Abstract
Factors influencing N-terminal pro-brain natriuretic peptide (NT-proBNP) level in heart failure patients with different cardiac functions were identified to explore the correlations with prognosis. Eighty heart failure patients with different cardiac functions treated in Yixing People's Hospital from January 2016 to June 2017 were selected, and divided into two groups (group with cardiac function in class II and below and group with cardiac function in class III and above), according to the cardiac function classification established by New York Heart Association (NYHA). Blood biochemical test and outcome analysis were conducted to measure serum NT-proBNP and matrix metalloproteinase-9 (MMP-9) levels in patients with different cardiac functions, and correlations between levels of NT-proBNP and MMP-9 and left ventricular ejection fraction (LVEF) level were analyzed in patients with different cardiac functions at the same time. In addition, risk factors for heart failure in patients with different cardiac functions were analyzed. Compared with the group with cardiac function in class III and above, the group with cardiac function in class II and below had significantly lower serum NT-proBNP and MMP-9 levels (p<0.05). For echocardiogram indexes, left ventricular end-diastolic diameter (LVEDD) and left ventricular end-systolic diameter (LVESD) in the group with cardiac function in class II and below were obviously lower than those in the group with cardiac function in class III and above (p<0.05), while LVEF was higher in group with cardiac function in class II and below than that in group with cardiac function in class III and above (p<0.05). NT-proBNP and MMP-9 levels were negatively correlated with LVEF level [r=−0.8517 and −0.8517, respectively, p<0.001 (<0.05)]. Cardiac function in class III and above, increased NT-proBNP, increased MMP-9 and decreased LVEF were relevant risk factors and independent risk factors for heart failure in patients with different cardiac functions. NT-proBNP and MMP-9 levels are negatively correlated with LVEF in patients regardless of the cardiac function class. Therefore, attention should be paid to patients who have cardiac function in class III and above, increased NT-proBNP and MMP-9 levels and decreased LVEF in clinical practices, so as to actively prevent and treat heart failure.
Keywords: cardiac function, heart failure, N-terminal pro-brain natriuretic peptide, influencing factors
Introduction
Most cardiovascular diseases develop to heart failure in their advanced stages, and thus lead to death. Although various clinical means currently used for the treatment of heart failure show certain clinical effects, the most common cause of death in patients in cardiovascular medicine department is still heart failure (1). At present, the most commonly used and the most effective method for clinical diagnosis of heart failure is echocardiogram combined with radionuclide imaging examination, but not all hospitals and patients have access to this diagnostic method (2). Especially in primary hospitals, most clinical diagnoses are performed based on clinical manifestations and physicians' experience, and error diagnoses and misdiagnoses cannot be avoided, so both false-positive and false-negative rates are high (3). Therefore, a diagnostic method with high positive rate and specificity is needed in clinical practices for early diagnosis and prognosis prediction of patients with heart failure (4).
Yu et al (5) reported that soluble growth stimulation expressed gene 2 (sST2), which was correlated with ischemic heart disease and heart failure, can be used to predict the prognosis of heart failure. However, this method is expensive and complex, so clinical popularization is difficult, especially for primary hospitals. N-terminal pro-brain natriuretic peptide (NT-proBNP) is a kind of B-type natriuretic peptide that is secreted and produced by the heart when heart failure occurs and ventricular and atrial pressure and volume loads were obviously increased (5). In the diagnosis of heart failure, NT-proBNP has advantages of being economic, simple and reproducible in clinical detections, and especially fits the need of a primary hospital (6). Matrix metalloproteinase-9 (MMP-9) is the most important cytokine that mediates myocardial remodeling and left ventricular dilatation, and plays important roles in the occurrence and development of heart failure (7). Yan et al (6) reported that MMP-9 could change the extracellular matrix of cardiomyocytes to promote the development of heart failure and provide important prognostic information for left ventricular remodeling in patients with heart failure. Vorovich et al (7) concluded that NT-proBNP was more clinically valuable than MMP-9 in diagnosing ventricular remodeling and predicting prognosis in patients with congestive heart failure. In this study, changes in MMP-9 and left ventricular ejection fraction (LVEF) in heart failure patients were analyzed, and NT-proBNP levels of heart failure patients with different cardiac function classifications were measured and values of risk factors of the occurrence of heart failure in evaluating the prognosis were analyzed.
