Abstract
Background
Evidence of the association of coal mining with health outcomes such as increased mortality and morbidity in the general population has been provided by epidemiological studies in the last 25 years. Given the diverse sources of data included to investigate different health outcomes in the exposed populations, the International Classification of Diseases (ICD) can be used as a single classification standard to compare the findings of studies conducted in different socioeconomic and geographic contexts. The ICD classifies diagnoses of diseases and other disorders as codes organized by categories and chapters.
Objectives
Identify the ICD codes found in studies of morbidity and/or mortality in populations resident or in proximity of coal mining and assess the methods of these studies conducting a systematic review.
Methods
A systematic database search of PubMed, EMBASE and Scopus following the PRISMA protocol was conducted to assess epidemiological studies from 1990 to 2016. The health outcomes were mapped to ICD codes and classified by studies of morbidity and/or mortality, and the categories and chapters of the ICD.
Results
Twenty-eight epidemiological studies with ecological design from the USA, Europe and China were included. The exposed populations had increased risk of mortality and/or morbidity by 78 ICD diagnosis categories and 9 groups of ICD categories in 10 chapters of the ICD: Neoplasms, diseases of the circulatory, respiratory and genitourinary systems, metabolic diseases, diseases of the eye and the skin, perinatal conditions, congenital and chromosomal abnormalities, and external causes of morbidity. Exposed populations had non-increased risk of 9 ICD diagnosis categories of diseases of the genitourinary system, and prostate cancer.
Conclusions
There is consistent evidence of the association of coal mining with a wide spectrum of diseases in populations resident or in proximity of the mining activities. The methods of the studies included in this review can be integrated with individual-level and longitudinal studies to provide further evidence of the exposure pathways linked to increased risk in the exposed populations.
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5505-7) contains supplementary material, which is available to authorized users.
Keywords: Mortality, Morbidity, Coal mining, Systematic review, International classification of diseases, Environmental health, Ecological studies, General population
Background
The impacts of coalmining on human health have been of scientific concern since the sixteen century [1]. Epidemiological research has provided evidence of the association of coal mining with diseases such as silicosis [2, 3] and chronic obstructive pulmonary disease [4] in studies of workers since the 1930s [5]. Epidemiological research has identified increased prevalence of chronic respiratory diseases [6], cardiovascular disease [7] and cancer [8], as well as physio-pathological mechanisms of respiratory diseases in coal miners [9]. The cumulated evidence of occupationally related studies is the main body of evidence about the association of diseases with exposure to coal mining.
In the last three decades epidemiological studies have increasingly investigated the impacts of coal mining on the general populations in proximity to coal mining [10]. These studies have found reduced health-related quality of life [11], increased perceptions of detrimental health conditions [12], and higher frequency of medical consultations [13] in communities resident or in proximity of coal mining. Research about the state of health of exposed populations has been conducted using data from self-report health status and health surveys [14, 15] or health care costs [16]. Studies using data from hospital records of these populations have found higher rates of morbidity and mortality due to respiratory diseases [10] and cancer [17], and measures of biomarkers have evidenced greater exposures to environmental contaminants associated with the mining activities [18–20]. Other studies have identified increased rates of dental disorders in coal mining regions of the USA [21] and Europe [22], and studies in mining regions of developing countries reported higher prevalence of parasitic diseases in communities residing nearby coal mining [23, 24]. The diverse health outcomes included in these studies show that the health impacts of coal mining on general population have been assessed using different approaches and sources of data.
This diversity of data is a challenge for more accurately determining the health outcomes associated with coal mining in populations in proximity to coal mining. Whereas surveys are important tools to measure health status, the indicators measured might not be comparable between studies conducted in different geographic and socioeconomic contexts [25]. On the other hand the biological effect of the exposures cannot always be established; for instance increased levels of biomarkers can be measured in people without having any manifestation of disease [20]. However health outcomes that can be categorized according to a standard such as the International Classification of Diseases (ICD) are reliable given the underlying medical diagnosis process, consistent between different regional contexts. The ICD classifies diagnoses in categories, blocks of categories, and chapters according to the organ systems and clinical criteria [26]. Records with medical diagnoses such as death certificates and hospital admissions register health outcomes that can be categorized with the ICD.
This paper presents a systematic review of studies of morbidity and/or mortality in populations resident or in proximity of coal mining and the diagnoses identified according to the ICD. The objectives of the study were to conduct a systematic search of epidemiological studies; identify the health outcomes found in the selected studies as classified by the ICD, and assess the methods of these studies.
Methods
This review was done following the PRISMA protocol [27]. The protocol can be accessed at http://www.crd.york.ac.uk/PROSPERO/; (record: CRD42016052555). PRISMA checklist shown in Additional file 1.
Systematic searches of studies reported in PubMed, EMBASE and Scopus between January 1990 and October 2016 were conducted. Keyword combinations of “coal mining”, “coal”, “prevalence”, “incidence”, “mortality”, “morbidity”, “health impact”, “health outcome”, “international classification of diseases”, “hospitalization”, “hospital discharge”, “hospital separation”, “disease” and “death” were used. Search strategies shown in additional file (see Additional file 2).
Eligibility criteria
For inclusion studies had to: 1) be designed to search for association between coal mining and morbidity and/or mortality in populations in proximity to coal mining; 2) obtain data from hospital records, death certificates and/or clinical assessments with medical diagnosis, 3) be published in English. Studies whose subjects of study were exclusively miners or workers were excluded.
Paper selection and retrieval
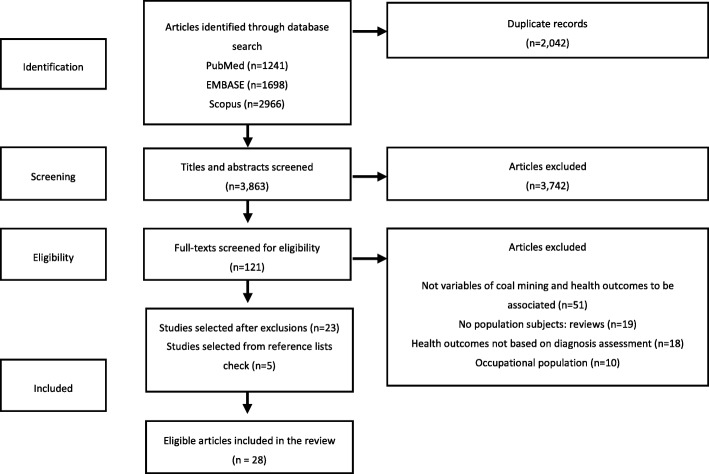
Records were first identified in the search strategy, titles and abstracts were screened, and full-text reports selected and reviewed to identify eligible studies. A check of the reference lists of the reports selected for full-text review was done to identify potentially eligible studies (Fig. 1).
Fig. 1.
Studies selection and retrieval flowchart
Data extraction and synthesis
A data form pre-piloted with 10 studies was used to extract data from eligible studies. The studies were organized in three classes: studies of mortality, morbidity and, both mortality and morbidity, according to the sources of data (i.e. death certificates, hospital records and general practitioner consultations) (Data extraction form shown in Additional file 3).
The results of each study were assessed to identify measures of the association of coal mining with mortality and/or morbidity (i.e. risk measures: relative risk, odds ratio, rate ratio and regression coefficient) in exposed versus non-exposed populations. Exposed populations were defined as residents of coal mining areas (e.g. counties with coal mining within their boundaries) or populations in proximity to coal mining (e.g. towns < 5 km to coal mining). The health outcomes were matched with ICD codes of diagnosis categories, block of categories, and/or chapters according to the ICD-10 2016 revision Clinical Modification (ICD-10-CM) defined by the National Centre of Health Statistics [28]. An ICD was listed to have “increased risk”/“non-increased risk” if there were one or more increased/no increased significant risk measures for that ICD in the exposed populations. Significance was establish as measures with p < 0.05 and confidence intervals not crossing the null value. Significant covariates were extracted and classified as sociodemographic, smoking, obesity/overweight, environmental, and other comorbidities. ICDs reported with the ICD-9 revision and health outcomes not reported as ICDs were classified by a medical doctor.
Critical appraisal of the studies was done using a modified scale of the checklist proposed by Dufault and Klar [29]. The assessment was based on 10 items with a maximum overall score of 12 points (Table 1). For each item, if a study did not meet the criteria the item was given a score of “0”, otherwise it received a score of “1”, or “2”. The grade of the studies were labelled: low (< 5 points); medium (5-8 points) and high relevance (> 8 points).
Table 1.
Assessment scale. Adapted from Dufault and Klar [29]
| Item | Description | |
|---|---|---|
| Study design and focus (max = 4) | Sample size (max = 2) | Number of ecologic units included in the analysis as a proportion of the total number of units (3 levels: < 11% = 0 points; 11-79% = 1 point; > 79% = 2 points) |
| Level of inference (max = 1) | The results of the analysis are not used to draw inferences for individuals | |
| Pre-specification of ecological units (max = 1) | Ecological units are selected to suit the hypothesis (as opposed to seemingly motivated by convenience or necessity such as the use of districts, towns or counties) | |
| Statistical methodology (max = 5) | Validity of statistical inferences (max = 2) | Number of ecological units per covariate (3 levels: 0-10 = 0 points; 10-20 = 1 point; > 20 = 2 points) |
| Use of covariates (max = 1) | Analysis adjusted for covariates (e.g. sociodemographic; environmental risk factors) | |
| Proper adjustment for covariates (max = 1) | Covariates are properly adjusted when regressed upon adjusted outcomes as recommended for ecological studies [30] | |
| Spatial effects (max = 1) | Inclusion of spatial analysis | |
| Quality of reporting (max = 3) | Statement of study design (max = 1) | Key elements of the study design are presented in the report |
| Justification of study design (max = 1) | Justification of the ecological analysis, the rationale and the objectives are presented in the report | |
| Discussion of cross-level bias and limitations (max = 1) | Readers are cautioned about the limitations of the ecological design and/or the ecological fallacy |
Two independent researchers (JC and PJ) carried out the literature search, articles selection process, data extraction and synthesis between October 2016 and February 2017. Discrepancies were discussed with a third researcher (SN) until consensus was reached.
