Abstract
Background: Soluble receptor of advanced glycation end-products (sRAGE) is widely expressed in various organs including male genital tract and spermatozoa. Their regulation depends on many simultaneous conditions that may occur. Male fertility is a multifactorial condition which is influenced by various parameters, some of which are detrimental to the spermatozoa. The aim of this study was to detect possible differences in sRAGE concentrations between serum and seminal plasma of infertile men, compared to fertile men population.
Methods: Seventy-five men were included in the study and divided into three groups: a group of fertile controls (age 34.8 ± 4.6 years, n =12) and two groups of men from infertile couples (age 36.1 ± 5.2 years) with normal (NS, n =10) and abnormal (AS, n =53) semen parameters, respectively. sRAGE was measured by ELISA in serum, and seminal plasma samples of all participants and biochemical, hormonal examinations, as well as anthropometric characteristics, were co-evaluated. Data were statistically analyzed using the chi-square test and the independent samples t-test. A two-tailed p <0.05 was considered significant.
Results: Serum sRAGE levels of fertile men were higher than those of men of infertile couples with AS or NS semen parameters (2,061 ± 884 pg/ml vs 1,673 ± 613 pg/ml and 1,411 ± 405 pg/ml, respectively; p <0.058). Seminal plasma sRAGE levels in fertile men were similar to the ones measured in both groups of men from infertile couples AS and NS (327 ± 81 pg/ml vs 322 ± 162 – 413 ± 207 pg/ml; p =0.197). Interestingly, the seminal plasma sRAGE levels in those three groups were significantly lower than the corresponding serum sRAGE levels (p <0.001).
Conclusion: Serum and seminal plasma sRAGE concentrations seem to show variations worth considering between fertile and infertile men. Moreover, further research is required to elucidate the role of the sRAGEs and oxidative stress in male infertility. HIPPOKRATIA 2017, 21(1): 19-24.
Keywords: Male infertility, soluble receptor of advanced glycation end-products, sRAGE, sperm analyses, advanced glycation end-products, AGEs, receptor of advanced glycation end-products, RAGE
Introduction
The World Health Organization (WHO) defines infertility as the inability to conceive a child after one year of regular, unprotected intercourse1. Approximately 50 % of cases of infertility can be related to male factors, exclusively or partially2. Semen analysis is a pivotal examination for the initial diagnostic approach of male infertility3.
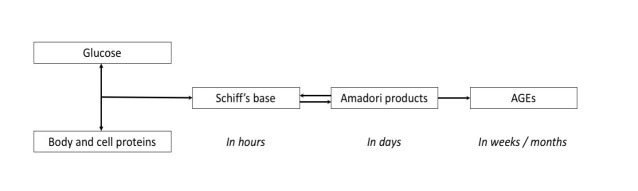
Advanced Glycation End-products (AGEs) are formed when a free carbonyl group of a carbohydrate binds to an amino group of a protein, lipid or nucleic acid in a non-enzymatic way (Maillard reaction)4. The result is the formation of a reversible Schiff base (aldimine), which in turn produces Amadori glycated proteins (Figure 1). The latter can be irreversibly rearranged into AGEs by a fast (days to weeks) or a slow (weeks to months) pathway5-7. Alternative pathways of AGE formation are the Namiki and Wolff pathways8. Best studied AGEs are Nε-carboxyethyl lysine (CEL), arginine pyrimidine, pentosidine, pyrraline, methylglyoxal (MG), glyoxal lysine, 3-deoxyglucosone (3-DG) and Nε-carboxymethyl lysine (CML)9. The contributing factors for AGE formation are the amount of proteins available for glycoxidation, the degree of hyperglycemia in terms of duration and pathological value, and the level of the oxidant stress in the environment. AGEs can also be formed in the process of normal aging due to cellular apoptosis10 or by leukocytes in semen even within WHO normal values11.
Figure 1. Formation of advanced glycation end products (AGEs).
