analyses is that all ophthalmic OCT manufacturers and also many research scientists currently implement linear models to capture the influence of age. In a linear model, two parameters are required: First, a point estimate of cpRNFLT for a fixed age (or diameter) and second, an estimate for how cpRNFLT changes per year, which we call “slope” in this work. The current analysis provides point estimates for specific age groups and slopes separately in depicted figures. This allows device manufacturers to store only these two values for each of the 768 measurement locations to quantify the location-specific deviations of a patient’s individual cpRNFLT from the norm. These individual deviations may be used by clinicians to support diagnostic statements. Furthermore, since optic neuropathies like glaucoma are progressive diseases, it is diagnostically important to compare the patients’ individual age slope with the normative age slope for the respective measurement location (or sector), as provided in our study. For this purpose, diameter slopes are relevant as well.
3. Results
From 17,974 eyes of 9069 participants, 3329 participants were excluded in total due to any of the following exclusion criteria (or a combination of them): any clinically significant findings based on prior ophthalmic examination of fundus images and obtained OCT scans (2676 subjects), nongradable images due to poor image quality (2 subjects), a glaucoma diagnosis reported in the interview (613 subjects), the presence of glaucoma medication among all the medications the participant took at the time of the test (38 subjects). The 188 eyes from 94 participants were excluded due to unreliable measurements. After all data selection procedures, 5646 eyes from 5646 participants were selected for data analyses. The of age was . There were 2553 male and 3093 female participants.
The detailed ethnic proportion of the participants in LIFE study can be found in Table 1. The subjects of the current investigation are predominantly Caucasian (99.22%). The recruitment of participants in the LIFE study was performed by randomly selecting Leipzig residents from the city registration office. Citizens were sent invitation letters, and study participation depended on response. In the years of the data acquisition, the east German city of Leipzig had a low percentage of foreign residents (between 5% and 10%), most of them from European countries. Among the very small proportion of residents of non-European race, the response rate was extraordinarily low, particularly due to language issues. Therefore, the percentage of non-Caucasian participants in the current data sample is negligible (0.78%), and a race-specific data analysis was not feasible.
Table 1.
The ethnic proportion of the participants in LIFE study.
| European Descent | Arabic/Middle Eastern Descent | Central Asian Descent | East Asian Descent | Latin American Descent | African Descent | Mixed Ethnicity |
|---|---|---|---|---|---|---|
| 99.22% | 0.22% | 0.20% | 0.12% | 0.09% | 0.06% | 0.09% |
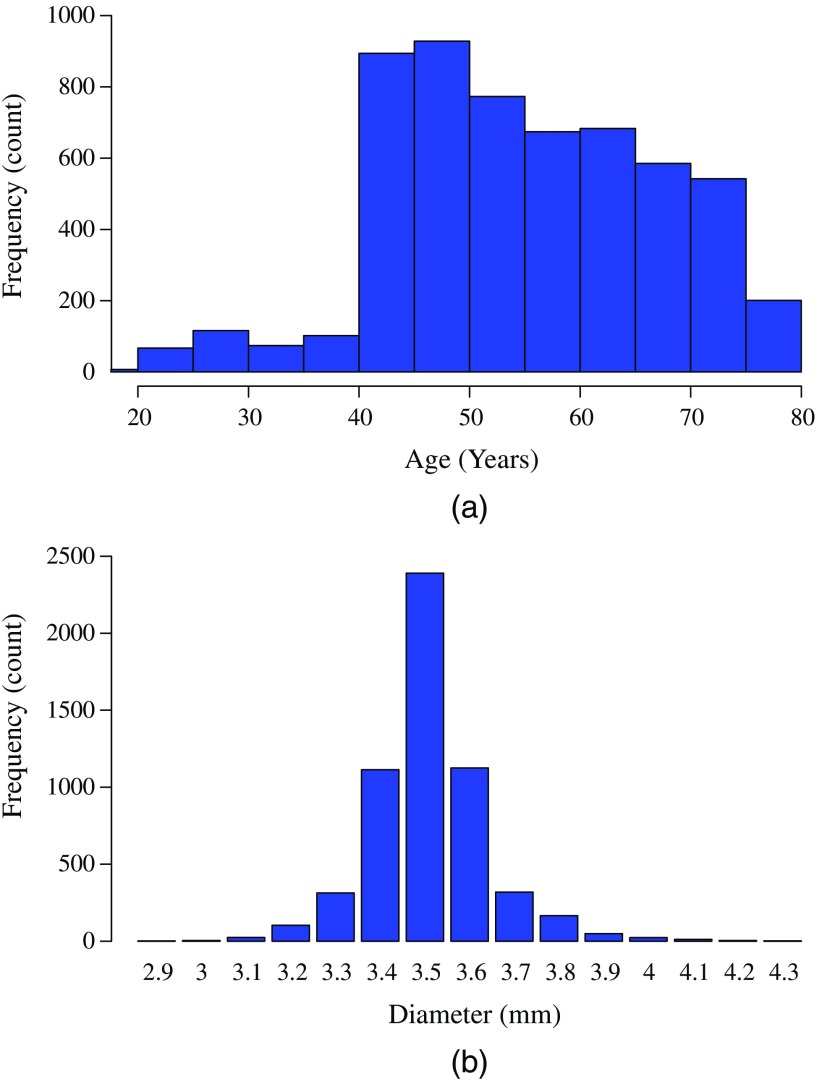
Figures 2(a) and 2(b) show the distributions of age and scan diameter over all subjects, respectively. Since the LIFE adult study focuses on the age group of 40 to 75 years, as detailed above, there were fewer subjects with age under 40 years. The trend that the number of subjects decreased with increasing age was due to excluding participants with clinical signs on OCT or fundus images or nongradable images, as described above, or due to excluding patients with diagnosed glaucoma or possible optic neuropathy, as shown in Fig. 2(a), since there was a higher proportion of those cases for older subjects. As shown in Fig. 2(b), the scan diameter was normally distributed with peak at the 3.5-mm diameter, which was the scan circle size for the standard eye model used on the machine with corneal radius set to be 7.8 mm and scan focus to be an individual measure of refractive error.
Fig. 2.
The distribution of (a) age and (b) scan diameter over all subjects. The LIFE adult study focuses on the age range of 40 to 75 years. While the Spectralis machine projects a measurement circle with a fixed radius of 12 deg into the eye, the size of the scan diameter on the retina varies with individual ocular parameters, particularly axial length and corneal curvature.
The scan diameter was mildly and inversely correlated to age (, ). The results of segmented regression from age to scan diameter suggested that the scan diameter was differently related to age for age group younger/older than 42.1 years old, which was detected as a break point for age by the segmented regression. For subjects under 42.1 years, there was no significant correlation between age and scan diameter (, ), whereas the correlation was () for subjects over 42.1 years. In addition, the global RNFLT was inversely correlated to scan diameter (, ) as expected. In comparison, the global RNFLT was inversely correlated to age (, ).
Table 2 shows the age slopes and values obtained from (1) “univariate regression” from age to global and quadrant-specific cpRNFLTs compared to the slopes and values of age and scan diameter obtained by (2) “multivariate regression” from age and diameter to global and quadrant-specific cpRNFLTs. Global cpRNFLT increased with decreasing scan diameter. Without considering the effect of scan diameter, the age slope was substantially underestimated () compared the age slope with adjusted effect of scan diameter (). Sectoral cpRNFLT decreased with increasing scan diameter except for the temporal cpRNFLT. Accordingly, the age slopes were mostly underestimated when not including the effect of scan diameter except for temporal cpRNFLT, for which the age slope was overestimated without including the effect of scan diameter. In addition, for the nasal sector, the age slope shifted from insignificant thickening to significant thinning after adjusting for the scan diameter effect.
Table 2.
The age slopes and values with (1) “univariate regression” from age to global and quadrant-specific cpRNFLTs in comparison to the slopes and values of age and scan diameter with (2) “multivariate regression” from age and diameter to global and quadrant-specific cpRNFLTs. The table is to demonstrate how the ocular magnification can bias the estimation of age-related thinning rate of global and quadrant cpRNFLT as most previous works have not included ocular magnification in their cpRNFLT norm model.
| RNFLT | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Age slope () | value for age | Age slope () | value for age | Diameter slope () | value for diameter | |
| Global | ||||||
| Temporal | 6.65 | |||||
| Superior | ||||||
| Nasal | 0.03 | 0.09 | ||||
| Inferior | ||||||
Table 3 shows the age slopes and values obtained by univariate regression from age to clock-hour-specific RNFLTs compared to the slopes and values of age and scan diameter obtained by multivariate regression. Mean cpRNFLT for clock-hour 8, 9, 10, and 11 increased with decreased scan diameter while the mean cpRNFLT for all other clock-hour sectors decreased. The sector with the strongest scan diameter effect was clock-hour 6. In addition, there were three clock-hour sectors (clock-hour 3, 4, and 6) with positive age slopes when not adjusting for the scan diameter effect, which were counter-intuitive if we assume that there is no age-related thickening. After adjusting the effect of scan diameter, all age slopes were negative, as expected. The fastest age-related thinning was in clock-hour 8 and 7 before and after adjusting the scan diameter effect.
Table 3.