Results
After exclusion of duplicates 3863 records were retrieved from the databases search. Initial titles and abstracts screening identified 121 potentially eligible studies. Independent full-text review reduced this number to 23. Five more studies were added from the reference lists for a final selection of 28 eligible studies (Fig. 1).
Characteristics of the eligible studies
The 28 selected studies were published between October 2000 and April 2016. Twenty two (79%) were conducted in the USA in the region of Appalachia with the exception of one study in Illinois [30]. Three studies (11%) from China investigated populations in Shanxi province. Two studies (7%) from the UK were conducted in North East England. One study (4%) from Spain covered all Spanish towns in proximity to mining activities (Table 2).
Table 2.
Characteristics of the studies selected in the review
| [citation] authors (year) | Country | Study class | Health outcomes scoped | Analytical method | Critical appraisal (relevance) | Funding |
|---|---|---|---|---|---|---|
| [47] Liao et al. (2016) | China | Mortality/ Morbidity | Neural tube defects | Spatial autocorrelation | Medium | NNSFC-YTF-IGSNRSa |
| [31] Woolley et al. (2015) | USA | Mortality | Malignant and non-malignant respiratory diseases, and external and all causes of death | Two sample t test | Medium | ARIES b |
| [49] Talbott et al. (2015) | USA | Morbidity | Diseases of the circulatory system | Linear regression, spatial regression | High | ARIES b |
| [30] Mueller et al. (2015) | USA | Mortality/ Morbidity | Cancer of lung, colon, breast, prostate, and all combined cancer | Linear regression, spatial autocorrelation | High | CTMPHD-EFCR c |
| [50] Lamm et al. (2015) | USA | Morbidity | Congenital anomalies | Poisson regression | Medium | ARIES b |
| [32] Buchanich et al. (2014) | USA | Mortality | Malignant neoplasms, and external and all causes of death | Negative binomial regression | Medium | ARIES b |
| [51] Brink et al. (2014) | USA | Morbidity | Diseases of the respiratory system | Linear regression | Medium | ARIES b |
| [52] Liu et al. (2013) | USA | Morbidity | Diabetes mellitus | Multilevel linear regression | Medium | JHERC-NIOSH d |
| [33] Fernandez-Navarro et al. (2012) | Spain | Mortality | Malignant neoplasms | Poisson regression, spatial regression | High | Spain Health Research Fund |
| [34] Borak et al. (2012) | USA | Mortality | All causes of death | Linear regression | Medium | National Mining Association |
| [35] Ahern and Hendryx (2012) | USA | Mortality | Malignant neoplasms | Linear regression | Medium | Not stated |
| [36] Esch and Hendryx (2011) | USA | Mortality | Chronic diseases of the circulatory system | Linear regression | High | Not stated |
| [53] Christian et al. (2011) | USA | Morbidity | Lung cancer | Spatial scan statistic | Medium | KLCRP e |
| [37] Hendryx (2011) | USA | Mortality | All causes of death | Linear regression | Medium | Not stated |
| [54] Ahern et al. (2011) | USA | Morbidity | Congenital anomalies | Poisson regression, spatial autocorrelation | High | Not stated |
| [55] Ahern, et al. (2011) | USA | Morbidity | Low birth weight | Linear regression | Medium | Not stated |
| [46] Liao et al. (2010) | China | Mortality/Morbidity | Neural tube defects | Poisson regression, spatial autocorrelation | High | PNNSFC -HTRDPC –NBRPP f |
| [38] Hitt and Hendryx (2010) | USA | Mortality | Cancer of the respiratory, digestive and genitourinary systems | Spatial autocorrelation | Medium | Not stated |
| [39] Hendryx et al. (2010) | USA | Mortality | Diseases of the respiratory and circulatory systems, all Malignant neoplasms, and all causes of death | Linear regression | Medium | Not stated |
| [40] Hendryx et al. (2010) | USA | Mortality | Cancer of the respiratory, digestive, genitourinary, hematopoietic, and central nervous systems, and melanoma | Linear regression, spatial autocorrelation | High | Not stated |
| [41] Hendryx and Ahern (2009) | USA | Mortality | All causes of death | Linear regression | Medium | Grant RRI-UWV g |
| [42] Hendryx (2009) | USA | Mortality | Diseases of the circulatory, respiratory, and genitourinary systems | Poisson regression | Medium | Grant RRI-UWV |
| [43] Hendryx et al. (2008) | USA | Mortality | Lung cancer | Linear regression | Medium | Grant RRI-UWV |
| [44] Hendryx (2008) | USA | Mortality | All causes of death | Linear regression | Medium | Not stated |
| [56] Hendryx et al. (2007) | USA | Morbidity | Lung cancer, diseases of the respiratory, circulatory, and musculoskeletal systems, diabetes, and mental disorders | Multilevel logistic regression | Medium | Not stated |
| [48] Gu et al. (2007) | China | Mortality/ Morbidity | Neural tube defects | Spatial autocorrelation | Medium | Grant h |
| [57] Howel et al. (2001) | UK | Morbidity | Diseases of the eyes and skin, and diseases of the respiratory system | Linear regression | Medium | Grant i |
| [58] Pless-Mulloli et al. (2000) | UK | Morbidity | Diseases of the eyes and skin, and diseases of the respiratory system | Linear regression | Medium | Grant j |
a National Natural Science Foundation of China and the Yong Talent Fund of the Institute of Geographic Sciences and the Natural Resources Search
b Industrial affiliate program at Virginia Tech; supported by members that include companies in the energy sector
c The Caryll Towsley Moy PhD Endowed Fund for Collaborative Research
d The Johns Hopkins Education and Research Centre, National Institute of Occupational Safety and Health
e Kentucky Lung Cancer Research Program
f The Project of the National Natural Science Foundation of China, the Hi-Tech Research and Development Program of China, the National Basic Research Priorities Program of the Ministry of Science and Technology of the People’s Republic of China, and the Knowledge Innovation Program
g Regional Research Institute, West Virginia University
h National project on Population and Health, China
i Medical Research Council (grant AIR/96/9) UK
j Northern and Yorkshire Regional research and development grant UK
Fourteen studies (50%) retrieved data from death certificates (studies of mortality), 10 (36%) from hospital records or general practitioner consultations (studies of morbidity), and 4 (14%) from both death certificates and hospital records (studies of mortality and morbidity).
Health outcomes and ICD codes
Thirteen (46%) of the eligible studies presented health outcomes already classified with the ICD-9 or ICD-10-CM revisions. Twenty three (82%) of the studies found significant risk measures for 88 ICD categories (single diagnosis), 9 blocks of ICD (groups of categories within the same chapter), 4 whole ICD chapters and 2 groups of combined chapters, in 10 out of 21 chapters of the ICD. These chapters include: neoplasms, diseases of the circulatory system, diseases of the respiratory system, diseases of the genitourinary system, endocrine and metabolic diseases, diseases of the eye and adnexa, diseases of the skin and subcutaneous tissue, conditions of the perinatal period, congenital malformations and chromosomal abnormalities, and external causes of morbidity. Five (18%) of the studies found non-significant risk measures (all increased) for ICD categories in the chapters: diseases of the circulatory system, congenital malformations and chromosomal abnormalities, and all combined chapters. Of all ICD categories, 31 were neoplasms, all malignant (i.e., cancer), affecting the following organ systems: integumentary, skeletal, endocrine, lymphatic and immune, respiratory, urinary, digestive, reproductive, and central nervous systems. Tables 3 and 4 show the list of ICD, organised by class of study and ICD chapter.
Table 3.