Patients and methods
General data
A total of 80 heart failure patients with different cardiac functions who received treatment in Yixing People's Hospital from January 2016 to June 2017 were chosen. All patients met the diagnostic criteria for heart failure established by the Chinese Medical Association in 2015, and were divided into two groups (group with cardiac function in class II and below and group with cardiac function in class III and above) in accordance with the cardiac function classification of New York Heart Association (NYHA). NYHA I patients have cardiac disease but without the resulting limitations of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnoea or anginal pain. NYHA II patients have cardiac disease resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnoea or anginal pain. NYHA III patients have cardiac disease resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary physical activity causes fatigue, palpitation, dyspnoea or anginal pain. NYHA IV patients have cardiac disease resulting in inability to carry on any physical activity without discomfort. Symptoms of cardiac insufficiency or of the anginal syndrome may be present even at rest (8). If any physical activity is undertaken, discomfort is increased. Before enrollment, all patients signed the informed consent or this was done by their authorized person, and this study obtained approvals from the Ethics Committee of Yixing People's Hospital (Yixing, China). Group with cardiac function in class II and below included 23 males and 17 females, age ranged from 45 to 75 years, with a mean age of 65.3±2.3 years old, of which 18 patients were combined with diabetes mellitus, and 15 patients were combined with hypertension; the group with cardiac function in class III and above consisted of 22 males and 18 females, and age ranged from 45 to 75 years, with an average age of 65.4±2.4 years, of which 17 patients were combined with diabetes mellitus and 15 patients were combined with hypertension. There were no statistically significant differences in sex, age, ratios of patients with diabetes mellitus and hypertension, levels of NT-proBNP, MMP-9 and LVEF between the two groups (p>0.05).
Methods for study and investigation
Blood biochemical test and outcome analysis were conducted. Elbow venous blood was extracted from all patients in the morning for measurement of serum NT-proBNP and MMP-9 levels. Echocardiogram examination was carried out, and correlations between NT-proBNP and MMP-9 levels in patients with different cardiac functions with LVEF level were analyzed at the same time. In terms of the analysis of risk factors, univariate analysis was first performed to process general data, such as sex, age, cardiac function, MMP-9, NT-proBNP and LVEF levels, incidence of diabetes mellitus and hypertension; then, multivariate logistic regression analyses were applied to identify independent risk factors for heart failure in patients with different cardiac functions. All researchers were trained, and a total of 160 questionnaires were sent to all patients and their attending physicians. The contents of questionnaires filled in by patients and their physicians were synthesized, analyzed and summarized.
Assessment methods
Serum samples of all patients were derived from fasting elbow venous blood extracted from patients on the day of diagnosis. For detection of MMP-9 and NT-proBNP, ethylenediamine tetraacetic acid dipotassium anti-coagulant and Sysmex XS-500i automatic blood biochemical analyzer were used, and all samples were sent for detection within 30 min after collection. The detection was performed via bi-directional lateral flow immunosorbent assay with reagents provided by ReLIA Biotechnologies, Inc. (Shenzhen, China), and physicians with >5 years of working experience in clinical laboratory were in strict accordance with instructions. Normal reference range of NT-proBNP was from 0 to 300. Normal reference range of MMP-9 was from 1.15 to 4.53 µg/l. Color Doppler echocardiography was performed using Sonos 5500 color Doppler ultrasound system with a frequency of 2.5–3.0 MHz. Calibration was performed automatically before measurement. Left ventricular end-diastolic diameter (LVEDD), left ventricular end-systolic diameter (LVESD), LVEF (%) and data relating to cardiac ultrasound were continuously measured 3 times and averaged by the same physician who had >5 years of working experience in ultrasonic diagnosis.
