Abstract
Aim
The number of elderly patients with heart failure is increasing in Japan owing to the increase in the aging population. In the field of emergency medicine, the treatment and management of elderly patients with heart failure are key issues. We aimed to clarify the clinical characteristics and outcomes of these patients.
Methods
We enrolled 72 consecutive patients (age, 76.5 ± 12.5 years) with heart failure who were admitted to our hospital between January 1 and December 31, 2010. The characteristics and outcomes of super‐elderly patients aged >85 years (n = 21) were compared with those of patients aged ≤85 years (n = 51).
Results
The overall prevalence of chronic atrial fibrillation was high (43.1%). Underlying diseases, left ventricular function, renal function, in‐hospital mortality, hospital stay period, and major complications were similar between the two groups. The super‐elderly group had a significantly higher mortality rate and lower event‐free survival rate after discharge (log–rank test, P = 0.0018 and P = 0.0032, respectively).
The incidence of readmission for heart failure recurrence was 55.0% in the super‐elderly group and 25.0% in the younger group.
Conclusion
There were no significant differences in the background characteristics and in‐hospital treatment between super‐elderly heart failure patients and younger patients. High mortality and cardiovascular event rates after discharge were observed in the super‐elderly group.
Keywords: Elderly, heart failure, prognosis
Introduction
Heart failure is the final form of cardiac disease and a major cause of mortality.1, 2 The proportion of elderly people in the Japanese population is currently increasing at an unprecedented rate. The number of individuals in Japan's “super‐aging” society has increased, and individuals in this population have various health problems according to the Annual Report on the Aging Society from the Japanese Cabinet Office.3 Consequently, escalating medical costs and an increased number of bedridden elderly people will be major problems. The prevalence of heart failure increases with advancing age.4 In the field of emergency medicine, the treatment and management of elderly heart failure patients are key issues.
The clinical characteristics, treatment, and outcomes of patients with heart failure have been well described by many studies and trials.5, 6 However, few studies have focused on super‐elderly patients (>85 years).7, 8 These patients have various levels of heart failure, and a variety of daily living activities and social backgrounds. In addition, they may have numerous concurrent diseases, including respiratory conditions, malignancies, and chronic kidney disease. It is important to clarify the clinical characteristics of elderly patients with heart failure in observational studies.
Methods
Study group
The study included 72 consecutive patients with acute heart failure or worsening chronic heart failure who were admitted to our hospital between January 1 and December 31, 2010. Attending physicians diagnosed heart failure by assessing symptoms, carrying out physical examinations, and evaluating chest radiography scans. Patients were divided into two groups according to age, and the findings were compared between the super‐elderly group (aged >85 years) and the younger group (aged ≤85 years).
The mean follow‐up period after discharge for all subjects was 429.6 ± 214.9 days. Occurrence of cardiovascular and other events was determined from medical records, including those of the referring hospital and/or direct interviews with the patients or their families. The primary endpoint was total death. The secondary endpoints were readmission for heart failure, cardiovascular events, and non‐cardiovascular events requiring admission. Cardiovascular events were defined as cardiac death, non‐fatal myocardial infarction, stroke, readmission for heart failure treatment, cardiac surgery, vascular surgery, or percutaneous coronary intervention.
In all cases, either the patients or their families provided written consent for use of the patient information for clinical research. The study protocol was approved by the committee of our hospital.
Data collection
Values of baseline variables, including demographic characteristics, comorbidities, and clinical and laboratory features at admission, were obtained by reviewing medical records. Blood samples were collected within 48 h of hospital admission. The estimated glomerular filtration rate was calculated using the four‐variable Modification of Diet in Renal Disease equation.9 Transthoracic echocardiography was carried out within 48 h of hospital admission. Echocardiographic data were obtained using standard methods by 2D, M‐mode, and Doppler evaluations. In accordance with Vasan and Levy criteria, patients with a left ventricular ejection fraction (LVEF) > 50% were regarded as having heart failure with preserved ejection fraction, and those with <50% LVEF were regarded as having heart failure with reduced ejection fraction (HFREF).10
Statistical analysis
Data were expressed as medians (interquartile range, 25–75%). When a continuous variable had a normal distribution, it was expressed as the mean ± standard deviation. Differences between two independent variables or incidences between two groups were compared using the Wilcoxon test or Fisher's exact test. Kaplan–Meier analysis was used to estimate the probability of the outcome, and probabilities between the two age groups were compared using the log–rank test. Multiple regression analysis was carried out using the Cox proportional hazards model after confirmation of several statistically significant factors by single regression and odds ratios with 95% confidence intervals were calculated. Statistical analysis was carried out using JMP version 8.0 software (SAS Institute, Cary, NC, USA). A P‐value <0.05 was considered statistically significant for all tests.
