ABSTRACT
To determine intraabdominal pressure (IAP) in women during CrossFit and to determine whether parity, age, or CrossFit experience affects IAP during CrossFit exercises, we evaluated 10 women: 5 experienced and active CrossFitters and 5 who were not regularly engaged in CrossFit. A Laborie urodynamics abdominal pressure probe with the Goby wireless system measured IAP during 10 repetitions of 13 different CrossFit exercises. Women had a mean age of 36 years. A significant difference was found between mean peak IAP of the 5 parous vs the 5 nulliparous women (P = 0.009). Experience with CrossFit did not affect mean peak IAP achieved with exercise. In some exercises, there was a significant change in IAP as participants progressed through repetitions (P = 0.003 for back squats and 0.04 for sit-ups). Participants achieved IAP values that were markedly higher than those previously published.
KEYWORDS: CrossFit, exercise, intraabdominal pressure, pelvic floor dysfunction
CrossFit has been shown to improve cardiovascular function and body composition,1 as well as meet recommended goals for cardiovascular activity for adults, but it is unclear what effects this type of activity has on the pelvic floor. Several studies have explored how exercise affects the location and function of the pelvic organs through imaging and questionnaires, yet results are inconsistent.2-5 This study sought to quantify peak intraabdominal pressure (IAP) in women performing CrossFit exercises. Additionally, it attempted to determine whether participants' parity, age, or prior experience with CrossFit affected IAP. Such information is important, because expert consensus suggests that long-term, elevated IAP predisposes women to pelvic floor dysfunction (PFD). A 2016 study estimated that 24% of women experience some PFD, and that number appears to be an underestimate, because asymptomatic women have demonstrated aspects of PFD such as pelvic organ prolapse on imaging.2,6-9 PFD impacts quality of life and is expensive to treat: urinary incontinence alone is estimated to have a direct cost of $12.4 billion annually in the United States.10 To our knowledge, this is the first attempt to quantify the pelvic pressures experienced during common CrossFit exercise movements.
METHODS
This observational, cross-sectional pilot study was approved by the Baylor Scott & White institutional review board. Informed consent was obtained prior to participation. Because this was a pilot study, no a priori power analysis was performed. Two cohorts of women were studied: 5 women who regularly participated in CrossFit classes and 5 who did not. Regular participation was defined as engaging in at least two CrossFit workouts per week for the last 6 months. Women in the non-CrossFit group had not participated in CrossFit workouts for at least a year. Women were recruited by word of mouth; no patients were recruited from a medical office. All women were physically active and able to engage in high-intensity exercise training. Exclusion criteria included age <18 years, known current or past history of pelvic organ prolapse diagnosis, diagnosed collagen disease, medical comorbidities that precluded performance of study exercises, current pregnancy, or pregnancy within the last 6 months as reported by participants.
Participants were fitted with a validated, air-filled IAP catheter of the Goby Laborie wireless system (Laborie Medical Technologies, Mississauga, ON, Canada) (Figure 1) that was placed vaginally. The Goby Laborie system has an acquisition frequency of 10 Hz, meaning that pressure measurements are taken 10 times per second. The catheter was taped to the labia majora to minimize migration. The Goby wireless system was strapped to the thigh. At rest, the pressure catheter was zeroed while standing. Women then engaged in an individual, simulated CrossFit class at the CrossFit gym with an instructor present. The simulated class included the same exercises for all participants, with the exception of double-unders, which some women were unable to perform. The exercises performed were back squats, burpees, deadlifts, front squats, kettlebell swings, lunges, pull-ups, push-ups, sit-ups, air squats, thrusters, wall balls, and jump rope with “double-unders,” if possible. The simulated class consisted of 10 repetitions of the exercises at a weight that the participant chose, based on her typical activity or what she felt she could perform. Visual example exercises can be found at the links provided in the references. Push-ups were performed from the knees if participants were unable to perform them from the toes. Pull-ups were performed with supportive bands when necessary.
Figure 1.
The Goby Laborie wireless system.
The participants' IAPs were measured and recorded continuously during exercises on Laborie Urodynamics Software. All IAP tracings were reviewed, and the maximal pressure generated during each repetition of the 13 exercises was measured with the software and recorded for analysis. The highest pressure generated in each repetition was used to calculate the mean and median maximal IAPs for the series of repetitions of each exercise within each subject. The means and medians for each exercise within subjects were highly correlated (P < 0.0001 with R2 of 0.995), so the mean maximal IAP was used for analysis. Data were analyzed using Statistica (Statsoft, Tulsa, OK) and included analysis of variance with repeated measures within subjects. Levene's test for homogeneity was used to test variance terms. P < 0.05 was accepted as significant.
