Summary
Prescribed physical activity/exercise training may reduce non-exercise physical activity resulting in no change in total daily energy expenditure and no or minimal exercise-induced weight loss. This systematic review evaluated cross-sectional, short-term (2–14 d), randomized and non-randomized trials which reported on the effect of prescribed physical activity/exercise on non-exercise physical activity/energy expenditure in healthy adults. PubMed and Embase were searched (from January 1990 to March 2013) for articles that presented data on the change in non-exercise physical activity/energy expenditure in response to prescribed physical activity/exercise training. Thirty-one articles were included in this review. One-hundred per cent of cross-sectional studies (n = 4), 90% of short-term studies (n = 10), 50% of non-randomized trials (n = 10) and 100% of randomized trials (n = 7) reported no reductions in non-exercise physical activity/energy expenditure in response to prescribed physical activity/exercise training. We found minimal evidence to support the hypothesis that prescribed physical activity/exercise training results in decreased non-exercise physical activity/energy expenditure in healthy adults. However, this literature is limited by the lack of adequately powered trials designed specifically to evaluate this hypothesis which have included assessments of both the energy expenditure of prescribed exercise and non-exercise energy expenditure using state-of-the-art techniques, i.e. indirect calorimetry and doubly labelled water, respectively.
Keywords: Compensation, energy expenditure, exercise, review
Introduction
Data from the 2009–2010 National Health Examination Survey suggest that 68.8% of those age ≥20 years are overweight (body mass index [BMI] ≥ 25 kg m−2), whereas 35.7% are obese (BMI ≥ 30 kg m−2) (1) with approximately 51% of US adults predicted to be obese by 2030 (2). Medical expenditures associated with the treatment of obesity and obesity-related conditions are estimated at greater than $147bn annually (2). Data from the National Health and Nutrition Survey (2003–2008) indicated that among adults (18–54 years), approximately 75% of women and 54% of men expressed a desire to lose weight, whereas 61% of women and 39% of men were actively pursuing weight control (3).
Exercise is recommended for weight management by several governmental agencies and professional organizations including the Association for the Study of Obesity (4), the Institute of Medicine (5), the US Federal guidelines on physical activity (6), Healthy People 2020 (7), the World Health Organization (4) and the American College of Sports Medicine (ACSM) (8). Compared with weight loss induced by energy restriction, weight loss achieved by exercise is composed predominantly of fat mass, whereas fat-free mass is preserved (9,10) and resting metabolic rate (RMR) is generally unchanged (11,12) or slightly increased (13,14), factors which may be associated with improved long-term weight loss maintenance. However, several reports have demonstrated that the accumulated energy balance induced by an exercise intervention alone is less negative than theoretically predicted for the imposed level of exercise-induced energy expenditure (15–17), most likely because of compensatory changes in energy intake, non-exercise energy expenditure or both (18–20). These compensatory changes reduce the magnitude of exercise-induced weight loss. Compensatory changes in energy intake and/or non-exercise energy expenditure are also suggested by studies reporting no additional weight loss with increased exercise dose (15,21,22).
As early as 1980, Epstein and Wing (23) suggested that a reduction of non-exercise energy expenditure might compensate for prescribed exercise training, thus resulting in no change in total daily energy expenditure and no or minimal exercise-induced weight loss. Although a number of studies have reported on the effect of exercise on non-exercise physical activity/energy expenditure, to date, there is no narrative or systematic reviews on this topic. Therefore, we conducted a systematic review to identify and evaluate studies that have employed a variety of designs, e.g. cross-sectional, short-term, non-randomized and randomized longitudinal trials, to assess the impact of exercise on non-exercise physical activity/energy expenditure. We also attempted to identify both exercise parameters including mode, frequency, intensity and duration, and participant characteristics including age, gender, body weight and activity level that may impact this association. Results of this review will clarify our understanding of the association between exercise and non-exercise physical activity/energy expenditure. This information will be useful for the design of weight management trials utilizing exercise and the potential identification of groups of participants for whom exercise may be most effective.
Methods
This systematic review was performed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (24,25).
Objectives
The objective of this systematic review was to address this question: does increased prescribed exercise alter non-exercise physical activity/energy expenditure in healthy adults?
Eligibility criteria
Primary source articles published in English language peer-reviewed journals that presented data on non-exercise physical activity/energy expenditure by level of occupational activity or prescribed exercise were eligible for inclusion in this systematic review. Specific eligibility criteria included types of studies: cross-sectional, short-term, and both non-randomized and randomized trials; types of participants: healthy adults (age 18 years and above); types of exercise interventions: aerobic, resistance, and combined aerobic and resistance training; types of outcome measures: no restrictions were placed on the assessment methods for the primary outcome (non-exercise physical activity/energy expenditure); other criteria: there were no restrictions on the length of interventions or the types of comparisons. We included cross-sectional comparisons between participants differing by level of prescribed exercise or occupational activity and longitudinal pre/post–within-group changes vs. non-exercise control or vs. a different level of prescribed exercise. Articles were excluded if they provided no data on non-exercise physical activity/energy expenditure by level of exercise, manipulated or controlled energy intake, were conducted in non-recreational athletes, individuals confined to whole-room calorimeters, or individuals with chronic disease.
Information sources
Studies were identified by searching electronic databases, related article reference lists and consulting with experts in the field. The search was applied to PubMed (1990 to present) and adapted for EMBASE (1990 to present). The last search was conducted on 15 March 2013. The search was developed as a collaborative effort of the research team in consultation with a Kansas University reference librarian and conducted by a co-author (SH). No attempts were made to contact study investigators or sponsors to acquire any information missing from the published article.
Search strategy
We used the following search terms for PubMed and Embase to identify potential articles with abstracts for review: ‘Physical activity’ [Title/Abstract] OR ‘Exercise’ [Title/Abstract] OR ‘training’ [Title/Abstract] OR ‘energy expenditure’ [Title/Abstract]) AND (off-exercise [Title/Abstract] OR nonexercise[Title/Abstract] OR non-exercise[Title/Abstract] OR activities of daily living [Title/Abstract] OR activity counts[Title/Abstract] OR spontaneous physical activity[Title/Abstract] OR spontaneous activity[Title/Abstract] OR compensation[Title/Abstract] OR compensatory[Title/Abstract]. Additional search terms were applied to eliminate case reports and studies involving participants with chronic disease, and to retrieve studies published in English and conducted in adults (age 18 years and above). Word truncation and the use of wildcards allowed for variations in spelling and word endings. The complete search strategy is presented in the Appendix.
Study selection
Retrieved abstracts were independently assessed for inclusion in the review by two investigators and coded as ‘yes’, ‘no’ or ‘maybe’. All investigators who participated in eligibility assessments were trained regarding study inclusion/exclusion criteria and completed practice eligibility assessments on 50 test abstracts prior to actual coding. Eligibility assessments on the practice abstracts were reviewed by the primary author (JED), and any coding problems were resolved. Disagreements regarding eligibility for inclusion were resolved via development of consensus among all co-authors. Full text articles for abstracts coded as ‘yes’ or ‘maybe’ were retrieved and reviewed independently by two co-authors prior to inclusion in the review. An Excel (Microsoft, Redmond, Washington, USA) spread sheet was developed and used to track eligibility status.
Data collection
Extracted data were entered into the University of Kansas secure REDCap (Research Electronic Data Capture, version 4.14.5) database (26). A REDCap data extraction form was developed, pilot tested on a sample of 10 studies (at least two studies of each of the four study designs included in this review) and revised accordingly. Relevant data were extracted from each manuscript by one author and verified by a second author. Disagreements were resolved by discussion. Data extracted from each article included basic study information (design, sample size, groups compared, exercise or physical activity groups/intervention[s]), participant characteristics (age, gender, BMI, minority status), energy and macronutrient assessment method, and results.
Risk of bias in individual studies
Risk of bias for randomized trials was independently evaluated by two authors using the Cochrane risk of bias tool (27). Risk of bias was assessed in the following domains: selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias. A third reviewer resolved and discrepancies in bias coding. Studies were not excluded on the basis of risk of bias.
Synthesis of results
Articles were grouped by study design: cross-sectional, short-term (2–14 d), non-randomized and randomized trials. There was a considerable heterogeneity across studies for several important parameters including (i) participant characteristics (age, gender, BMI, activity level); (ii) exercise prescriptions (mode, frequency, intensity, duration); (iii) comparison groups (interventions: pre- vs. post-exercise, exercise vs. non-exercise control, varying amounts of exercise); (iv) intervention length; (v) assessment of non-exercise physical activity/energy expenditure (accelerometer, heart rate, activity diary, doubly labelled water) and (vi) outcome variable (accelerometer counts, pedometer steps, energy expenditure, etc.). Given this heterogeneity, a meta-analysis was considered inappropriate. Results based on the extracted data were instead synthesized and presented grouped by study design.
Results
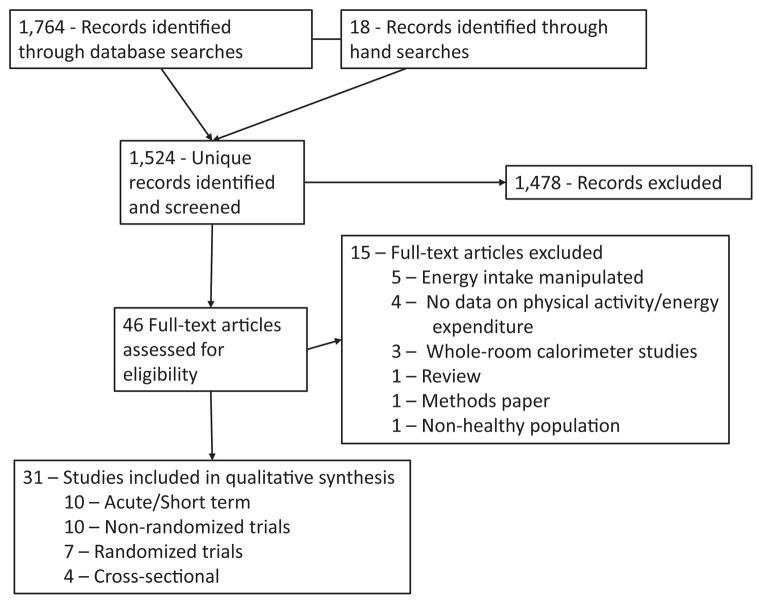
The initial database search plus hand searching identified 1524 unique records of which 1478 were excluded based on review of title and abstract. Full-text articles for the remaining 46 citations were reviewed. Fifteen articles did not satisfy the inclusion criteria and were excluded; thus, 31 articles were included in the review (Fig. 1).