Results
Clinical characteristics
Of the study group, almost all patients were older adults (76.5 ± 12.5 years), including 83% aged >65 years. Twelve patients (17%) were under 65 years of age. Table 1 shows the baseline clinical characteristics and comorbidities in the two patient groups. There was no significant difference between the two groups in the prevalence of underlying cardiac diseases. Underlying cardiac disease that had been precisely diagnosed was observed in only a few patients in the super‐elderly group. Chronic atrial fibrillation showed a high overall prevalence (43.1%). There was no significant difference between the two groups in terms of renal function, B‐type natriuretic peptide level, LVEF, or HFREF rate.
Table 1.
Heart failure patient characteristics and comorbidities (n = 72)
| Younger group, age ≤85 years | Super‐elderly group, age >85 years | P‐value | |
|---|---|---|---|
| n = 51 | n = 21 | ||
| Male, n (%) | 30 (58.8) | 8 (38.0) | NS |
| Underlying cardiac disease, n (%) | |||
| Chronic ischemic, n (%) | 16 (31.4) | 7 (33.3) | NS |
| Acute coronary syndrome, n (%) | 2 (3.9) | 1 (4.8) | NS |
| Hypertensive, n (%) | 3 (5.9) | 0 (0) | NS |
| Aortic valve stenosis, n (%) | 4 (7.8) | 2 (9.5) | NS |
| Other valvular, n (%) | 3 (5.9) | 3 (14.3) | NS |
| Cardiomyopathic, n (%) | 6 (11.8) | 0 (0) | NS |
| Myocarditis, n (%) | 2 (3.9) | 0 (0) | NS |
| Others, n (%) | 4 (7.8) | 2 (9.5) | NS |
| Atrial fibrillation | |||
| Paroxysmal, n (%) | 2 (3.9) | 2 (9.5) | NS |
| Chronic, n (%) | 22 (43.1) | 9 (42.9) | NS |
| Implanted cardiac pacemaker/defibrillator, n (%) | 3 (5.9) | 2 (9.5) | NS |
| Peripheral arterial disease, n (%) | 3 (5.9) | 0 (0) | NS |
| Lung disease, n (%) | 5 (9.8) | 2 (9.5) | NS |
| Serum creatinine, mg/dL | |||
| Median | 1.1 | 0.9 | NS |
| Interquartile range | 0.8–1.3 | 0.8–1.4 | |
| Blood urea nitrogen, mg/dL | 28.8 ± 18.0 | 32.6 ± 18.1 | NS |
| Estimated glomerular filtration rate, mL/min | 49.7 ± 21.6 | 48.0 ± 19.6 | NS |
| >60, n (%) | 16 (31.4) | 5 (23.8) | NS |
| 30–60, n (%) | 25 (49.0) | 13 (61.9) | NS |
| <30, n (%) | 10 (19.6) | 3 (14.3) | NS |
| B‐type natriuretic peptide, pg/mL | |||
| Median | 556 | 521 | NS |
| Interquartile range | 349–1268 | 372–1410 | |
| Left ventricular ejection fraction, % | 50.4 ± 15.6 | 53.2 ± 16.6 | NS |
| HFREF (EF < 50%), n (%) | 23 (45.1) | 7 (33.3) | NS |
| HFPEF (EF > 51%), n (%) | 28 (54.9) | 14 (66.7) | NS |
EF, ejection fraction; HFREF, heart failure with reduced ejection fraction; HFPEF, heart failure with preserved ejection fraction; NS, not significant.
Table 2 shows patient data on admission and in‐hospital treatments. Hospital stay periods were similar between the two groups. Intensive care was less common in the super‐elderly group (P = 0.0520). In‐hospital mortality was comparable between the two groups. There was no significant difference in non‐fatal events, including stroke (Table 3).
Table 2.