ICD-10-CM diagnosis categories, block of categories and chapters identified in studies of mortality and mortality/morbidity
| ICD | Increased risk y/n / NSa / Oa [citation] | Total exposed | Values |
|---|---|---|---|
| Chapter: Neoplasms | |||
| C00-C97 (All malignant neoplasms) | y [30, 32, 38–40] | Population in 214 USA counties | RR ranging 1.01-1.06 p < 0.05. Increased regression coefficients for residence and coal production c |
| C15 (Cancer of oesophagus) | y [35] | Population in 82 USA counties | r = 0.766(SE = 0.353) p < 0.05 SMR in coal mining counties |
| C16 (Cancer of stomach) | y [35] | Population in 82 USA counties | r = 0.935(SE = 0.482) p < 0.05 SMR in coal mining counties |
| C18, C19, C20, C21 (Cancer of: colon, recto-sigmoid, rectum, anus) | y [30, 33, 35] | Population in 157 USA counties and 48 Spanish towns | RR = 1.27(1.12-1.44) MR men-women and RR = 1.31(1.13-1.52) MR men in towns <5Km to coal mining. Increased regression coefficients for residence, coal production and type of coal mining county c |
| C22 (Cancer of liver and intrahepatic bile ducts) | y [33, 35] | Population in 82 USA counties and 48 Spanish towns | r = 0.788(SE = 0.395) p < 0.05 SMR in coal mining counties. RR = 1.69(1.09-2.63) MR men in towns <5Km to coal mining |
| C32 (Cancer of larynx) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.36/0.42 p < 0.002 SMR in coal mining counties |
| C33 (Cancer of trachea) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.36/0.42 p < 0.002 SMR in coal mining counties |
| C34 (Cancer of bronchus and lung) | y [30, 33, 35, 40, 43] | Population in 82 USA counties and 48 Spanish towns | RR = 1.22(1.01-1.49) MR men-women, RR = 1.29(1.05-1.59) MR men in towns <5Km to coal mining. Increased regression coefficients for residence, coal production, type of mining and type of coal mining county c |
| C30-C39 (Cancer of respiratory and intrathoracic organs) | y [38] / O [31] | Population in 29 USA counties | Pearson coefficient = 0.47 p < 0.01 SMR in counties with 1000Tons mined /Km2. O: increased rates in a graphical analysis and comparative t-test |
| C43 (Melanoma) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C53 (Cervical cancer) | y [35] | Population in 82 USA counties | r = 0.699(SE = .325) p < 0.05 SMR in coal mining counties |
| C61 (Prostate cancer) | n [30] | Population in 75 USA counties | r = −0.32 p ≤ 0.005 SMR by coal production and type of coal mining county |
| C67 (Cancer of bladder) | y [35] | Population in 82 USA counties | r = 1.33(SE = .438) p < 0.01 SMR in coal mining counties |
| C70 (Cancer of meninges) | y [40] | Population in 29 USA counties | r = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C71 (Brain cancer) | y [33, 40] | Population in 29 USA counties and 48 Spanish towns | RR = 1.75(1.19-2.57) MR men in towns <5Km to coal mining. Increased regression coefficients for residence and type of mining c |
| C72 (Cancer of spinal cord, cranial nerves and other parts of central nervous system) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C73 (Thyroid cancer) | y [33] | Population in 48 Spanish towns | RR = 2.05(1.01-4.13) MR men, RR = 1.70(1.02-2.84) MR women, in towns <5Km to coal mining |
| C81 (Hodgkin lymphoma) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C82, C83, C84, C85 (Follicular/non-follicular, mature T/NK-cell, and other specified/unspecified non-Hodgkin lymphomas | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C88 (Malignant immuno-proliferative diseases and other B-cell lymphomas) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C90 (Multiple myeloma and plasmacytoma) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C91, C92, C93, C94, C95 (Lymphoid, myeloid, monocytic, other specified leukemia, unspecified leukemia) | y [35, 40] | Population in 82 USA counties | r = 1.102(SE = .554) p < 0.05 SMR in coal mining counties. r/adjustedR2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| C96 (Unspecified cancer of lymphoid, hematopoietic and related tissue) | y [40] | Population in 29 USA counties | r/adjusted R2 = 0.441/0.16 p < 0.002 SMR in coal mining counties, r = 0.324/0.1 p < 0.02 SMR by coal production |
| Chapter: Diseases of the circulatory system | |||
| I00-I78 (All diseases of the circulatory system, except unclassified and unspecific) | y [39] / NS [39] | Population in 139 USA counties | r = 14.32(6.61) p < 0.03 SMR in high production coal mining counties. NS. 5.17 (5.97) p < 0.39 SMR in low production coal mining counties |
| I10 (Essential Hypertension) | y [36, 42] / n [42] b | Population in 129 USA counties | RR ranging 0.96-1.28 in coal mining counties c. r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| I11 (Hypertensive heart disease) | y [36, 42] / n [42] b | Population in 129 USA counties | RR ranging 0.96-1.28 in coal mining counties c. r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| I12 (Hypertensive chronic kidney disease) | y / n [42] b | Population in 129 USA counties | RR ranging 0.96-1.28 in coal mining counties c. |
| I13 (Hypertensive heart and chronic kidney disease) | y [36] | Population in 90 USA counties | r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| I21 (ST elevation and non-ST myocardial infarction) | y [36, 42] / n [42] b | Population in 129 USA counties | RR ranging 0.96-1.28 in coal mining counties c. r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| I24 (Other acute ischemic heart diseases) | y / n [42] b | Population in 129 USA counties | RR ranging 0.96-1.2) in coal mining counties c |
| I25 (Chronic ischemic heart disease) | y [36, 42] /n [42] b | Population in 129 USA counties | RR ranging 0.96-1.2) in coal mining counties c. r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| I31, I33, (Endocarditis, other diseases of pericardium) | y / n [42] b | Population in 129 USA counties | RR ranging 0.89-1.10 in coal mining counties c |
| I40 (Acute myocarditis) | y / n [42] b | Population in 129 USA counties | RR ranging 0.89-1.10 in coal mining counties c |
| I50 (Heart failure) | y [36, 42] /n [42] b | Population in 129 USA counties | RR ranging 0.89-1.10 in coal mining counties c. r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| I70 (Atherosclerosis) | y [36] | Population in 90 USA counties | r = 16.9(7.5) p < 0.03 SMR in coal mining counties, r = 11.4(5.5) p < 0.05 SMR by coal production |
| Chapter: Diseases of the respiratory system (J00-J99) | y [39] / O [31] | Population in 139 USA counties | r = 6.29(SE = 1.79) p < 0.001 SMR in coal mining counties, r = 9.81(SE = 2.32) p < 0.0001 SMR by type of coal mining county. O: increased rates in a graphical analysis and comparative t-test |
| J12, J13, J14, J15, J16, J17, J18 (Viral pneumonia, and pneumonia due to: streptococcus, Haemophilus influenzae, other bacteria, non-classified organism, unspecified organism) | y / n [42] b | Population in 129 USA counties | RR ranging 0.89-1.13 in coal mining counties c |
| J20, J21 (Acute bronchitis, bronchiolitis) | y / n [42] b | Population in 129 USA counties | RR ranging 0.89-1.13 in coal mining counties c |
| J22 (Unspecified acute lower respiratory infection) | y / n [42] b | Population in 129 USA counties | RR ranging 0.89-1.13 in coal mining counties c |
| J40, J41, J42 (Mucopurulent, simple, and not specified Bronchitis) | y / n [42] b | Population in 129 USA counties | RR = 1.07(1.04-1.10) males, RR = 1.11(1.07-1.15) females; in coal mining counties |
| J43, J44 (Emphysema, other chronic obstructive pulmonary disease) | y / n [42] b | Population in 129 USA counties | RR = 0.94(0.90-0.98) females in coal mining counties |
| J45 (Asthma) | y / n [42] b | Population in 129 USA counties | RR = 1.04(1.02-1.06) males in coal mining counties |
| Chapter: Diseases of the genitourinary system | |||
| N03, N04, N05 (Chronic/unspecified nephritic syndrome, nephrotic syndrome) | y [42] | Population in 129 USA counties | RR ranging 1.08-1.19 in coal mining counties c |
| N17, N18, N19 (Acute and unspecific kidney failure, chronic kidney disease) | y [42] | Population in 129 USA counties | RR ranging 1.08-1.19 in coal mining counties c |
| Chapter: External causes of morbidity (V00-V99) | y / n [32] b / O [31] | Population in 31 USA counties | RR ranging 0.91-1.12 in coal mining counties c. O: increased rates in a graphical analysis and comparative t-test |
| ICD categories in more than one ICD chapter | |||
| A00-Y89 (All combined internal and external causes) | y [32, 39, 41] / n [32] b / NS [34] / O [31] | Population in 139 USA counties | RR ranging 0.97-1.03 in coal mining counties c. Increased regression coefficients for residence and type of mining c. NS: r = 4.68(8.96) p < 0.6003 SMR in coal mining counties d. O: increased rates in a graphical analysis and comparative t-test |
| A00-R99 (All combined internal causes) | y [37, 44] | Population in 139 USA counties | Adjusted r ranging 21.5-63.0 SMR by residence and type of mining c |
| ICD categories in studies of mortality and morbidity | |||
| Chapter: Congenital malformations, deformations and chromosomal abnormalities | |||
| Q00, Q01, Q05, Q04.2 (Anencephaly, encephalocele, spina bifida, holoprosencephaly) | y [46] / O [47] / O-NS [48] | 204 geographical grid points in Heshun province (China). 46 villages in Zhongyang and Jiaokou Counties (China) | RR = 1.338(1.004-1.783) p < 0.05 cases to mothers resident in coal mining areas. O: increased rate cases in populations < 8 km to coal transport roads (p < 0.007), not measure provided. O-NS: higher mortality rate (281.2/10000) in villages closer to coal mining plants/control population: chi-square test (p < 0.364) |
Increased risk y/n: one or more risk measure increased/non-increased in exposed versus non-exposed populations. r regression coefficient, SE standard error, MR mortality rate, RR relative risk, SMR standardised mortality rate
a NS/O: Not significant/Other measure
b Disparities found in different exposed sub-groups
c All risk measures provided in additional material [see Additional file 4].
d These results were disputed, and the article subjected to erratum
Table 4.