Statistical analysis
Statistical treatment was performed via Statistical Product and Service Solutions (SPSS) 21.0. Measurement data were expressed as mean ± standard deviation (SD), and t-test was used for comparisons between the two groups, and χ2 test was used for intragroup comparisons. Univariate and multivariate logistic regression analyses were used to analyze relevant risk factors for heart failure in patients with different cardiac functions. Correlations between LVEF and NT-proBNP, and between LVEF and MMP-9, were analyzed using Spearman's rank method. P<0.05 indicates that the difference was statistically significant.
Results
Comparison of serum NT-proBNP and MMP-9 levels in patients with different cardiac functions
The levels of serum NT-proBNP and MMP-9 in the group with cardiac function in class II and below were significantly lower than those in the group with cardiac function in class III and above (p<0.05) (Table I).
Table I.
Comparison of serum NT-proBNP and MMP-9 levels in patients with different cardiac functions (x±s).
| Different cardiac functions | NT-proBNP (pg/ml) | MMP-9 (µg/l) |
|---|---|---|
| Cardiac function in class II and below | 156.8±25.1a | 2.02±0.06a |
| Cardiac function in class III and above | 458.9±56.3 | 4.11±0.12 |
| t | 30.996 | 98.524 |
| P-value | <0.001 | <0.001 |
P<0.05, compared with patients with heart function grade III and above. NT-proBNP, N-terminal pro-brain natriuretic peptide; MMP-9, matrix metalloproteinase-9.
Comparison of levels of detected data relating to echocardiogram between the two groups
Compared with the group with cardiac function in class III and above, group with cardiac function in class II and below had obviously lower LVEDD and LVESD (p<0.05), but higher LVEF (p<0.05) in echocardiogram indexes (Table II).
Table II.
Comparison of LVEDD, LVESD and LVEF in patients with different cardiac functions (x±s).
| Different cardiac functions | LVEDD (mm) | LVESD (mm) | LVEF (%) |
|---|---|---|---|
| Cardiac function in class II and below | 46.8±3.6a | 43.5±2.9a | 46.5±2.9a |
| Cardiac function in class III and above | 65.6±5.3 | 63.3±5.0 | 35.6±1.9 |
| t | 18.558 | 21.665 | 19.884 |
| P-value | <0.001 | <0.001 | <0.001 |
P<0.05, compared with patients with heart function grade III and above. LVEDD, left ventricular end-diastolic diameter; LVESD, left ventricular end-systolic diameter; LVEF, left ventricular ejection fraction.
Analysis of correlation between NT-proBNP and LVEF levels in patients with different cardiac functions
The analysis showed that there was a negative correlation between NT-proBNP and LVEF levels [r=−0.8517, p<0.001 (<0.05)] (Fig. 1).
Figure 1.
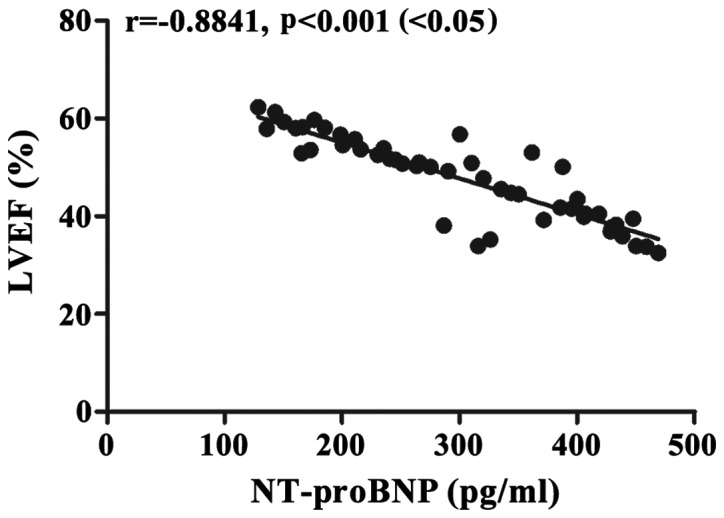
Correlation analysis between NT-proBNP and LVEF levels in patients with different degrees of cardiac function. The analysis suggests that NT-proBNP level is negatively related to LVEF level [r=−0.8517, p<0.001 (<0.05)]. NT-proBNP, N-terminal pro-brain natriuretic peptide; LVEF, left ventricular ejection fraction.