Figure 1.
Flow diagram.
Cross-sectional studies
The four cross-sectional studies identified comprised ~13% of the total number of studies included in this review (Table 1).
Table 1.
Cross-sectional studies
| Study | Participants | Comparison | Activity assessment | Results |
|---|---|---|---|---|
| Parsons et al. (2009) (28) | 4531 men; 4594 women Age = 44–45 BMI = NR |
Occupational vs. leisure time PA | Self-report of work and leisure PA over the past 12 months Outcomes: MET-h week−1 |
Leisure PA MET-h week−1 increased with increased work MET-h week−1 in men but not in women |
| Tigbe et al. (2011) (30) | 56 walking postal workers 51 men; five women Age = 38 (9)* BMI = 26.2 (3) 56 postal office administrative staff. 46 men; 10 women Age = 40 (7) BMI = 27.4 (4) |
Compared 24-hr PA between groups with high (walking postal delivery workers) and low (postal administrative office workers) occupational PA | Uniaxial accelerometer over 7 consecutive days | Delivery staff were more active than administrative staff during work hours but not during non-work hours or on non-work days. Following active work days or on non-work days, delivery staff did not in engage in more sedentary activity than administrative staff |
| Withers et al. (1998) (31) | 12 women; long term exercisers Averaged 8.6 h week−1 or aerobic exercise for a mean of 22 years Age = 55.2 (7) BMI = 20.8 (2.3) 12 women; no long-term exercise Age = 57.5 (5.3) BMI = 22.7 (2.1) Six never exercised, six with no regular exercise for a mean of 16 years |
Long-term exercisers vs. non-exercising women | 7 d activity diary DWL in the eight most active and the eight least active participants. Non-exercise EE = TDEE – (RMR + TEF + EEEx) |
Diary data indicated long-term exercisers had significantly higher total daily EE compared with non-exercisers DLW data showed no difference in non-exercise EE between long-term exercisers and non-exercisers |
| Wolin et al. (2008) (29) NHANES 1999–2000 data |
2550 men Age = 43.2 (0.5) BMI = NR 29.6% minority 2898 women Age = 44.8 (0.5) BMI = NR 31.3% minority |
Compared leisure time moderate/vigorous PA by level of occupational PA | Survey: participants reported frequency and duration of moderate and vigorous PA over the past 30 d Outcome: h week−1 Occupational activity was self-reported as one of four levels |
Mean leisure time PA increased with increased occupational PA after control for gender, race, age, education and employment status in the total sample. However, in models stratified by gender, this effect was seen only in men. |
Mean (SD).
DLW, doubly labelled water; EE, energy expenditure; EEEx, exercise energy expenditure; NHANES, National Health and Nutrition Examination Survey; NR, not reported; PA, physical activity; SD, standard deviation; TDEE, total daily energy expenditure; TEF, thermic effect of food.
Cross-sectional studies: study characteristics
Sample size: median (range) sample size for cross-sectional studies was 2780 (24–9,125).
Comparisons: two studies compared usual leisure time physical activity by level of occupational activity (28,29). One study compared 24-h physical activity between groups with high or low levels of occupational activity (30), whereas one study compared 7-d physical activity levels between women who did or did not participate in recreational aerobic exercise (31).
Physical activity assessment: two studies employed physical activity self-reports (28,29), one used a portable accelerometer (30), and one study used an activity diary and also assessed energy expenditure in a subsample using doubly labelled water (31).
Cross-sectional studies: participant characteristics
Age: the median (range) age across the four studies was 44 (39–56) years.
Gender: three studies included both men and women (28–30), whereas one study included only women (31).
BMI: the mean BMI in the two studies that provided data on this parameter was 26.8 (30) and 21.8 kg m−2 (31).
Minority representation: minority representation in the one study that provided data on this parameter was ~31% (29).
Cross-sectional studies: results
Parsons et al. (28) and Wolin et al. (29) both reported increased occupational activity was associated with increased leisure time physical activity assessed by self-report in men but not in women. Tigbe et al. (30) found no difference in non-work hours or non-work day physical activity, assessed by accelerometer, between administrative postal staff (sedentary) and walking postal delivery workers. Withers et al (31) compared physical activity over 7 d in women who were habitual exercisers (averaged 8.6 h week−1 over 22 years) with sedentary women. Total daily energy expenditure assessed by an activity diary was significantly higher in exercisers compared with non-exercisers. However, no between-group differences in non-exercise energy expenditure were shown between a subsample of exercisers (n = 8 most active) and non-exercisers (n = 8 least active) when energy expenditure was assessed using doubly labelled water.
Short-term studies
The 10 short-term studies comprised ~32% of the total studies identified for this review (Table 2). The majority of these studies (six of 10) employed cross-over designs (32–37), which compared non-exercise physical activity/energy expenditure between conditions of prescribed vs. no prescribed exercise. Short-term studies have also compared physical activity between exercise and non-exercise days in participants in supervised exercise programmes (38–40) or before and after advice to increase daily walking activity (41).
Table 2.
Short-term studies
| Study | Participants | Length | Intervention | Activity assessment | Results |
|---|---|---|---|---|---|
| Alahmadi et al. (2011) (32) | 16 men Age = 26.5 (3.0) BMI = 30.0 (5.6) |
7 d | Cross-over with two conditions:
|
Tri-axial accelerometer worn 3 d before the exercise session, day of the exercise session; and 3 d following the exercise session | Exercise had no significant effect on non-exercise accelerometer output (counts min−1) on the day of the exercise session or over 2 d following the exercise session. There was a delayed increase in non-exercise accelerometer output 48 h post-completion of the high intensity exercise session |
| King et al. (1997) (37) | Eight men Age = 26 (5.2) BMI = 22.4 (1.8) |
2 d | Cross-over with two conditions over 2 consecutive days.
|
Activity diary recorded in 15-min intervals over 2 d | No effect of condition on activity profiles during the 2 h following either morning or afternoon exercise sessions. No significant effect of condition on evening activity profiles |
| Koulouri et al. (2006) (41) | Seven men; five women Age = 28.2 (NR) BMI = 22.5 (NR) |
3 weeks | 1 week habitual activity followed by 2 weeks with advice to increase walking by 2000 steps d−1 | 7 d uniaxial accelerometer, 7 d pedometer and an activity diary during habitual and increased walking | Per study design, there was a significant increase in steps day−1 in the walking vs. the habitual activity condition. Study condition had no significant effect on EE assessed by diary; however; there was a significant increase in EE assessed by accelerometer |
| Lynch et al. (2009) (38) | 19 men; one woman Age = 48 (10.5) BMI = 25.5 (2.9) |
8 d | Activity comparison between days when participating in a university faculty/staff basketball session vs. non-basketball days | Pedometer over 8 consecutive days | Mean steps day−1 were not significantly different between non-basketball week days, non-basketball week end days and basketball days (minus basketball steps) |
| McLaughlin et al. (2006) (33) | Eight men Age = 23 (1) BMI = 25.3 (5.3) Eight women Age = 24 (3) BMI = 21.9 (1.6) |
16 d | Cross-over with two conditions:
|
HR monitoring with individual HR/EE calibration with activity diaries Non-exercise EE = TDEE – Net EEEx |
No significant difference in non-exercise EE between exercise and control conditions |
| Stubbs et al. (2002) (35) | Six women Age = 23 (0.6) BMI = 21.4 (1.0) |
7 d | Cross-over with three conditions, each over 7 d
|
Daily HR monitoring with individual HR/EE calibration Non-exercise EE = TDEE – EEEx. |
TDEE increased significantly across control, moderate exercise and high exercise conditions. There was no significant difference in non-exercise EE between the three conditions |
| Stubbs et al (2002) (34) | Six men Age = 31 (5) BMI = 23.3 (2.4) |
7 d | Cross-over with three conditions, each over 7 d
|
Daily HR monitoring with individual HR/EE calibration Non-exercise EE = TDEE –EEEx. |
TDEE was significantly higher with high exercise vs. moderate exercise or control There was no significant difference in non-exercise EE between control, moderate or high exercise However, there was a significant decrease in non-exercise EE over the 7 d in both the moderate and high exercise conditions but not in controls |
| Tudor-Locke et al. (2002) (39) | Six men; 12 women Age = 69 (9.5) BMI = 25.6 (4.3) |
9 d | Participants were attending a supervised exercise programme that met Mondays, Wednesdays and Fridays at 8:15–9:30 AM. Included warm-up, aerobic activity (brisk walking) and RT | Pedometer over 9 d | Total average steps day−1 were significantly higher on exercise week days vs. non-exercise week days. No significant difference in steps outside the exercise programme between exercise and non-exercise days |
| Washburn & Ficker (1999) (40) | Three men; 15 women Age = 72.6 (4.6) BMI = 25.2 (4.6) |
3 d | Participants were attending a supervised exercise programme that met Mondays, Wednesdays and Fridays. 6–9 AM. Included warm-up, aerobic activity (walk, jog, aerobic dance) and RT | Uniaxial accelerometer worn on exercise and non-exercise days | No significant difference in accelerometer counts during the non-exercise class period (9 AM–12 midnight) between exercise class and non-exercise class days |
| Whybrow et al. (2008) (36) | Six men Age = 29.7 (5.9) BMI = 24.2 (2.2) Six women Age = 24.7 (5.9) BMI = 22.9 (1.6) |
14 d | Cross-over with three conditions:
|
DLW over 14 d | Non-exercise EE (TDEE – EEEx) was not significantly different between study conditions |
Mean (SD).