The age slopes and values with univariate regression from age to clock-hour-specific RNFLTs in comparison to the slopes and values of age and scan diameter with multivariate regression from age and diameter to clock-hour-specific RNFLTs.
| RNFLT | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Age slope () | value for age | Age slope () | value for age | Diameter slope () | value for diameter | |
| 1 O’clock | 0.05 | |||||
| 2 O’clock | ||||||
| 3 O’clock | 0.07 | 0.03 | ||||
| 4 O’clock | 0.05 | 0.001 | 0.09 | |||
| 5 O’clock | 0.03 | |||||
| 6 O’clock | 0.02 | 0.54 | ||||
| 7 O’clock | ||||||
| 8 O’clock | 13.22 | |||||
| 9 O’clock | 5.19 | |||||
| 10 O’clock | 3.34 | 0.005 | ||||
| 11 O’clock | 8.06 | |||||
| 12 O’clock | ||||||
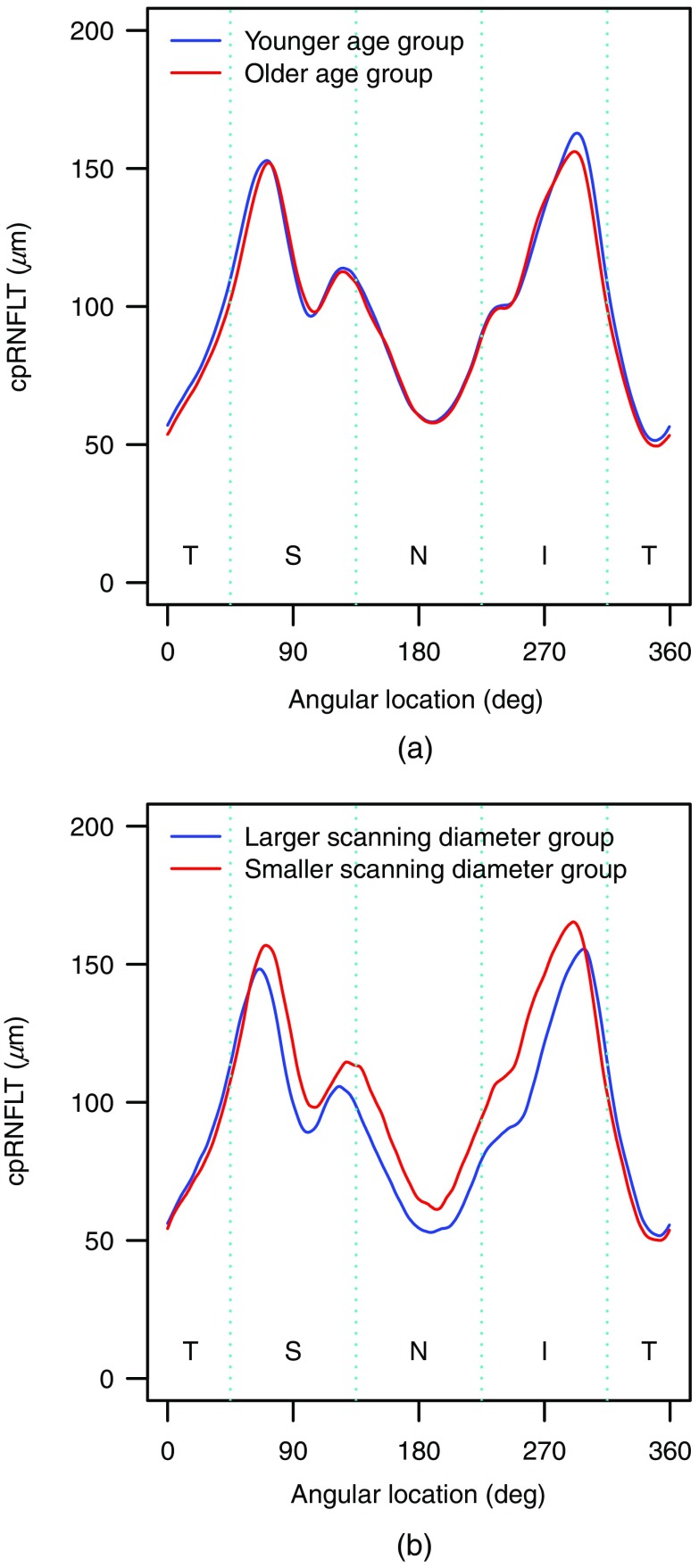
Figure 3 shows the spatial profile of the mean cpRNFLT for (a) younger (35 to 45 years) and older (55 to 65 years) age groups and (b) larger () and smaller () scan diameter groups for subjects, respectively. To decouple the interactive effects between age and scan diameter on mean cpRNFLT: for age group comparison, we restricted the scan diameter to 3.5 mm, which was the most frequent diameter among the participants; for scan diameter group comparison, we restricted the subject age to be under 42.1 years, as we did not find a significant correlation between diameter and age for this age group (see above). Overall, the cpRNFLT peaks of the older group (555 subjects between 55-65 years) are more nasal than those of the younger group (454 subjects between 35 to 45 years). The superior and inferior peaks of the older group were located at 2.80 deg () and 2.83 deg () nasal to the younger group. The cpRNFLT peaks of the smaller scan diameter group were more nasal than the larger scan diameter group. The superior and inferior peaks of the smaller scan diameter group (97 subjects) were located at 9.77 deg () and 7.83 deg () nasal to the larger scan diameter group (194 subjects). There was no significant group age difference () between the smaller (37.1 years) and larger (36.2 years) scan diameter groups.
Fig. 3.
The spatial profile of the mean cpRNFLT for (a) younger (454 subjects between 35 and 45 years) and older (555 subjects between 55 and 65 years) age groups for subjects with 3.5 mm scan diameter and (b) larger () and smaller () scan diameter groups for subjects under 42.1 years, respectively.
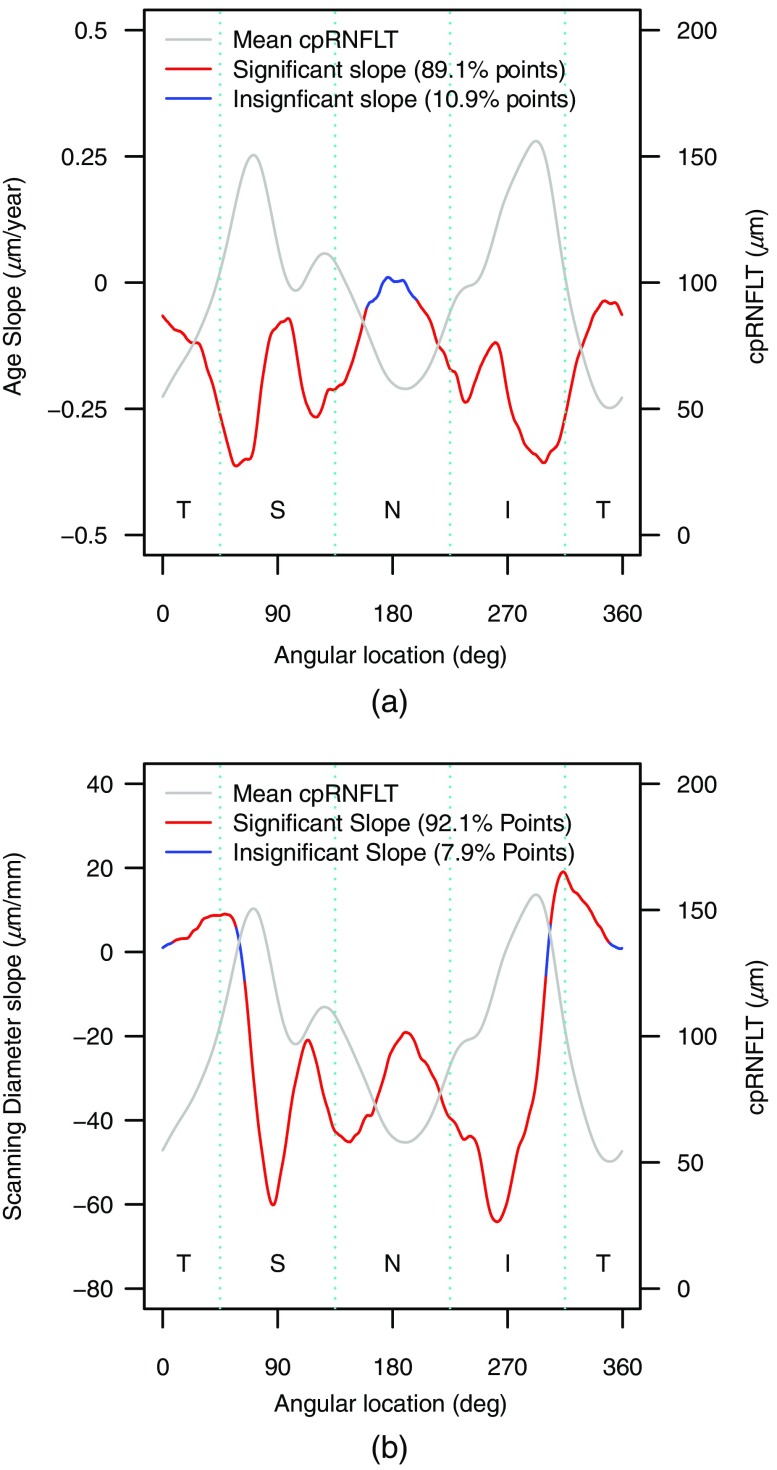
Figures 4(a) and 4(b) show the spatial profile of age and scan diameter slopes to predict cpRNFLT in comparison to the spatial profile of mean RNFLT for all age subjects, respectively. The superior and inferior locations with largest age-related thinning rates were positioned at 9.76 deg and 3.78 deg ( for both, bootstrapping) temporal to the mean superior and inferior RNLFT peaks. Conversely, the superior and inferior locations with cpRNFLT, which presented with the steepest change for a decrease in scan diameter were positioned at 15.32 deg and 30.65 deg ( for both, bootstrapping) nasal to the mean superior and inferior RNLFT peaks.
Fig. 4.
The spatial profile of (a) age slope and (b) scan diameter slope to predict cpRNFLT in comparison to the spatial profile of mean cpRNFLT for all subjects. This figure is the visualization of our pointwise cpRNFLT model based on age and scan diameter, which is described in detail in Table 4 in the Appendix.