RESULTS
Ten women were enrolled in the study, with a mean age of 36 years and a range of 26 to 48 years. Half of the women were parous. There was no difference in mean peak IAP when accounting for age.
There was a statistically significant difference in the mean peak pressures of the different exercises (P < 0.0001), as displayed in (Figure 2a). The highest IAPs were generated during double-unders, push-ups, front squats, and wall balls. The difference between the mean peak pressures of parous vs nulliparous women was statistically significant, as noted in (Figure 2a) (P = 0.009). The difference was not uniform: parous women achieved higher IAP with pushups, whereas nulliparous women achieved higher IAP when performing jump rope, thrusters, and wall balls. When comparing women who were regular CrossFit participants with those who were not, there was no difference in mean peak IAP achieved with each exercise, as shown in (Figure 2b).
Figure 2.
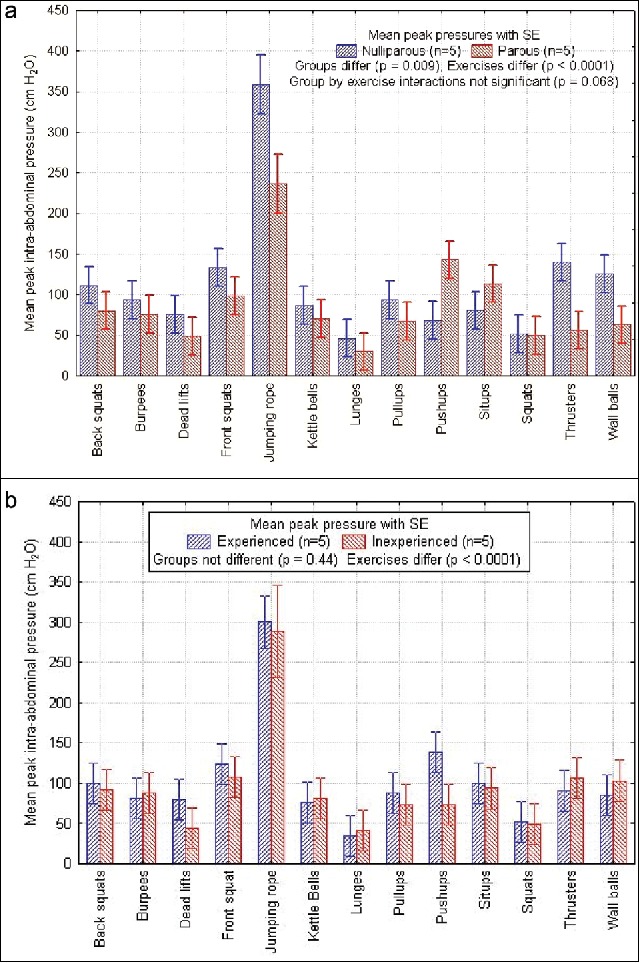
(a) Histogram of mean peak intraabdominal pressure (IAP) differentiated by type of CrossFit exercise and parity. There was a statistically significant difference between mean IAP generated by parous and nonparous women (P = 0.009). This was especially apparent for jump rope, push-ups, thrusters, and wall balls. (b) Histogram of mean peak IAP differentiated by type of CrossFit exercise and experience with CrossFit. The statistically significant difference between exercises was again demonstrated (P ≤ 0.0001), yet there was no statistically significant difference between the pressures generated by women with or without CrossFit experience (P = 0.44).
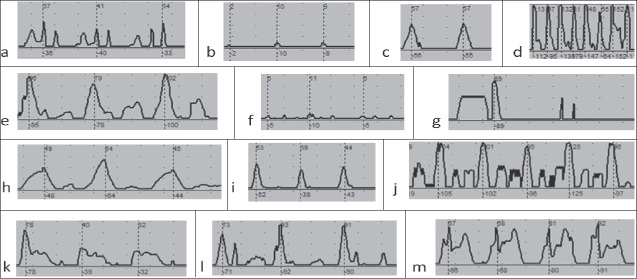
The pressure curve for each exercise was unique, with some exercises having unimodal or multimodal pressure curves (Figure 3). These pressure curve shapes were characteristic for each exercise and were consistent across participants (Figure 4).
Figure 3.