BMI, body mass index; DLW, doubly labelled water; EE, energy expenditure; EEEx, exercise energy expenditure; HR, heart rate; NR, not reported; RMR, resting metabolic rate; RT, resistance training; SD, standard deviation; TDEE, total daily energy expenditure.
Short-term studies: study characteristics
Sample size: the median (range) sample size across the 10 short-term studies was 14 (6–20) participants.
Trial duration: the median (range) trial duration was 7 (2–16) d.
Exercise intensity/duration: exercise intensity in the two studies that reported this parameter was 70% maximal heart rate (37) and 53% maximal oxygen consumption (33). Exercise duration ranged from 60 to 120 min session−1 in the five studies that prescribed exercise by time (32,34–37). Four studies dosed exercise by level of energy expenditure relative to body weight (34–36) or absolute energy expenditure (33). Prescriptions ranged from 21.4 (42) to 57.1 kJ kg−1 body weight (36) and 2092 kJ d−1 above RMR (33).
Physical activity/energy expenditure assessment: physical activity/energy expenditure was assessed using a variety of measures. These included portable accelerometers in three studies (32,40,41), heart rate monitoring with individual heart rate/energy expenditure calibration in thee studies (33–35), pedometers in two studies (38,39), activity diary in one study (37) and doubly labelled water in one study (36). Non-exercise physical activity was the outcome measure in six studies (32,37–41), whereas non-exercise energy expenditure was the outcome in four studies (33–36).
Assessment of exercise energy expenditure: six studies assessed the energy expenditure of the prescribed exercise. Four studies used heart rate with individual heart rate/energy expenditure calibration (33–35), one study used indirect calorimetry (37) and one study estimated exercise energy expenditure from treadmill speed and grade (32).
Short-term studies: participant characteristics
Age: the median (range) age across the 10 studies was 29 (23–73) years.
Gender: six studies included both men and women (33,36,38–41), three included men only (32,34,37) and one study included only women (35).
BMI: the median (range) BMI across the 10 studies was 23.6 (21.4–30.0) kg/m2. Four of 10 studies included overweight participants, (33,38–40) whereas only one study included obese participants (32).
Minority status: one study described the minority representation in the study sample (100% white) (33). No study reported non-exercise physical activity/energy expenditure by race or ethnicity.
Participant activity level: participants recruited for the majority of short-term studies (Six of 10, 60%) were physically active (33,37–41). Two studies recruited sedentary or moderately active participants, (32,36) whereas two studies did not describe participant baseline physical activity (34,35).
Short-term studies: results
Non-Exercise physical activity/energy expenditure: nine of 10 short-term studies (90%) reported no significant effect of prescribed exercise on non-exercise physical activity (37–41) or non-exercise energy expenditure (33–36). Alahmadi et al. (32) reported a significant increase in non-exercise physical activity 48 h after completing 60 min of high intensity interval treadmill walking (5 min at 6 km h−1, 10% grade, 5 min at 6 km h−1, 0% grade) in a sample of overweight and obese, sedentary, young adult men.
Effect of study parameters on non-exercise physical activity/energy expenditure
Exercise mode: no study provided a direct comparison on the effect of exercise mode on non-exercise physical activity/energy expenditure. A variety of exercise modes was investigated including treadmill (32,37) or outdoor (41) walking/running, cycle ergometer (33–36), adult fitness classes (39,40) and recreational basketball (38).
Exercise intensity: no short-term study evaluated the impact of exercise intensity on non-exercise physical activity/energy expenditure.
Exercise duration: no significant difference in non-exercise physical activity/energy expenditure was observed in the three studies that included more than one duration of prescribed exercise (34–36).
Exercise time of day: King et al. (37) reported no difference in physical activity 2 h after completing a 50 min exercise session at 70% maximal heart rate either in the morning or afternoon. Tudor-Locke et al. (39) and Washburn & Ficker (40) both reported no difference in non-exercise physical activity on days when participants completed morning exercise compared with non-exercise days.
Effect of participant characteristics on non-exercise physical activity/energy expenditure
Age: no study evaluated the effect of age on non-exercise physical activity/energy expenditure. The median age in the nine of 10 short-term trials reporting no change in non-exercise physical activity/energy expenditure was 29 years (33–41).
Gender: although six studies included both men and women, (33,36,38–41) no study reported on gender differences in non-exercise physical activity/energy expenditure. Results from two separate studies using identical exercise protocols and assessments of non-exercise energy expenditure in samples of men (34) and women (35) found a significant decrease in non-exercise energy expenditure over 7 d in men but not in women.
BMI: no study provided data on the effect of BMI on non-exercise physical activity/energy expenditure. Fifty percent of short-term trials were conducted in normal weight individuals (i.e. BMI < 25 kg m−2).
Baseline activity level: no study provided data on the effect of baseline level of physical activity on non-exercise physical activity/energy expenditure. The majority of short-term studies was conducted in active individuals.
Non-randomized trials
The 10 non-randomized trials comprised ~32% of the total studies identified for this review (Table 3). Most trials (seven of 10) evaluated changes in non-exercise physical activity/energy expenditure in a single group (no control) assigned to complete a longitudinal aerobic (19,43–47) or a resistance training protocol (48). Two trials compared changes in non-exercise physical activity/energy expenditure between participants in a combined aerobic plus resistance training protocol with non-randomly assigned controls, (49,50) whereas one trial compared differences in non-exercise physical activity/energy expenditure between women who participated in an 8-week exercise programme at a commercial exercise facility with a group of non-exercise volunteer controls (51).
Table 3.
Non-randomized trials
| Study | Participants | Length | Intervention | PA assessment | Results |
|---|---|---|---|---|---|
| Colley et al. (2010) (43) | 13 women Age = 41.1 (12.1)* BMI = 33.9 (4.5) |
8 weeks | Moderate intensity walking with target = 1500 kcal week−1 4 weeks supervised, 4 weeks unsupervised. | 14 consecutive days. Tri-axial accelerometer at baseline and during weeks 3–4 DLW – baseline and during weeks. 3–4 on seven participants Non-exercise EE = TDEE-(RMR + TEF + EEEx) |
Accelerometer: No change in the time spend in sedentary, light or moderate activity from baseline to week 4 DLW: Non-exercise EE deceased significantly from baseline to week 4. Six of the seven participants with DLW assessments decreased non-exercise EE over the 4-week period. Participants who were less fit at baseline had greater decreases in non-exercise EE |
| Di Blasio et al. (2012) (44) | 34 women Age = 55.9 (3.6) BMI = 26.9 (4.2) |
13 weeks | Group walks 4 d week−1. Month 1: 40 min at RPE 11 on 15-point scale Month 2: 50 min at RPE 11 Month 3. 50 min at RPE 13 |
SenseWear Pro2 armband at baseline and end. 3 consecutive days including 2 weeks and 1 weekend day including both training and non-training days. | No significant change in TDEE or non-exercise EE in the complete sample. However, 19 of 34 participants (56%) showed significant increases in TDEE and non-exercise EE, whereas 15 of 34 participants (44%) showed significant decreases in TDEE and non-exercise EE |
| Goran & Poehlman (1992) (45) | Five women Age = 63 (5) BMI = 23.9 (NR) Six men Age = 68(7) BMI = 24 (NR) |
8 weeks | Cycle ergometer 3 d week−1. Progressed from net EE of 150 kcal session−1, 60% VO2 max at week 1 to a goal of 300 kcal session−1, 85% VO2 max | DLW baseline and end Non-exercise EE = TDEE – (RMR + TEF + EEEx) |
Non-exercise EE was significantly reduced baseline to end |
| Hunter et al. (2000) (48) | Eight men Seven women Age = 66.8 (3.7) BMI = 24.8(3.9) |
26 weeks | Supervised RT, 3 d week−1, two sets, 10 reps, 65–80% 1-rep max, 10 exercises | DLW baseline and last 2 weeks of RT AEE was estimated by subtracting RMR from TDEE after reducing TDEE by 10% to account for the thermic response to meals Free-living physical activity (min d−1) was derived from AEE (kJ d−1) by using the ARTE index | Both TDEE and TDEE minus the average daily EE of RT was significantly increased baseline to end Mean change in AEE was large (>500 kJ) but non-significant ARTE was increased significantly baseline to end |
| Keytel et al. (2001) (51) | Control: 10 women Age = 55(5) BMI = NR Exercise: nine women Age = 58 (7) BMI = NR |
8 weeks | Control: no exercise Exercise: Walking, 3 d week−1, 70–75% HR max. |
24-hr TDEE estimated from HR monitoring with individual HR/EE calibration at baseline and end | No significant differences in TDEE either between exercise and control, or before or after exercise training. No significant differences in TDEE on exercise vs. non-exercise days |
| Manthou et al. (2010) (19) | 34 women Age = 31.7(8.1) BMI = 29.3 (4.3) |
8 weeks | 150 min week−1 supervised cycle ergometer exercise at 72–77% age-predicted max HR in one of two patterns:
|
TDEE estimated from 7 d HR monitoring with individual HR/EE calibration in conjunction with 7-d activity diaries at baseline and end. Non-exercise EE = TDEE – EEEx. |
TDEE increased significantly from baseline to end. Non-exercise EE increased significantly in responders (n = 11; fat loss ≥ predicted) and decreased significantly in non-responders (n = 23; achieved less than predicted fat loss) |
| Meijer et al. (1991) (46) | 16 men Age = 37.1 (3) BMI = 22.7 (1.7) 16 women Age = 35.3 (3.9) BMI = 23.3 (2.0) |