The association of AGEs with diabetes mellitus (DM) is well established12,13. Formation of AGEs promotes activation of signaling pathways via cell surface receptors, the most common being the receptor for AGEs (RAGEs)14. AGE - RAGE interaction induces NADPH oxidase and production of reactive oxygen (ROS) and nitrogen species. This cascade results in further AGE formation, especially if the kidney function is impaired15, establishing a vicious circle16. Of particular interest are the soluble forms of RAGE (sRAGE): cRAGE (cleaved) and esRAGE (endogenous secretory) isoforms17 that act as a decoy to prevent the AGE-RAGE interaction18. The hyperglycemic environment in DM produces AGE-related mediators that may result in macro- and microvascular complications, such as diabetic retinopathy, cataract, atherosclerosis, nephropathy, neuropathy, embryopathy, and impaired wound healing13,19,20. Although AGEs have been examined in the field of female infertility, especially in polycystic ovary syndrome (PCOS)21and AGE-induced inflammation22, little is known about the possible association of AGEs and RAGEs with male infertility, in patients without diabetes23 or infection. It has been reported that AGEs inhibit testosterone production and secretion by Leydig cells by inducing the production of ROS. Such toxic activity may affect fertility24,25. The aim of the current study was to detect possible differences in serum and seminal sRAGEs concentrations in men with infertility in comparison with a fertile population.
Methods
Patient characteristics and clinical samples
Between October 2009 and May 2012, a total of 76 men were enrolled in this study from the outpatient unit of reproductive endocrinology of the First Department of Obstetrics and Gynecology of Papageorgiou General Hospital. Men from infertile couples aged 27-51 years (mean ± standard deviation: 36.1 ± 5.2) were divided into two groups with normal (NS, n =10) or abnormal (AS, n =53) semen parameters. The controls were fertile men aged 28-45 years (34.8 ± 4.6; n =12). One man from infertile couple was excluded from the statistical analysis as semen analysis couldn’t be conducted to his sample. Sixty-three out of seventy-five participants who were included in the statistical analysis, originated from infertile couples. Exclusion criteria for all groups were: i) infection with fever during the preceding three months and ii) use of antibiotics during the same period. Inclusion criteria for men of infertile couples were: i) not being able to conceive after 12 months of unprotected sexual intercourses1 and ii) willing to investigate their fertility status. Inclusion criteria for control men were: i) proven fertility (pregnant woman within the previous 12 months by spontaneous conception) and ii) normal semen parameters. All assessed men provided written consent. The study was approved by the Bioethics Committee of the Faculty of Medicine, Aristotle University of Thessaloniki, Greece (No 230, 27/08/2016).
Experimental procedures
Based on the standard semen analysis of the two samples they provided, each male participant from infertile couples was categorized into one of the following two groups: Normal semen (NS) men and abnormal semen (AS) men with at least one pathological parameter in the three basic categories of semen analysis, e.g., concentration, motility, and morphology. Medical history (personal history, family history, lifestyle, occupational and environmental hazards, substance abuse) was recorded, and physical examination (anthropometric parameters, examination of genitalia) was performed in all participants. Men from infertile couples were asked additional questions regarding the duration of their infertility, the existence or not of a previous pregnancy, the frequency of sexual intercourses, as well as the wife’s age. The coexistence of medical conditions that could affect male fertility status either directly or indirectly (urogenital infections, varicocele, cryptorchidism, mumps, thyroid, pituitary and adrenal diseases, chronic respiratory, kidney and liver diseases, cystic fibrosis, tuberculosis, neurological diseases, arterial hypertension, and medications) were considered. We also took into account the existence of DM in every participant as well as in his family medical history. Lifestyle, work conditions, and habits were thoroughly discussed (smoking, excessive consumption of alcohol, diet, physical fitness, exercise, adequate rest, stress, nature of work, excessive exposure to radiation, workplace and residence).