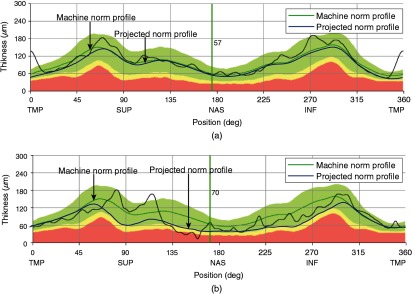
This detailed cpRNFLT results based on over 5600 participants allow a comparison with the cpRNFLT norms of the Spectralis OCT device (based on only 201 eyes of 201 participants), which are employed for the standard clinical printout. Here, we illustratively perform this comparison for two cases. Figures 5(a) and 5(b) show the spatial profile of projected mean cpRNFLT norms based on our age and scan diameter model for a 47-year old subject with 3.5-mm scan diameter and a 75 years subject with 4.4-mm scan diameter in comparison to the Spectralis OCT machine norms, respectively. Those two exemplary cases were chosen to represent the variation of age and scan diameter. For the superior temporal region of the 47-year old participant with 3.5-mm scan diameter, our projected mean cpRNFLT was thinner than the machine norms, and the superior peak of our projected norms was more nasal than the machine norms, which might be explained by our findings in Fig. 4(a) that the fastest age-related thinning locations were temporal to the mean cpRNFLT peaks. The difference between our projected norms and machine norms might also be caused by the possibly higher resolution in our study, as we calculated pointwise models for all 768 measurement points. The considerably lower population size for the Spectralis norms might not have allowed such a pointwise approach. For the 75-year old subject with 4.4-mm scan diameter, our projected norms were substantially thinner than the machine norms and the mean cpRNFLT peak locations of our projected norms were more nasal compared to the machine norms, which might be mostly explained by the current findings in that larger scan diameter corresponding to thinner cpRNFLT and more temporal cpRNFLT peaks, as shown in Figs. 3(b) and 4(b).
Fig. 5.
The spatial profile of age-specific cpRNFLT norms for (a) a 47-year-old subject with 3.5-mm scan diameter and (b) a 75-year-old subject with 4.4-mm scan diameter. For this graphical comparison, our projected norms (thick blue lines) were overlaid on the printouts of the two example participants. The thin black lines denote the actual measurement values of the subjects and are ignored here. Instead, our comparison focuses on the dark green lines, which denote the medians of the machine norms for these two ages.
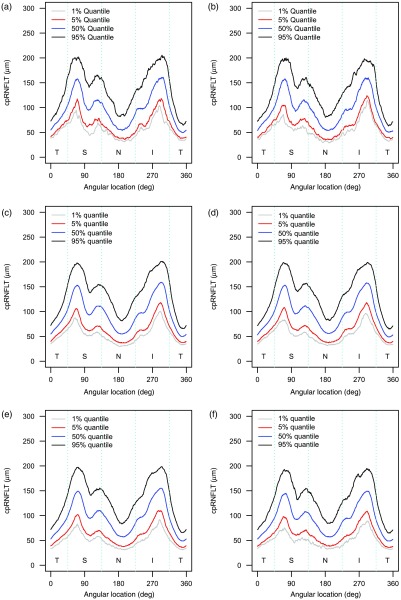
To enhance comparisons with previously published age-specific cpRNFLT norms or the norms used by the different OCT machines, all of which ignored effects of scan diameter, we additionally provide the cpRNFLT quantiles of the study participants for different age decades, as shown in Fig. 6. Finally, this study provides the numerical coefficients for the multivariate regression models of all 768 measurement points in the Appendix, which may help scientists or manufacturers to apply both age and diameter corrections to cpRNFLT measurements.
Fig. 6.
The spatial profile of cpRNFLT at different quantiles for different age groups: (a) 19 to 30 years old, (b) 30 to 40 years old, (c) 40 to 50 years old, (d) 50 to 60 years old, (e) 60 to 70 years old, and (f) 70 to 80 years old.
4. Discussion
In this study, we not only verified the strong negative correlation between age and cpRNFLT at an unprecedented level of detail based on over 5600 participants of a population-based study but also demonstrated detailed location-specific effects of the scan diameter independent of as well as in relation to age. Our results with a spatial resolution of 768 measurement points show that both parameters are strongly location-specific, which could not be sufficiently described by previous studies that focused on global averages or coarsely defined sectors. In particular, increasing age and decreasing scan diameter are related to cpRNFLT profiles with more nasalized superior and inferior peaks. The very detailed graphical and numerical presentation of our results in the Appendix may help researchers and manufacturers to improve their normative cpRNFLT models.
A further central finding of this study is the significant “correlation between age and scan diameter” for participants of age 42.1 or older. As cpRNFLT decreases with age as well as with increasing scan diameter commonly reported in literature, the systematic decrease of the diameter with age for participants older than 42.1 years implies that the true age-specific cpRNFLT thinning effect is underestimated for elderly individuals if the values are not corrected for diameter. In addition, there are implications for clinical practice, as current disease progression models for optic neuropathies like glaucoma are typically based on cpRNFLT slopes over time. Our results demonstrate, for instance, that in the absence of diameter correction, which is current clinical practice, a slope that indicates glaucomatous nerve fiber layer thinning in a young patient will be steeper than the slope for an elderly patient, even if both patients suffer from exactly the same level of thinning, because the elderly patient is additionally subject to a decrease of the scan diameter over time.
Previous works typically explained differences in scan diameter with axial ametropia.10,11 For axial myopia, the extension in ocular length yields larger diameters of the projection of the circle on the retina, and cpRNFLT correction models have been proposed based on ocular axial length.10 This effect, however, is unlikely to explain the relationship between diameter and age for elderly participants of the current study, as there are no indications that axial length systematically decreases at higher age. Instead, we assume this relationship to be caused by lens-related effects. Elderly individuals are not only subject to the well-known effect of presbyopia, which concerns near vision, but also to previously documented hyperopic shifts for distance vision.20,21 These lens-related phenomena might explain the systematic decrease in scan diameter, which is otherwise typical for axial hyperopia in younger individuals.
Regarding the particular value of the results of the current investigation compared to the previous studies on ocular magnification and cpRNFLT,10,11 two aspects need to be highlighted. First, our considerably larger sample size of over 5000 subjects substantially improves the reliability of the normative results and furthermore allows an unprecedented level of detail in terms of spatial resolution (measurements at 768 locations on the circle). In the previous studies, fewer than 300 subjects participated (e.g., 269 subjects in the work by Kang et al.10 and 45 subjects in the work by Savini et al).11 Our large age-stratified sample allows us to cover a wide age range from 19 to 80 years, whereas the age range in the work by Kang et al.10 was restricted between 19 and 26 years. Note that optic neuropathies predominantly affect elderly people, which further stresses the additional benefit of the current results. Second, and more importantly, our study adjusts the effects of age and ocular magnification simultaneously. Only by this, we were able to show that age and scan diameter interact for elderly populations, so that adjusting the effects of axial length alone might not be sufficient for the generation of new cpRNFLT norms. This finding, which previous studies were unable to detect, is of special importance for scientists and OCT manufacturers alike.
As all participants who reported to have been diagnosed with glaucoma were excluded, regardless of whether they took glaucoma medication or had any clinically significant findings on their fundus/OCT images or nongradable images, participants who erroneously reported having glaucoma would have been excluded in our study as well. The strict exclusion criteria ensured to discard any subject with possible confounding diseases.
We did not exclude subjects based on cataract. First, cataract does not pathologically affect the cpRNFLT, and second, by excluding all cataract patients, we would unnecessarily bias our normative models. This is of particular importance, as due to the high cataract prevalence in elderly populations, a large proportion of patients presenting at clinical glaucoma services for cpRNFLT measurement will have cataracts, so that cpRNFLT norms should include cataract patients to account for the fact of its frequent occurrence in the total population to avert sampling bias.
This investigation also has limitations. First, the cross-sectional design of this study does not allow tracking changes of the scan diameter over age on an individual base. This will be made possible based on follow-up measurements on the same subjects in future. Second, the dataset contains an imbalanced gender ratio. Potential gender effects should be further investigated as part of future analyses. Third, the current study is based on subjects that are predominantly Caucasian, which restricts the applicability of extracted norms to Caucasian populations, and future studies are needed to investigate how generalizable the results are with respect to other ethnicities. However, it has to be noted that the current normative dataset of the Spectralis SD-OCT device approved by the US Food and Drug Administration is also solely based on a Caucasian population. Last, as the scan diameter reported by the Spectralis machine in mm for each subject is estimated based on the scan focus setting made by the operator and standard corneal curvature with a default value of 7.8 mm for mean anterior corneal radius, two further limitations of Spectralis scan diameter calculation also apply to the current dataset: (a) the manual setting of the focus is subjective and may vary between operators and (b) corneal radius is not measured on an individual basis in the current study.
Axial length was not measured in the course of the LIFE study due to capacity limitations, so it was not available for the current data analysis. The availability of axial length data would extend the scientific utility of the current work. However, none of the clinically used OCT machines currently measures axial length, so its inclusion, while interesting for the scientific community, would probably not be of immediate relevance to the improvement of cpRNFLT norms of current OCT devices. Instead, the current analysis employs scan diameter as the measure of ocular magnification, which is related to axial length and is immediately available from the OCT machine. This scan diameter is routinely calculated by the machine from the scan focus, based on a specific eye model.14 While the major part of scan diameter variance is explained by axial length, it additionally contains lens-related aspects not covered by axial length, and the current investigation indeed found a significant relationship of scan diameter and age, which could not have been revealed by including axial length alone.