Analysis on correlation of MMP-9 level with LVEF level in patients with different cardiac functions
The analysis revealed that MMP-9 level had a negative relation with LVEF level [r=−0.8517, p<0.001 (<0.05)] (Fig. 2).
Figure 2.
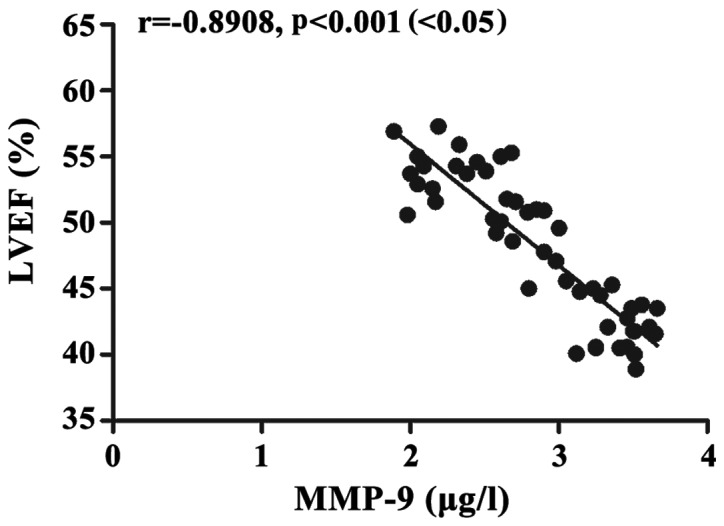
Correlation analysis between MMP-9 and LVEF levels in patients with different degrees of cardiac functions. The analysis indicates that there is a negative correlation between MMP-9 and LVEF levels [r=−0.8908, p<0.001 (<0.05)]. MMP-9, matrix metalloproteinase-9; LVEF, left ventricular ejection fraction.
Univariate analysis identified relevant factors for heart failure in patients with different cardiac functions
Univariate analysis showed that cardiac function in class III and above, increased NT-proBNP, upward MMP-9 and downward LVEF were relevant risk factors of the occurrence of heart failure in patients with different cardiac functions (Table III).
Table III.
Univariate analysis on relevant factors of the occurrence of heart failure in patients with different cardiac functions.
| Relevant factors | Case | Heart failure | t or χ2 | P-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 45 | 25 | 0.020 | 0.887 |
| Female | 35 | 20 | ||
| Age (years) | ||||
| >60 | 55 | 32 | 2.557 | 0.110 |
| ≤60 | 25 | 13 | ||
| Cardiac function | ||||
| Cardiac function | ||||
| in class II and below | 40 | 7 | 45.741 | <0.001 |
| Cardiac function | ||||
| in class III and above | 40 | 38 | ||
| MMP-9 (µg/l) | ||||
| Normal | 35 | 5 | 44.525 | <0.001 |
| Upward | 45 | 40 | ||
| NT-proBNP | ||||
| Normal | 20 | 1 | 27.280 | <0.001 |
| Upward | 60 | 45 | ||
| LVEF (%) | ||||
| Normal | 30 | 3 | 38.769 | <0.001 |
| Downward | 50 | 42 | ||
| Combined with diabetes | ||||
| Yes | 35 | 21 | 0.356 | 0.551 |
| No | 45 | 24 | ||
| Combined with hypertension | ||||
| Yes | 30 | 15 | 0.762 | 0.383 |
| No | 50 | 30 |
MMP-9, matrix metalloproteinase-9; NT-proBNP, N-terminal pro-brain natriuretic peptide; LVEF, left ventricular ejection fraction.
Multivariate logistic regression analysis of the occurrence of heart failure in patients with different cardiac functions
Multivariate logistic regression analysis showed that cardiac function in class III and above, increased NT-proBNP, increased MMP-9 and decreased LVEF were independent risk factors of the occurrence of heart failure in patients with different cardiac functions (Table IV).
Table IV.