Semen samples were collected by masturbation after a period of sexual abstinence of three to four days. Liquefaction of each sample was achieved on a laboratory rotator for up to 1h at 37 oC. Once liquefaction was achieved, standard semen analysis was performed according to the WHO 2010 manual3 by the same microbiologist, who was specifically trained for this purpose. Semen analysis consisted of macroscopic analysis (liquefaction, volume, pH, viscosity), microscopic analysis (sperm concentration, motility, vitality) and preparation of stained Papanicolaou smears for evaluation of morphology and leukocyte concentration. All assessments were carried out in duplicates. Sperm and serum samples were kept and centrifuged in order to measure sRAGE. Also, blood sampling was performed to test for glycosylated hemoglobin, biochemical, and hormonal parameters.
Seminal plasma samples were separated by centrifugation at 1,000 g for 10 min and kept at -60oC, to be used for the assessment of sRAGE. sRAGE levels were also measured in blood serum of each participant. Both seminal and serum total sRAGE concentrations were determined by enzyme-linked immunosorbent assay (ELISA; R&D Systems, Minneapolis, MN, USA), in duplicate measurements. The reference range was 382 - 4,329 pg/ml (mean ± standard deviation: 1,655 ± 693 pg/ml) for the seminal plasma sRAGE and 368 - 4,354 pg/ml (1,794 ± 755 pg/ml) for the serum sRAGE. Inter-assay and intra-assay co-efficient of variations of the sRAGE ELISA were 8.3 % and 5.5 %, respectively. The minimum detectable dose (MDD) of human RAGE ranged from 1.23 - 16.14 pg/ml.
In every participant, glycosylated hemoglobin 1c (HbA1c) was measured by HA-8160 HPLC analyzer (Arkray Inc., Kyoto, Japan). Also, high-density lipoprotein (HDL)-cholesterol, low-density lipoprotein (LDL)-cholesterol, total cholesterol, and triglycerides were evaluated by Architect c16000 clinical chemistry photometric analyzer (Abbott, IL, USA). Additionally, hormonal profiles, including follicular stimulating hormone (FSH), luteinizing hormone (LH), prolactin, sex-hormone binding globulin (SHBG), thyroid stimulating hormone (TSH), and total testosterone were determined by Advia Centaur XP immunoassay system for multiple sample analyses (Siemens, Dublin, Ireland).
Statistical analysis
All data were analyzed with the Statistical Package for the Social Sciences (SPSS) for Windows, Version 17.0 (SPSS Inc., Chicago, IL, USA). Data are presented as percentages for categorical variables and mean and standard deviation for continuous variables. Differences in categorical and continuous variables between groups were assessed with the chi-square test and the independent samples t-test, respectively. In all cases, a two-tailed p <0.05 was considered significant.
Results
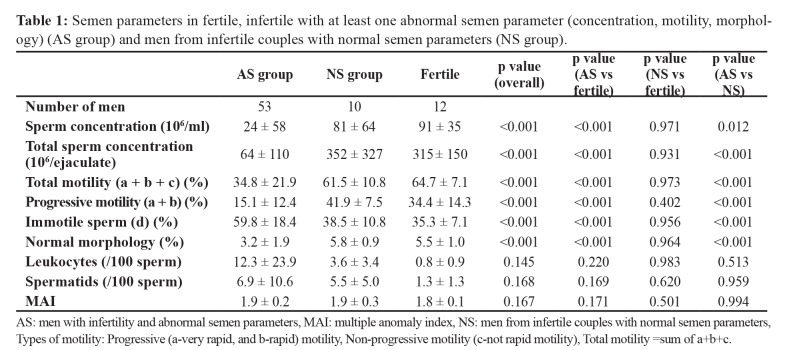
There were no differences between fertile and infertile AS men regarding clinical history, family history of diabetes, smoking status, diet habits, exercise habits, accompanying diseases or exposure to radiation, or other occupational hazards. As expected, there were significant differences between infertile AS and fertile groups, in the majority of semen parameters (Table 1; p <0.001). Further classification of the type of infertility according to semen parameters depicts the presence of pathological morphology mostly combined with another pathological semen parameter (Table 2).
Table 1. Semen parameters in fertile, infertile with at least one abnormal semen parameter (concentration, motility, morphology) (AS group) and men from infertile couples with normal semen parameters (NS group).