The current work is of immediate relevance for scientists, engineers, and OCT manufacturers. The investigation of the impact of age and ocular magnification (scan diameter) on a clinically very important measurement protocol (cpRNFLT) has an unprecedentedly high spatial resolution (768 measurement locations on the scan circle), which can be achieved due to this extraordinarily large sample size (5646 subjects). While this study clearly has clinical utility by demonstrating the considerable impact of these parameters, the main consequence of this work targets research into the engineering of the OCT device itself and its inherent norms. The current work clearly demonstrates that: (a) the location specificity of existing age norms used in the Spectralis OCT machine, based on only 201 subjects,17 can be significantly improved by the presented detailed, high resolution model’ (b) the location specificity and the quantitative effect of the scan diameter is at least as substantial as the effect of age. Diameter effects are currently entirely neglected by OCT machines, and while they have previously been discussed in the literature, although only indirectly in the context of axial length, a location-specific quantification of the effect and the introduction of detailed normative distributions (detailed in Table 4 in the Appendix) are novel, to our best knowledge; (c) we demonstrate that scan diameter decreases with age, which is also, to our best knowledge, an entirely novel finding. One of the conclusions of this newly reported relationship, particularly important for OCT manufacturers, is that it is insufficient to base personalized cpRNFLT norms on axial length, as suggested by numerous previous works. Axial length remains constant in elderly subjects, but the scan diameter nevertheless systematically decreases, which indicates lens-related explanations; and (d) normative models are of particular importance for medical device manufactures with a need to be integrated into OCT machines. The quantitative presentation of our results and the particular level of numerical and statistical details is aimed at research scientists of ophthalmic companies and allows not only the support of the generation of novel cpRNFLT norms, which is the main purpose of our study, but also subsequently the implementation of diagnostic models for disease progression by comparing these normative cpRNFLT slopes to individual slopes of patients, etc.
Table 4.
The age slope, scan diameter slope, and intercept of the multivariate regression model with accompanying values for all 768 measurement points on the scan circle with starting point on the horizontal line towards the temporal direction, as illustrated in Fig. 1.
| Age slope | Age value | Diameter slope | Diameter value | Intercept | Intercept value | |
|---|---|---|---|---|---|---|
| Point 1 | 1.01 | 0.4 | 54.86 | |||
| Point 2 | 1.1 | 0.37 | 55.08 | |||
| Point 3 | 1.21 | 0.32 | 55.17 | |||
| Point 4 | 1.31 | 0.29 | 55.35 | |||
| Point 5 | 1.38 | 0.26 | 55.62 | |||
| Point 6 | 1.53 | 0.22 | 55.62 | |||
| Point 7 | 1.55 | 0.21 | 56.08 | |||
| Point 8 | 1.66 | 0.18 | 56.21 | |||
| Point 9 | 1.76 | 0.16 | 56.35 | |||
| Point 10 | 1.85 | 0.14 | 56.55 | |||
| Point 11 | 1.91 | 0.13 | 56.86 | |||
| Point 12 | 1.86 | 0.14 | 57.54 | |||
| Point 13 | 1.92 | 0.12 | 57.85 | |||
| Point 14 | 2.05 | 0.1 | 57.89 | |||
| Point 15 | 2.1 | 0.09 | 58.24 | |||
| Point 16 | 2.13 | 0.09 | 58.62 | |||
| Point 17 | 2.26 | 0.07 | 58.62 | |||
| Point 18 | 2.37 | 0.05 | 58.7 | |||
| Point 19 | 2.43 | 0.05 | 58.99 | |||
| Point 20 | 2.52 | 0.04 | 59.2 | |||
| Point 21 | 2.64 | 0.03 | 59.18 | |||
| Point 22 | 2.71 | 0.03 | 59.4 | |||
| Point 23 | 2.84 | 0.02 | 59.34 | |||
| Point 24 | 2.9 | 0.02 | 59.55 | |||
| Point 25 | 2.95 | 0.02 | 59.79 | |||
| Point 26 | 2.94 | 0.02 | 60.25 | |||
| Point 27 | 3.01 | 0.02 | 60.38 | |||
| Point 28 | 3.01 | 0.02 | 60.81 | |||
| Point 29 | 3.07 | 0.01 | 60.97 | |||
| Point 30 | 3.15 | 0.01 | 61.07 | |||
| Point 31 | 3.12 | 0.01 | 61.6 | |||
| Point 32 | 3.19 | 0.01 | 61.79 | |||
| Point 33 | 3.15 | 0.01 | 62.33 | |||
| Point 34 | 3.16 | 0.01 | 62.8 | |||
| Point 35 | 3.22 | 0.01 | 62.93 | |||
| Point 36 | 3.17 | 0.01 | 63.61 | |||
| Point 37 | 3.24 | 0.01 | 63.76 | |||
| Point 38 | 3.18 | 0.02 | 64.47 | |||
| Point 39 | 3.23 | 0.01 | 64.71 | |||
| Point 40 | 3.18 | 0.02 | 65.43 | |||
| Point 41 | 3.26 | 0.02 | 65.62 | |||
| Point 42 | 3.25 | 0.02 | 66.12 | |||
| Point 43 | 3.33 | 0.01 | 66.32 | |||
| Point 44 | 3.44 | 0.01 | 66.39 | |||
| Point 45 | 3.61 | 0.009 | 66.24 | |||
| Point 46 | 3.75 | 0.008 | 66.3 | |||
| Point 47 | 3.99 | 0.005 | 65.9 | |||
| Point 48 | 4.21 | 0.003 | 65.61 | |||
| Point 49 | 4.42 | 0.002 | 65.32 | |||
| Point 50 | 4.65 | 0.001 | 64.98 | |||
| Point 51 | 4.82 | 0.001 | 64.85 | |||
| Point 52 | 4.98 | 64.77 | ||||
| Point 53 | 5.14 | 64.7 | ||||
| Point 54 | 5.19 | 64.99 | ||||
| Point 55 | 5.27 | 65.15 | ||||
| Point 56 | 5.37 | 65.3 | ||||
| Point 57 | 5.43 | 65.57 | ||||
| Point 58 | 5.48 | 65.93 | ||||
| Point 59 | 5.64 | 65.85 | ||||
| Point 60 | 5.87 | 65.59 | ||||
| Point 61 | 6.07 | 65.46 | ||||
| Point 62 | 6.24 | 65.43 | ||||
| Point 63 | 6.49 | 65.16 | ||||
| Point 64 | 6.74 | 65.01 | ||||
| Point 65 | 7.03 | 64.64 | ||||
| Point 66 | 7.29 | 64.47 | ||||
| Point 67 | 7.55 | 64.28 | ||||
| Point 68 | 7.65 | 64.7 | ||||
| Point 69 | 7.83 | 64.9 | ||||
| Point 70 | 7.96 | 65.22 | ||||
| Point 71 | 8.03 | 65.81 | ||||
| Point 72 | 8.07 | 66.51 | ||||
| Point 73 | 8.13 | 67.14 | ||||
| Point 74 | 8.17 | 67.86 | ||||
| Point 75 | 8.2 | 68.61 | ||||
| Point 76 | 8.26 | 69.21 | ||||
| Point 77 | 8.3 | 69.84 | ||||
| Point 78 | 8.37 | 70.45 | ||||
| Point 79 | 8.45 | 70.98 | ||||
| Point 80 | 8.54 | 71.46 | ||||
| Point 81 | 8.56 | 72.22 | ||||
| Point 82 | 8.63 | 72.86 | ||||
| Point 83 | 8.63 | 73.76 | ||||
| Point 84 | 8.67 | 74.54 | ||||
| Point 85 | 8.64 | 75.57 | ||||
| Point 86 | 8.69 | 76.36 | ||||
| Point 87 | 8.72 | 77.25 | ||||
| Point 88 | 8.7 | 78.35 | ||||
| Point 89 | 8.71 | 79.37 | ||||
| Point 90 | 8.63 | 80.73 | ||||
| Point 91 | 8.7 | 81.58 | ||||
| Point 92 | 8.74 | 82.56 | ||||
| Point 93 | 8.65 | 83.95 | ||||
| Point 94 | 8.69 | 84.97 | ||||
| Point 95 | 8.65 | 86.23 | ||||
| Point 96 | 8.69 | 87.23 | ||||
| Point 97 | 8.68 | 88.47 | ||||
| Point 98 | 8.71 | 89.52 | ||||
| Point 99 | 8.77 | 90.45 | ||||
| Point 100 | 8.81 | 91.53 | ||||
| Point 101 | 8.9 | 92.4 | ||||
| Point 102 | 8.96 | 0.001 | 93.4 | |||
| Point 103 | 8.98 | 0.001 | 94.51 | |||
| Point 104 | 9 | 0.001 | 95.69 | |||
| Point 105 | 9.02 | 0.001 | 96.82 | |||
| Point 106 | 9.02 | 0.001 | 98.08 | |||
| Point 107 | 8.96 | 0.002 | 99.57 | |||
| Point 108 | 8.94 | 0.002 | 100.93 | |||
| Point 109 | 8.91 | 0.002 | 102.27 | |||
| Point 110 | 8.87 | 0.002 | 103.71 | |||
| Point 111 | 8.84 | 0.003 | 105.14 | |||
| Point 112 | 8.84 | 0.003 | 106.42 | |||
| Point 113 | 8.76 | 0.004 | 108.07 | |||
| Point 114 | 8.65 | 0.004 | 109.79 | |||
| Point 115 | 8.53 | 0.005 | 111.57 | |||
| Point 116 | 8.34 | 0.006 | 113.52 | |||
| Point 117 | 8.19 | 0.008 | 115.36 | |||
| Point 118 | 7.95 | 0.01 | 117.56 | |||
| Point 119 | 7.69 | 0.01 | 119.73 | |||
| Point 120 | 7.34 | 0.02 | 122.18 | |||