5 months | Running 3–4 d week−1 (1 d supervised) for a total distance of 15–25 km week−1 after 8 weeks and 25–40 km week−1 after 20 weeks | 7 d accelerometer at baseline, 8 and 20 weeks DLW: random sub-sample of four men and four women at baseline and 20 weeks. |
Accelerometer: No effect of exercise training on non-exercise accelerometer output DLW: TDEE minus sleep EE increased in both men and women which was only partially because of the net EE of running. Suggest that non-exercise EE increased by 55% and 28% in men and women, respectively |
| Meijer et al. (1999) (49) | Control four women; three men Age = 57.4 (2.6) Exercise eight women; seven men Age = 58.9 (3.5) BMI = 25.6 (3.1) |
12 weeks | Supervised exercise 2 d week−1. 1 to 60-min group session of various aerobic activities. 1 to 90-min individual session of nine exercises using cardio and weight-stack machines (two sets, 10 reps, eight exercises) |
14-d tri-axial accelerometer at baseline, 6 and 12 weeks | At 12 weeks, the mean non-exercise accelerometer output on training days was significantly lower than on non-training days. No significant differences in non-exercise accelerometer output between training and non-training days was noted at week 6. |
| Meijer et al. (2000) (50) | Control six men; five women Age = 59 (4) BMI = 26 (3) Exercise 11 men; 11 women Age = 63 (8) BMI = 29 (4) |
12 weeks | Supervised exercise 2 d week−1. 1 to 60-min group session of various aerobic activities. 1 to 90-min individual session of nine exercises using cardio and weight-stack machines (two sets, 10 reps, eight exercises). Intensity ~50% HR reserve. |
14-d tri-axial accelerometer at baseline, 6 and 12 weeks | At 12 weeks, the mean non-exercise accelerometer output on training days was significantly lower than on non-training days. No significant differences in non-exercise accelerometer output between training and non-training days was noted at week 6. |
| Morio et al. (1998) (47) | Five men; eight women Age = 62.8 (2.3) BMI = 25.2 (NR) |
14 weeks | Supervised cycle ergometer exercise, 3 d week−1 Weeks 1–2: 20 min at 50% VO2 max Weeks 3–14: Interval training alternating between 50% VO2 max (5 min) and 3 min at lactate threshold. Exercise intensity was 61% VO2 max at week 7 and 63% at week 14. |
7-d activity diary at base, 7 weeks and 14 weeks. EE of usual recorded activities assessed by whole room calorimetry. Non-exercise EE = TDEE – (sleep EE + EEEx) |
Non-exercise EE decreased significantly both at 7 weeks (4.8%) and 14 weeks (7.7%) |
Mean (SD).
AEE, activity energy expenditure; ARTE, activity-related time equivalent; DLW, doubly labelled water; EE, energy expenditure; EEEx, exercise energy expenditure; HR, heart rate; NR, not reported; RMR, resting metabolic rate; RPE, rating of perceived exertion; SD, standard deviation; TDEE, total daily energy expenditure; TEF, thermic effect of food.
Non-randomized trials: study characteristics
Sample size/completion rate: the median (range) sample size across the 10 non-randomized trials was 21 (11–34). The completion rate in the one trial that reported this information was 83% (44).
Trial length: the median (range) length of non-randomized trials was 12 (8–26) weeks.
Exercise mode: four of the 10 non-randomized trials employed indoor or outdoor walking/running (43,44,46,51), three used cycle ergometer exercise (19,45,47), two used a combination of fitness centre-based aerobic and resistance training (49,50), and one trial used resistance training only (48).
Exercise supervision: all exercise sessions were supervised in six trials (19,45,47–50) and partially supervised in four trials (43,44,46,51).
Exercise prescription (frequency): the median (range) exercise frequency was 3 (2–5) d/week.
Exercise prescription (intensity): two trials prescribed intensity as a percentage of maximal VO2 (volume of oxygen consumed min−1) (45,47), two by percentage of maximal heart rate (19,51), one by heart rate reserve (50) and one by ratings of perceived exertion (44). The median (range) of intensity prescriptions was 74% (62–85%) maximal VO2; 73% (70–77%) maximal heart rate, 50% heart rate reserve; and perceived exertion 11–13 on a 15-point scale. Resistance training in the study by Hunter et al (48) was conducted at 65–85% one repetition maximum. Prescribed exercise intensity was not reported in three trials (43,46,49).
Exercise prescription (duration). Five trials prescribed exercise duration by time (19,44,47,49,50), two by level of exercise energy expenditure (43,45) and two by walking/running distance (46,51). The median (range) duration of exercise for the five trials prescribing exercise by time was 150 (60–200) min/week. The median (range) for trials prescribing exercise by energy expenditure was 975 (450–1500) kcal/week. Prescribed walking distance was 3–6 km d−1 (51), and running distance was 25–40 km week−1 (46).
Compliance with the exercise protocol: four trials reported the percentage of exercise sessions attended (range 83–100%) (19,44,49,50), whereas one trial reported the level of exercise energy expenditure (prescribed 1500 kcal week−1; achieved 1434 kcal week−1) (43). Compliance with the exercise protocol was not reported in five trials (45–48,51).
Physical activity/energy expenditure assessment: physical activity/energy expenditure was assessed by accelerometer in two trials (49,50), both accelerometer and doubly labelled water in two trials (43,46), heart rate monitoring with individual heart rate/energy expenditure calibration in two trials (19,51), doubly labelled water in two trials (45,48), an activity diary in one trial (47), and a SenseWear (BodyMedia, Pittsburgh, PA, USA) arm band in one trial (44). Non-exercise energy expenditure was the outcome measure in six trials (19,44,45,47,48,51), both non-exercise energy expenditure and non-exercise physical activity were the outcomes in two trials, (43,46) whereas non-exercise physical activity was the outcome in two trials (49,50).
Assessment of exercise energy expenditure: five trials assessed the energy expenditure of the prescribed exercise. Three trials used heart rate with individual heart rate/energy expenditure calibration (19,43,45), one trial used indirect calorimetry (48) and one trial used a whole-room calorimeter (47).
Non-randomized trials: participant characteristics
Age: the median (range) age across all non-randomized trials was 58 (32–67) years.
Gender: six trials (60%) included both men and women (45–50), whereas four trials (42%) included women only (19,43,44,51).
BMI: the median (range) BMI was 27 (23–34) kg/m2. Five of the nine trials that reported BMI had a mean sample BMI in the overweight category (i.e. 25–29.9 kg m−2), (19,44,47,49,50) whereas the mean sample BMI was classified as obese (i.e. ≥30 kg m−2) in one trial (43) and normal weight (i.e. <25 kg m−2) in three trials (45,46,48).
Minority status: one study described the minority representation in the study sample (100% white) (48). No study reported non-exercise physical activity/energy expenditure by race or ethnicity.
Participant activity level: nine of the 10 non-randomized trials that described inclusion criteria for level of baseline physical activity recruited sedentary participants (19,43,44,46–51).
Non-randomized trials: results
Non-exercise physical activity/energy expenditure: five of 10 non-randomized trials reported a significant decrease in non-exercise physical activity (49,50) or non-exercise energy expenditure (43,45,47) resulting from participation in prescribed exercise. Increased non-exercise energy expenditure was reported in two trials: one in response to resistance (48) and one in response to aerobic exercise training (46). Interestingly, Meijer et al. (46) reported increased non-exercise energy expenditure assessed by doubly labelled water in a small subsample of participants (n = 4 men, n = 4 women) but found no effect of exercise on non-exercise physical activity as assessed by accelerometer in the complete sample (n = 16 men, n = 16 women). One trial showed no change in mean non-exercise energy expenditure in a sample of 34 women participating in a walking programme (4 d week−1, 13 weeks); however, non-exercise energy expenditure was significantly increased in 56% and decreased in 44% of women (44). Manthou et al. (19) reported a significant increase in total daily energy expenditure from baseline to end study (8 weeks) in 34 women who completed 150 min week−1 of supervised cycle ergometer exercise which suggests either no change or an increase in non-exercise energy expenditure. However, non-exercise energy expenditure was increased significantly in responders (fat loss >predicted) compared with non-responders (fat loss <predicted). Keytel et al. (51) reported no difference in total daily energy expenditure assessed by 24-h heart rate monitoring in a sample of women who completed an 8-week, partially supervised walking protocol.
Effect of study parameters on non-exercise physical activity/energy expenditure
Exercise mode: no study compared non-exercise physical activity/energy expenditure by mode of exercise training. Decreased non-exercise physical activity/energy expenditure has been shown across a variety of exercise modes including group exercise classes, consisting of a combination of aerobic and resistance exercise (49,50), outdoor walking (43) and cycle ergometer exercise (45,47). Increased non-exercise energy expenditure has been shown with both aerobic (46) and resistance training (48). No change in non-exercise physical activity/energy expenditure has been reported with outdoor walking (44).
Level of exercise energy expenditure/duration: no study compared non-exercise physical activity/energy expenditure by level of exercise energy expenditure or duration of exercise. Decreased non-exercise physical activity/energy expenditure has been shown with exercise energy expenditures of 900 (45) and 1500 kcal week−1 (43), durations of 75 (47) and 150 min week−1 (49,50) and walking 9–18 km week−1 (51). Non-exercise physical activity/energy expenditure increased in response to a running programme that progressed from 15 to 40 km week−1 (46). No change in non-exercise physical activity/energy expenditure has been shown with 200 min week−1 of walking exercise (44).