AS: men with infertility and abnormal semen parameters, MAI: multiple anomaly index, NS: men from infertile couples with normal semen parameters, Types of motility: Progressive (a-very rapid, and b-rapid) motility, Non-progressive motility (c-not rapid motility), Total motility =sum of a+b+c.
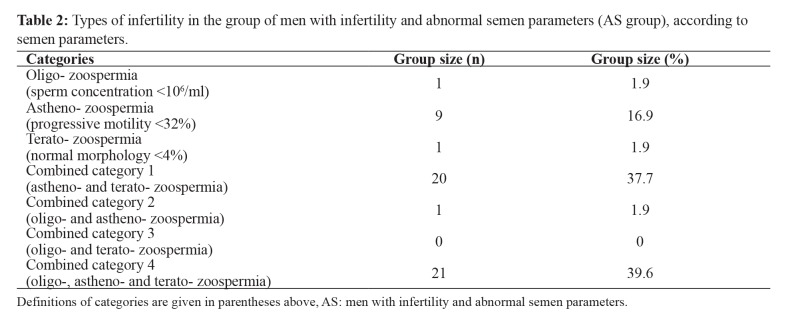
Table 2. Types of infertility in the group of men with infertility and abnormal semen parameters (AS group), according to semen parameters.
Definitions of categories are given in parentheses above, AS: men with infertility and abnormal semen parameters.
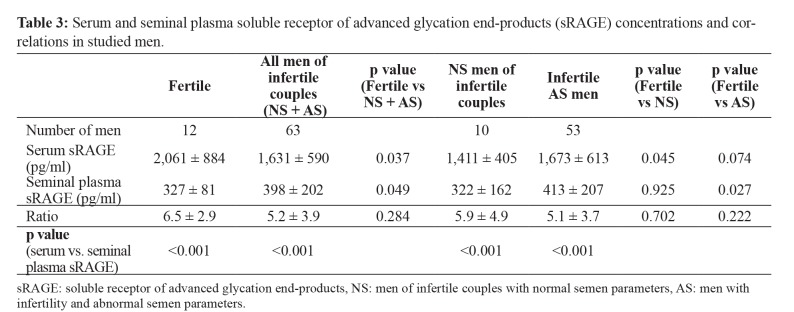
Serum sRAGE concentrations were higher in fertile men as opposed to the overall group of men from infertile couples (AS + NS) (Table 3). Seminal plasma sRAGE concentrations in fertile men were similar to those of NS men from infertile couples but lower than those of infertile AS men. In all groups of studied men (fertile, NS, AS), serum concentrations of sRAGE were significantly higher compared to seminal plasma sRAGE (Table 3; p <0.001). Seminal sRAGE concentrations were negatively correlated with HbA1c with marginal significance (r =-0.265, p =0.053). No other correlation was detected between serum or seminal sRAGE concentrations and any other hormonal, metabolic or seminal parameters (Table 4).
Table 3. Serum and seminal plasma soluble receptor of advanced glycation end-products (sRAGE) concentrations and correlations in studied men.
sRAGE: soluble receptor of advanced glycation end-products, NS: men of infertile couples with normal semen parameters, AS: men with infertility and abnormal semen parameters.
Table 4. Correlation among soluble receptor of advanced glycation end-products (sRAGE) concentrations in serum and seminal plasma and main hormonal, metabolic and seminal parameters in all studied men (n =75).