ICD-10-CM diagnosis categories, block of categories and chapters identified in studies of morbidity
| ICD | Increased risk y/n / NSa [citation] | Total exposed | Values |
|---|---|---|---|
| Chapter: Neoplasms | |||
| C18-C21 (Colorectal cancer) | y [30] | Population in 75 USA counties | r = 0.37 p < 0.009 incidence rate in recently mined coal mining counties |
| C34 (Cancer of bronchus and lung) | y [30, 53] | Population in 75 USA counties | Adjusted r = 0.36 p < 0.001 incidence rate in coal mining counties. RR = 1.21 p < 0.01 and RR = 1.17 p < 0.01 in 2 clusters with coal mining counties |
| Chapter: Endocrine, nutritional and metabolic diseases | |||
| E10, E11, E13 (Diabetes mellitus type 1 and 2, other specified diabetes mellitus) | y [52] | Population in 225 USA minor civil divisions | r = 0.116(0.059) p < 0.05 blood sugar levels by coal mining area density, r = 0.124(0.056) p < 0.01 blood sugar levels by proximity to abandoned coalmines |
| Chapter: Diseases of the eye and adnexa | |||
| H57.9 (Unspecific disorder of eyes) | y / n [57, 58] b | 5 northern England communities (2000-20,000 persons) | Adjusted OR = 0.23(0.10-0.49) GP-consultations in 1 of 5 communities (1.4 km to coal mining). Adjusted OR = 1.43(1.20-1.70) GP-consultations in all other communities (0.8-1.3 Km to coal mining) |
| Chapter: Diseases of the circulatory system (I00-I99) | NS [49] | Population in 28 USA counties | Adjusted hospitalisation rates in coal mining counties by type and coal production = r ranging 0.01-0.05 (p > 0.05) |
| I10, I11, I12, I13, I15 (Primary HTA, hypertensive heart disease and chronic kidney disease, secondary hypertension) | y [56] | Population in 73 USA counties | OR = 1.003(1.001-1.005) hospitalisation rates in coal mining counties by coal production |
| Chapter: Diseases of the respiratory system (J00-J99) | y [51] | Population in 28 USA counties | r = 0.064(0.025) men-women, r = 0.064(0.022) p < 0.006 men, r = 0.063(0.029) p < 0.032 women; hospitalisation rates in coal mining counties, by coal production |
| J40, J41, J42, J43, J44, J47 (Specified/unspecified bronchitis, emphysema, chronic obstructive pulmonary disease, bronchiectasis) | y [56] | Population in 73 USA counties | OR = 1.003(1.001-1.006) hospitalisation rates in coal mining counties |
| J98.9 Unspecific respiratory disorders | y / n [57, 58] b | 5 northern England communities (2000-20,000 persons) | Adjusted OR = 0.23(0.10-0.49) GP-consultations in 1 of 5 communities (1.4 km to coal mining). Adjusted OR = 1.43(1.20-1.70) GP-consultations in all other communities (0.8-1.3 Km to coal mining) |
| Chapter: Diseases of the skin and subcutaneous tissue | |||
| L98.9 (Unspecific disorders of skin) | y / n [57, 58] b | 5 northern England communities (2000-20,000 persons) | Adjusted OR = 0.23(0.10-0.49) GP-consultations in 1 of 5 communities (1.4 km to coal mining). Adjusted OR = 1.43(1.20-1.70) GP-consultations in all other communities (0.8-1.3 Km to coal mining) |
| Chapter: Diseases of the genitourinary system | |||
| N00.3, N00.8, N00.9, N01.3, N02.2, N03, N04, N05, N08 (Acute nephritic syndromes, hematuria with diffuse membranous glomerulonephritis, chronic nephritic syndrome, nephrotic syndrome, unspecified nephritic syndrome and glomerular disorders classified elsewhere) | n [56] | Population in 73 USA counties | OR = 0.997(0.994-0.999) hospitalisation rates in coal mining counties |
| N17, N18, N19 (Acute and unspecific kidney failure, chronic kidney disease) | n [56] | Population in 73 USA counties | OR = 0.997(0.994-0.999) hospitalisation rates in coal mining counties |
| N25, N26.9, N27 (Unspecific contracted and small kidney, renal sclerosis) | n [56] | Population in 73 USA counties | OR = 0.997(0.994-0.999) hospitalisation rates in coal mining counties |
| Chapter: Certain conditions originating in the perinatal period | |||
| P07.0, P07.1 (Extremely and other low birth weight new-born) | y [55] | Mothers in 29 USA counties | OR = 1.16(1.08-1.25) p < 0.0002, OR = 1.14(1.04-1.25) p < 0.0033; cases in coal mining counties |
| Chapter: Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) | y [50, 54] / NS [50] | New-borns in 86 USA counties | Adjusted PRR ranging 1.10-1.63 new-born hospitalisations in coal mining counties (adjusted for socioeconomic variables). Crude PRR ranging 1.43-2.39 p < 0.001 new-born hospitalisations in coal mining counties. NS: Adjusted PRR ranging 1.01-1.08 p > 0.05 new-born hospitalisations in coal mining counties (adjusted by type and group of hospital) |
| Q00-07 (Congenital malformations of the nervous system) | y [54] | New-borns in 86 USA counties | Adjusted PRR = 1.36(1.11-1.67) new-born hospitalisations in coal mining counties |
| Q20-34 (Congenital malformations of the circulatory and respiratory systems) | y [54] | New-borns in 86 USA counties | Adjusted PRR = 1.93(1.73-2.15) new-born hospitalisations in coal mining counties |
| Q35-45 (Congenital malformations of the digestive system) | y [54] | New-borns in 86 USA counties | Adjusted PRR = 1.41(1.17-1.71) new-born hospitalisations in coal mining counties |
| Q50-64 (Congenital malformations of genitals and urinary system) | y [54] | New-borns in 86 USA counties | Adjusted PRR = 1.35(1.19-1.54) new-born hospitalisations in coal mining counties |
| Q65-79 (Congenital malformations and deformations of the musculoskeletal system) | y [54] | New-borns in 86 USA counties | Adjusted PRR = 1.30(1.20-1.41) new-born hospitalisations in coal mining counties |
| Q80-89 (Other congenital malformations) | y [54] | New-borns in 86 USA counties | Adjusted PRR = 1.13(1.04-1.23) new-born hospitalisations in coal mining counties |
Increased risk y/n: one or more risk measure increased/non-increased in exposed versus non-exposed populations. r regression coefficient, OR odds ratio, RR relative risk, PRR prevalence rate ratio
a NS: Not significant
b Disparities found in different exposed sub-groups
All risk measures provided in additional material [see Additional file 4]
Mortality
Significant risk measures of mortality were found in 12 studies of mortality [31–44] and one study of mortality and morbidity [30]. Increased risk of mortality in exposed populations was found for 7 grouped ICDs (blocks, chapters and groups of combined chapters) and 64 ICD categories in the following chapters: neoplasms, diseases of the circulatory system, diseases of the respiratory system, diseases of the genitourinary system, and external causes of morbidity. Non-increased risk of mortality in exposed populations was found for 2 grouped ICDs and 28 ICD categories in the chapters: neoplasms, diseases of the circulatory system, diseases of the respiratory system, diseases of the genitourinary system, and external causes of morbidity (Table 3).
One of the studies [34] found non-significant increased risk of mortality in exposed populations by all causes of disease although the article was subjected to erratum after the results were disputed [45]. Two of the studies [32, 42] found both increased and non-increased risk of mortality in exposed populations for ICD categories in 4 chapters of the ICD (diseases of the circulatory system, diseases of the respiratory system, diseases of the genitourinary system, external causes of disease), and one group of ICD chapters (all combined internal and external causes). These disparities were found in some but not all exposed population sub-groups included in the studies. One of the studies [31] did not calculate risk and rather identified increased mortality for ICDs in three chapters (neoplasms, diseases of the respiratory system, and external causes of morbidity) from a graphical analysis of rates in exposed /non-exposed populations.
Exposed populations were residents of USA counties with occurrence of coal mining (coal mining counties) in all mortality studies with exception of one study [33] that included populations in Spanish towns in proximity to coal mining.
Mortality and morbidity
Three studies of live and still births found increased and non-increased risk measures with different significance for association of residence and proximity to coal mining with congenital malformations and chromosomal abnormalities. Liao et al. [46] found increased risk in mothers resident in coal mining counties, and identified increased rates in populations in proximity to coal mining (measure not provided) [47]. Gu et al. [48] found higher (although non-significant difference) mortality rates in villages closer to coal mining plants compared to control populations (Table 3).
Morbidity
Significant risk measures of morbidity were found in 10 studies of morbidity [49–58] and one study of mortality and morbidity [30]. Increased risk of morbidity in exposed populations was found for 9 grouped ICDs (blocks and chapters) and 21 ICD categories in the following chapters: neoplasms, endocrine, nutritional and metabolic diseases, diseases of the eye and adnexa, diseases of the circulatory systems, diseases of the respiratory system, diseases of the skin and subcutaneous tissue, conditions of the perinatal period, and congenital malformations and chromosomal abnormalities. Non-increased risk of morbidity in exposed populations was found for 18 ICD categories in the chapters: diseases of the eye and adnexa, diseases of the respiratory and genitourinary systems, and diseases of the skin and subcutaneous tissue (Table 4).
One of the studies [49] found non-significant risk (increased) of morbidity by diseases of the circulatory system (whole chapter) in exposed populations. One study [50] found non-significant risk (increased) of congenital malformations in new-borns to mothers resident in coal mining counties after adjustment by groups and type of hospitals. Two of the studies [57, 58] found that children in proximity to coal mining have both increased and non-increased risk of ICD categories in three chapters of the ICD (diseases of the eye and adnexa; diseases of the skin and subcutaneous tissue, diseases of the circulatory system). These disparities were found in one out of five exposed sub-groups included in the two studies.
Exposed populations were residents of USA coal mining counties and USA minor civil divisions in all morbidity studies, with exception of two studies [57, 58] of communities in proximity to coal mining in northern England.
Covariates
All of the studies with the exception of two [31, 50] included covariates for adjustment in the statistical analysis. Sociodemographic variables included socioeconomic indicators, race/ethnicity, education level, and health-care access. Environmental variables included soil or land cover type, proximity to rivers and faults, elevation, exposure to pesticides, levels of heavy metals in soil, and indoor and outdoor pollution. Twenty five (89%) of the studies adjusted for sociodemographic variables, 13 (46%) for smoking, 6 (21%) for obesity and/or overweight, 5 (19%) for other comorbidities or family history of comorbidity, and 4 (14%) for environmental variables.
Studies design and methods
All studies followed an ecological design (i.e. one or more variables included, at the group level). Regression analyses were used in 23 (82%) of the studies. Six of the studies (21%) included both regression and spatial analyses. Four (14%) of the studies conducted only spatial analyses (Table 2).