Exercise intensity: no study compared non-exercise physical activity/energy expenditure by level of exercise intensity. Decreased non-exercise physical activity/energy expenditure has been shown with exercise energy intensities of 60–85% VO2 max (45,47) and ~50% heart rate reserve (50). No change in non-exercise physical activity/energy expenditure has been shown with exercise at 70–77% max heart rate (19,51).
Effect of participant characteristics on non-exercise physical activity/energy expenditure
Age: no study evaluated the effect of age on changes in non-exercise physical activity/energy expenditure in response to exercise training. Studies were generally conducted in adults with a median age of 58 years which was older than the median age of participants in or short-term studies (29 years) and similar to the median age of participants in randomized trials (53 years).
Gender: none of the six non-randomized trials that included both men and women reported changes in non-exercise physical activity/energy expenditure by gender (45–50).
BMI: no study evaluated the effect of BMI on changes in non-exercise physical activity/energy expenditure in response to exercise training. Three of the 10 non-randomized trials that reported a significant decrease in non-exercise physical activity/energy expenditure were conducted in overweight individuals (47,49,50), and one each in normal weight (45) and obese individuals (43). One trial did not report participant BMI (51).
Fitness/activity level: one non-randomized trial reported that low baseline fitness was associated with greater decreases in non-exercise energy expenditure (43). Non-randomized trials were generally conducted in sedentary individuals (19,43,44,46–51).
Randomized trials
The seven randomized trials constituted ~23% of the total number of studies identified for this review (Table 4). The majority of randomized trials (5/7) compared non-exercise physical activity/energy expenditure between participants randomly assigned to an exercise group/groups vs. a non-exercise control (15,21,52–54). One trial compared non-exercise physical activity/energy expenditure between different exercise durations and intensities (55), whereas one trial compared aerobic, resistance, and a combination of aerobic and resistance training (56). With the exception of the trial by Rosenkilde et al. (21), who reported both efficacy and intent-to-treat results, all other randomized trials employed an efficacy approach.
Table 4.
Randomized trials
| Study | Participants | Length | Intervention | Exercise/Activity assessment | Results |
|---|---|---|---|---|---|
| Church et al. (2009) (15) | Control: 94 women Age = 57.2 (5.9)* BMI = 32.2 (3.9) Exercise- 4 kcal kg−1 week−1 (KKW) 139 women Age = 57.9 (6.5) BMI = 31.4 (3.7) Exercise- 8 KKW 85 women Age = 56.7 (6.4) BMI = 32.2 (4.1) Exercise-12 KKW 93 women Age = 56.4 (6.3) BMI = 31.1 (3.6) |
6 months | (i) control, no exercise (ii) exercise, three to four sessions week−1 at 50% VO2 max designed to achieve energy expenditures of 4, 8 and 12 KKW Exercise alternated between semi-recumbent bike and treadmill |
Pedometers worn daily except during exercise training | No significant between-group differences in mean daily steps at 6 months No significant change in mean daily steps from baseline to 6 months in any exercise group |
| Fujita et al. (2003) (52) | Control: 15 men; 16 women Exercise: 15 men; 16 women Age = 67.1 (NR) BMI = NR |
25 weeks with 6-month follow-up | (i) Control, two 2-h classes (1-h lecture on non-exercise topic, 1-h board games). Asked to attend one session month−1 (ii) Exercise, 2–3 h supervised exercise classes week−1. Endurance exercise –cycle ergometer at 50–60% HR reserve and RT with resistance bands |
Activity diary 3 consecutive week days pre and post. TDEE (kcal kg−1 d−1) calculated by (activity time × MET value)/body weight | TDEE increased significantly pre- to post-intervention in exercise group but not controls. The change in TDEE was significant only in women. At 6-month follow-up, TDDE was significantly higher in than baseline in the exercise group |
| Hollowell et al. (2009) (55) | Control: four men; four women Age = 51 (7) BMI = 31 (3) Exercise: low amount/moderate intensity three men, five women. Age = 57(6) BMI = 29 (3) Exercise: low amount/vigorous intensity 10 men; 10 women. Age = 54 (6) BMI = 30 (3) Exercise: high amount/vigorous intensity Age = 51 (6) BMI = 30 (2) |
8 months | Control: no exercise Exercise: three to five times week−1 Low amount/moderate intensity: 40–55% −1 VO2 peak to achieve EE of 5023 kJ week Low amount/vigorous intensity: 65–85% VO2 peak to achieve EE of 5023 kJ week−1 High amount/vigorous intensity: 65–85% −1 VO2 peak to achieve EE of 8372 kJ week |
7 d tri-axial accelerometer at baseline and end Removed accelerometer data during exercise sessions and 30 min pre- and post-exercise. |
No between-group differences for change in non-exercise EE Change in total PA energy expenditure was significantly greater in high amount/vigorous intensity vs. control and between low amount/vigorous intensity and high amount/vigorous intensity |
| Rangan et al. (2011) (56) | Aerobic training: 14 men, 14 women Age = 51.8 (9.2) BMI = 30.5 (3.1) RT: eight men; 20 women Age = 50.6 (12.4) BMI = 30.3 (3.1) Aerobic + RT: 10 men; 16 women. Age = 47.5 (11.0) BMI = 30.9 (3.2) |
8 months | Aerobic: Treadmill, elliptical or cycle ergometer exercise ramped over 8–10 weeks. for a goal EE of 14 KKW. RT: 3 d week−1., three sets, 8–12 reps, eight major muscle groups. Aerobic + RT: Linear combination of both exercise prescriptions |
7 d tri-axial accelerometer at baseline and end Removed accelerometer data during exercise sessions and 30 min pre- and post-exercise |
No significant change in non-exercise PA from baseline to end study in any group |
| Rosenkilde et al. (2012) (21) | Control: 17 men Age = 31(6) BMI = 28 (2.3) Moderate dose exercise (MOD): 18 men Age = 30(7) BMI = 28.6(1.8) High-dose exercise (HIGH): 18 men Age = 28(5) BMI = 27.6(1.4) |
13 weeks | Control: no exercise MOD: Treadmill running/cycling 300 kcal d−1. Higher intensity sessions (>70% VO2 max) 3 d week−1 HIGH: Same as MOD with goal of 600 kcal d−1 |
3 d uniaxial accelerometer at baseline and the average of accelerometer output obtained at 6 and 11 weeks post-randomization. Non-exercise PA was obtained by subtracting activity counts during prescribed exercise from total activity counts |
Increase in total activity counts was significantly greater in both MOD and HIGH vs. control No significant difference for change in non-exercise PA in any group Note: Non-exercise PA was increased 37% (p = 0.09) in MOD vs. control |
| Turner et al. (2010) (53) | Control: 14 men Age = 53(4) BMI = 27.6 (3) Exercise: 15 men. Age = 55 (5) BMI = 28.1(2.7) |
24 weeks | Control: no exercise Exercise: Walk/run/cycle or cross-training. Progressed from 30 min, 3 d week−1. at ~50% VO2 max at weeks 1–2 to 60 min. 4 d week−1 at 70% VO2 max by week 24. Approximately 10% of exercise sessions were supervised. |
7 consecutive days monitoring with a synchronized HR-accelerometer device at baseline, weeks 2, 9 and 18 during the intervention, and during 2 weeks of detraining. Non-exercise EE = TDEE – EEEx. EEEx was estimated from electronic monitoring system on exercise equipment | No change in non-exercise EE across the study period Trend for non-exercise EE to be maintained in the exercise group relative to a decrease over time in the control group |
| Van Etten et al. (1997) (54) | Control: eight men Age = 35(6) BMI = 23.6(NR) Exercise: 18 men Age = 33 (6) BMI = 23.8 (NR) |
18 weeks | Control: No exercise Exercise: Supervised RT, 2 non-consecutive days week−1, three sets, 15 reps, 10 exercises |
Two methods at baseline and end, 7 d triaxial accelerometer DLW on 12 of 18 exercisers. Non-training EE = (TDEE + TEF + sleep EE + net EEEx) |
No change in non-training EE assessed by accelerometer in exercise or control groups No change in DLW assessed non-training EE in the exercise group |
Mean (SD).
DLW, doubly labelled water; EE, energy expenditure; EEEx, exercise energy expenditure; HR, heart rate; KKW, kcal kg−1 week−1; NR, not reported; PA, physical activity; RT, resistance training; SD, standard deviation; TDEE, total daily energy expenditure; TEF, thermic effect of food.
Randomized trials: study characteristics
Sample size/completion rate: the median (range) sample size across the seven randomized trials was 53 (26–411). The median (range) proportion of randomized participants who completed the intervention and provided data for non-exercise physical activity/energy expenditure was 87% (38–100%).
Trial length: the median (range) length of the seven randomized trials was 24 (13–32) weeks.
Exercise mode: the majority of randomized trials (four of seven, 57%) involved laboratory-based aerobic exercise conducted on cycle ergometers/rowers/steppers/treadmills (15,21,55), or outdoor walking/running (53); two trials used a combination of resistance and aerobic training, (52,56) and one trial involved resistance training only (54).
Exercise supervision: all exercise sessions were supervised in five of seven (71%) of randomized trials (15,52,54–56) and partially supervised in two trials (29%) (21,53).
Exercise prescription (frequency): exercise frequency ranged from 3 to 5 d/week in groups randomized to aerobic exercise and 2–3 d week−1 for groups randomized to resistance training.
Exercise prescription (intensity): in the six randomized trials that included aerobic exercise, intensity was prescribed as a percentage of maximal/peak VO2 in five trials (15,21,53,55,56), whereas one trial prescribed exercise intensity as a percent of heart rate reserve (52). The median (range) of intensity prescriptions was 65% (50–85%) of maximal VO2. Exercise was prescribed at 50–60% of heart rate reserve in the one trial that employed this method (52).