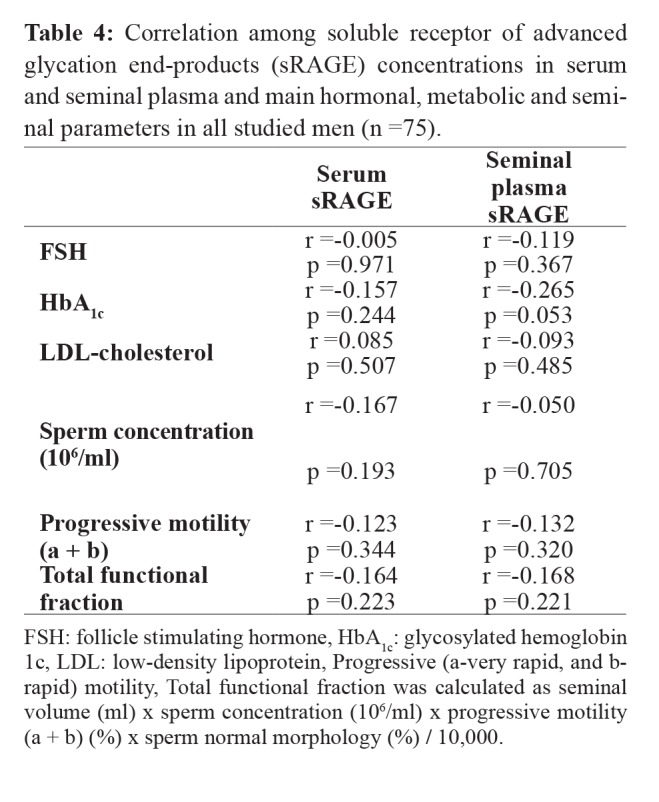
FSH: follicle stimulating hormone, HbA1c: glycosylated hemoglobin 1c, LDL: low-density lipoprotein, Progressive (a-very rapid, and brapid) motility, Total functional fraction was calculated as seminal volume (ml) x sperm concentration (106/ml) x progressive motility (a + b) (%) x sperm normal morphology (%) / 10,000.
Discussion
The main purpose of this study was to detect possible differences in seminal plasma and/or serum sRAGEs concentrations in infertile men as compared to fertile men population. In particular, we measured the sRAGE levels in men who were either normozoospermic or had abnormalities in parameters of their sperm analysis. Although there is a plethora of studies in the literature on soluble sRAGE measurements with ELISA, the source of clinical samples in those studies were either blood serum alone or seminal plasma whereas their study population was only men with DM26,27. As sRAGE products are widely expressed in various organs including male genital tract and spermatozoa, in an attempt to gain additional information on the multifaceted roles of sRAGE we investigated the probable relation of sRAGE to non-diabetic infertile individuals.
sRAGE is the secretory splice isoform of RAGE, and its concentration is proportional to the RAGE concentration found in biological fluids28. Mallidis et al localized AGE and RAGE in the male genital tract (testis and epididymis) and showed that the local production of AGEs/RAGEs in seminal plasma is possibly related to normal or pathologic causes29. Due to the role of sRAGE as a decoy to prevent the AGE-RAGE interaction18, quantitative measurement of sRAGE has been associated with a variety of clinical applications as a marker in several RAGE-mediated disorders. Clinical studies have evaluated the importance of sRAGE as a biomarker linked to diseases mostly associated with DM, such as coronary artery disease, rheumatoid arthritis, Alzheimer’s disease and hypertension. But sRAGE is also associated with other conditions, such as extreme longevity, end-stage renal disease, and acute lung injury28. Also, sRAGE has been correlated with the success of therapeutic pharmacological responses on a number of diseases30.
In this research study, we found significantly higher concentrations of serum sRAGE in fertile as opposed to AS men and NS men from infertile couples and that all participants had sRAGE levels that were significantly higher than those in seminal plasma. In contrast, we found comparable sRAGE levels in the seminal plasma of all participants. To our knowledge, only Oborna et al, measured sRAGE concentrations in serum and seminal plasma with ELISA, but only in men with normal semen parameters, without providing information on their diabetic status23. Their results are in accordance with ours regarding higher concentrations of serum sRAGE in all men compared to their seminal plasma ones. We came down to four possible explanations. First, the presence of high mitochondrial concentrations in the spermatozoa may produce increased amounts of ROS, eventually leading to high amounts of sRAGE. Second, the oxidative stress, produced even by normal counts of leukocytes, constitutes an additional source of increased sRAGE levels31. Third, the increased clearance of AGE ligands/sRAGE complexes, caused by the number of barriers that exist in the male genital system, may result in lower levels of sRAGE in seminal plasma. Fourth, the 100-fold higher concentration of testosterone in seminal plasma, as a consequence of blood-testis barrier could result in lower levels of sRAGE32.