Multivariate logistic regression analysis of patients with cardiac function in class III and above.
| Different cardiac functions | Wald test value | OR | Degree of freedom | SE | P-value |
|---|---|---|---|---|---|
| Cardiac function in class III and above | 5.288 | 0.949 | 0.937 | 2.014 | 0.011 |
| Increased NT-proBNP | 10.653 | 2.620 | 0.964 | 0.057 | 0.025 |
| Increased MMP-9 | 6.215 | 1.363 | 0.311 | 0.153 | 0.047 |
| Decreased LVEF | 6.625 | 1.669 | −0.512 | 0.199 | 0.010 |
OR, odds ratio; SE, standard error; NT-proBNP, N-terminal pro-brain natriuretic peptide; MMP-9, matrix metalloproteinase-9; LVEF, left ventricular ejection fraction.
Discussion
Heart failure is a clinical disease with increased pre- and post-loading volumes of the heart, stasis of blood flow, and insufficient supply of blood and oxygen to main organs because of the dysfunctions of systolic and diastolic capacities and reduced pumping capability of the heart (9). In recent years, with changes in people's lifestyle and diet structure, the occurrence and development of cardiovascular diseases show an increasing trend, and onset age is also becoming younger (10). In addition, there are increasing number of inducements of heart failure, so the morbidity of heart failure is getting higher and higher, seriously threatening the life and health of humans (11). Patients with early heart failure only have complaints such as fatigue, decreased exercise tolerance and increased heart rate, which can easily be ignored (12), but with the prolonged course of disease and the aggravation of disease, patients may show manifestations including dyspnea on exertion, orthopnea, lung rale and even pink frothy sputum, which can reduce cardiac function and increase difficulties in treatment (13). Therefore, how to realize rapid and effective early diagnosis of heart failure in clinical practices and evaluate the prognosis of patients at the same time is the focus and hotspot of current studies (14). Previous study has shown (5) that plasma NT-proBNP level, which is positively correlated with the severity of heart failure, can be used as a sensitive index in assessing changes of cardiac function.
In this study, patients with different cardiac functions were divided into a group with cardiac function of class II and below and a group with cardiac function of class III and above. Comparisons of serum NT-proBNP and MMP-9 levels between the two groups revealed that the group with cardiac function in class II and below had significantly lower serum NT-proBNP and MMP-9 levels than the group with cardiac function in class III and above, suggesting that NT-proBNP and MMP-9 levels are relatively low in patients with lower class of cardiac function. At the same time, the results of the echocardiogram were compared between the two groups, and showed that LVEDD and LVESD were obviously lower in the group with cardiac function in class II and below than those in group with cardiac function in class III and above. LVEF in the group with cardiac function in class II and below was higher than that in the group with cardiac function in class III and above, indicating that patients with cardiac function in class II and below have both lower LVEDD and LVESD, but higher LVEF than patients with cardiac function in class III and above. Furthermore, analyses on correlations of NT-proBNP and MMP-9 levels with LVEF level in patients with different cardiac functions showed that NT-proBNP and MMP-9 levels were negatively related to LVEF level, which was consistent with the finding of Yan et al (6), indicating that LVEF declined with increase in NT-proBNP and MMP-9 levels, and Vorovich et al (7) suggested that NT-proBNP is superior to MMP-9 in the diagnosis and prognosis of heart failure. Moreover, analyses of factors related to the occurrence of heart failure in patients with different cardiac functions suggested that class III and above cardiac function, increased NT-proBNP and MMP-9 levels and decreased LVEF level were the relevant and independent risk factors for heart failure.