Intraabdominal pressure tracings are markedly different for different CrossFit exercises: (a) wall ball, (b) deadlift, (c) back squat, (d) double-under, (e) front squat, (f) kettlebell, (g) burpee, (h) lunge, (i) squat, (j) push-up, (k) sit-up, (l) thruster, and (m) pull-up. Maximal pressure measurements can be seen at the dotted line; the value is in centimeters of water.
Figure 4.
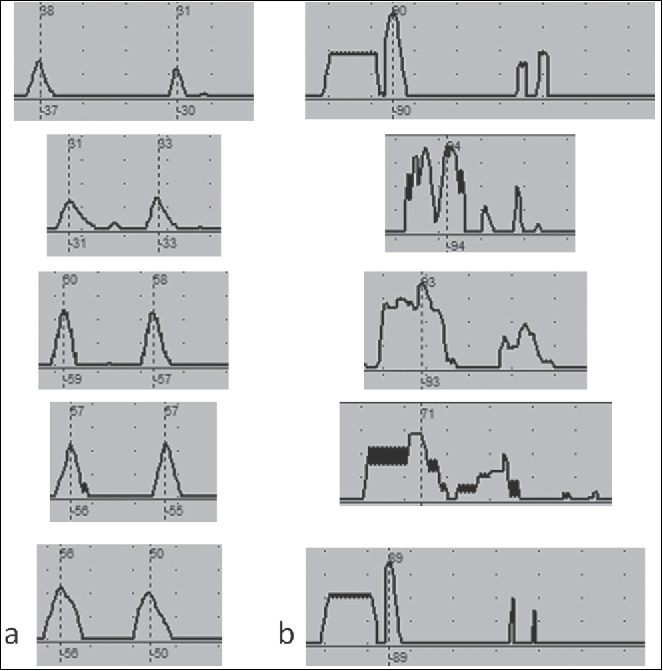
Intraabdominal pressure tracing shape is recognizable and characteristic across participants. These examples of characteristic pressure tracings were collected during (a) back squats and (b) burpees. Maximal pressure measurements can be seen at the dotted line; the value is above in centimeters of water.
Some exercises required the use of additional weight in the form of a wall ball, kettlebell, or weight bar. When comparing exercises that were body weight only to those that required the use of additional weight, there was no statistically significant difference.
As participants continued through the repetitions of a single exercise, there was a statistically significant change in the pressure generated at times. For example, among participants performing back squats, there was a statistically significant increase in IAP as they progressed through repetitions (P = 0.003). Yet, among those performing sit-ups, there was a trend of decreasing pressures through the repetitions that was also statistically significant (P = 0.04).
DISCUSSION
We report for the first time IAP generated during CrossFit exercises. We have successfully confirmed that even within one high-intensity exercise regimen, the maximum IAPs, duration of increased IAP, and shape of the pressure curve differed greatly by exercise.
This study's strengths include the incorporation of exercises from an increasingly popular exercise program. Additionally, this is the first study of its type in the CrossFit population. All IAPs were measured using a common validated tool. Another positive aspect is the presence of a certified CrossFit trainer, ensuring minimal variability in form for each activity. Study limitations include small sample, patient-selected weight, variable exercise time, and the inability to assess the impact or lack thereof of exercise order on IAP. We were unable to control for participants' level of effort and fatigue. Though none of the women in the study had severe obesity, body mass index was not formally assessed, which was another limitation. Body mass index has been shown to have a weak correlation with IAP during some activities in prior studies.11
The data revealed an expected difference in maximal IAP and shape of the IAP pressure curve between different exercises. A previous article by Shaw et al outlined the difference in maximal IAP and shapes of IAP curves during exercises, such as jumping and sit-ups.12 It is still unclear what is more concerning in terms of stress to the pelvic floor: maximal pressure or duration of pressure that could perhaps be measured as area under the curve.
The IAP generated by participants was higher than expected in some exercises, especially when performing double-unders: one participant generated a mean IAP of 429 cm H2O; all participants generated mean IAP > 200 cm H2O. This IAP is higher than values previously reported during exercises, as seen in Table 1.12-15 Our data show that IAPs have variable trends, increasing through repetitions in some exercises and decreasing in others. It is possible that changes in breathing, overall fatigue, or fatigue of the focused muscle groups could contribute to this variation. Breathing or breath control has been shown to affect IAP during lifting; however, we were unable to control for this across subjects.16
Table 1.
