Abstract
Background
Traditional assessment and treatment of bipolar disorder (BD) often overlooks an important feature of the illness, mood instability (MI). MI - the presence of intense, rapidly shifting emotional states - is associated with a number of poor prognostic outcomes. This study examined whether MI among adolescents with BD was cross-sectionally related to bipolar subtype (I vs. II) and prognostically associated with symptoms and functioning over 3 months.
Methods
Participants included 145 adolescents (mean age: 15.6 yrs. ± 1.4) with BD I or II with a mood episode in the previous 3 months. Depression and (hypo)mania instability were computed using the root mean square successive difference (rMSSD) score, reflecting both the size and temporal order of changes in weekly depression and (hypo)mania scores (over 12 weeks) from the Adolescent Longitudinal Interval Follow-Up Evaluation.
Results
Greater depression instability was associated with BD II, whereas greater (hypo)mania instability was associated with BD I. Baseline MI, particularly depression, predicted more instability, a higher percentage of weeks in a clinical mood state, and poorer global functioning over 3 months, even when covarying concurrent mood severity scores.
Limitations
The clinical measure of symptoms used retrospective reports of clinically significant symptoms only. We were unable to standardize medication use or adherence.
Conclusions
MI differs by diagnostic subtype, is relatively stable over time, and predicts clinical and functional outcomes. Targeting MI should be considered a clinical focus to augment traditional methods of assessing and treating BD during adolescence to enhance clinical and functional outcomes.
Keywords: Mood Disorders, Affective Instability, Psychosocial Functioning, Childhood-Onset Bipolar Disorder, Adolescence
1. Introduction
Bipolar disorder (BD) is characterized by severe and episodic mood changes. Course of illness is typically operationalized as the number and length of clinically significant episodes of mania or depression and/or the average symptom severity within these episodes. Although essential in characterizing the course of illness, focusing on episodes alone overlooks other features of BD, notably, the fluctuation of mood states over time, including the periods between episodes. Mood instability (MI) is the experience of intense, rapidly shifting emotional states during mood episodes as well as during remission (Henry et al., 2008). Research has demonstrated that MI during euthymic periods among adults with BD is associated with poor prognostic variables (e.g., earlier age of onset) and outcomes (e.g., increased likelihood of hospitalization, lifetime comorbidity with anxiety or substance use disorder(Bonsall et al., 2012; Henry et al., 2008; Marwaha et al., 2014; Patel et al., 2015).
MI has been defined and measured inconsistently using both broad classifications (e.g., presence/absence of frequent mood changes) and specific dimensions (e.g., number and degree of shifts between and within specific affective states; (Koenigsberg, 2010). Methods of measuring MI have ranged from self-report measures to clinician ratings to ecological momentary assessments (Henry et al., 2001; Marwaha et al., 2014). These and other methodological inconsistencies have made results difficult to generalize across studies.
In normative populations, the presence or absence of “lots of mood changes in recent years” was associated with suicidal thoughts and increased use of healthcare services in a large community sample (Marwaha et al., 2013). In the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), higher levels of MI (i.e., number of mood changes observed by treating clinicians) predicted a lower likelihood of recovery from a bipolar depressive episode over a one-year treatment period (Stange et al., 2016). Frequent changes in illness polarity (defined as changes from depression to euthymia or to hypomania) were associated with poorer work functioning, financial problems, interpersonal conflicts, and disrupted leisure time among euthymic adults with BD (Strejilevich et al., 2013).