NT-proBNP, mainly synthesized by cardiomyocytes, is a biological natural hormone with the highest expression in cardiac ventricles, and is secreted mainly in the case of passive ventricular dilatation and volume overload (15). With the longer half-time and expression time, and higher detection sensitivity than type-B natriuretic peptide in patients with heart failure, NT-proBNP is considered to be one of the specific markers of early cardiac dysfunction, and can be used for early diagnosis of heart failure in clinical practice (16). When patients suffer from heart failure caused by various degrees of decompensation, the level of NT-proBNP secreted into ventricular cells is increased distinctly (17). High class of cardiac function reflects poor cardiac function, and is the cause of increased ventricular end-diastolic pressure, left ventricular enlargement, decreased ejection fraction (18), and increased NT-proBNP level. Although many studies on the relationship between the level of NT-proBNP and the development of heart failure have been reported (19), most patients were diagnosed based on clinical manifestations or New York Heart Function scores, and objective data were not used, especially for the LVEF evaluated by color Doppler echocardiography. In this study, correlation between NT-proBNP levels and LVEF was analyzed. Combined with the New York Heart Function assessment, we found that NT-proBNP and MMP-9 levels were elevated and LVEF levels decreased in patients with grade III cardiac function or beyond. These patients have high-risk of heart failure and prognosis is poor. Attention should be paid to these patients during clinical treatment (20).
In conclusion, patients with cardiac function in class II and below have relatively lower NT-proBNP and MMP-9 levels; NT-proBNP and MMP-9 levels are negatively correlated with LVEF in patients with different degrees of cardiac function; attention should be paid to patients with cardiac function in class III and above, increased NT-proBNP and MMP-9 levels and decreased LVEF in clinical practice, so as to actively prevent and treat heart failure.
Acknowledgements
Not applicable.
Funding
This study was supported by the Scientific Research Project of Wuxi Health Bureau (MS201535).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
LX and YC conceived and designed the study. YJ collected the patient data. SY was responsible for the analysis and interpretation of the data. LX drafted and revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Yixing People's Hospital (Yixing, China). Signed informed consents were obtained from the patients or the guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Isah IA, Sadoh WE, Iduoriyekemwen NJ. Usefulness of amino terminal pro-B-type natriuretic peptide in evaluating children with cardiac failure. Cardiovasc Diagn Ther. 2017;7:380–388. doi: 10.21037/cdt.2017.05.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raedle-Hurst T, Mueller M, Meinitzer A, Maerz W, Dschietzig T. Homoarginine-A prognostic indicator in adolescents and adults with complex congenital heart disease? PLoS One. 2017;12:e0184333. doi: 10.1371/journal.pone.0184333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Darkner S, Goetze JP, Chen X, Henningsen K, Pehrson S, Svendsen JH. Natriuretic propeptides as markers of atrial fibrillation burden and recurrence (from the AMIO-CAT Trial) Am J Cardiol. 2017;120:1309–1315. doi: 10.1016/j.amjcard.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 4.Jiang R, Zhao QH, Wu WH, Zhang R, Yuan P, Gong SG, He J, Luo CJ, Qiu HL, Wang L, et al. Efficacy and safety of a calcium sensitizer, levosimendan, in patients with right heart failure due to pulmonary hypertension. Clin Respir J. 2018;12:1518–1525. doi: 10.1111/crj.12699. [DOI] [PubMed] [Google Scholar]