| Point 121 | 7 | 0.02 | 124.54 | |||
| Point 122 | 6.56 | 0.04 | 127.24 | |||
| Point 123 | 6.17 | 0.05 | 129.72 | |||
| Point 124 | 5.64 | 0.07 | 132.68 | |||
| Point 125 | 5.05 | 0.11 | 135.78 | |||
| Point 126 | 4.45 | 0.16 | 138.91 | |||
| Point 127 | 3.82 | 0.23 | 142.14 | |||
| Point 128 | 3.08 | 0.33 | 145.69 | |||
| Point 129 | 2.31 | 0.46 | 149.33 | |||
| Point 130 | 1.44 | 0.65 | 153.29 | |||
| Point 131 | 0.64 | 0.84 | 156.97 | |||
| Point 132 | 0.92 | 161.17 | ||||
| Point 133 | 0.67 | 165.56 | ||||
| Point 134 | 0.45 | 170.04 | ||||
| Point 135 | 0.26 | 174.74 | ||||
| Point 136 | 0.13 | 179.55 | ||||
| Point 137 | 0.06 | 184.47 | ||||
| Point 138 | 0.02 | 189.63 | ||||
| Point 139 | 0.006 | 194.82 | ||||
| Point 140 | 0.002 | 200.1 | ||||
| Point 141 | 205.68 | |||||
| Point 142 | 211.17 | |||||
| Point 143 | 217.23 | |||||
| Point 144 | 222.97 | |||||
| Point 145 | 229.14 | |||||
| Point 146 | 235.28 | |||||
| Point 147 | 241.69 | |||||
| Point 148 | 247.82 | |||||
| Point 149 | 253.62 | |||||
| Point 150 | 259.42 | |||||
| Point 151 | 264.78 | |||||
| Point 152 | 269.83 | |||||
| Point 153 | 275.04 | |||||
| Point 154 | 279.25 | |||||
| Point 155 | 283.66 | |||||
| Point 156 | 288.17 | |||||
| Point 157 | 292.4 | |||||
| Point 158 | 296.42 | |||||
| Point 159 | 300.17 | |||||
| Point 160 | 303.88 | |||||
| Point 161 | 307.11 | |||||
| Point 162 | 310.27 | |||||
| Point 163 | 312.8 | |||||
| Point 164 | 315.23 | |||||
| Point 165 | 317.64 | |||||
| Point 166 | 319.85 | |||||
| Point 167 | 322 | |||||
| Point 168 | 324.08 | |||||
| Point 169 | 326.42 | |||||
| Point 170 | 328.71 | |||||
| Point 171 | 330.66 | |||||
| Point 172 | 332.85 | |||||
| Point 173 | 334.58 | |||||
| Point 174 | 336.5 | |||||
| Point 175 | 338.08 | |||||
| Point 176 | 339.45 | |||||
| Point 177 | 0.001 | 340.68 | ||||
| Point 178 | 0.002 | 341.34 | ||||
| Point 179 | 0.003 | 342.29 | ||||
| Point 180 | 0.005 | 342.53 | ||||
| Point 181 | 0.007 | 342.96 | ||||
| Point 182 | 0.009 | 342.82 | ||||
| Point 183 | 0.01 | 342.34 | ||||
| Point 184 | 0.01 | 341.54 | ||||
| Point 185 | 0.01 | 340.62 | ||||
| Point 186 | 0.02 | 339.16 | ||||
| Point 187 | 0.02 | 337.47 | ||||
| Point 188 | 0.02 | 335.49 | ||||
| Point 189 | 0.02 | 332.82 | ||||
| Point 190 | 0.02 | 329.78 | ||||
| Point 191 | 0.02 | 326.57 | ||||
| Point 192 | 0.02 | 322.64 | ||||
| Point 193 | 0.02 | 318.49 | ||||
| Point 194 | 0.03 | 314.54 | ||||
| Point 195 | 0.03 | 310.58 | ||||
| Point 196 | 0.03 | 306.28 | ||||
| Point 197 | 0.03 | 302.32 | ||||
| Point 198 | 0.03 | 298.55 | ||||
| Point 199 | 0.03 | 294.7 | ||||
| Point 200 | 0.03 | 291.18 | ||||
| Point 201 | 0.03 | 287.71 | ||||
| Point 202 | 0.03 | 284.22 | ||||
| Point 203 | 0.03 | 280.41 | ||||
| Point 204 | 0.02 | 276.83 | ||||
| Point 205 | 0.02 | 272.76 | ||||
| Point 206 | 0.02 | 268.81 | ||||
| Point 207 | 0.02 | 264.62 | ||||
| Point 208 | 0.03 | 260.3 | ||||
| Point 209 | 0.03 | 256.1 | ||||
| Point 210 | 0.03 | 252.03 | ||||
| Point 211 | 0.02 | 247.7 | ||||
| Point 212 | 0.02 | 243.66 | ||||
| Point 213 | 0.02 | 239.57 | ||||
| Point 214 | 0.01 | 235.74 | ||||
| Point 215 | 0.009 | 232.3 | ||||
| Point 216 | 0.005 | 229.13 | ||||
| Point 217 | 0.003 | 225.76 | ||||
| Point 218 | 0.001 | 222.88 | ||||
| Point 219 | 220.21 | |||||
| Point 220 | 217.66 | |||||
| Point 221 | 215.6 | |||||
| Point 222 | 213.86 | |||||
| Point 223 | 211.63 | |||||
| Point 224 | 209.96 | |||||
| Point 225 | 208.3 | |||||
| Point 226 | 206.34 | |||||
| Point 227 | 204.7 | |||||
| Point 228 | 202.9 | |||||
| Point 229 | 201.35 | |||||
| Point 230 | 199.89 | |||||
| Point 231 | 198.3 | |||||
| Point 232 | 197.08 | |||||
| Point 233 | 195.52 | |||||
| Point 234 | 194.27 | |||||
| Point 235 | 192.99 | |||||
| Point 236 | 191.97 | |||||
| Point 237 | 191.33 | |||||
| Point 238 | 190.32 | |||||
| Point 239 | 189.81 | |||||
| Point 240 | 189.69 | |||||
| Point 241 | 189.52 | |||||
| Point 242 | 189.55 | |||||
| Point 243 | 190.04 | |||||
| Point 244 | 190.79 | |||||
| Point 245 | 191.46 | |||||
| Point 246 | 192.81 | |||||
| Point 247 | 194.43 | |||||
| Point 248 | 196.07 | |||||
| Point 249 | 197.76 | |||||
| Point 250 | 199.69 | |||||
| Point 251 | 201.47 | |||||
| Point 252 | 203.79 | |||||
| Point 253 | 205.57 | |||||
| Point 254 | 207.91 | |||||
| Point 255 | 209.86 | |||||
| Point 256 | 212.18 | |||||
| Point 257 | 214.24 | |||||
| Point 258 | 216.56 | |||||
| Point 259 | 219.03 | |||||
| Point 260 | 221.31 | |||||
| Point 261 | 223.88 | |||||
| Point 262 | 226.51 | |||||
| Point 263 | 228.89 | |||||
| Point 264 | 231.58 | |||||
| Point 265 | 234.03 | |||||
| Point 266 | 236.48 | |||||
| Point 267 | 238.81 | |||||
| Point 268 | 240.68 | |||||
| Point 269 | 242.79 | |||||
| Point 270 | 244.37 | |||||
| Point 271 | 246.04 | |||||
| Point 272 | 247.5 | |||||
| Point 273 | 249.03 | |||||
| Point 274 | 250.44 | |||||
| Point 275 | 251.69 | |||||
| Point 276 | 252.87 | |||||
| Point 277 | 254.1 | |||||
| Point 278 | 255.94 | |||||
| Point 279 | 257.59 | |||||
| Point 280 | 259.2 | |||||
| Point 281 | 260.84 | |||||
| Point 282 | 262.72 | |||||
| Point 283 | 263.97 | |||||
| Point 284 | 265.56 | |||||
| Point 285 | 266.89 | |||||
| Point 286 | 267.67 | |||||
| Point 287 | 268.62 | |||||
| Point 288 | 269.09 | |||||
| Point 289 | 269.33 | |||||
| Point 290 | 269.71 | |||||
| Point 291 | 269.5 | |||||
| Point 292 | 269.2 | |||||
| Point 293 | 269.13 | |||||
| Point 294 | 269.31 | |||||
| Point 295 | 269.21 | |||||
| Point 296 | 269.08 | |||||
| Point 297 | 268.95 | |||||
| Point 298 | 268.63 | |||||
| Point 299 | 268.48 | |||||
| Point 300 | 268.38 | |||||
| Point 301 | 268.41 | |||||
| Point 302 | 268.26 | |||||
| Point 303 | 268.32 | |||||
| Point 304 | 268.09 | |||||
| Point 305 | 268.16 | |||||
| Point 306 | 267.9 | |||||
| Point 307 | 267.71 | |||||
| Point 308 | 267.31 | |||||
| Point 309 | 266.81 | |||||
| Point 310 | 266.37 | |||||
| Point 311 | 265.93 | |||||
| Point 312 | 265.28 | |||||
| Point 313 | 264.55 | |||||
| Point 314 | 264.11 | |||||
| Point 315 | 262.87 | |||||
| Point 316 | 261.69 | |||||
| Point 317 | 260.24 | |||||
| Point 318 | 259 | |||||
| Point 319 | 257.3 | |||||
| Point 320 | 255.96 | |||||
| Point 321 | 254.38 | |||||
| Point 322 | 253.13 | |||||
| Point 323 | 251.63 | |||||
| Point 324 | 250.51 | |||||
| Point 325 | 249.54 | |||||
| Point 326 | 248.36 | |||||
| Point 327 | 247.13 | |||||
| Point 328 | 245.92 | |||||
| Point 329 | 244.25 | |||||
| Point 330 | 242.6 | |||||
| Point 331 | 240.72 | |||||
| Point 332 | 238.48 | |||||
| Point 333 | 236.32 | |||||
| Point 334 | 0.001 | 234.34 | ||||
| Point 335 | 0.002 | 232.18 | ||||
| Point 336 | 0.004 | 230.02 | ||||
| Point 337 | 0.007 | 227.91 | ||||
| Point 338 | 0.01 | 226.06 | ||||
| Point 339 | 0.02 | 224.55 | ||||
| Point 340 | 0.03 | 222.87 | ||||
| Point 341 | 0.04 | 221.4 | ||||
| Point 342 | 0.06 | 219.96 | ||||
| Point 343 | 0.07 | 219.21 | ||||
| Point 344 | 0.08 | 218.3 | ||||
| Point 345 | 0.1 | 217.89 | ||||
| Point 346 | 0.12 | 217.18 | ||||
| Point 347 | 0.12 | 216.67 | ||||
| Point 348 | 0.13 | 215.97 | ||||
| Point 349 | 0.13 | 215.17 | ||||
| Point 350 | 0.14 | 214.2 | ||||
| Point 351 | 0.13 | 212.69 | ||||