Exercise prescription (duration). Three randomized trials prescribed exercise duration by energy expenditure/kilogram body weight (15,55,56), two by time (52,53) and one by level of exercise energy expenditure (21). Exercise time was 60 (53) and 120 min d−1 (52); 300 and 600 kcal d−1 (21); 4, 8 and 12 kcal kg−1 week−1 (15); 14 kcal kg−1 week−1 (56); and 59 and 96 kJ kg−1 week−1 (55). Resistance training in the study by VanEtten et al. (54) consisted of three sets of 15 reps over 10 exercises.
Compliance with the exercise protocol: five studies presented data relative to participant compliance with the exercise training protocol as assessed by the percentage of scheduled exercise sessions attended (15,21,53,54,56). The median (range) percentage of exercise sessions attended was 96% (84–99%).
Physical activity/energy expenditure assessment: physical activity/energy expenditure was assessed by accelerometer in three trials (21,55,56). Trials also used a heart rate/accelerometer device (53), pedometers (15), activity diaries (52), and both accelerometers and doubly labelled water (54). Non-exercise energy expenditure was the outcome measure in four trials (52–55), whereas non-exercise physical activity was the outcome in three trials (15,21,56).
Assessment of exercise energy expenditure: four trials assessed the energy expenditure of the prescribed exercise. Two trials used heart rate with individual heart rate/energy expenditure calibration (21,54), one trial used indirect calorimetry (15) and one trial used date, time and duration of each exercise session recorded by an electronic monitoring system (53).
Randomized trials: participant characteristics
Age: the median (range) age across all randomized trials was 53 (34–67) years.
Gender: three trials included both men and women (52,55,56), three trials included only men (21,53,54) and one trial included only women (15). Only one of the three trials that included both men and women provided separate results by gender (52).
BMI: the median (range) BMI for participants over the six randomized trials that provided baseline BMI data was 29.1 (23.7–31.1) kg/m2. Two randomized trials evaluated overweight participants (i.e. BMI 25–29.9 kg m−2) (21,53), whereas the mean sample BMI was classified as obese (i.e. >30 kg m−2) in three trials (15,55,56) and normal weight (i.e. BMI < 25 kg m−2) in one trial (54).
Minority status: one study described the minority representation in the study sample (36.5% minority) (15). No study reported non-exercise physical activity/energy expenditure by race or ethnicity.
Participant activity level: six of the seven non-randomized trials that described inclusion criteria for level of baseline physical activity recruited sedentary participants (15,21,53–56).
Randomized trials: results
Non-exercise physical activity/energy expenditure: five of the seven randomized trials provided data on the response of either non-exercise physical activity (15,21,56) or non-exercise energy expenditure (53,55), resulting from participation in prescribed aerobic (15,21,53,55), or a combination of aerobic and resistance exercise (56). No change in either non-exercise physical activity or non-exercise energy expenditure was reported in any of these five trials. Fujita et al (52) reported a significant increase in total daily energy expenditure in response to a combination of aerobic and resistance training which indirectly suggests that non-exercise energy expenditure was not decreased. No change in non-exercise energy expenditure was reported in the one trial that evaluated the response to resistance training (54).
Effect of study parameters on non-exercise physical activity/energy expenditure
Exercise mode: no significant differences in non-exercise physical activity were shown in the one randomized trial that compared the effects of aerobic, resistance, and a combination of aerobic and resistance training (56). No changes in non-exercise physical activity energy expenditure were shown for laboratory-based aerobic exercise conducted on cycle ergometers/rowers/steppers/treadmills (15,21,55), outdoor walking/running (53), a combination of resistance and aerobic training (52), and resistance training alone (54).
Level of exercise energy expenditure/duration: three randomized trials compared non-exercise physical activity/energy expenditure by level of exercise energy expenditure or exercise duration (15,21,55). No differences in non-exercise physical activity/energy expenditure have been shown in response to exercise training at 4, 8 and 12 kcal kg−1 week−1 (15), 5023 and 8372 kJ week−1 (55) or 900 and 1800 kcal week−1 (21).
Exercise intensity: the one randomized trial that compared non-exercise energy expenditure by level of exercise intensity (40–55% vs. 65–85% VO2 peak) found no significant difference by intensity groups (55). No differences in non-exercise physical activity/energy expenditure have been shown with exercise over a range of 50–85% maximal VO2 (15,21,53,55,56). Effect of participant characteristics on non-exercise physical activity/energy expenditure
Age: no randomized trials evaluated the effect of age on changes in non-exercise physical activity/energy expenditure in response to exercise training. Randomized trials were conducted in adults with a median age of 53 years, which was similar to the age of participants in non-randomized trials (58 years) and older than participants in short-term trials (29 years)
Gender: no randomized trials provided data on gender differences for changes in non-exercise physical activity/energy expenditure in response to exercise training. However, studies that have included only men (21,53,54) or women (15) have both shown no change in non-exercise physical activity/energy expenditure in response to exercise training. Fujita et al. (52) reported significant increases in total daily energy expenditure in response to exercise training in women but not in men, providing indirect evidence for decreased non-exercise energy expenditure in men.
BMI: no randomized trials evaluated the effect of BMI on changes in non-exercise physical activity/energy expenditure in response to exercise training. No change in non-exercise physical activity/energy expenditure was reported in trials including normal weight (54), overweight (21,53) or obese (15,55,56) participants.
Fitness/activity level: no randomized trials compared changes in non-exercise physical activity/energy expenditure by level of baseline fitness or physical activity. Randomized trials were generally conducted in previously sedentary individuals (15,21,53–56).
Risk of bias: the risk of bias for all randomized trials is presented in Table 5. The description of the procedures for random sequence generation was unclear in approximately 29% of randomized trials. Four trials adequately described randomization procedures and were considered low risk of bias (21,52,55,56), whereas one trial was considered high risk for randomization bias based on failure to provide any description of the randomization process (54). No trials described procedures for allocation concealment. Blinding participants and personnel is not feasible in an exercise trial. Although blinding of personnel performing outcome assessments is feasible, these procedures were not described in any of the seven randomized trials. The risk of attrition bias was high in three trials where the study sample represented only 38.8% (55), 43% (56) and 53.7% (53) of those randomized at baseline.
Table 5.
Risk of bias
| Study | Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias |
|---|---|---|---|---|---|---|---|
| Church et al. (2009) (15) | Unclear | NR | High risk | NR | Low risk | Low risk | High risk |
| Fujita et al. (2003) (52) | Low risk | NR | High risk | NR | Low risk | Low risk | High risk |
| Hollowell et al (2009) (55) | Low risk | NR | High risk | NR | High risk | Low risk | High risk |
| Rangan et al (2011) (56) | Low risk | NR | High risk | NR | High risk | Low risk | High risk |
| Rosenkilde et al. (2012) (21) | Low risk | NR | High risk | NR | Low risk | Low risk | High risk |
| Turner et al. (2010) (53) | Unclear | NR | High risk | NR | High risk | Low risk | High risk |
| VanEtten et al. (1997) (54) | High risk | NR | High risk | NR | Low risk | Low risk | High risk |
NR, not reported.
Discussion
Summary of evidence
We systematically reviewed 31 studies utilizing a variety of designs including cross-sectional, short-term, non-randomized and randomized trials to address this question: does increased prescribed exercise alter non-exercise physical activity/energy expenditure in healthy adults? It has been hypothesized that a reduction in non-exercise energy expenditure might compensate for the increased energy expenditure of prescribed exercise, resulting in no change in total daily energy expenditure and no or minimal exercise-induced weight loss (23). Based on our review of 31 studies utilizing a variety of study designs, we find no compelling evidence to support this hypothesis. Only five of 31(16%) studies included in this review reported a significant decrease in non-exercise physical activity assessed by accelerometer (49,50) or non-exercise energy expenditure assessed by doubly labelled water (43,45) or an activity diary (47). In contrast, four studies included in this review (13%) suggested increased non-exercise physical activity/energy expenditure in response to both increased occupational activity and exercise training (28,29,46,48). For example, results from two cross-sectional studies suggested higher levels of occupational activity were associated with higher levels of leisure time activity (28,29), whereas two non-randomized trials reported significantly increased non-exercise energy expenditure in response to both aerobic (46) and resistance training (48). All five studies that reported decreased non-exercise physical activity/energy expenditure employed a non-randomized design, included primarily aerobic exercise training and were conducted in sedentary overweight or obese older adults, median age of 61 years (43,45,47,49,50). Interestingly, the median age across all other study designs that found no evidence for decreased non-exercise physical activity/energy expenditure was 44 (range 29–53 years). These results suggest that non-exercise physical activity/energy expenditure may decrease in response to exercise training in older individuals. However, this hypothesis has not been evaluated in a trial comparing change in non-exercise physical activity/energy expenditure between older and younger participants in response to identical exercise training protocols.
Limitations in the available literature
There are several important limitations in the literature available for this systematic review. The most critical limitation is that no studies were specifically designed and adequately powered to detect significant between- or within-group differences in non-exercise physical activity/energy expenditure in response to exercise training. However, the randomized trial by Fujita et al. (52) was powered to evaluate changes in total daily energy expenditure in response to a combination of cycle ergometer and resistance exercise training. Although all 10 non-randomized trials were specifically designed to evaluate the effect of exercise training on non-exercise physical activity/energy expenditure, the majority of these trials (60%) were conducted in small samples of <20 total participants or <20 participants/group (43,45,47,48,50,51). The two randomized trials (~29%) that were conducted specifically to evaluate the effect of exercise training on non-exercise physical activity/energy expenditure were also conducted in small samples of <20 participants/group (53,54).