- 5.Yu J, Oh PC, Kim M, Moon J, Park YM, Lee K, Suh SY, Han SH, Byun K, Ahn T, et al. Improved early risk stratification of patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention using a combination of serum soluble ST2 and NT-proBNP. PLoS One. 2017;12:e0182829. doi: 10.1371/journal.pone.0182829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan AT, Yan RT, Spinale FG, Afzal R, Gunasinghe HR, Arnold M, Demers C, McKelvie RS, Liu PP. Plasma matrix metalloproteinase-9 level is correlated with left ventricular volumes and ejection fraction in patients with heart failure. J Card Fail. 2006;12:514–519. doi: 10.1016/j.cardfail.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Vorovich EE, Chuai S, Li M, Averna J, Marwin V, Wolfe D, Reilly MP, Cappola TP. Comparison of matrix metalloproteinase 9 and brain natriuretic peptide as clinical biomarkers in chronic heart failure. Am Heart J. 2008;155:992–997. doi: 10.1016/j.ahj.2008.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raphael C, Briscoe C, Davies J, Whinnett Ian Z, Manisty C, Sutton R, Mayet J, Francis DP. Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart. 2007;93:476–482. doi: 10.1136/hrt.2006.089656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang KW, Fox S, Mojaver S, Maisel AS. Using biomarkers to guide heart failure management. Expert Rev Cardiovasc Ther. 2017;15:729–741. doi: 10.1080/14779072.2017.1366312. [DOI] [PubMed] [Google Scholar]
- 10.Felker GM, Anstrom KJ, Adams KF, Ezekowitz JA, Fiuzat M, Houston-Miller N, Januzzi JL, Jr, Mark DB, Piña IL, Passmore G, et al. Effect of natriuretic peptide-guided therapy on hospitalization or cardiovascular mortality in high-risk patients with heart failure and reduced ejection fraction: A randomized clinical trial. JAMA. 2017;318:713–720. doi: 10.1001/jama.2017.10565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai Y, Yang J, Takagi A, Konishi H, Miyazaki T, Masuda H, Shimada K, Miyauchi K, Daida H. In-hospital and long-term outcomes of congestive heart failure: Predictive value of B-type and amino-terminal pro-B-type natriuretic peptides and their ratio. Exp Ther Med. 2017;14:1715–1721. doi: 10.3892/etm.2017.4686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clerico A, Zaninotto M, Passino C, Plebani M. New issues on measurement of B-type natriuretic peptides. Clin Chem Lab Med. 2017;56:32–39. doi: 10.1515/cclm-2017-0433. [DOI] [PubMed] [Google Scholar]
- 13.Mozzini C, Di Dio Perna M, Pesce G, Garbin U, Pasini Fratta AM, Ticinesi A, Nouvenne A, Meschi T, Casadei A, Soresi M, et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time. Intern Emerg Med. 2018;13:27–33. doi: 10.1007/s11739-017-1738-1. [DOI] [PubMed] [Google Scholar]
- 14.Kang CK, Pope M, Lang CC, Kalra PR. Iron deficiency in heart failure: Efficacy and safety of intravenous iron therapy. Cardiovasc Ther. 2017;35:59–62. doi: 10.1111/1755-5922.12301. [DOI] [PubMed] [Google Scholar]
- 15.Shou X, Lin J, Xie C, Wang Y, Sun C. Plasma IL-37 elevated in patients with chronic heart failure and predicted major adverse cardiac events: A 1-year follow-up study. Dis Markers. 2017;2017:9134079. doi: 10.1155/2017/9134079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iacoviello L, Bonaccio M, Di Castelnuovo A, Costanzo S, Rago L, De Curtis A, Assanelli D, Badilini F, Vaglio M, Persichillo M, et al. Moli-sani study Investigators: Frontal plane T-wave axis orientation predicts coronary events: Findings from the Moli-sani study. Atherosclerosis. 2017;264:51–57. doi: 10.1016/j.atherosclerosis.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Luedde M, Winkler T, Heinsen FA, Rühlemann MC, Spehlmann ME, Bajrovic A, Lieb W, Franke A, Ott SJ, Frey N. Heart failure is associated with depletion of core intestinal microbiota. ESC Heart Fail. 2017;4:282–290. doi: 10.1002/ehf2.12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toma M, Mak GJ, Chen V, Hollander Z, Shannon CP, Lam KKY, Ng RT, Tebbutt SJ, Wilson-McManus JE, Ignaszewski A, et al. Differentiating heart failure phenotypes using sex-specific transcriptomic and proteomic biomarker panels. ESC Heart Fail. 2017;4:301–311. doi: 10.1002/ehf2.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darche FF, Baumgärtner C, Biener M, Müller-Hennessen M, Vafaie M, Koch V, Stoyanov K, Rivinius R, Katus HA, Giannitsis E. Comparative accuracy of NT-proBNP and MR-proANP for the diagnosis of acute heart failure in dyspnoeic patients. ESC Heart Fail. 2017;4:232–240. doi: 10.1002/ehf2.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medvedeva EA, Berezin II, Shchukin YV. Galectin-3, markers of oxidative stress and renal dysfunction in patients with chronic heart failure. Kardiologiia. 2017;57:46–50. (In Russian) [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