| Point 352 | 0.15 | 210.59 | ||||
| Point 353 | 0.15 | 208.7 | ||||
| Point 354 | 0.16 | 206.39 | ||||
| Point 355 | 0.17 | 203.75 | ||||
| Point 356 | 0.18 | 201.26 | ||||
| Point 357 | 0.18 | 199.11 | ||||
| Point 358 | 0.21 | 196.74 | ||||
| Point 359 | 0.23 | 194.4 | ||||
| Point 360 | 0.25 | 192.39 | ||||
| Point 361 | 0.29 | 190.13 | ||||
| Point 362 | 0.35 | 188.01 | ||||
| Point 363 | 0.39 | 185.87 | ||||
| Point 364 | 0.51 | 183.79 | ||||
| Point 365 | 0.61 | 181.1 | ||||
| Point 366 | 0.74 | 179.08 | ||||
| Point 367 | 0 | 0.85 | 176.69 | |||
| Point 368 | 0 | 0.92 | 174.61 | |||
| Point 369 | 0 | 0.99 | 172.23 | |||
| Point 370 | 0 | 0.92 | 170.06 | |||
| Point 371 | 0 | 0.89 | 167.8 | |||
| Point 372 | 0.01 | 0.81 | 165.55 | |||
| Point 373 | 0.01 | 0.77 | 163.06 | |||
| Point 374 | 0.01 | 0.71 | 160.55 | |||
| Point 375 | 0.01 | 0.63 | 158.35 | |||
| Point 376 | 0.01 | 0.63 | 155.45 | |||
| Point 377 | 0.01 | 0.61 | 153.27 | |||
| Point 378 | 0.01 | 0.6 | 150.97 | |||
| Point 379 | 0.01 | 0.61 | 149.18 | |||
| Point 380 | 0.01 | 0.63 | 147.21 | |||
| Point 381 | 0.01 | 0.68 | 145.89 | |||
| Point 382 | 0.01 | 0.69 | 144.33 | |||
| Point 383 | 0.01 | 0.77 | 143.49 | |||
| Point 384 | 0.01 | 0.8 | 142.29 | |||
| Point 385 | 0 | 0.85 | 140.99 | |||
| Point 386 | 0 | 0.86 | 140.13 | |||
| Point 387 | 0 | 0.92 | 138.99 | |||
| Point 388 | 0 | 0.92 | 137.86 | |||
| Point 389 | 0 | 0.9 | 136.7 | |||
| Point 390 | 0 | 0.9 | 135.88 | |||
| Point 391 | 0 | 0.92 | 135.15 | |||
| Point 392 | 0 | 0.92 | 134.3 | |||
| Point 393 | 0 | 0.91 | 133.31 | |||
| Point 394 | 0 | 0.9 | 132.42 | |||
| Point 395 | 0 | 0.9 | 131.85 | |||
| Point 396 | 0 | 0.87 | 131.02 | |||
| Point 397 | 0 | 0.89 | 130.46 | |||
| Point 398 | 0 | 0.85 | 129.45 | |||
| Point 399 | 0 | 0.86 | 129.03 | |||
| Point 400 | 0 | 0.82 | 127.98 | |||
| Point 401 | 0.01 | 0.79 | 127.05 | |||
| Point 402 | 0 | 0.81 | 126.25 | |||
| Point 403 | 0 | 0.82 | 125.6 | |||
| Point 404 | 0 | 0.85 | 125.19 | |||
| Point 405 | 0 | 0.93 | 125.08 | |||
| Point 406 | 0 | 0.97 | 124.98 | |||
| Point 407 | 0 | 0.91 | 124.88 | |||
| Point 408 | 0.78 | 125.38 | ||||
| Point 409 | 0.69 | 125.46 | ||||
| Point 410 | 0.56 | 125.98 | ||||
| Point 411 | 0.47 | 126.22 | ||||
| Point 412 | 0.37 | 126.66 | ||||
| Point 413 | 0.31 | 127.05 | ||||
| Point 414 | 0.26 | 127.82 | ||||
| Point 415 | 0.23 | 128.37 | ||||
| Point 416 | 0.18 | 129.19 | ||||
| Point 417 | 0.16 | 130.27 | ||||
| Point 418 | 0.13 | 131.35 | ||||
| Point 419 | 0.11 | 132.22 | ||||
| Point 420 | 0.1 | 133.32 | ||||
| Point 421 | 0.09 | 134.63 | ||||
| Point 422 | 0.08 | 135.85 | ||||
| Point 423 | 0.07 | 137.6 | ||||
| Point 424 | 0.06 | 139.07 | ||||
| Point 425 | 0.06 | 140.76 | ||||
| Point 426 | 0.04 | 142.75 | ||||
| Point 427 | 0.04 | 144.21 | ||||
| Point 428 | 0.03 | 146.22 | ||||
| Point 429 | 0.02 | 147.94 | ||||
| Point 430 | 0.02 | 149.56 | ||||
| Point 431 | 0.01 | 151.23 | ||||
| Point 432 | 0.01 | 152.58 | ||||
| Point 433 | 0.008 | 153.8 | ||||
| Point 434 | 0.007 | 154.72 | ||||
| Point 435 | 0.006 | 155.41 | ||||
| Point 436 | 0.005 | 156.32 | ||||
| Point 437 | 0.004 | 157.12 | ||||
| Point 438 | 0.004 | 157.65 | ||||
| Point 439 | 0.003 | 158.66 | ||||
| Point 440 | 0.003 | 159.76 | ||||
| Point 441 | 0.002 | 160.85 | ||||
| Point 442 | 0.002 | 162.33 | ||||
| Point 443 | 0.002 | 163.17 | ||||
| Point 444 | 0.002 | 164.58 | ||||
| Point 445 | 0.001 | 166.27 | ||||
| Point 446 | 167.87 | |||||
| Point 447 | 169.66 | |||||
| Point 448 | 171.18 | |||||
| Point 449 | 172.96 | |||||
| Point 450 | 174.57 | |||||
| Point 451 | 176.35 | |||||
| Point 452 | 177.9 | |||||
| Point 453 | 179.59 | |||||
| Point 454 | 181.25 | |||||
| Point 455 | 182.9 | |||||
| Point 456 | 184.62 | |||||
| Point 457 | 186.43 | |||||
| Point 458 | 188.58 | |||||
| Point 459 | 190.72 | |||||
| Point 460 | 192.68 | |||||
| Point 461 | 194.94 | |||||
| Point 462 | 197.16 | |||||
| Point 463 | 199.59 | |||||
| Point 464 | 201.71 | |||||
| Point 465 | 204.21 | |||||
| Point 466 | 206.55 | |||||
| Point 467 | 209.35 | |||||
| Point 468 | 211.55 | |||||
| Point 469 | 214 | |||||
| Point 470 | 216.25 | |||||
| Point 471 | 218.3 | |||||
| Point 472 | 220.46 | |||||
| Point 473 | 222.39 | |||||
| Point 474 | 224.73 | |||||
| Point 475 | 226.68 | |||||
| Point 476 | 228.85 | |||||
| Point 477 | 230.5 | |||||
| Point 478 | 232.18 | |||||
| Point 479 | 233.74 | |||||
| Point 480 | 235.13 | |||||
| Point 481 | 236.31 | |||||
| Point 482 | 237.59 | |||||
| Point 483 | 238.5 | |||||
| Point 484 | 239.56 | |||||
| Point 485 | 240.7 | |||||
| Point 486 | 241.67 | |||||
| Point 487 | 242.77 | |||||
| Point 488 | 243.99 | |||||
| Point 489 | 244.99 | |||||
| Point 490 | 246.43 | |||||
| Point 491 | 247.77 | |||||
| Point 492 | 249.4 | |||||
| Point 493 | 251.05 | |||||
| Point 494 | 252.96 | |||||
| Point 495 | 254.69 | |||||
| Point 496 | 256.42 | |||||
| Point 497 | 258.07 | |||||
| Point 498 | 259.8 | |||||
| Point 499 | 261.5 | |||||
| Point 500 | 262.98 | |||||
| Point 501 | 264.46 | |||||
| Point 502 | 265.58 | |||||
| Point 503 | 266.57 | |||||
| Point 504 | 266.77 | |||||
| Point 505 | 267.28 | |||||
| Point 506 | 267.29 | |||||
| Point 507 | 267.07 | |||||
| Point 508 | 266.87 | |||||
| Point 509 | 266.3 | |||||
| Point 510 | 266.21 | |||||
| Point 511 | 265.65 | |||||
| Point 512 | 265.05 | |||||
| Point 513 | 265.02 | |||||
| Point 514 | 264.93 | |||||
| Point 515 | 264.65 | |||||
| Point 516 | 264.67 | |||||
| Point 517 | 264.86 | |||||
| Point 518 | 265.31 | |||||
| Point 519 | 265.34 | |||||
| Point 520 | 265.89 | |||||
| Point 521 | 266.17 | |||||
| Point 522 | 266.78 | |||||
| Point 523 | 267.81 | |||||
| Point 524 | 268.79 | |||||
| Point 525 | 270.1 | |||||
| Point 526 | 271.57 | |||||
| Point 527 | 273.1 | |||||
| Point 528 | 275.16 | |||||
| Point 529 | 277.3 | |||||
| Point 530 | 279.59 | |||||
| Point 531 | 282.38 | |||||
| Point 532 | 285.12 | |||||
| Point 533 | 288.38 | |||||
| Point 534 | 291.75 | |||||
| Point 535 | 295.08 | |||||
| Point 536 | 298.64 | |||||
| Point 537 | 302.27 | |||||
| Point 538 | 305.75 | |||||
| Point 539 | 309.38 | |||||
| Point 540 | 313.14 | |||||
| Point 541 | 316.47 | |||||
| Point 542 | 320.28 | |||||
| Point 543 | 323.31 | |||||
| Point 544 | 326.5 | |||||
| Point 545 | 329.65 | |||||
| Point 546 | 332.47 | |||||
| Point 547 | 334.92 | |||||
| Point 548 | 337.6 | |||||
| Point 549 | 339.65 | |||||
| Point 550 | 341.64 | |||||
| Point 551 | 343.4 | |||||
| Point 552 | 345.14 | |||||
| Point 553 | 346.8 | |||||
| Point 554 | 348.21 | |||||
| Point 555 | 349.44 | |||||
| Point 556 | 350.76 | |||||
| Point 557 | 351.86 | |||||
| Point 558 | 352.92 | |||||
| Point 559 | 354.17 | |||||
| Point 560 | 355.03 | |||||
| Point 561 | 355.84 | |||||
| Point 562 | 356.58 | |||||
| Point 563 | 357.13 | |||||
| Point 564 | 357.72 | |||||
| Point 565 | 358.1 | |||||
| Point 566 | 358.24 | |||||
| Point 567 | 358.33 | |||||
| Point 568 | 358.44 | |||||
| Point 569 | 358.35 | |||||
| Point 570 | 358.16 | |||||
| Point 571 | 358.15 | |||||
| Point 572 | 357.52 | |||||
| Point 573 | 357.33 | |||||
| Point 574 | 356.93 | |||||
| Point 575 | 356.36 | |||||
| Point 576 | 355.55 | |||||