The literature is also limited by the lack of studies that have employed state-of-the-art techniques to evaluate the impact of exercise training on non-exercise energy expenditure. In the context of weight management, it is important to assess the effect of participation in exercise training on non-exercise energy expenditure rather than non-exercise physical activity. However, the impact of exercise training on non-exercise energy expenditure was reported in only 14 of 31 studies (~45%) identified for this review (33–35,43–48,51,53–55). Only six of those 14 studies, with a total sample size of 65 participants, assessed non-exercise energy expenditure using measures of total daily energy expenditure assessed by doubly labelled water, considered the gold standard for the measurement of energy expenditure in free-living individuals (57). These six studies included a variety of designs: one short-term crossover (36), four non-randomized trials (43,45,46,48) and one randomized trial (54). Estimation of non-exercise energy expenditure using doubly labelled water also requires accurate assessments of both resting and exercise energy expenditure. Although all six studies assessed resting energy expenditure using indirect calorimetry, only one non-randomized trial assessed exercise energy expenditure by indirect calorimetry (46). This trial evaluated the impact of running 24–40 km week−1 in preparation for a half-marathon competition on non-exercise energy expenditure in a small sample of eight normal weight individuals. Other trials used less precise measures of exercise energy expenditure. These included heart rate with individual heart rate/energy expenditure calibrations (43,45,54), estimates of exercise energy expenditure (indirect calorimetry) obtained from a previous trial which used a similar exercise training protocol (48) or calculated physical activity level (total energy expenditure divided by resting energy expenditure) (36). Thus, no studies included in this review were both adequately powered and provided estimates of non-exercise energy expenditure obtained using state-of-the-art techniques.
The available literature is also limited by an insufficient number of studies that have evaluated the impact of either exercise parameters or participant characteristics on non-exercise physical activity/energy expenditure. For example, no studies were identified that have evaluated the effect of age, gender, race/ethnicity, BMI, and only one study that reported the association of baseline physical fitness on the response of non-exercise energy expenditure to exercise training (43). The impact of exercise mode (56) and intensity (55) has each been assessed in only one study. Although six studies, three short-term (34–36) and three randomized trials (15,21,55) evaluated the impact of exercise duration/energy expenditure on non-exercise physical activity/energy expenditure, only one short-term study (14 d) provided assessments of non-exercise energy expenditure using double-labelled water (36). Evidence for the influence of the time of day at which exercise training is performed on non-exercise physical activity/energy expenditure is available only from three short-term trials (37,39,40). No studies have evaluated the effect of exercise frequency, intermittent vs. continuous exercise or the time course of any change in non-exercise physical activity/energy expenditure. Information relative to the impact of both exercise parameters and participant characteristics on non-exercise physical activity energy expenditure would inform the design and delivery of exercise-based weight management programmes.
Limitations of this review
Our conclusions should be cautiously interpreted as they are based on both data primarily from suboptimal study designs (e.g. cross-sectional, short-term, non-randomized trials) and from randomized trials with a high risk of one or more forms of bias. In addition, we did not contact authors to obtain missing data or for clarification of any information presented in the published reports; therefore, missing information may reflect reporting bias as opposed to any limitations in the conduct of the study.
Conclusions
The present systematic review found no evidence to suggest that exercise training has a significant effect on non-exercise physical activity/energy expenditure. However, as previously discussed, the available literature on this topic suffers numerous methodological shortcomings. Therefore, we recommend additional randomized trials designed to evaluate the impact of exercise training on non-exercise physical activity/energy expenditure in overweight/obese adults that (i) are powered specifically to detect clinically significant differences; (ii) assess non-exercise energy expenditure using measures of total daily energy expenditure assessed by doubly labelled water and using measurements of resting and exercise energy expenditure in calculating non-exercise energy expenditure; (iii) evaluate the impact of both exercise parameters (mode, frequency, intensity, duration, time of day, intermittent vs. continuous) and participant characteristics (age, gender, BMI, race/ethnicity, fitness/activity level; and (iv) evaluate levels of exercise for weight management currently recommended by governmental agencies or professional organizations such as the International Association for the Study of Obesity, the Institute of Medicine and ACSM.
Acknowledgments
This review was supported by the International Life Science Institute
Appendix
Complete search strategy
‘Physical activity’ [Title/Abstract] OR ‘Exercise’ [Title/Abstract] OR ‘training’ [Title/Abstract] OR ‘energy expenditure’ [Title/Abstract]) AND (off-exercise[Title/Abstract] OR nonexercise[Title/Abstract] OR non-exercise[Title/Abstract] OR activities of daily living[Title/Abstract] OR activity counts[Title/Abstract] OR spontaneous physical activity[Title/Abstract] OR spontaneous activity[Title/Abstract] OR compensation[Title/Abstract] OR compensatory[Title/Abstract]) NOT ‘multiple sclerosis’ [Title/Abstract] NOT spinal[Title/Abstract] NOT paraplegia[Title/Abstract] NOT stroke[Title/Abstract] NOT athletes[Title/Abstract] NOT Alzheimer’s[Title/Abstract] NOT fibromyalgia[Title/Abstract] NOT wheelchair[Title/Abstract] NOT (‘surgical procedures, operative’ [MeSH Terms] OR ‘general surgery’ [MeSH Terms]) NOT cancer[Title/Abstract] NOT COPD[Title/Abstract] NOT ‘dialysis’ [Title/Abstract] NOT pregnant[Title/Abstract] NOT ‘injury’ [Title/Abstract] NOT HIV[Title/Abstract] NOT children[Title/Abstract] NOT parkinson[Title/Abstract] NOT heart failure[Title/Abstract] AND (hasabstract[text] AND (‘1990/01/01’ [PDAT]: ‘2013/03/11’ [PDAT]) AND ‘humans’ [MeSH Terms] AND English[lang] AND (‘adult’ [MeSH Terms:noexp] OR ‘middle aged’ [MeSH Terms]).
Footnotes
Potential Conflict of Interests
JD and RW are investigators of individual trials included in this review. The authors declare that they have no other competing interests.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of Body Mass Index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28:w822–ww31. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003–2008 Study. Int J Obes (Lond) 2011;35:1063–1070. doi: 10.1038/ijo.2010.229. [DOI] [PubMed] [Google Scholar]
- 4.Saris WH, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4:101–114. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine, Panel on Macronutrients, Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Natl Academy Press; Washington DC: 2005. [Google Scholar]
- 6.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Office of Disease Prevention & Health Promotion; Washington DC: 2008. [accessed March 2012]. [WWW document]. URL http://www.health.gov/paguidelines. [Google Scholar]
- 7.U.S. Department of Health and Human Services. Healthy People 2020. Office of Disease Prevention and Health Promotion; Washington, DC: 2010. [accessed March 2012]. [WWW document]. URL http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=33. [Google Scholar]
- 8.Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 9.Donnelly JE, Hill JO, Jacobsen DJ, et al. Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women: the Midwest Exercise Trial. Arch Intern Med. 2003;163:1343–1350. doi: 10.1001/archinte.163.11.1343. [DOI] [PubMed] [Google Scholar]
- 10.Slentz CA, Duscha BD, Johnson JL, et al. Effects of the amount of exercise on body weight, body composition, and measures of central obesity – STRRIDE – a randomized controlled study. Arch Intern Med. 2004;164:31–39. doi: 10.1001/archinte.164.1.31. [DOI] [PubMed] [Google Scholar]
- 11.Wilmore JH, Stanforth PR, Hudspeth LA, et al. Alterations in resting metabolic rate as a consequence of 20 wk of endurance training: the HERITAGE Family Study. Am J Clin Nutr. 1998;68:66–71. doi: 10.1093/ajcn/68.1.66. [DOI] [PubMed] [Google Scholar]
- 12.Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006;36:239–262. doi: 10.2165/00007256-200636030-00005. [DOI] [PubMed] [Google Scholar]
- 13.Gilliat-Wimberly M, Manore MM, Woolf K, Swan PD, Carroll SS. Effects of habitual physical activity on the resting metabolic rates and body compositions of women aged 35 to 50 years. J Am Diet Assoc. 2001;101:1181–1188. doi: 10.1016/S0002-8223(01)00289-9. [DOI] [PubMed] [Google Scholar]
- 14.Potteiger JA, Kirk EP, Jacobsen DJ, Donnelly JE. Changes in resting metabolic rate and substrate oxidation after 16 months of exercise training in overweight adults. Int J Sport Nutr Exerc Metab. 2008;18:79–95. doi: 10.1123/ijsnem.18.1.79. [DOI] [PubMed] [Google Scholar]