Data on admission and in‐hospital treatment in patients admitted for heart failure (HF) (n = 72)
| Younger group, age ≤85 years | Super‐elderly group, age >85 years | P‐value | |
|---|---|---|---|
| n = 51 | n = 21 | ||
| Type of HF | |||
| Acute HF (first attack), n (%) | 36 (70.6) | 11 (52.4) | NS |
| Worsening of chronic HF, n (%) | 15 (29.4) | 10 (47.6) | NS |
| Admission by ambulance, n (%) | 11 (21.6) | 4 (19.0) | NS |
| Hospital stay, days | |||
| Median | 23.5 | 22.0 | NS |
| Interquartile range | 12.3–34.8 | 18.0–41.8 | |
| Intensive treatment, n (%) | 14 (27.5) | 1 (4.8) | 0.0520 |
| Respirator/BiPAP, n (%) | 2 (3.9) | 1 (4.8) | NS |
| Cardiovascular surgery, n (%) | 3 (5.9) | 0 (0) | NS |
| Pacemaker implantation, n (%) | 3 (5.9) | 0 (0) | NS |
| IABP, n (%) | 1 (2.0) | 0 (0) | NS |
| PCI/EVT, n (%) | 5 (9.8) | 0 (0) | NS |
BiPAP, bilevel positive airway pressure ventilation; EVT, endovascular treatment; IABP, intra‐aortic balloon pumping; NS, not significant; PCI, percutaneous coronary intervention.
Table 3.
In‐hospital outcome for patients admitted with heart failure (n = 72)
| Younger group, age ≤85 years | Super‐elderly group, >85 years | P‐value | |
|---|---|---|---|
| n = 51 | n = 21 | ||
| In‐hospital death, n (%) | 3 (5.9) | 1 (4.8) | NS |
| Cause of death | |||
| Heart failure, n (%) | 2 (3.9) | 1 (4.8) | NS |
| GI bleeding, n (%) | 1 (2.0) | 0 (0) | NS |
| Non‐fatal event | |||
| Stroke, n (%) | 3 (5.9) | 0 (0) | NS |
| GI bleeding, n (%) | 1 (2.0) | 1 (4.8) | NS |
| Pneumonia, n (%) | 4 (7.8) | 1 (4.8) | NS |
GI, gastrointestinal; NS, not significant.
Outcomes
Kaplan–Meier estimates of the survival rate after discharge are shown in Figure 1. The 1‐year mortality rate was 46.1% in the super‐elderly group and 13.4% in the younger group. The super‐elderly group had significantly higher mortality rates than the younger group (log–rank test, P = 0.0018). Figure 2 shows the cardiovascular event‐free survival rates. The rate of cardiovascular event‐free survival at 1 year was 15.0% in the super‐elderly group and 55.7% in the younger group. The super‐elderly group had a significantly lower event‐free survival rate than the younger group (log–rank test, P = 0.0032).
Figure 1.
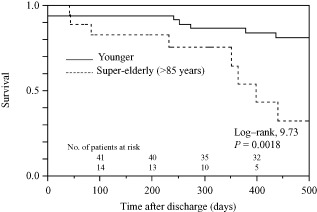
Kaplan–Meier estimates of overall survival after discharge in super‐elderly (aged >85 years; n = 20) and younger (aged ≤85 years; n = 48) heart failure patients.
Figure 2.
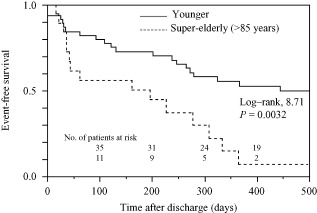
Kaplan–Meier estimates of cardiovascular event‐free survival after discharge in super‐elderly (aged >85 years; n = 20) and younger (aged ≤85 years; n = 48) heart failure patients.
Forty‐eight patients in the younger group and 20 in the super‐elderly group survived up to hospital discharge. Table 4 shows their clinical outcome after discharge. Two patients died of fatal stroke in the super‐elderly group. In both groups, the main cause of death was heart failure. Readmission for recurrence of heart failure was the most frequent event. The incidence of readmission for recurrence of heart failure was 55.0% in the super‐elderly group and 25.0% in the younger group.
Table 4.