| Point 577 | 354.54 | |||||
| Point 578 | 353.41 | |||||
| Point 579 | 352.03 | |||||
| Point 580 | 350.76 | |||||
| Point 581 | 348.97 | |||||
| Point 582 | 347.32 | |||||
| Point 583 | 345.91 | |||||
| Point 584 | 344.1 | |||||
| Point 585 | 342.4 | |||||
| Point 586 | 340.32 | |||||
| Point 587 | 338.67 | |||||
| Point 588 | 337 | |||||
| Point 589 | 334.97 | |||||
| Point 590 | 332.95 | |||||
| Point 591 | 331.02 | |||||
| Point 592 | 329.27 | |||||
| Point 593 | 327.47 | |||||
| Point 594 | 326.05 | |||||
| Point 595 | 324.89 | |||||
| Point 596 | 323.86 | |||||
| Point 597 | 323.23 | |||||
| Point 598 | 322.89 | |||||
| Point 599 | 322.3 | |||||
| Point 600 | 322.07 | |||||
| Point 601 | 321.8 | |||||
| Point 602 | 321.22 | |||||
| Point 603 | 320.61 | |||||
| Point 604 | 320.07 | |||||
| Point 605 | 319.3 | |||||
| Point 606 | 318.26 | |||||
| Point 607 | 316.98 | |||||
| Point 608 | 315.5 | |||||
| Point 609 | 314.12 | |||||
| Point 610 | 312.31 | |||||
| Point 611 | 310.72 | |||||
| Point 612 | 309.16 | |||||
| Point 613 | 307.46 | |||||
| Point 614 | 305.97 | |||||
| Point 615 | 304.49 | |||||
| Point 616 | 303.29 | |||||
| Point 617 | 301.71 | |||||
| Point 618 | 300.43 | |||||
| Point 619 | 298.63 | |||||
| Point 620 | 296.45 | |||||
| Point 621 | 293.98 | |||||
| Point 622 | 291.53 | |||||
| Point 623 | 288.54 | |||||
| Point 624 | 284.92 | |||||
| Point 625 | 281.56 | |||||
| Point 626 | 277.65 | |||||
| Point 627 | 273.04 | |||||
| Point 628 | 268.32 | |||||
| Point 629 | 263.5 | |||||
| Point 630 | 258.26 | |||||
| Point 631 | 252.54 | |||||
| Point 632 | 246.99 | |||||
| Point 633 | 241.22 | |||||
| Point 634 | 235.16 | |||||
| Point 635 | 228.88 | |||||
| Point 636 | 222.56 | |||||
| Point 637 | 215.78 | |||||
| Point 638 | 208.76 | |||||
| Point 639 | 0.004 | 201.94 | ||||
| Point 640 | 0.02 | 194.68 | ||||
| Point 641 | 0.08 | 187.38 | ||||
| Point 642 | 0.25 | 179.86 | ||||
| Point 643 | 0.54 | 172.58 | ||||
| Point 644 | 0.94 | 165.23 | ||||
| Point 645 | 1.29 | 0.69 | 158.48 | |||
| Point 646 | 2.84 | 0.39 | 151.69 | |||
| Point 647 | 4.33 | 0.2 | 145.05 | |||
| Point 648 | 5.74 | 0.09 | 138.67 | |||
| Point 649 | 6.95 | 0.04 | 132.95 | |||
| Point 650 | 8.17 | 0.02 | 127.18 | |||
| Point 651 | 9.32 | 0.006 | 121.64 | |||
| Point 652 | 10.34 | 0.002 | 116.57 | |||
| Point 653 | 11.39 | 111.3 | ||||
| Point 654 | 12.34 | 106.37 | ||||
| Point 655 | 13.19 | 101.8 | ||||
| Point 656 | 13.94 | 97.55 | ||||
| Point 657 | 14.7 | 93.2 | ||||
| Point 658 | 15.31 | 89.46 | ||||
| Point 659 | 15.94 | 85.52 | ||||
| Point 660 | 16.45 | 82.03 | ||||
| Point 661 | 16.98 | 78.44 | ||||
| Point 662 | 17.4 | 75.19 | ||||
| Point 663 | 17.79 | 72.08 | ||||
| Point 664 | 18.09 | 69.26 | ||||
| Point 665 | 18.4 | 66.38 | ||||
| Point 666 | 18.66 | 63.64 | ||||
| Point 667 | 18.84 | 61.25 | ||||
| Point 668 | 18.92 | 59.19 | ||||
| Point 669 | 19.03 | 57.04 | ||||
| Point 670 | 19.1 | 55.04 | ||||
| Point 671 | 19.03 | 53.55 | ||||
| Point 672 | 18.89 | 52.37 | ||||
| Point 673 | 18.78 | 51.08 | ||||
| Point 674 | 18.45 | 50.55 | ||||
| Point 675 | 18.2 | 49.86 | ||||
| Point 676 | 17.89 | 49.32 | ||||
| Point 677 | 17.45 | 49.3 | ||||
| Point 678 | 17.14 | 48.78 | ||||
| Point 679 | 16.76 | 48.6 | ||||
| Point 680 | 16.47 | 48.1 | ||||
| Point 681 | 16.14 | 47.75 | ||||
| Point 682 | 15.86 | 47.3 | ||||
| Point 683 | 15.47 | 47.19 | ||||
| Point 684 | 15.14 | 46.97 | ||||
| Point 685 | 14.9 | 46.39 | ||||
| Point 686 | 14.71 | 45.65 | ||||
| Point 687 | 14.44 | 45.26 | ||||
| Point 688 | 14.39 | 44.07 | ||||
| Point 689 | 14.26 | 43.23 | ||||
| Point 690 | 14.18 | 42.23 | ||||
| Point 691 | 14.09 | 41.29 | ||||
| Point 692 | 14.01 | 40.38 | ||||
| Point 693 | 13.97 | 39.3 | ||||
| Point 694 | 13.75 | 38.88 | ||||
| Point 695 | 13.61 | 38.3 | ||||
| Point 696 | 13.43 | 37.83 | ||||
| Point 697 | 13.25 | 37.35 | ||||
| Point 698 | 13.06 | 36.97 | ||||
| Point 699 | 12.84 | 36.65 | ||||
| Point 700 | 12.62 | 36.43 | ||||
| Point 701 | 12.46 | 35.93 | ||||
| Point 702 | 12.25 | 35.64 | ||||
| Point 703 | 12.12 | 35.08 | ||||
| Point 704 | 11.96 | 34.61 | ||||
| Point 705 | 11.88 | 33.86 | ||||
| Point 706 | 11.63 | 33.77 | ||||
| Point 707 | 11.57 | 33.03 | ||||
| Point 708 | 11.38 | 32.72 | ||||
| Point 709 | 11.22 | 32.33 | ||||
| Point 710 | 11.05 | 32.01 | ||||
| Point 711 | 10.84 | 31.78 | ||||
| Point 712 | 10.61 | 31.71 | ||||
| Point 713 | 10.37 | 31.65 | ||||
| Point 714 | 10.15 | 31.54 | ||||
| Point 715 | 9.86 | 31.69 | ||||
| Point 716 | 9.73 | 31.2 | ||||
| Point 717 | 9.44 | 31.37 | ||||
| Point 718 | 9.21 | 31.33 | ||||
| Point 719 | 8.86 | 31.73 | ||||
| Point 720 | 8.57 | 31.97 | ||||
| Point 721 | 8.26 | 32.3 | ||||
| Point 722 | 7.99 | 32.58 | ||||
| Point 723 | 7.73 | 32.77 | ||||
| Point 724 | 7.42 | 33.25 | ||||
| Point 725 | 7.15 | 33.6 | ||||
| Point 726 | 6.94 | 33.77 | ||||
| Point 727 | 6.71 | 34 | ||||
| Point 728 | 6.47 | 34.3 | ||||
| Point 729 | 6.3 | 34.41 | ||||
| Point 730 | 6.2 | 34.26 | ||||
| Point 731 | 6.04 | 34.36 | ||||
| Point 732 | 5.89 | 34.41 | ||||
| Point 733 | 5.65 | 34.84 | <0.001 | |||
| Point 734 | 5.43 | 35.23 | <0.001 | |||
| Point 735 | 5.14 | 35.9 | ||||
| Point 736 | 0.001 | 4.82 | 36.7 | |||
| Point 737 | 0.001 | 4.56 | 37.34 | |||
| Point 738 | 0.001 | 4.21 | 38.37 | |||
| Point 739 | 0.002 | 3.97 | 39 | |||
| Point 740 | 0.001 | 3.64 | 40.02 | |||
| Point 741 | 0.001 | 3.41 | 0.001 | 40.74 | ||
| Point 742 | 0.001 | 3.2 | 0.002 | 41.4 | ||
| Point 743 | 2.93 | 0.005 | 42.29 | |||
| Point 744 | 2.77 | 0.008 | 42.85 | |||
| Point 745 | 2.5 | 0.02 | 43.8 | |||
| Point 746 | 2.38 | 0.02 | 44.23 | |||
| Point 747 | 2.17 | 0.04 | 44.98 | |||
| Point 748 | 2.07 | 0.05 | 45.37 | |||
| Point 749 | 1.9 | 0.08 | 45.97 | |||
| Point 750 | 1.78 | 0.1 | 46.43 | |||
| Point 751 | 1.69 | 0.12 | 46.73 | |||
| Point 752 | 1.57 | 0.15 | 47.25 | |||
| Point 753 | 1.49 | 0.18 | 47.56 | |||
| Point 754 | 1.44 | 0.19 | 47.86 | |||
| Point 755 | 0.001 | 1.36 | 0.22 | 48.23 | ||
| Point 756 | 0.001 | 1.29 | 0.25 | 48.6 | ||
| Point 757 | 0.001 | 1.26 | 0.26 | 48.92 | ||
| Point 758 | 0.001 | 1.13 | 0.32 | 49.59 | ||
| Point 759 | 1.03 | 0.37 | 50.21 | |||
| Point 760 | 1.01 | 0.38 | 50.61 | |||
| Point 761 | 0.99 | 0.39 | 51.06 | |||
| Point 762 | 0.87 | 0.45 | 51.89 | |||
| Point 763 | 0.82 | 0.48 | 52.54 | |||
| Point 764 | 0.81 | 0.49 | 53.05 | |||
| Point 765 | 0.77 | 0.51 | 53.66 | |||
| Point 766 | 0.81 | 0.5 | 54.06 | |||
| Point 767 | 0.79 | 0.51 | 54.62 | |||
| Point 768 | 0.93 | 0.44 | 54.64 |
To summarize, in this work, we study the interrelationship between cpRNFLT, age, and scan diameter at an unprecedented level of detail. These results may help researchers and manufacturers to improve their normative cpRNFLT models. Besides, we reveal a systematic relationship between age and diameter, which is restricted to elderly people based on our results. This finding likely has clinical relevance, as current disease progression methods to quantify cpRNFLT thinning over time are based on slopes, which are assumed to be independent of the baseline age of patients. Therefore, pathological cpRNFLT thinning might be underestimated in elderly patients compared to younger patients.