The ecological units were assigned according to administrative divisions (e.g., counties or towns) and geographical points. All studies from the USA used county as the ecological unit with the exception of one study [52] that used minor civil divisions (i.e. administrative divisions of a county). Two studies in China [46, 47] used points in a grid designed for the study, the study in Spain [33] used towns, and one study in China [48] used buffer distance units.
Critical appraisal of the studies
The studies were assessed using a modified scale of a checklist designed for quality assessment of ecological studies [29]. None of the studies scored low relevant: seven (25%) of the studies scored high and 21 (75%) scored medium in the assessment scale. The scores for each item are presented in Table 5.
Table 5.
Critical appraisal of selected studies. Modified scale from Dufault and Klar [29]
| Author (year) | Study design and focus | Statistical methodology | Quality of reporting | Score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | Level of inference | Pre-specification of ecological units | Validity of statistical inferences | Use of covariates | Spatial effects | Proper adjustment for covariates | Statement of study design | Justification of study design | Discussion of cross-level bias and limitations | Points | |
| Liao et al. (2016) | 2 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 7 |
| Woolley et al. (2015) | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 5 |
| Talbott et al. (2015) | 2 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 1 | 9 |
| Mueller et al. (2015) | 2 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 1 | 1 | 10 |
| Lamm et al. (2015) | 2 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 5 |
| Buchanich et al. (2014) | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | 1 | 7 |
| Brink et al. (2014) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 7 |
| Liu et al. (2013) | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 0 | 1 | 0 | 8 |
| Fernandez-Navarro et al. (2012) | 2 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 1 | 9 |
| Ahern and Hendryx (2012) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 1 | 0 | 8 |
| Borak et al. (2012) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 6 |
| Ahern et al. (2011) | 2 | 1 | 0 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| Esch and Hendryx (2011) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 1 | 1 | 9 |
| Christian et al. (2011) | 2 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 1 | 0 | 8 |
| Hendryx (2011) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 7 |
| Ahern, MacKay and Hamilton (2011) | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 7 |
| Liao et al. (2010) | 2 | 1 | 1 | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 10 |
| Hendryx et al. (2010a) | 2 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 1 | 9 |
| Hendryx, Fedorko and Halverson (2010) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 7 |
| Hitt and Hendryx (2010) | 2 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 5 |
| Hendryx (2009) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 7 |
| Hendryx and Ahern (2009) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 6 |
| Hendryx (2008) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 7 |
| Hendryx et al. (2008) | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 6 |
| Hendryx et al. (2007) | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 1 | 0 | 1 | 9 |
| Gu et al. (2007) | 2 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 6 |
| Howel et al. (2001) | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 7 |
| Pless-Mulloli et al. (2000) | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 7 |
Discussion
The ICD diagnosis codes presented in this systematic review unify health outcomes found in diverse studies in a single standard classification. We mapped ICDs to reported health outcomes in studies of population in proximity or resident of coal mining areas. These populations have increased risk of a wide spectrum of diseases encompassing 78 ICD categories and 9 groups of ICDs, classified in 10 out of 21 chapters of the ICD-10-CM. The ICDs were reported by studies of mortality and/or morbidity designed to assess ecological exposures, namely ecological studies, in the USA, UK, Spain and China.
Scope of health outcomes and ICDs identified in the selected studies
The majority of the studies found increased risk of one or more ICD diagnosis categories in exposed versus non-exposed, especially for ICDs in the chapters neoplasms, diseases of the circulatory and respiratory systems, and congenital anomalies; that were reported in both mortality and morbidity studies. Two thirds of the studies found increased mortality by cancer in exposed populations and nearly 40% of all ICDs identified were ICD categories of cancer. Most of the mortality studies found higher risk of cancer of lung and colon, and all combined cancer, and two of the morbidity studies found increased risk of cancer of lung and colon. These results show a consistent association of coal mining with higher mortality and morbidity by cancer in populations near coal mining.
The association of coal mining with cancer has been documented in epidemiological studies of workers since the 1930s [5], and increased risk of cancer of lung and stomach has been evidenced in epidemiological studies of occupational exposed populations [5, 59, 60]. It should be noted that populations in studies of this review could include coalminers that were part of the chosen exposed communities. Given that most coalminers are men, almost all of the studies conducted statistical analyses adjusting by gender to segregate populations with and without occupational exposure. The results evidence an association of coal mining with cancer of lung and colon, adjusted by gender, in the exposed populations. Furthermore, the study of Fernandez-Navarro et al. found increased risk of colorectal and thyroid cancer in only women of populations in proximity to coal mining [33]. They also found that only men in these populations had increased risk of cancer of liver, brain and thyroid, a group of diagnoses for which there is scarce research from studies of workers. These findings suggest some association of coal mining with cancer of organs scarcely investigated in studies of both occupational and non-occupational exposed populations.
The other ICDs of cancer in this review include categories such as cancer of stomach, oesophagus, kidney, bladder, brain, leukaemia and cervical cancer. There is little research about these diseases in the general population, regarding their proximity to coal mining. Studies of coal miners have found increased risk of cancer of stomach, kidney and bladder [17]. Other studies in coal miners found increased risk of leukaemia [61] and cancer of brain [62] although the results were inconclusive and exposures could be related to electrical and magnetic fields rather than contact with sub products of the mining activities. For some ICD categories of cancer found in this review such as cancer of oesophagus, brain and meninges, thyroid, leukaemia and cervical cancer, we did not find evidence of their association with occupational exposures. The increased risk of these diverse types of cancer in the general population studied can indicate that cancer development follows different exposure pathways in communities resident, or in proximity of coal mining. Whereas in ecological studies other risk factors such as socioeconomic variables can account for effects at the group level of the analysis, all studies in this review conducted analyses adjusting for sociodemographic and other variables (with the exception of one study that adjusted only for type of hospitals [50]). The multiple ICDs of cancer identified in studies of this review reflect that cancer more than a disease in isolation is in fact many diseases -mostly chronic- of different organ systems. Since coal mining implies industrial activities prolonged for many years, eventually different exposure pathways can relate coal mining with biological insult on diverse organ systems that result in disease.
Exposure pathways need to be considered for the increased risk of congenital anomalies found in some of the studies. The five studies that included live or still births to mothers resident or in proximity of coal mining found increased risk of congenital anomalies, yet there was variation in the significance of the results. Two studies [46, 47] found increased risk of neural tube defects (NTD), i.e. congenital anomalies of the nervous system, and a third study found increased but non-significant, mortality by NTD in live and still births in populations close to coal mining [48]. These findings were consistent with a fourth study by Ahern et al. that found increased risk of hospitalisation by NTD and congenital anomalies in other four organ systems, as well as all combined congenital anomalies [54]. The fifth study (Lamm et al.) used the same sample of Ahern et al. (USA counties) and found non-significant (increased) risk of hospitalisation by all combined congenital anomalies, after adjustment by type and groups of hospitals [50]. The study of Lamm et al. however, did not adjust by socioeconomic variables. The combined evidence of these studies suggests that pregnant women resident or in proximity of coal mining have a higher risk of carrying pregnancies affected by congenital malformations or chromosomal abnormalities.
The possible exposure pathways related to congenital anomalies in populations in proximity to coal mining are not established although it is accepted that most congenital anomalies result from interaction between both genetic and environmental factors [63]. There is increasing evidence of the association of congenital anomalies with exposure to environmental risk factors. Increased risk of congenital anomalies was found in mothers with higher blood levels of environmental pollutants such as arsenic and cadmium in coal mining areas of China [64]. These results follow another study that reported higher blood concentrations of arsenic and cadmium from coal mining in pregnant women from the same region [65]. Increased rates of congenital malformations and adverse pregnancy outcomes have been associated with air pollution [66, 67] and there are established links between congenital anomalies and environmental tobacco smoke [68, 69]. Moreover, environmental exposures have been associated with low birth weight, a perinatal condition with physio-pathological mechanisms related to congenital anomalies [70, 71]. One of the morbidity studies in this review (Ahern et al.) found increased risk of low and extremely low birth weight in new-borns to mothers resident in coal mining counties [55]. The women included in the Ahern et al. study [55] were part of the same populations in the studies that found increased risk of congenital anomalies in the USA. This supports the plausibility of exposure pathways between coal mining and pathogenic effects on the foetus development and low birth weight.
Almost 40% of the mortality studies searched the association of coal mining with all combined causes of disease. Five of these studies found increased risk of mortality by all causes in people resident of USA open-cut coal mining counties and one more study identified increased rates of mortality in a comparative analysis [31]. Only one of the mortality studies found non-significant (increased) mortality by all combined causes in a re-analysis of data used in three other mortality studies in this review [34]. However the original authors disputed the methods and results, and the article was subjected to erratum [45]. All of these studies adjusted their analyses for socioeconomic variables and other covariates such as smoking and other co-morbidities. These findings consistently show that communities resident in USA coal mining counties bear a higher risk of general mortality compared to non-coal mining counties.
A smaller number of the studies found significant risk of diseases of the circulatory and respiratory systems in residents of coal mining areas. Esch and Hendryx found higher mortality by five ICDs of chronic cardiovascular diseases in exposed populations [36]. These findings were consistent with a study of Hendryx who found increased risk for the same ICD categories and other 16 ICD categories of diseases of the respiratory system [44]. This study however, also found non-increased risk of all of the ICD categories in different exposed subgroups of population. Whereas three studies of morbidity found increased risk of hospitalisations and medical consultations by respiratory diseases [56–58] the studies of Pless-Mulloli et al. [58] and Howel et al. [57] found non-increased rates of consultations in one out of five subgroups of exposed communities. From the results of these studies in the general population there is a significant association between coal mining and diseases of the circulatory and respiratory systems although there is not consistency in the studies’ findings to characterise the trend by these diseases in affected communities.