Clinical outcome after discharge in patients admitted with heart failure (n = 68)
| Younger group, age ≤85 years | Super‐elderly group, age >85 years) | |
|---|---|---|
| n = 48 | n = 20 | |
| Total death, n (%) | 7 (14.6) | 8 (40.0) |
| Cause of death | ||
| Sudden cardiac death, n | 0 | 0 |
| Acute myocardial infarction, n | 0 | 0 |
| Heart failure, n | 4 | 5 |
| Renal failure, n | 1 | 1 |
| Stroke, n | 0 | 2 |
| Malignant disease, n | 1 | 0 |
| Unknown, n | 1 | 0 |
| Non‐fatal event | ||
| Cardiovascular event | ||
| Readmission for heart failure, n (%) | 12 (25.0) | 11 (55.0) |
| Cardiac surgery, n (%) | 1 (2.0) | 0 (0) |
| Vascular surgery, n (%) | 0 (0) | 0 (0) |
| PCI, n (%) | 3 (6.3) | 0 (0) |
| Stroke, n (%) | 0 (0) | 1 (5.0) |
| Non‐cardiovascular event | ||
| GI bleeding, n (%) | 1 (2.0) | 0 (0) |
| Pneumonia, n (%) | 1 (2.0) | 0 (0) |
GI, gastrointestinal; PCI, percutaneous coronary intervention.
In a multivariate analysis of various factors that may have affected mortality, age and coronary artery disease were found to be independent predictors of total death (Table 5). Only age was found to be an independent predictor of cardiovascular events (Table 6).
Table 5.
Predictors of total death after discharge in patients admitted with heart failure (n = 68)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Hazard ratio (95%CI) | P‐value | Hazard ratio (95%CI) | P‐value | |
| Age | 1.084 (1.031–1.494) | 0.0007 | 1.089 (1.032–1.155) | 0.0009 |
| Male sex | 0.914 (0.366–2.315) | 0.8459 | n.a. | |
| Coronary artery disease | 3.061 (1.233–7.949) | 0.0162 | 2.934 (1.175–7.678) | 0.0214 |
| Atrial fibrillation | 1.024 (0.396–2.534) | 0.9597 | n.a. | |
| Left ventricular ejection fraction | 1.000 (0.973–1.028) | 0.9992 | n.a. | |
| B‐type natriuretic peptide | 0.428 (0.999–1.000) | 0.6666 | n.a. | |
| Estimated GFR | 0.987 (0.966–1.009) | 0.2430 | n.a. | |
| Peripheral arterial disease | 3.290 (0.511–12.076) | 0.1765 | n.a. | |
| Lung disease | 4.387 (0.974–14.573) | 0.0535 | n.a. | |
CI, confidence interval; GFR, glomerular filtration rate; n.a., not applicable.
Table 6.
Predictors of cardiovascular events after discharge in patients admitted with heart failure (n = 68)
| Univariate analysis | ||
|---|---|---|
| Hazard ratio (95%CI) | P‐value | |
| Age | 1.048 (1.015–1.088) | 0.0026 |
| Male sex | 0.771 (0.402–1.481) | 0.4304 |
| Coronary artery disease | 1.717 (0.881–3.283) | 0.1102 |
| Atrial fibrillation | 0.986 (0.506–1.885) | 0.9664 |
| Left ventricular ejection fraction | 0.973 (0.979–1.021) | 0.9700 |
| B‐type natriuretic peptide | 1.036 (1.000–1.000) | 0.9739 |
| Estimated GFR | 0.996 (0.980–1.012) | 0.6129 |
| Peripheral arterial disease | 0.418 (0.023–1.940) | 0.3213 |
| Lung disease | 1.892 (0.561–4.804) | 0.2698 |
CI, confidence interval; GFR, glomerular filtration rate.
Discussion
The present investigation aimed to clarify the clinical characteristics and outcomes of super‐elderly patients with heart failure in our hospital. We found that the studied population had a high prevalence of chronic atrial fibrillation. However, there was no difference in underlying diseases, including atrial fibrillation, between the super‐elderly and younger groups. In‐hospital mortality and the occurrence of major complications were comparable between the two groups, as was the length of hospital stay. Invasive treatment was carried out more frequently in the younger group. The super‐elderly group had a poorer prognosis and higher readmission rate after discharge.