Examining MI is especially relevant among children and adolescents with mood disorders. Childhood-onset BD is associated with a more severe course of illness than adult-onset BD, including more polarity switches, longer periods with subthreshold symptoms, more mixed symptoms and increased suicidal behaviors (Birmaher and Axelson, 2006; Perlis et al., 2004; Propper et al., 2015). MI has been found to predict the onset of bipolar spectrum disorders over 7-8 years among youth with a first or second-degree relative with BD (Birmaher et al., 2013; Hafeman et al., 2016; Kochman et al., 2005). In children and adolescents with major depressive disorder, higher levels of cyclothymic temperament, MI and emotional over-reactivity are associated with more suicidal ideation, suicide attempts, aggressive behaviors, and psychotic symptoms over a 5-year period (Kochman et al., 2005). These results suggest that MI may be a predictor of BD onset as well as a predictor of poorer course of illness in major depression. There is little research, however, on the relevance of MI to the clinical course of youth with a diagnosis of bipolar I (BD I) or bipolar II disorder (BD II).
This study aimed to clarify the role of MI in the clinical course of adolescents with BD I or BD II who were seeking treatment. We measured MI through weekly Psychiatric Status Ratings on the Adolescent Longitudinal Interval Follow-up Examination (Keller et al., 1987), obtained retrospectively for the 3 months before participants were randomly assigned to one of two psychosocial interventions (plus medications), and again after 3 months of treatment. We examined whether baseline MI (measured 3 months prior to randomization) was associated with follow-up clinical and psychosocial outcomes (measured 3 months after randomization). We hypothesized that baseline MI scores would be: 1) higher in adolescents with BD I than in adolescents with BD II, particularly when MI was calculated on hypomanic/manic symptoms; 2) stable over a 3-month period; 3) associated with a higher percentage of weeks at follow-up in which adolescents had clinically significant mood symptoms; and 4) associated with poorer global functioning over 3 months.
2. Methods
2.1 Overview
Data for this study were drawn from a 2-year randomized controlled trial of family-focused treatment for adolescents (FFT-A) or enhanced care (EC, brief psychoeducation), plus good practice pharmacotherapy. The study ran from August 2006 to July 2010 at three U.S. sites: University of Colorado, Boulder, CO; University of Pittsburgh School of Medicine, Pittsburgh, PA; the University of Cincinnati/Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio. Participants were referred through community practitioners, inpatient and outpatient psychiatric units, advertisements, and public presentations. Further study design details can be found in a previous manuscript (Miklowitz et al., 2014).
The overall aim of the present study was to determine whether, in this sample of adolescents with BD I and BD II, baseline MI (3 months prior to randomization) was correlated with bipolar subtype, follow-up mood symptoms and follow-up global functioning (3 months after randomization). Assignment to FFT-A or EC was examined as a covariate.
This study was approved by the institutional review boards of all three universities. Consent was obtained from all study patients and family members.
2.2. Participants
The study included 145 participants between the ages of 12 years, 0 months to 18 years, 1 month along with at least one parent or step-parent. To be eligible for participation, adolescents had to meet criteria for a DSM-IV-TR diagnosis of BD I or I determined by the “Kiddie” Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version (K-SADS-PL; (Chambers et al., 1985). Additional inclusion criteria required an episode of depression, mania, hypomania, or mixed disorder in the 3 months before enrollment, with symptoms of at least moderate severity (≥ 17 on the K-SADS Mania Rating Scale or ≥ 16 on the K-SADS Depression Rating Scale; Axelson et al., 2003; Chambers et al., 1985). Exclusion criteria included a DSM-IV-TR diagnosis for a current substance abuse/dependence disorder or pervasive developmental disorder. Reliability for the K-SADS was determined using 12 diagnostic interview tapes rated by an average of 12 raters at each site; intraclass rs were .89 for K-SADS Depression Rating Scale Scores and .81 for Mania Rating Scale scores.