Published intraabdominal pressures
| Maximal intra-abdominal pressures (range) (cm H2O) |
||||
|---|---|---|---|---|
| Variable | Shaw et al12 | Coleman et al13 | Coleman et al14 | Weir et al15 |
| Median or mean value | Median | Mean | Mean | Mean |
| Cough | 91 (34–200) | 81–149a | ||
| Walk | 25 (15–37) | 51 (22–89) | 147 | |
| Run | 67 (32–99) | |||
| Lift [weight] | 49 (14–120) [18 kg] | 88 (62–133) [13.6 kg] | 149 [16 kg] | |
| Seated shoulder press [weight] | 19 (10–37) [9.1 kg] | |||
| Full sit-ups/roll-ups | 60 (14–129) | 50–51 (29–77) | ||
| Push-ups from knees | 15 (4–43) | |||
| Jumping | 91 (26–154) | 127 | ||
Small, medium, and forceful cough included.
Other studies have assessed IAP during Pilates exercises17 and found that IAPs generated during Pilates were generally less than those generated by a simple sit-to-stand exercise encountered during daily activity. The benefits of Pilates include improved dynamic balance,18 increased abdominal and upper body endurance, improved postural alignment,19 and improved pelvic floor strength.20 Yet Pilates does not meet the guidelines of the Centers for Disease Control and Prevention for decreasing the leading cause of mortality in the United States—cardiovascular disease: “150 minutes of moderate physical activity or 75 minutes of intense physical activity each week; muscle-strengthening activities (such as lifting weights) … that are moderate or high intensity and involve all major muscle groups on 2 or more days a week.”21 High-intensity exercise programs, such as CrossFit, meet these guidelines and have been proven to increase overall aerobic fitness and improve body composition.12
Parous women generated statistically different IAPs compared to their nulliparous counterparts in certain exercises. Though one may presume that prior pregnancy could change the muscle tone or function of the abdominal wall and/or pelvic floor during exercise, the etiology of these differences was beyond the scope of this study.
Our study showed variable IAPs generated during CrossFit and opens the door for research on high-intensity exercise regimens with a focus on the pelvic floor. Potential research includes better definition of how exercise form, fatigue, or breathing affects IAP. Additionally, women who have been long-term, active participants of high-intensity workout regimens could be assessed for PFD. Though the general consensus is that increased pressure on the pelvic floor results in long-term morbidity, this connection has yet to be proven. Even more ambiguous are the long-term effects of exercise that increase pressure on the pelvic floor. Only one study linked strenuous physical activity during adolescence to stress urinary incontinence as an adult,4 yet that study used standardized questionnaires to assess prior activity, which could introduce powerful recall bias.
Given the clear benefits of high-intensity exercise in protecting women against the number one cause of death in the United States, it is too early to discourage women from engaging in high-intensity exercise, such as CrossFit. This research is the first step toward understanding how CrossFit's high-intensity exercise regimen affects the pelvic floor. More research is needed to explore the long-term effects of high-intensity exercise on the pelvic floor, cardiovascular health, quality of life, and life expectancy.
Funding Statement
Dr. Kuehl reports funding from the Anderly Research Endowment and the Noble Centennial Endowed Chair for Research in Obstetrics and Gynecology. All other authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Sally and Damon Phillips and the staff and athletes of CrossFit DSP; Chandler Carroll for manuscript support; and Eric McLaughlin for Laborie photo.