The prevalence of atrial fibrillation increases with age. The Framingham study reported that the prevalence rate rises markedly in people aged >70 years.11 The prevalence of atrial fibrillation in those aged >80 years is 5% in Japan.12 In the ATTEND study, a major clinical observational study of heart failure during hospitalization in Japan, the mean age of the study population was 73.0 ± 13.8 years, and the prevalence of atrial fibrillation was 36.0%.13 In a large study from Europe (EuroHeart Failure Survey), the mean age was 71.7 years, and the prevalence of atrial fibrillation was 38.6%.6 The mean age of patients in our study was 76.5 ± 12.5 years, which is higher than the mean ages reported in the abovementioned studies. Thus, the prevalence of atrial fibrillation (43.1%) in our study was relatively high. In the present study, the prevalence of chronic atrial fibrillation in the super‐elderly group was similar to that in the younger group. Even in those aged >85 years, the prevalence of chronic atrial fibrillation was not sharply increased. Recent major trials on the management of atrial fibrillation have not shown any differences between rate and rhythm control therapies in the rates of mortality and cardiovascular events, including stroke.14, 15 However, considering the high prevalence of chronic atrial fibrillation in this study, chronic atrial fibrillation may have contributed to the onset and exacerbation of heart failure in these elderly patients.
The number of underlying diseases and their severity has been thought to increase with age. However, the present study revealed no significant difference between the younger group and super‐elderly group in terms of background characteristics, including underlying diseases. We deemed underlying cardiac disease to be present in only a few super‐elderly patients (Table 1). We believe that super‐elderly patients may have not been examined by deterministic and invasive techniques such as myocardial biopsy or coronary angiography. Furthermore, some patients may have previously refused detailed examinations and hospitalization. There may also have been some cases in which past medical histories and examination results are unknown due to repeated doctor and hospital changes. The results of this study do not imply that super‐elderly patients have fewer underlying diseases. Clarifying the details of past medical histories and underlying diseases in super‐elderly patients is difficult. In the present study, patient information was mainly obtained from medical records retrospectively, which may have further complicated this issue. This is one of the significant limitations of this study.
The incidences of in‐hospital complications and mortality are thought to increase with increasing age. However, these parameters were comparable between the two groups in this study. Thus, even if a patient with heart failure is super‐elderly, in‐hospital medical treatment should be properly carried out. Furthermore, we should focus on care after discharge, because super‐elderly heart failure patients have a poor prognosis.
Even though cardiac disease and other underlying diseases should be adequately treated, the decline in physical activity and the progression of dementia in elderly patients must be focused upon. Kawai et al. reported that social support is not sufficient in super‐elderly patients with heart failure in Japan.16 Lack of social support may be one of the causes of readmission for recurrence of heart failure. In‐home management of patients with heart failure, and the precise evaluation of the precipitating factor and its avoidance are important. The main precipitating factors related to daily life are excessive effort and over‐intake of water or salt. In super‐elderly patients, aspiration pneumonia due to swallowing difficulties may be a cause of heart failure exacerbation, and general weakness due to appetite loss may also be related to exacerbation. A decline in physical and cognitive functions leads to failure in oral medicine management. Moreover, patients may not be able to regularly visit the hospital. Aggressive interventions, such as more frequent home visits, may be necessary and it is important to account for individual patient circumstances. The early detection of heart failure symptoms and support of hospital visits and treatment would be very beneficial to the elderly. Daily living assistance and counseling for the prevention of depression may also be required. In addition, it may be necessary to consider a cardiac rehabilitation program that can serve the majority of super‐elderly patients. In the near future, heart failure‐certified nurses will play an active role in the management of super‐elderly patients with heart failure in Japanese clinical practice. Furthermore, the “palliative care” proposed in the Guidelines for Treatment of Acute Heart Failure (JCS 2011)17 needs to be actively discussed.
This study has several limitations. First, the number of patients analyzed is too small to draw a definitive conclusion, and this was an observational study from a single institution. Moreover, >80% of the study population was aged ≥65 years, therefore, the study did not include a sufficient number of relatively young patients with heart failure. Firmer conclusions could be drawn from analyses of data obtained from population‐based multicenter prospective registries. Second, the diagnostic criteria for heart failure were not precisely determined, and admission for treatment was decided by the attending physician alone. Finally, asymptomatic events were probably not reflected in the results.