One of the studies [30] found non-increased risk of prostate cancer in exposed populations. Whereas no other study of this review included prostate cancer, these findings concur with results of studies in workers reviewed by Jenkins et al. [17]. We did not find published evidence to support biological plausibility of lower risk of prostate cancer in coal mining exposed populations. Nevertheless, a hypothetical protective effect of coal mining on prostate cancer has been explored previously in coalminers although the authors did not infer specific exposure pathways or hazards related to the lower risk [72]. On the other hand, Hendryx et al. found lower ORs of hospitalizations rates in residents of USA coal mining counties by 15 ICD categories of diseases of the genitourinary system [56]. In another study Hendryx found only increased mortality rates for some of these ICDs in similar populations [42], however these two studies differ in the sources of data (death certificates versus hospital records). These findings suggest a lower risk of diagnoses involving organs of the genitourinary system in residents of USA coal mining counties related with underlying mechanisms not yet investigated. Girschik et al. [72] conducted a systematic review of prostate cancer in studies of coal miners, measuring a combined effect size of 0.74 (95% CI 0.67 to 0.81), and suggested some occupational conditions as possible explanations. Nevertheless the proposed mechanisms do not extrapolate to the results in studies of this review, and their link with possible exposure pathways need to be investigated in further research.
Methodological design of the studies and control of bias
The selection criteria in this systematic review did not include a specific study design yet all of the studies selected followed an ecological design (one or more variables grouped as rates or percentages). This circumstance is telling of some of the complexities faced by authors when addressing research of health outcomes associated with environmental exposures (e.g. exposures related with coal mining), that are eminently ecological. In many cases, the choice of this kind of design is the only way to conduct the research given the limitations to access protected data. A third of the authors of studies in this review noted that they follow an ecological design given restrictions to access individual data. The use of an ecological design in all selected studies, besides being an indicator of consistency seems to be adequate to approach important characteristics of the exposure, for example; the large regionalisation of coal mining areas, the indiscriminate impacts on surrounding populations and the validity of spatial and spatiotemporal analyses. Notwithstanding ecological studies have several limitations, especially the risk of ecological bias (i.e. confounding effect introduced by grouping variables). The PRISMA statement requires an assessment of risk of bias for studies included in systematic reviews, preferably with the use of standardised scales [27]. We used a modified assessment scale that has been applied in other reviews of ecological studies [73], instead of adapting standard scales more generally used (e.g. Newcastle-Ottawa scale). We consider this as the best approach to assess ecological studies, which include methodological characteristics such as samples based on ecological units and spatial analyses along with other statistical tests that cannot be evaluated with other assessment scales.
In the critical appraisal, all of the studies scored medium or highly relevant though there was important variability between scores of the scale’s criteria. The most pertinent issue was related to the use and adjustment for covariates in regression analyses to control risk of ecological bias [74]. Only seven of the studies conducted a proper adjustment for covariates as suggested for ecological studies [75]. All other studies did not include covariates in the regression analyses or included covariates measured as percentages instead of adjusting by age (as done for dependent variables). Given that calculation of age-adjusted rates for covariates is not always possible because of lack, or restrictions of data sources, this is a common limitation of ecological studies. However there were consistent results between studies that did proper adjustment for covariates and 17 studies that did not, while including similar exposed/non-exposed populations (e.g. the study of Buchanic et al. [32] and the studies of Henryx et al. [39], Hit and Hendryx [38], and Woolley et al. [31]). Likewise these results concurred with two of the studies conducted in regions other than the Appalachia [30, 33] indicating minor distortion (if any) of the results. Another aspect of the critical appraisal was related to the “quality of reporting” criterion. Only half of the studies did include an explicit statement about the study design, and discussed the risk of ecological bias. This presupposes a greater responsibility for the reader to be aware of the studies’ design and draw conclusions from their results. We analysed results of each study regarding the populations sampled and considering consistency between results of different studies. Since ecological studies are most useful to provide exploratory analysis and generate hypothesis, rather than establishing causal links [76] the quality assessment of the studies did not affect majorly our synthesis and interpretation of results. None of the studies scored low relevant and there were consistent results in two or more studies, for risk characterisation of ICD categories in most of the ICD chapters, as discussed in the previous section.
The results of studies selected in this review can contribute to hypothesis testing in further research. A good example is in the results of the study of Liu et al. who found significant increased levels of blood sugar in diabetic residents of USA coal mining counties after adjustment for covariates [52]. Peer review literature about diseases of the endocrine system in populations in proximity to coal mining is scarce and these findings suggest an association needed to be studied in other coal mining regions. In another study, Hendryx found increased risk of mortality for, amid other diseases, acute bronchitis, bronchiolitis and emphysema in residents of coal mining counties [42]. To the best of our knowledge, this is the first epidemiological study to measure a significant association of coal mining with these ICD categories in exposed populations. Whereas these findings can be corroborated with longitudinal studies, they are also complementary for research in the environmental health field: Inclusion of large groups of diagnosis categories can allow identification of underlying associations that cannot be measured in studies of more specific groups of diseases. Most of the studies in this review were designed to measure risk of diseases already studied for their association with coal mining, in part because of supporting evidence provided by studies in coalminers. The inclusion in the analysis of groups of disease beyond diagnosis categories restricted to results of previous research can evidence increased risk of unexpected health outcomes and lead to further research about different exposure pathways.
Limitations
Our search criteria excluded studies for which ICD codes could not be assigned because the sources of health data were not validated on medical diagnoses. This restricted the inclusion of health conditions or disorders associated with coal mining detected in surveys and other non-medical assessments. We considered more relevant to focus on the validity of health outcomes and the use of a single classification standard. Studies of only coalminers were excluded. Since workers could be part of the population in proximity to coal mining, their exclusion could impact the ICDs to be identified. However studies of workers are usually designed to assess occupational exposures (e.g. vibration, use/not use of masks), and coalminers are mostly men, two characteristics that are not representative of the general population. We balanced the exclusion of studies of occupational exposed populations against the chance of selection bias of ICDs in populations in the vicinity of coal mining. All selected studies in the review followed an ecological design. The issues related to ecological studies treated in the discussion imply that the interpretation of results for individual studies must be contextualised with the populations sampled and the statistical analyses of each study. Given that the selected articles were published in English, we did not assess studies from other coal mining regions reported in other languages. Whereas there seems to be a significant regional concentration of studies, we could not identify ICDs associated with coal mining in regions other than the USA, Europe and China.
Conclusions
There is consistent evidence of the association of coal mining with a wide spectrum of diseases, especially cancer and congenital anomalies, in populations resident or in proximity of the mining activities. The studies that have investigated these associations were designed to measure exposures at the group level thus other research methods such as individual-level and longitudinal studies can be integrated to provide further evidence of the exposure pathways. Although coal mining is undertaken worldwide, the majority of the studies have been conducted in a few countries. More epidemiological studies of populations in coal mining areas are needed to expand the results of this review to most geographical regions.
Additional files
Checklist of items of the PRISMA protocol addressed. (DOCX 26 kb)
Search strategies carried on Pubmed, Embase and Scopus. (DOCX 17 kb)
Data extraction form, Items of data collected from the eligible studies. (DOCX 18 kb)
All measures of risk and covariates reported in the eligible studies. (DOCX 167 kb)
Acknowledgements
The authors want to thank Scott Macintyre for his valuable advice on the systematic search strategy and Dr. Ruby Michael for spirited discussions and relevant comments on the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this manuscript and its additional files.
Abbreviations
- ICD
International classification of diseases
- ICD-10-CM
International classification of diseases 10th edition, clinical modification
Authors’ contributions
JC and PJ carried out the literature search, articles selection, data extraction and synthesis. JC classified the health outcomes according to the ICD-10-CM and was the main contributor to writing the manuscript. SN collaborated in the synthesis and was the third researcher when JC and PJ did not reach consensus. PJ and PS were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable
Competing interests
The authors declare that they have no competing interests
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5505-7) contains supplementary material, which is available to authorized users.
Contributor Information
Javier Cortes-Ramirez, Phone: +61730697196, Email: j.cortesramirez@uq.edu.au.
Suchithra Naish, Email: s.naish@qut.edu.au.
Peter D Sly, Email: p.sly@uq.edu.au.
Paul Jagals, Email: p.jagals@uq.edu.au.
References
- 1.McDonald WC, DuBruck EE. Fifteenth-century studies: Boydell & Brewer, Incorporated; 2000.