Acknowledgments
This publication is supported by Leipzig Research Centre for Civilization Diseases (LIFE), an organizational unit affiliated to the Medical Faculty of Leipzig University. LIFE is funded by means of the European Union, by the European Regional Development Fund (ERDF) and by funds of the Free State of Saxony within the framework of the excellence initiative (project numbers: 713-241202, 713-241202, 14505/2470, 14575/2470). This work is also supported by the following organization and grants BrightFocus Foundation, Lions Foundation, Grimshaw-Gudewicz Foundation, Research to Prevent Blindness, NEI Core Grant P30EYE003790 and NIH Grants R21 EY027882. The authors would like to express their sincere thanks to Verena Brendler (LIFE) and Yvonne Dietz (LIFE) for data management and for obtaining the combined parameters to make this analysis possible. Furthermore, the authors would like to thank Dr. Matthias Nuechter (LIFE) for his enthusiastic support for this collaborative research.
Biographies
Mengyu Wang is a postdoctoral fellow in ophthalmology at Harvard Medical School. He received his PhD degree in structural engineering and mechanics from the University of Pittsburgh in 2014. He has a diverse research background from computational mechanics, breast cancer imaging of ophthalmology. His current research focuses on developing computational approaches using image processing, statistics, machine learning, and biomechanics to better understand eye diseases and eventually improve diagnosis, prognosis, and treatment to save sight.
Tobias Elze is an assistant professor in ophthalmology at Harvard Medical School. He received his PhD degree in computer science from Max Planck Institute for Mathematics in the Sciences in Leipzig, Germany, in 2011. He is the author of more than 20 research papers. His current research interests include applications of optical coherence tomography to the field of ophthalmology in order to improve the diagnosis of eye diseases and to monitor their progression over time.
Franziska G. Rauscher is a vision scientist at Leipzig University, Germany. She received her PhD in visual science from City University London in 2009. Her expertise covers both theoretical and applied aspects of optics, vision science, and ophthalmology. She heads a multidisciplinary team on diverse topics in experimental ophthalmology centered on various imaging modalities. Furthermore, she is leading the eye examinations within two large population-based studies, extracting inter-relationships leading to a new knowledge-base.
Biographies for the other authors are not available.
Appendix.
Table 4 provides the numerical coefficients of age slope, scan diameter slope, and intercept for the multivariate regression models of cpRNFLT for all 768 measurement points on the scan circle with starting point on the horizontal line towards the temporal direction. Table 4 may help scientists or manufacturers to apply both age and diameter corrections to cpRNFLT measurements.
Disclosures
None of the authors has any conflict of interest to disclose.
References
- 1.Medeiros F. A., et al. , “Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography,” Am. J. Ophthalmol. 139(1), 44–55 (2005). 10.1016/j.ajo.2004.08.069 [DOI] [PubMed] [Google Scholar]
- 2.Kanamori A., et al. , “Evaluation of the glaucomatous damage on retinal nerve fiber layer thickness measured by optical coherence tomography,” Am. J. Ophthalmol. 135(4), 513–520 (2003). 10.1016/S0002-9394(02)02003-2 [DOI] [PubMed] [Google Scholar]
- 3.Bendschneider D., et al. , “Retinal nerve fiber layer thickness in normals measured by spectral domain OCT,” J. Glaucoma 19(7), 475–482 (2010). 10.1097/IJG.0b013e3181c4b0c7 [DOI] [PubMed] [Google Scholar]
- 4.Bowd C., et al. , “Imaging of the optic disc and retinal nerve fiber layer: the effects of age, optic disc area, refractive error, and gender,” J. Opt. Soc. Am. A 19(1), 197–207 (2002). 10.1364/JOSAA.19.000197 [DOI] [PubMed] [Google Scholar]
- 5.Parikh R. S., et al. , “Normal age-related decay of retinal nerve fiber layer thickness,” Ophthalmology 114(5), 921–926 (2007). 10.1016/j.ophtha.2007.01.023 [DOI] [PubMed] [Google Scholar]
- 6.Leung C. K., et al. , “Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a prospective analysis of age-related loss,” Ophthalmology 119(4), 731–737 (2012). 10.1016/j.ophtha.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 7.Sung K. R., et al. , “Effects of age on optical coherence tomography measurements of healthy retinal nerve fiber layer, macula, and optic nerve head,” Ophthalmology 116(6), 1119–1124 (2009). 10.1016/j.ophtha.2009.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budenz D. L., et al. , “Determinants of normal retinal nerve fiber layer thickness measured by stratus OCT,” Ophthalmology 114(6), 1046–1052 (2007). 10.1016/j.ophtha.2006.08.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bayraktar S., Bayraktar Z., Yilmaz Ö. F., “Influence of scan radius correction for ocular magnification and relationship between scan radius with retinal nerve fiber layer thickness measured by optical coherence tomography,” J. Glaucoma 10(3), 163–169 (2001). 10.1097/00061198-200106000-00004 [DOI] [PubMed] [Google Scholar]
- 10.Kang S. H., et al. , “Effect of myopia on the thickness of the retinal nerve fiber layer measured by cirrus HD optical coherence tomography,” Invest. Ophthalmol. Visual Sci. 51(8), 4075–4083 (2010). 10.1167/iovs.09-4737 [DOI] [PubMed] [Google Scholar]
- 11.Savini G., et al. , “The influence of axial length on retinal nerve fibre layer thickness and optic-disc size measurements by spectral-domain OCT,” Br. J. Ophthalmol. 96(1), 57–61 (2011). 10.1136/bjo.2010.196782 [DOI] [PubMed] [Google Scholar]
- 12.Hood D. C., “Improving our understanding, and detection, of glaucomatous damage: an approach based upon optical coherence tomography (OCT),” Prog. Retinal Eye Res. 57, 46–75 (2017). 10.1016/j.preteyeres.2016.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nowroozizadeh S., et al. , “Influence of correction of ocular magnification on spectral-domain OCT retinal nerve fiber layer measurement variability and performance influence of ocular magnification on RNFL measurements,” Invest. Ophthalmol. Visual Sci. 55(6), 3439–3446 (2014). 10.1167/iovs.14-13880 [DOI] [PubMed] [Google Scholar]
- 14.Garway-Heath D., et al. , “Measurement of optic disc size: equivalence of methods to correct for ocular magnification,” Br. J. Ophthalmol. 82(6), 643–649 (1998). 10.1136/bjo.82.6.643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carl Zeiss Meditec, Inc., Cirrus HD-OCT User Manual, Carl Zeiss Meditec, Inc., Dublin, California: (2012). [Google Scholar]
- 16.Loeffler M., et al. , “The LIFE-adult-study: objectives and design of a population-based cohort study with 10, 000 deeply phenotyped adults in Germany,” BMC Public Health 15, 691 (2015). 10.1186/s12889-015-1983-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heidelberg Engineering, Inc., Spectralis HRA+OCT User Guide Software Version 5.3, Heidelberg Engineering, Inc., Heidelberg, Germany: (2010). [Google Scholar]
- 18.R Core Team, “R: a language and environment for statistical computing. Vienna, Austria; 2014,” http://www.R-project.org (17 October 2016).
- 19.Benjamini Y., Hochberg Y., “Controlling the false discovery rate: a practical and powerful approach to multiple testing,” J. R. Stat. Soc. Ser. B (Methodol.) 57, 1, 289–300 (1995). [Google Scholar]
- 20.Wang Q., et al. , “Refractive status in the beaver dam eye study,” Invest. Ophthalmol. Visual Sci. 35(13), 4344–4347 (1994). [PubMed] [Google Scholar]
- 21.Katz J., Tielsch J. M., Sommer A., “Prevalence and risk factors for refractive errors in an adult inner city population,” Invest. Ophthalmol. Visual Sci. 38(2), 334–340 (1997). [PubMed] [Google Scholar]