The lower serum sRAGE levels and the decreased ratio of sRAGE to AGE in early pregnancy have been associated with the subsequent development of preeclampsia in women with type I DM33. This finding generated the question in our study whether the sRAGE levels could be attributed to the development of preeclampsia or the existence of diabetes mellitus. Moreover, insulin resistance has been associated with hypercoagulative and proinflammatory status34. From this point of view, not having diabetic participants was an advantage in our study since increased sRAGE levels could be attributed either to diabetes or a counterbalancing mechanism. In our case, sRAGE levels can only be attributed to the fertility status of the male participant.
Nevertheless, there are specific limitations to this pilot study. Inability to reach statistical significance in the negative correlation of seminal sRAGE with HbA1c may be due to the fact that our study was underpowered to detect such difference. Additionally, the use of biomarkers specific for lipid peroxidation and sperm DNA fragmentation would provide a broader vision of the oxidative stress status and its effect on sperm DNA. The fertility status of the female partner of the infertile couple was not evaluated as it would not affect the degree of men infertility. Nevertheless, it would provide most complete medical history on the reproductive capacity of the couple.
Conclusion
Serum and seminal sRAGE concentrations have distinct differences between fertile and infertile men. The results of this study have provided information that may formulate hypotheses of possible biochemical links and paths explaining the reason they have emerged. However, further research is required to elucidate the role of the sRAGEs and oxidative stress in male infertility.
Conflict of interest
None of the authors declared conflict of interest.
Acknowledgement
The authors would like to warmly thank all men who participated in this study.
References
- 1.World Health Organization History taking. Rowe JP, Comhaire HF, Hargreave BT, Mahmoud MAA (eds). World Health Organization. WHO Manual for the Standarized Investigation, Diagnosis and Management of the Infertile Male. 1st edition, Cambridge University Press, Cambridge. 2000:5–16. [Google Scholar]
- 2.McClure N, Mallidis C. Male infertility, a clinical reflection. Expert Rev Obs Gynecol. 2007;2:825–832. [Google Scholar]
- 3.World Health Organization , Department of Reproductive Health and Research Semen analysis. Cooper GT, Aitken J, Auger J, Baker G, Barratt LRC, Behre MH, et al (eds). WHO Laboratory Manual for the Examination and Processing of human semen. 5th edition, UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in HRP, WHO Department of RHR, Geneva. 2010:7–114. [Google Scholar]
- 4.John WG, Lamb EJ. The Maillard or browning reaction in diabetes. Eye. 1993;7:230–237. doi: 10.1038/eye.1993.55. [DOI] [PubMed] [Google Scholar]
- 5.Dyer DG, Dunn JA, Thorpe SR, Lyons TJ, McCance DR, Baynes JW. Accumulation of Maillard reaction products in skin collagen in diabetes and aging. Ann N Y Acad Sci. 1992;663:421–422. doi: 10.1111/j.1749-6632.1992.tb38687.x. [DOI] [PubMed] [Google Scholar]
- 6.Bierhaus A, Hofmann M, Ziegler R, Nawroth P. AGEs and their interaction with AGE-receptors in vascular disease and diabetes mellitus. I. The AGE concept. Cardiovasc Res. 1998;37:586–600. doi: 10.1016/s0008-6363(97)00233-2. [DOI] [PubMed] [Google Scholar]
- 7.Shaw SM, Crabbe MJ. Monitoring the progress of non-enzymatic glycation in vitro. Int J Pept Protein Res. 1994;44:594–602. doi: 10.1111/j.1399-3011.1994.tb01149.x. [DOI] [PubMed] [Google Scholar]