2.3 Measures
2.3.1 Adolescent Longitudinal Follow-Up Evaluation
Weekly mood ratings were derived from the Adolescent Longitudinal Interval Follow-Up Evaluation (ALIFE; Keller et al., 1987(Birmaher et al., 2009a; Keller et al., 1987). This interview-based measure generates weekly Psychiatric Status Ratings (PSRs) for depression using a 6-point severity scale (1 = no symptoms, 2–4 = subthreshold symptoms, 5 = meets full threshold DSM-4 criteria for major depression for that week, without psychosis or extreme impairment in functioning, 6 = full threshold DSM-4 major depression criteria for that week, with psychosis or extreme impairment in functioning). The 6-point hypomania PSR follows similar criteria, but a rating of 5 refers to full threshold DSM-4 criteria for hypomania, with change in functioning, and 6 refers to severe threshold DSM-4 criteria for hypomania, with change in functioning. There is a separate weekly rating for the presence or absence of mania (1 = no manic symptoms, 5 = meets full threshold DSM-4 criteria for mania without psychosis or extreme impairment in functioning, 6 = full threshold DSM-4 criteria for mania with psychosis or with extreme impairment in functioning). Independent evaluators based weekly ratings on the consensus of the adolescent and parent’s retrospective reports covering the 12 weeks prior to randomization. Inter-rater reliabilities for the 6-point PSR scores averaged 0.74 (intraclass r) for depression and mania or hypomania scores.
2.3.2 Children’s Global Assessment Scale
The Children’s Global Assessment Scale (CGAS) is a measure of global functioning over a 2-week period. Its values range from 1, representing the most functionally impaired, to 100, representing full health with scores above 70 indicating normal functioning. The measure has been found to have good concurrent and discriminant validity (Shaffer et al., 1983). CGAS scores for this study reflected the lowest 2-week rating of global functioning recorded during follow-up (3 months after randomization).
2.4 Procedures
Adolescents and at least one parent were interviewed at baseline and a 3-month follow-up assessment. The baseline interview consisted of a clinical assessment covering the 12 weeks prior to randomization using the KSADS, the Adolescent LIFE interview and the PSRs (depression, hypomania, mania) and the CGAS. The follow-up assessments (conducted 3 months after randomization) included the PSRs (depression, hypomania, mania) and the CGAS. Ratings of all measures reflected a consensus between adolescent and parent reports.
The baseline rating of mood instability (based on A-LIFE PSR scores) and the baseline rating of the severity of the episode that brought the adolescent into the study (a depressed, manic, hypomanic, or mixed episode by the K-SADS Depression and Mania Rating Scales) overlapped by design. We were interested in measuring mood instability during an acute period in which the child had at least a 1- or 2-week mood episode, and again at the end of a 3-month recovery period when their symptoms were expected to have stabilized.
2.5 Mood Instability and Symptom Severity Scores
Depression and (hypo)mania instability were computed using the root mean square successive difference (rMSSD) score method, a score that reflects the extent to which consecutively-measured moods differ from one another over a defined period (Ebner-Priemer and Trull, 2009; Jahng et al., 2008; Trull et al., 2008). The baseline rMSSD scores were derived from PSR ratings of the 12 weeks before randomization to treatments and the follow-up rMSSD scores for the 12 weeks after randomization. The rMSSD reflects both the size and the temporal order of changes in weekly depression and (hypo)mania scores on the PSRs. The squared difference between symptom severity scores at each consecutive time point was independently computed for depression and (hypo)mania and averaged for each participant across 12 weeks. The square root of the average was then used to compute the rMSSD. Higher rMSSD scores indicate more depression or (hypo)mania instability. Previous reports have demonstrated the construct validity of this method (Ebner-Priemer and Trull, 2009; Jahng et al., 2008).
Percentage of weeks in a depressive or (hypo)manic state was determined using weekly depression and (hypo)mania PSR scores. Baseline percentage of weeks in a depressed (i.e., a PSR score of 5 or higher) or (hypo)manic state was calculated as the number of weeks before randomization in which the participant met DSM-IV criteria for a syndromally depressive or (hypo)manic state divided by the number of weeks in that interval. Follow-up percentage of depressed or (hypo)manic weeks was calculated as the number of weeks within the 12 weeks following randomization an individual met criteria for a depressed or (hypo)manic state divided by the number of weeks in the post-randomization interval (most typically 12, although average number of weeks = 15.97 (SD = 3.67)).