In this study, we investigated the characteristics of super‐elderly patients with heart failure. It was difficult to clarify the details of the background characteristics of super‐elderly patients. In‐hospital treatment was similar between super‐elderly and younger patients. Mortality and cardiovascular event rates after discharge were high in the super‐elderly group. Age was found to be an independent predictor. Ensuring adequate medical and social support after discharge may be one of the effective measures for improving the prognosis. Further studies are needed to achieve more appropriate management of these patients.
Conflict of Interest
None.
Acknowledgments
We thank all staff of Sapporo Social Insurance Hospital for their kind contributions.
References
- 1. Hunt SA, Abraham WT, Chin MH et al ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J. Am. Coll. Cardiol. 2005; 46: e1–82. [DOI] [PubMed] [Google Scholar]
- 2. Swedberg K, Cleland J, Dargie H et al Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur. Heart J. 2005; 26: 1115–1140. [DOI] [PubMed] [Google Scholar]
- 3. Cabinet Office, Government of Japan . Annual Report on the Aging Society. 2012. [cited 1 Dec 2013]. Available from: http://www8.cao.go.jp/kourei/whitepaper/w-2013/zenbun/25pdf_index.html.
- 4. Massie BM, Shah NB. Evolving trends in the epidemiologic factors of heart failure: rationale for preventive strategies and comprehensive disease management. Am. Heart J. 1997; 133: 703–712. [DOI] [PubMed] [Google Scholar]
- 5. Adams KF Jr, Fonarow GC, Emerman CL et al Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am. Heart J. 2005; 149: 209–216. [DOI] [PubMed] [Google Scholar]
- 6. Harjola VP, Follath F, Nieminen MS et al Characteristics, outcomes, and predictors of mortality at 3 months and 1 year in patients hospitalized for acute heart failure. Eur. J. Heart Fail. 2010; 12: 239–248. [DOI] [PubMed] [Google Scholar]
- 7. Pilotto A, Addante F, Franceschi M et al Multidimensional Prognostic Index based on a comprehensive geriatric assessment predicts short‐term mortality in older patients with heart failure. Circ. Heart Fail. 2010; 3: 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Conde‐Martel A, Formiga F, Pérez‐Bocanegra C et al Clinical characteristics and one‐year survival in heart failure patients more than 85 years of age compared with younger. Eur. J. Intern. Med. 2013; 24: 339–345. [DOI] [PubMed] [Google Scholar]
- 9. Manjunath G, Sarnak MJ, Levey AS. Prediction equations to estimate glomerular filtration rate: an update. Curr. Opin. Nephrol. Hypertens. 2001; 10: 785–792. [DOI] [PubMed] [Google Scholar]
- 10. Vasan RS, Levy D. Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation 2000; 101: 2118–2121. [DOI] [PubMed] [Google Scholar]
- 11. Fuster V, Rydén LE, Cannom DS et al ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation 2006; 114: e257–354. [DOI] [PubMed] [Google Scholar]
- 12. Iguchi Y, Kimura K, Aoki J et al Prevalence of atrial fibrillation in community‐dwelling Japanese aged 40 years or older in Japan: analysis of 41,436 non‐employee residents in Kurashiki‐city. Circ. J. 2008; 72: 909–913. [DOI] [PubMed] [Google Scholar]
- 13. Sato N, Kajimoto K, Keida T et al TEND Investigators. Clinical features and outcome in hospitalized heart failure in Japan (from the ATTEND Registry). Circ. J. 2013; 77: 944–951. [DOI] [PubMed] [Google Scholar]
- 14. Wyse DG, Waldo AL, DiMarco JP et al A comparison of rate control and rhythm control in patients with atrial fibrillation. N. Engl. J. Med. 2002; 347: 1825–1833. [DOI] [PubMed] [Google Scholar]
- 15. Roy D, Talajic M, Nattel S et al Rhythm control versus rate control for atrial fibrillation and heart failure. N. Engl. J. Med. 2008; 358: 2667–2677. [DOI] [PubMed] [Google Scholar]
- 16. Kawai Y, Inoue N, Onishi K. Clinical picture and social characteristics of super‐elderly patients with heart failure in Japan. Congest. Heart Fail. 2012; 18: 327–332. [DOI] [PubMed] [Google Scholar]
- 17. JCS Joint Working Group . Guidelines for treatment of acute heart failure (JCS 2011)—digest version. Circ. J. 2013; 77: 2157–2201. [DOI] [PubMed] [Google Scholar]