- 8.Ferreira AE, Ponces Freire AM, Voit EO. A quantitative model of the generation of N (epsilon)-(carboxymethyl)lysine in the Maillard reaction between collagen and glucose. Biochem J. 2003;376:109–121. doi: 10.1042/BJ20030496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monnier VM, Sell DR, Genuth S. Glycation products as markers and predictors of the progression of diabetic complications. Ann N Y Acad Sci. 2005;1043:567–581. doi: 10.1196/annals.1333.065. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal A, Said TM. Oxidative stress, DNA damage and apoptosis in male infertility: a clinical approach. BJU Int. 2005;95:503–507. doi: 10.1111/j.1464-410X.2005.05328.x. [DOI] [PubMed] [Google Scholar]
- 11.Sharma RK, Pasqualotto AE, Nelson DR, Thomas AJ Jr, Agarwal A. Relationship between seminal white blood cell counts and oxidative stress in men treated at an infertility clinic. J Androl. 2001;22:575–583. [PubMed] [Google Scholar]
- 12.Giardino I, Edelstein D, Brownlee M. Nonenzymatic glycosylation in vitro and in bovine endothelial cells alters basic fibroblast growth factor activity. A model for intracellular glycosylation in diabetes. J Clin Invest. 1994;94:110–117. doi: 10.1172/JCI117296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed N. Advanced glycation endproducts--role in pathology of diabetic complications. Diabetes Res Clin Pract. 2005;67:3–21. doi: 10.1016/j.diabres.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Matsumoto S, Yoshida T, Murata H, Harada S, Fujita N, Nakamura S, et al. Solution structure of the variable-type domain of the receptor for advanced glycation end products: new insight into AGE-RAGE interaction. Biochemistry. 2008;47:12299–12311. doi: 10.1021/bi800910v. [DOI] [PubMed] [Google Scholar]
- 15.Wong A, Dukic-Stefanovic S, Gasic-Milenkovic J, Schinzel R, Wiesinger H, Riederer P, et al. Anti-inflammatory antioxidants attenuate the expression of inducible nitric oxide synthase mediated by advanced glycation endproducts in murine microglia. Eur J Neurosci. 2001;14:1961–1967. doi: 10.1046/j.0953-816x.2001.01820.x. [DOI] [PubMed] [Google Scholar]
- 16.Basta G, Lazzerini G, Del Turco S, Ratto GM, Schmidt AM, De Caterina R. At least 2 distinct pathways generating reactive oxygen species mediate vascular cell adhesion molecule-1 induction by advanced glycation end products. Arterioscler Thromb Vasc Biol. 2005;25:1401–1407. doi: 10.1161/01.ATV.0000167522.48370.5e. [DOI] [PubMed] [Google Scholar]
- 17.Vazzana N, Santilli F, Cuccurullo C, Davì G. Soluble forms of RAGE in internal medicine. Intern Emerg Med. 2009;4:389–401. doi: 10.1007/s11739-009-0300-1. [DOI] [PubMed] [Google Scholar]
- 18.Bierhaus A, Humpert PM, Morcos M, Wendt T, Chavakis T, Arnold B, et al. Understanding RAGE, the receptor for advanced glycation end products. J Mol Med (Berl) 2005;83:876–886. doi: 10.1007/s00109-005-0688-7. [DOI] [PubMed] [Google Scholar]
- 19.Hogan M, Cerami A, Bucala R. Advanced glycosylation endproducts block the antiproliferative effect of nitric oxide. Role in the vascular and renal complications of diabetes mellitus. J Clin Invest. 1992;90:1110–1115. doi: 10.1172/JCI115928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yamagishi S. Advanced glycation end products and receptor-oxidative stress system in diabetic vascular complications. Ther Apher Dial. 2009;13:534–539. doi: 10.1111/j.1744-9987.2009.00775.x. [DOI] [PubMed] [Google Scholar]
- 21.Merhi Z. Advanced glycation end products and their relevance in female reproduction. Hum Reprod. 2014;29:135–145. doi: 10.1093/humrep/det383. [DOI] [PubMed] [Google Scholar]