- 2.Department of Health and Human Services Health effects of occupational exposure to respirable crystalline silica. Natl Inst Occup Saf Health. 2002;129:1–2. [Google Scholar]
- 3.Green FH, Althouse R, Weber KC. Prevalence of silicosis at death in underground coal miners. Am J Ind Med. 1989;16(6):605–615. doi: 10.1002/ajim.4700160601. [DOI] [PubMed] [Google Scholar]
- 4.Boschetto P, Quintavalle S, Miotto D, Lo Cascio N, Zeni E, Mapp CE. Chronic obstructive pulmonary disease (COPD) and occupational exposures. J Occup Med Toxicol. 2006;1:11. doi: 10.1186/1745-6673-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stocks P. On the death rates from Cancer of the stomach and respiratory diseases in 1949-53 among coal miners and other male residents in counties of England and Wales. Br J Cancer. 1962;16(4):592–598. doi: 10.1038/bjc.1962.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graber JM, Stayner LT, Cohen RA, Conroy LM, Attfield MD. Respiratory disease mortality among US coal miners; results after 37 years of follow-up. Occup Environ Med. 2014;71(1):30–39. doi: 10.1136/oemed-2013-101597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai Z, Wang X, Tan H, Huang Y, Lu C. Effect of underground work on cardiovascular system in coal miners. Zhong nan da xue xue bao Yi xue ban = J Cent S Univ Med Sci. 2015;40(10):1103–1108. doi: 10.11817/j.issn.1672-7347.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Espitia-Perez L, Sosa MQ, Salcedo-Arteaga S, Leon-Mejia G, Hoyos-Giraldo LS, Brango H, Kvitko K, da Silva J, Henriques JA. Polymorphisms in metabolism and repair genes affects DNA damage caused by open-cast coal mining exposure. Mutat Res Genet Toxicol Envi Mutagen. 2016;808:38–51. doi: 10.1016/j.mrgentox.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Gulumian M, Borm PJ, Vallyathan V, Castranova V, Donaldson K, Nelson G, Murray J. Mechanistically identified suitable biomarkers of exposure, effect, and susceptibility for silicosis and coal-worker’s pneumoconiosis: a comprehensive review. J Toxicol Environ Health B Crit Rev. 2006;9(5):357–395. doi: 10.1080/15287390500196537. [DOI] [PubMed] [Google Scholar]
- 10.Hendryx M. The public health impacts of surface coal mining. Extractive Ind Soc. 2015;2(4):820–826. doi: 10.1016/j.exis.2015.08.006. [DOI] [Google Scholar]
- 11.Zullig KJ, Hendryx M. A comparative analysis of health-related quality of life for residents of U.S. counties with and without coal mining. Public Health Rep. 2010;125(4):548–555. doi: 10.1177/003335491012500410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hendryx M. Personal and family health in rural areas of Kentucky with and without mountaintop coal mining. J Rural Health. 2013;29(SUPPL.1):s79–s88. doi: 10.1111/jrh.12016. [DOI] [PubMed] [Google Scholar]
- 13.Moffatt S, Pless-Mulloli T. “It wasn’t the plague we expected.” parents’ perceptions of the health and environmental impact of opencast coal mining. Soc Sci Med. 2003;57(3):437–451. doi: 10.1016/S0277-9536(02)00369-6. [DOI] [PubMed] [Google Scholar]
- 14.Meacham SL, Sukpraprut S, Goessl C, Stevens W, Meisha D. 2nd environmental considerations in energy production conference: 2015. 2015. Prevalence rates of adult obesity and environmental factors impacting health in coal producing and non-coal producing appalachian counties in Southwest Virginia; pp. 273–283. [Google Scholar]
- 15.Hota P, Behera B. Coal mining in Odisha: an analysis of impacts on agricultural production and human health. Extractive Ind Soc. 2015;2(4):683–693. doi: 10.1016/j.exis.2015.08.007. [DOI] [Google Scholar]
- 16.Máca V, Melichar J. The health costs of revised coal mining limits in northern bohemia. Energies. 2016;9(2):1–20. doi: 10.3390/en9020081. [DOI] [Google Scholar]
- 17.Jenkins WD, Christian WJ, Mueller G, Robbins KT. Population cancer risks associated with coal mining: a systematic review. PLoS One. 2013;8(8):e71312. doi: 10.1371/journal.pone.0071312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quiroz-Arcentales L, Hernandez-Florez LJ, Agudelo Calderon CA, Medina K, Robledo-Martinez R, Osorio-Garcia SD. PM10 exposure-related respiratory symptoms and disease in children living in and near five coal-mining areas in the Cesar department of Colombia. Rev Salud Publica (Bogota) 2013;15(1):66–79. [PubMed] [Google Scholar]
- 19.Shi GL, Lou LQ, Zhang S, Xia XW, Cai QS. Arsenic, copper, and zinc contamination in soil and wheat during coal mining, with assessment of health risks for the inhabitants of Huaibei, China. Environ Sci Pollut Res. 2013;20(12):8435–8445. doi: 10.1007/s11356-013-1842-3. [DOI] [PubMed] [Google Scholar]
- 20.Yapici G, Can G, Kiziler AR, Aydemir B, Timur IH, Kaypmaz A. Lead and cadmium exposure in children living around a coal-mining area in Yatagan, Turkey. Toxicol Ind Health. 2006;22(8):357–362. doi: 10.1177/0748233706071740. [DOI] [PubMed] [Google Scholar]
- 21.Hendryx M, Ducatman AM, Zullig KJ, Ahern MM, Crout R. Adult tooth loss for residents of US coal mining and Appalachian counties. Community Dent Oral Epidemiol. 2012;40(6):488–497. doi: 10.1111/j.1600-0528.2012.00691.x. [DOI] [PubMed] [Google Scholar]
- 22.Mielnik-Blaszczak M, Stachurski P, Tomankiewicz M. Occurrence of non-carious enamelopathies in the children living in the vicinity of the coal mine Bogdanka. Annales Universitatis Mariae Curie-Skłodowska Medicina. 2004;59(2):157–161. [PubMed] [Google Scholar]
- 23.Martinez-Tovar JG, Rebollar-Tellez EA, Fernandez Salas I. Seroprevalence of T. Cruzi infection in blood donors and Chagas cardiomyopathy in patients from the coal mining region of Coahuila, Mexico. Revista do Instituto de Medicina Tropical de Sao Paulo. 2014;56(2):169–174. doi: 10.1590/S0036-46652014000200014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Carli GA, Mentz M, Rott MB, Da Silva ACA, Wendorff A, Tasca T, Castilhos DS, De Carli G, Montenegro RA, Mylius L. Studies on prevalence of intestinal parasites infections in the urban and rural population of coal mine area in Arroio dos Ratos city, Rio Grande do Sul state. Revista Brasileira de Farmacia. 1997;78(4):83–85. [Google Scholar]
- 25.Terebessy A, Czeglédi E, Balla BC, Horváth F, Balázs P. Medical students’ health behaviour and self-reported mental health status by their country of origin: a cross-sectional study. BMC Psychiatry. 2016;16(1):171. doi: 10.1186/s12888-016-0884-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO. International classification of diseases Vol 2 instruction manual: WHO Library Cataloguing-in-Publication Data; 2016.
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC: International classification of diseases, tenth revision, clinical modification (ICD-10-CM). 2017, https://www.cdc.gov/nchs/icd/icd10cm.htm# FY 2017 release of ICD-10-CM (Accessed 22 Oct 2016).
- 29.Dufault B, Klar N. The quality of modern cross-sectional ecologic studies: a bibliometric review. Am J Epidemiol. 2011;174(10):1101–1107. doi: 10.1093/aje/kwr241. [DOI] [PubMed] [Google Scholar]
- 30.Mueller GS, Clayton AL, Zahnd WE, Hollenbeck KM, Barrow ME, Jenkins WD, Ruez DR., Jr Geospatial analysis of Cancer risk and residential proximity to coal mines in Illinois. Ecotoxicol Environ Saf. 2015;120:155–162. doi: 10.1016/j.ecoenv.2015.05.037. [DOI] [PubMed] [Google Scholar]
- 31.Woolley SM, Meacham SL, Balmert LC, Talbott EO, Buchanich JM. Comparison of mortality disparities in central Appalachian coal- and non-coal-mining counties. J Occup Environ Med. 2015;57(6):687–694. doi: 10.1097/JOM.0000000000000435. [DOI] [PubMed] [Google Scholar]
- 32.Buchanich JM, Balmert LC, Youk AO, Woolley SM, Talbott EO. General mortality patterns in appalachian coal-mining and non-coal-mining counties. J Occup Environ Med. 2014;56(11):1169–1178. doi: 10.1097/JOM.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 33.Fernandez-Navarro P, Garcia-Perez J, Ramis R, Boldo E, Lopez-Abente G. Proximity to mining industry and cancer mortality. Sci Total Environ. 2012;435-436:66–73. doi: 10.1016/j.scitotenv.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 34.Borak J, Salipante-Zaidel C, Slade MD, Fields CA. Mortality disparities in Appalachia: reassessment of major risk factors. J Occup Environ Med. 2012;54(2):146–156. doi: 10.1097/JOM.0b013e318246f395. [DOI] [PubMed] [Google Scholar]
- 35.Ahern M, Hendryx M. Cancer mortality rates in Appalachian mountaintop coal mining areas. J Environ Occup Sci. 2012;1(2):63–70. doi: 10.5455/jeos.20120702022809. [DOI] [Google Scholar]
- 36.Esch L, Hendryx M. Chronic cardiovascular disease mortality in mountaintop mining areas of central Appalachian states. J Rural Health. 2011;27(4):350–357. doi: 10.1111/j.1748-0361.2011.00361.x. [DOI] [PubMed] [Google Scholar]
- 37.Hendryx M. Poverty and mortality disparities in central Appalachia: mountaintop mining and environmental justice. J Health Disparities Res Pract. 2011;4(3):6. [Google Scholar]
- 38.Hitt NP, Hendryx M. Ecological integrity of streams related to human Cancer mortality rates. EcoHealth. 2010;7(1):91–104. doi: 10.1007/s10393-010-0297-y. [DOI] [PubMed] [Google Scholar]
- 39.Hendryx M, Fedorko E, Halverson J. Pollution sources and mortality rates across rural-urban areas in the United States. J Rural Health. 2010;26(4):383–391. doi: 10.1111/j.1748-0361.2010.00305.x. [DOI] [PubMed] [Google Scholar]
- 40.Hendryx M, Fedorko E, Anesetti-Rothermel A. A geographical information system-based analysis of cancer mortality and population exposure to coal mining activities in West Virginia, United States of America. Geospat Health. 2010;4(2):243–256. doi: 10.4081/gh.2010.204. [DOI] [PubMed] [Google Scholar]