References
- 1.Smith MM, Sommer AJ, Starkoff BE, et al.. CrossFit-based high-intensity power training improves maximal aerobic fitness and body composition. J Strength Cond Res. 2013;27:3159–3172. doi: 10.1519/JSC.0b013e318289e59f. PMID:23439334. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Mias NL, Martinez-Franco E, Aguado J, et al.. Pelvic organ prolapse and stress urinary incontinence, do they share the same risk factors? Eur J Obstet Gynecol Reprod Biol. 2015;190:52–57. doi: 10.1016/j.ejogrb.2015.04.015. PMID:25984809. [DOI] [PubMed] [Google Scholar]
- 3.Middlekauff ML, Egger MJ, Nygaard IE, et al.. The impact of acute and chronic strenuous exercise on pelvic floor muscle strength and support in nulliparous healthy women. Am J Obstet Gynecol. 2016;215:316. e1-e7. doi: 10.1016/j.ajog.2016.02.031. PMID:26899909. [DOI] [PubMed] [Google Scholar]
- 4.Nygaard IE, Shaw JM, Bardsley T, et al.. Lifetime physical activity and female stress urinary incontinence. Am J Obstet Gynecol. 2015;213:e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Almeida MB, Barra AA, Saltiel F, et al.. Urinary incontinence and other pelvic floor dysfunctions in female athletes in Brazil: a cross-sectional study. Scand J Med Sci Sports. 2015;26:1109–1116. doi: 10.1111/sms.12546. PMID:26369504. [DOI] [PubMed] [Google Scholar]
- 6.Anderson KM, Davis K, Flynn BJ. Urinary incontinence and pelvic organ prolapse. Med Clin North Am. 2015;99:405–416. doi: 10.1016/j.mcna.2014.11.011. PMID:25700591. [DOI] [PubMed] [Google Scholar]
- 7.Hallock JL, Handa VL. The epidemiology of pelvic floor disorders and childbirth: an update. Obstet Gynecol Clin North Am. 2016;43:1–13. doi: 10.1016/j.ogc.2015.10.008. PMID:26880504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Johnson B, Li F, et al.. The effect of body mass index on pelvic floor support 1 year postpartum. Reprod Sci. 2016;23:234–238. doi: 10.1177/1933719115602769. PMID:26494698. [DOI] [PubMed] [Google Scholar]
- 9.Cimsit C, Yoldemir T, Akpinar IN. Prevalence of dynamic magnetic resonance imaging–identified pelvic organ prolapse in pre- and postmenopausal women without clinically evident pelvic organ descent. Acta Radiol. 2016;57:1418–1424. doi: 10.1177/0284185115589123. PMID:26041768. [DOI] [PubMed] [Google Scholar]
- 10.Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001;98:398–406. PMID:11530119. [DOI] [PubMed] [Google Scholar]
- 11.Levine B, Kaplanek B, Jaffe WL. Pilates training for use in rehabilitation after total hip and knee arthroplasty: a preliminary report. Clin Orthop Relat Res. 2009;467:1468–1475. doi: 10.1007/s11999-009-0779-9. PMID:19283437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaw JM, Hamad NM, Coleman TJ, et al.. Intra-abdominal pressures during activity in women using an intra-vaginal pressure transducer. J Sports Sci. 2014;32:1176–1185. doi: 10.1080/02640414.2014.889845. PMID:24575741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coleman TJ, Hamad NM, Shaw JM, et al.. Effects of walking speeds and carrying techniques on intra-abdominal pressure in women. Int Urogynecol J. 2015;26:967–974. doi: 10.1007/s00192-014-2593-5. PMID:25527480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coleman TJ, Nygaard IE, Holder DN, Egger MJ, Hitchcock R. Intra-abdominal pressure during Pilates: unlikely to cause pelvic floor harm. Int Urogynecol J. 2015;26:1123–1130. doi: 10.1007/s00192-015-2638-4. PMID:25672647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weir LF, Nygaard IE, Wilken J, Brandt D, Janz KF. Postoperative activity restrictions: any evidence? Obstet Gynecol. 2006;107(Pt 1):305–309. doi: 10.1097/01.AOG.0000197069.57873.d6. PMID:16449116. [DOI] [PubMed] [Google Scholar]
- 16.Cozen DM. Use of Pilates in foot and ankle rehabilitation. Sports Med Arthrosc Rev. 2000;8:395–403. doi: 10.1097/00132585-200008040-00011. [DOI] [Google Scholar]
- 17.Bryan M, Hawson S. The benefits of Pilates exercise in orthopaedic rehabilitation. Tech Orthop. 2003;18:126–129. doi: 10.1097/00013611-200303000-00018. [DOI] [Google Scholar]
- 18.Johnson EG, Larsen A, Ozawa H, et al.. The effects of Pilates-based exercise on dynamic balance in healthy adults. J Bodyw Mov Ther. 2007;11:238–242. doi: 10.1016/j.jbmt.2006.08.008. [DOI] [Google Scholar]
- 19.Kloubec JA. Pilates for improvement of muscle endurance, flexibility, balance, and posture. J Strength Cond Res. 2010;24:661–667. doi: 10.1519/JSC.0b013e3181c277a6. PMID:20145572. [DOI] [PubMed] [Google Scholar]
- 20.Culligan PJ, Scherer J, Dyer K, et al.. A randomized clinical trial comparing pelvic floor muscle training to a Pilates exercise program for improving pelvic muscle strength. Int Urogynecol J. 2010;21:401–408. doi: 10.1007/s00192-009-1046-z. PMID:20094704. [DOI] [PubMed] [Google Scholar]
- 21.Office of Disease Prevention and Health Promotion Physical activity guidelines for Americans. https://health.gov/paguidelines/guidelines/. Accessed December6, 2016. [Google Scholar]