- 15.Church TS, Martin CK, Thompson AM, et al. Changes in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal women. PLoS ONE. 2009;4:e4515. doi: 10.1371/journal.pone.0004515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King NA, Caudwell P, Hopkins M, et al. Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss. Obesity. 2007;15:1373–1383. doi: 10.1038/oby.2007.164. [DOI] [PubMed] [Google Scholar]
- 17.King NA, Hopkins M, Caudwell P, Stubbs RJ, Blundell JE. Individual variability following 12 weeks of supervised exercise: identification and characterization of compensation for exercise-induced weight loss. Int J Obes (Lond) 2008;32:177–184. doi: 10.1038/sj.ijo.0803712. [DOI] [PubMed] [Google Scholar]
- 18.Westerterp K. Pattern and intensity of physical activity. Nature. 2001;410:539. doi: 10.1038/35069142. [DOI] [PubMed] [Google Scholar]
- 19.Manthou E, Gill JMR, Wright A, Malkova D. Behavioral compensatory adjustments to exercise training in overweight women. Med Sci Sports Exerc. 2010;42:1221–1228. doi: 10.1249/MSS.0b013e3181c524b7. [DOI] [PubMed] [Google Scholar]
- 20.Stubbs RJ, Hughes DA, Johnstone AM, et al. Rate and extent of compensatory changes in energy intake and expenditure in response to altered exercise and diet composition in humans. Am J Physiol Regul Integr Comp Physiol. 2004;286:R350–R358. doi: 10.1152/ajpregu.00196.2003. [DOI] [PubMed] [Google Scholar]
- 21.Rosenkilde M, Auerbach P, Reichkendler MH, et al. Body fat loss and compensatory mechanisms in response to different doses of aerobic exercise-a randomized controlled trial in overweight sedentary males. Am J Physiol Regul Integr Comp Physiol. 2012;303:R571–RR79. doi: 10.1152/ajpregu.00141.2012. [DOI] [PubMed] [Google Scholar]
- 22.Donnelly JE, Honas JJ, Smith BK, et al. Aerobic exercise alone results in clinically significant weight loss for men and women: midwest exercise trial 2. Obesity. 2013;21:E219–E228. doi: 10.1002/oby.20145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Epstein LH, Wing RR. Aerobic exercise and weight. Addict Behav. 1980;5:371–388. doi: 10.1016/0306-4603(80)90011-8. [DOI] [PubMed] [Google Scholar]
- 24.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:e1–37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and work-flow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins JPT, Altman DG, Sterne JAC, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. [Accessed March 2012]. Chapter 8: Assessing risk of bias in included studies. Available from www.cochrane-handbook.org. [Google Scholar]
- 28.Parsons TJ, Thomas C, Power C. Estimated activity patterns in British 45 year olds: cross-sectional findings from the 1958 British birth cohort. Eur J Clin Nutr. 2009;63:978–985. doi: 10.1038/ejcn.2009.6. [DOI] [PubMed] [Google Scholar]
- 29.Wolin KY, Bennett GG. Interrelations of socioeconomic position and occupational and leisure-time physical activity in the National Health and Nutrition Examination Survey. J Phys Act Health. 2008;5:229–241. doi: 10.1123/jpah.5.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tigbe WW, Lean ME, Granat MH. A physically active occupation does not result in compensatory inactivity during out-of-work hours. Prev Med. 2011;53:48–52. doi: 10.1016/j.ypmed.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 31.Withers RT, Smith DA, Tucker RC, Brinkman M, Clark DG. Energy metabolism in sedentary and active 49- to 70-yr-old women. J Appl Physiol. 1998;84:1333–1340. doi: 10.1152/jappl.1998.84.4.1333. [DOI] [PubMed] [Google Scholar]
- 32.Alahmadi MA, Hills AP, King NA, Byrne NM. Exercise intensity influences nonexercise activity thermogenesis in overweight and obese adults. Med Sci Sports Exerc. 2011;43:624–631. doi: 10.1249/MSS.0b013e3181f7a0cb. [DOI] [PubMed] [Google Scholar]
- 33.McLaughlin R, Malkova D, Nimmo MA. Spontaneous activity responses to exercise in males and females. Eur J Clin Nutr. 2006;60:1055–1061. doi: 10.1038/sj.ejcn.1602417. [DOI] [PubMed] [Google Scholar]
- 34.Stubbs RJ, Sepp A, Hughes DA, et al. The effect of graded levels of exercise on energy intake and balance in free-living men, consuming their normal diet. Eur J Clin Nutr. 2002;56:129–140. doi: 10.1038/sj.ejcn.1601295. [DOI] [PubMed] [Google Scholar]
- 35.Stubbs RJ, Sepp A, Hughes DA, et al. The effect of graded levels of exercise on energy intake and balance in free-living women. Int J Obes (Lond) 2002;26:866–869. doi: 10.1038/sj.ijo.0801874. [DOI] [PubMed] [Google Scholar]
- 36.Whybrow S, Hughes DA, Ritz P, et al. The effect of an incremental increase in exercise on appetite, eating behaviour and energy balance in lean men and women feeding ad libitum. Br J Nutr. 2008;100:1109–1115. doi: 10.1017/S0007114508968240. [DOI] [PubMed] [Google Scholar]
- 37.King NA, Lluch A, Stubbs RJ, Blundell JE. High dose exercise does not increase hunger or energy intake in free living males. Eur J Clin Nutr. 1997;51:478–483. doi: 10.1038/sj.ejcn.1600432. [DOI] [PubMed] [Google Scholar]
- 38.Lynch KB, Corbin CB, Sidman CL. Testing compensation: does recreational basketball impact adult activity levels? J Phys Act Health. 2009;6:321–326. doi: 10.1123/jpah.6.3.321. [DOI] [PubMed] [Google Scholar]
- 39.Tudor-Locke C, Ainsworth BE, Thompson RW, Mathews CE. Comparison of pedometer and accelerometer measures of free-living physical activity. Med Sci Sports Exerc. 2002;34:2045–2051. doi: 10.1097/00005768-200212000-00027. [DOI] [PubMed] [Google Scholar]
- 40.Washburn RA, Ficker JL. Physical activity scale for the elderly (PASE): the relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness. 1999;39:336–340. [PubMed] [Google Scholar]
- 41.Koulouri AA, Tigbe WW, Lean MEJ. The effect of advice to walk 2000 extra steps daily on food intake. J Hum Nutr Diet. 2006;19:263–266. doi: 10.1111/j.1365-277X.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 42.Stubbs RJ, Hughes DA, Johnstone AM, et al. A decrease in physical activity affects appetite, energy, and nutrient balance in lean men feeding ad libitum. Am J Clin Nutr. 2004;79:62–69. doi: 10.1093/ajcn/79.1.62. [DOI] [PubMed] [Google Scholar]
- 43.Colley RC, Hills AP, King NA, Byrne NM. Exercise-induced energy expenditure: implications for exercise prescription and obesity. Patient Educ Couns. 2010;79:327–332. doi: 10.1016/j.pec.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 44.Di Blasio A, Ripari P, Bucci I, et al. Walking training in postmenopause: effects on both spontaneous physical activity and training-induced body adaptations. Menopause. 2012;19:23–32. doi: 10.1097/gme.0b013e318223e6b3. [DOI] [PubMed] [Google Scholar]
- 45.Goran MI, Poehlman ET. Endurance training does not enhance total energy expenditure in healthy elderly persons. Am J Physiol. 1992;263:E950–E957. doi: 10.1152/ajpendo.1992.263.5.E950. [DOI] [PubMed] [Google Scholar]
- 46.Meijer GA, Janssen GM, Westerterp KR, et al. The effect of a 5-month endurance-training programme on physical activity: evidence for a sex-difference in the metabolic response to exercise. Eur J Appl Physiol Occup Physiol. 1991;62:11–17. doi: 10.1007/BF00635626. [DOI] [PubMed] [Google Scholar]
- 47.Morio B, Montaurier C, Pickering G, et al. Effects of 14 weeks of progressive endurance training on energy expenditure in elderly people. Br J Nutr. 1998;80:511–519. doi: 10.1017/s0007114598001603. [DOI] [PubMed] [Google Scholar]
- 48.Hunter GR, Wetzstein CJ, Fields DA, Brown A, Bamman MM. Resistance training increases total energy expenditure and free-living physical activity in older adults. J Appl Physiol. 2000;89:977–984. doi: 10.1152/jappl.2000.89.3.977. [DOI] [PubMed] [Google Scholar]
- 49.Meijer EP, Westerterp KR, Verstappen FT. Effect of exercise training on total daily physical activity in elderly humans. Eur J Appl Physiol Occup Physiol. 1999;80:16–21. doi: 10.1007/s004210050552. [DOI] [PubMed] [Google Scholar]
- 50.Meijer EP, Westerterp KR, Verstappen FT. Effect of exercise training on physical activity and substrate utilization in the elderly. Int J Sports Med. 2000;21:499–504. doi: 10.1055/s-2000-7419. [DOI] [PubMed] [Google Scholar]
- 51.Keytel LR, Lambert MI, Johnson J, Noakes TD, Lambert EV. Free living energy expenditure in post menopausal women before and after exercise training. Int J Sport Nutr Exerc Metab. 2001;11:226–237. doi: 10.1123/ijsnem.11.2.226. [DOI] [PubMed] [Google Scholar]
- 52.Fujita K, Nagatomi R, Hozawa A, et al. Effects of exercise training on physical activity in older people: a randomized controlled trial. J Epidemiol. 2003;13:120–126. doi: 10.2188/jea.13.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Turner J, Markovitch D, Betts J, Thompson D. Nonprescribed physical activity energy expenditure is maintained with structured exercise and implicates a compensatory increase in energy intake. Am J Clin Nutr. 2010;92:1009–1016. doi: 10.3945/ajcn.2010.29471. [DOI] [PubMed] [Google Scholar]
- 54.Van Etten LM, Westerterp KR, Verstappen FT, Boon BJ, Saris WH. Effect of an 18-wk weight-training program on energy expenditure and physical activity. J Appl Physiol. 1997;82:298–304. doi: 10.1152/jappl.1997.82.1.298. [DOI] [PubMed] [Google Scholar]
- 55.Hollowell RP, Willis LH, Slentz CA, et al. Effects of exercise training amount on physical activity energy expenditure. Med Sci Sports Exerc. 2009;41:1640–1644. doi: 10.1249/MSS.0b013e31819c71a4. [DOI] [PubMed] [Google Scholar]
- 56.Rangan VV, Willis LH, Slentz CA, et al. Effects of an 8-month exercise training program on off-exercise physical activity. Med Sci Sports Exerc. 2011;43:1744–1751. doi: 10.1249/MSS.0b013e3182148a7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schoeller DA. Recent advances from application of doubly labeled water to measurement of human energy expenditure. J Nutr. 1999;129:1765–1768. doi: 10.1093/jn/129.10.1765. [DOI] [PubMed] [Google Scholar]