- 41.Hendryx M, Ahern MM. Mortality in Appalachian coal mining regions: the value of statistical life lost. Public Health Rep. 2009;124(4):541–550. doi: 10.1177/003335490912400411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hendryx M. Mortality from heart, respiratory, and kidney disease in coal mining areas of Appalachia. Int Arch Occup Environ Health. 2009;82(2):243–249. doi: 10.1007/s00420-008-0328-y. [DOI] [PubMed] [Google Scholar]
- 43.Hendryx M, O'Donnell K, Horn K. Lung cancer mortality is elevated in coal-mining areas of Appalachia. Lung Cancer. 2008;62(1):1–7. doi: 10.1016/j.lungcan.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 44.Hendryx M. Mortality rates in Appalachian coal mining counties: 24 years behind the nation. Environ Justice. 2008;1(1):5–11. doi: 10.1089/env.2008.0500. [DOI] [Google Scholar]
- 45.Hendryx M, Ahern M. Reply to Borak et al “mortality disparities in Appalachia: reassessment of major risk factors”. J Occup Environ Med. 2012;54(7):768–769. doi: 10.1097/JOM.0b013e318254622f. [DOI] [PubMed] [Google Scholar]
- 46.Liao Y, Wang J, Wu J, Driskell L, Wang W, Zhang T, Xue G, Zheng X. Spatial analysis of neural tube defects in a rural coal mining area. Int J Environ Health Res. 2010;20(6):439–450. doi: 10.1080/09603123.2010.491854. [DOI] [PubMed] [Google Scholar]
- 47.Liao Y, Zhang Y, He L, Wang J, Liu X, Zhang N, Xu B. Temporal and spatial analysis of neural tube defects and detection of geographical factors in Shanxi Province, China. PLoS One. 2016;11(4):e0150332. doi: 10.1371/journal.pone.0150332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gu X, Lin L, Zheng X, Zhang T, Song X, Wang J, Li X, Li P, Chen G, Wu J. High prevalence of NTDs in Shanxi Province: a combined epidemiological approach. Birth Defects Res A Clin Mol Teratol. 2007;79(10):702–707. doi: 10.1002/bdra.20397. [DOI] [PubMed] [Google Scholar]
- 49.Talbott EO, Sharma RK, Buchanich J, Stacy SL. Is there an association of circulatory hospitalizations independent of mining employment in coal-mining and non-coal-mining counties in West Virginia? J Occup Environ Med. 2015;57(4):e30–e36. doi: 10.1097/JOM.0000000000000425. [DOI] [PubMed] [Google Scholar]
- 50.Lamm SH, Li J, Robbins SA, Dissen E, Chen R, Feinleib M. Are residents of mountain-top mining counties more likely to have infants with birth defects? The West Virginia experience. Birth Defects Res A Clin Mol Teratol. 2015;103(2):76–84. doi: 10.1002/bdra.23322. [DOI] [PubMed] [Google Scholar]
- 51.Brink LL, Talbott EO, Stacy S, Marshall LP, Sharma RK, Buchanich J. The association of respiratory hospitalization rates in WV counties, total, underground, and surface coal production and sociodemographic covariates. J Occup Environ Med. 2014;56(11):1179–1188. doi: 10.1097/JOM.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 52.Liu AY, Curriero FC, Glass TA, Stewart WF, Schwartz BS. The contextual influence of coal abandoned mine lands in communities and type 2 diabetes in Pennsylvania. Health Place. 2013;22:115–122. doi: 10.1016/j.healthplace.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 53.Christian WJ, Huang B, Rinehart J, Hopenhayn C. Exploring geographic variation in lung cancer incidence in Kentucky using a spatial scan statistic: elevated risk in the Appalachian coal-mining region. Public Health Rep. 2011;126(6):789–796. doi: 10.1177/003335491112600604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahern MM, Hendryx M, Conley J, Fedorko E, Ducatman A, Zullig KJ. The association between mountaintop mining and birth defects among live births in central Appalachia, 1996-2003. Environ Res. 2011;111(6):838–846. doi: 10.1016/j.envres.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 55.Ahern M, Mullett M, MacKay K, Hamilton C. Residence in coal-mining areas and low-birth-weight outcomes. Matern Child Health J. 2011;15(7):974–979. doi: 10.1007/s10995-009-0555-1. [DOI] [PubMed] [Google Scholar]
- 56.Hendryx M, Ahern MM, Nurkiewicz TR. Hospitalization patterns associated with Appalachian coal mining. J Toxicol Environ Health A. 2007;70(24):2064–2070. doi: 10.1080/15287390701601236. [DOI] [PubMed] [Google Scholar]
- 57.Howel D, Pless-Mulloli T, Darnell R. Consultations of children living near open-cast coal mines. Environ Health Perspect. 2001;109(6):567–571. doi: 10.1289/ehp.01109567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pless-Mulloli T, Howel D, King A, Stone I, Merefield J, Bessell J, Darnell R. Living near opencast coal mining sites and children’s respiratory health. Occup Environ Med. 2000;57(3):145–151. doi: 10.1136/oem.57.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Swaen GM, Meijers JM, Slangen JJ. Risk of gastric cancer in pneumoconiotic coal miners and the effect of respiratory impairment. Occup Environ Med. 1995;52(9):606–610. doi: 10.1136/oem.52.9.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Coggon D, Barker DJ, Cole RB. Stomach cancer and work in dusty industries. Br J Ind Med. 1990;47(5):298–301. doi: 10.1136/oem.47.5.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gilman PA, Ames RG, McCawley MA. Leukemia risk among U.S. white male coal miners. A case-control study. J Occup Med. 1985;27(9):669–671. [PubMed] [Google Scholar]
- 62.Brown AM, Christie D, Taylor R, Seccombe MA, Coates MS. The occurrence of cancer in a cohort of new South Wales coal miners. Aust N Z J Public Health. 1997;21(1):29–32. doi: 10.1111/j.1467-842X.1997.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 63.Greene NDE, Stanier P, Moore GE. The emerging role of epigenetic mechanisms in the etiology of neural tube defects. Epigenetics. 2011;6(7):875–883. doi: 10.4161/epi.6.7.16400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jin X, Tian X, Liu Z, Hu H, Li X, Deng Y, Li N, Zhu J. Maternal exposure to arsenic and cadmium and the risk of congenital heart defects in offspring. Reprod Toxicol. 2016;59:109–116. doi: 10.1016/j.reprotox.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 65.Jin L, Liu J, Ye B, Ren A. Concentrations of selected heavy metals in maternal blood and associated factors in rural areas in Shanxi Province, China. Environ Int. 2014;66:157–164. doi: 10.1016/j.envint.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 66.Jacobs M, Zhang G, Chen S, Mullins B, Bell M, Jin L, Guo Y, Huxley R, Pereira G. The association between ambient air pollution and selected adverse pregnancy outcomes in China: a systematic review. Sci Total Environ. 2017;579:1179–1192. doi: 10.1016/j.scitotenv.2016.11.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gianicolo EA, Mangia C, Cervino M, Bruni A, Andreassi MG, Latini G. Congenital anomalies among live births in a high environmental risk area--a case-control study in Brindisi (southern Italy) Environ Res. 2014;128:9–14. doi: 10.1016/j.envres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 68.Tang X, Hobbs CA, Cleves MA, Erickson SW, MacLeod SL, Malik S. Genetic variation affects congenital heart defect susceptibility in offspring exposed to maternal tobacco use. Birth Defects Res A Clin Mol Teratol. 2015;103(10):834–842. doi: 10.1002/bdra.23370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu X, Nie Z, Chen J, Guo X, Ou Y, Chen G, Mai J, Gong W, Wu Y, Gao X, et al. Does maternal environmental tobacco smoke interact with social-demographics and environmental factors on congenital heart defects? Environ Pollut. 2018;234:214–222. doi: 10.1016/j.envpol.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 70.Darrow LA, Klein M, Strickland MJ, Mulholland JA, Tolbert PE. Ambient air pollution and birth weight in full-term infants in Atlanta, 1994–2004. Environ Health Perspect. 2011;119(5):731–737. doi: 10.1289/ehp.1002785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adams-Chapman I, Hansen NI, Shankaran S, Bell EF, Boghossian NS, Murray JC, Laptook AR, Walsh MC, Carlo WA, Sanchez PJ, Van Meurs KP, Das A, Hale EC, Newman NS, Ball MB, Higgins RD, Stoll BJ. Ten-Year Review of Major Birth Defects in VLBW Infants. Pediatrics. 2013;132(1):49–61. doi: 10.1542/peds.2012-3111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Girschik J, Glass D, Ambrosini GL, Fritschi L. Could mining be protective against prostate cancer? A study and literature review. Occup Environ Med. 2010;67(6):365–374. doi: 10.1136/oem.2009.047092. [DOI] [PubMed] [Google Scholar]
- 73.Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, Oladapo OT, Souza JP, Tunçalp Ö, Vogel JP, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12:57. doi: 10.1186/s12978-015-0043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greenland S, Morgenstern H. Ecological Bias, confounding, and effect modification. Int J Epidemiol. 1989;18(1):269–274. doi: 10.1093/ije/18.1.269. [DOI] [PubMed] [Google Scholar]
- 75.Rosenbaum PR, Rubin DB. Difficulties with regression analyses of age-adjusted rates. Biometrics. 1984;40(2):437–443. doi: 10.2307/2531396. [DOI] [PubMed] [Google Scholar]
- 76.Hall AJ. Ecological studies and debate on rotavirus vaccine and intussusception. Lancet. 2001;358(9289):1197–1198. doi: 10.1016/S0140-6736(01)06337-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Checklist of items of the PRISMA protocol addressed. (DOCX 26 kb)
Search strategies carried on Pubmed, Embase and Scopus. (DOCX 17 kb)
Data extraction form, Items of data collected from the eligible studies. (DOCX 18 kb)
All measures of risk and covariates reported in the eligible studies. (DOCX 167 kb)
Data Availability Statement
All data generated or analysed during this study are included in this manuscript and its additional files.