- 22.Irani M, Minkoff H, Seifer DB, Merhi Z. Vitamin D increases serum levels of the soluble receptor for advanced glycation end products in women with PCOS. J Clin Endocrinol Metab. 2014;99:E886–E890. doi: 10.1210/jc.2013-4374. [DOI] [PubMed] [Google Scholar]
- 23.Oborna I, Malickova K, Fingerova H, Brezinova J, Horka P, Novotny J, et al. A randomized controlled trial of lycopene treatment on soluble receptor for advanced glycation end products in seminal and blood plasma of normospermic men. Am J Reprod Immunol. 2011;66:179–184. doi: 10.1111/j.1600-0897.2011.00984.x. [DOI] [PubMed] [Google Scholar]
- 24.Zhao YT, Qi YW, Hu CY, Chen SH, Liu Y. Advanced glycation end products inhibit testosterone secretion by rat Leydig cells by inducing oxidative stress and endoplasmic reticulum stress. Int J Mol Med. 2016;38:659–665. doi: 10.3892/ijmm.2016.2645. [DOI] [PubMed] [Google Scholar]
- 25.Chen Y, Wu Y, Gan X, Liu K, Lv X, Shen H, et al. Iridoid glycoside from Cornus officinalis ameliorated diabetes mellitus-induced testicular damage in male rats: Involvement of suppression of the AGEs/RAGE/p38 MAPK signaling pathway. J Ethnopharmacol. 2016;194:850–860. doi: 10.1016/j.jep.2016.10.079. [DOI] [PubMed] [Google Scholar]
- 26.Tan KC, Shiu SW, Chow WS, Leng L, Bucala R, Betteridge DJ. Association between serum levels of soluble receptor for advanced glycation end products and circulating advanced glycation end products in type 2 diabetes. Diabetologia. 2006;49:2756–2762. doi: 10.1007/s00125-006-0394-1. [DOI] [PubMed] [Google Scholar]
- 27.Koutroumani N, Partsalaki I, Lamari F, Dettoraki A, Gil AP, Karvela A, et al. Protective mechanisms against oxidative stress and angiopathy in young patients with diabetes type 1 (DM1) J Pediatr Endocrinol Metab. 2013;26:309–317. doi: 10.1515/jpem-2012-0183. [DOI] [PubMed] [Google Scholar]
- 28.Geroldi D, Falcone C, Emanuele E. Soluble receptor for advanced glycation end products: from disease marker to potential therapeutic target. Curr Med Chem. 2006;13:1971–1978. doi: 10.2174/092986706777585013. [DOI] [PubMed] [Google Scholar]
- 29.Mallidis C, Agbaje I, Rogers D, Glenn J, McCullough S, Atkinson AB, et al. Distribution of the receptor for advanced glycation end products in the human male reproductive tract: prevalence in men with diabetes mellitus. Hum Reprod. 2007;22:2169–2177. doi: 10.1093/humrep/dem156. [DOI] [PubMed] [Google Scholar]
- 30.Yan SF, Ramasamy R, Schmidt AM. Soluble RAGE: therapy and biomarker in unraveling the RAGE axis in chronic disease and aging. Biochem Pharmacol. 2010;79:1379–1386. doi: 10.1016/j.bcp.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril. 2003;79:829–843. doi: 10.1016/s0015-0282(02)04948-8. [DOI] [PubMed] [Google Scholar]
- 32.Meng J, Holdcraft RW, Shima JE, Griswold MD, Braun RE. Androgens regulate the permeability of the blood-testis barrier. Proc Natl Acad Sci U S A. 2005;102:16696–16700. doi: 10.1073/pnas.0506084102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu Y, Hanssen KF, Kalyanaraman V, Chirindel A, Jenkins AJ, Nankervis AJ, et al. Reduced soluble receptor for advanced glycation end-products (sRAGE) scavenger capacity precedes pre-eclampsia in Type 1 diabetes. BJOG. 2012;119:1512–1520. doi: 10.1111/j.1471-0528.2012.03463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ota K, Yamagishi S, Kim M, Dambaeva S, Gilman-Sachs A, Beaman K, et al. Elevation of soluble form of receptor for advanced glycation end products (sRAGE) in recurrent pregnancy losses (RPL): possible participation of RAGE in RPL. Fertil Steril. 2014;102:782–789. doi: 10.1016/j.fertnstert.2014.06.010. [DOI] [PubMed] [Google Scholar]