2.6 Data Analyses
The data were analyzed using IBM SPSS version 22 (Statistical Package for the Social Sciences). Descriptive statistics and frequency distributions were calculated for all demographic and illness history variables (e.g., sex, race, ethnicity, living status, SES, age, age of onset of first depression and (hypo)mania symptoms).
The primary study questions concerned (1) the relationships between baseline depression or (hypo)mania instability and bipolar subtype (type I vs II), taking into account the medications the patients were taking at baseline; (2) whether baseline MI was stable over the follow-up period, and (3) whether baseline MI predicted follow-up percentage of weeks in depressed/(hypo)manic states and follow-up global functioning.
For data analyses, PSR scores for hypomania and mania were collapsed into one 8-point scale labeled (hypo)mania, the assumption being that these mood states are on a continuum where full hypomania is less severe than full mania. To distinguish hypomania from mania on this single scale, scores between 1 and 6 were identical to those of the original PSR hypomania scale. A PSR score of 7 on the 8-pt (hypo)mania scale meant that the participant had at least a week in which fully syndromal manic symptoms were present with accompanying functional impairment. A PSR score of 8 meant one week with severe manic symptoms, with psychosis and/or extreme impairment, usually requiring hospitalization.
Spearman correlations and one-way ANOVAs were conducted to examine the relationships between demographic variables (e.g., age, sex) and baseline depression and (hypo)mania instability; significant relationships were included as covariates in the primary regression models. Next, we computed logistic regression models in which the predictor variables were baseline depression and (hypo)mania instability and the outcome variable was bipolar subtype (I vs. II). We then computed multiple regression models in which the predictor variables were baseline depression or (hypo)mania instability and the outcome variables were follow-up depression or (hypo)mania instability scores, follow-up percentage of weeks depressed or (hypo)manic, and follow-up global functioning (CGAS). Covariates included in both models were treatment group (FFT-A, EC) and baseline mood symptom severity of the models’ respective mood state (baseline percentage of weeks depressed or (hypo)manic).
3. Results
3.1. Descriptive Statistics and Frequency Distributions
A total of 145 adolescents and families participated in the study, with 77 meeting DSM-IV criteria for BD I and 68 for BD II (Table 1). The overall mean age was 15.6 years (SD = 1.4) with 79 females and 66 males. Adolescents with BD I had a significantly higher percentage of weeks with (hypo)mania during the baseline period (M = 30.02, SD = 33.70) compared to those with BD II (M = 11.76, SD = 18.21; F1, 144 = 15.86, p < .0001). Participants with BD I did not differ from those with BD II on percentage of weeks depressed scores during the baseline period. For a comparison between mean depression PSRs (sum of 12 weekly PSRs divided by 12 weeks) and actual weekly PSR scores, calculated across participants, see Figures 1 and 2. These figures show the information that is lost when an average score is calculated over 12 weeks versus examined weekly. The frequent mood fluctuations that are clearly present are not captured in the average score suggesting that another method may be more useful in understanding the MI present in BD.
Table 1.
Demographics and Clinical Characteristics of Adolescents with Bipolar I and Bipolar II Disorder
| BDI (N=77) |
BDII (N=68) |
Total (N=145) |
|
|---|---|---|---|
|
| |||
| Characteristics | N | N | N |
| Female | 39 | 40 | 79 |
| Nonwhite | 13 | 11 | 24 |
| Hispanic | 6 | 6 | 12 |
| Lives with both biological parents | 26 | 24 | 50 |
| Current comorbid disorders | |||
| Anxiety Disorder | 25 | 32 | 57 |
| Attention Deficit Hyperactivity Disorder | 27 | 21 | 68 |
| Oppositional Defiant or Conduct Disorder | 27 | 15 | 42 |
|
| |||
| Mean (SD) | Mean (SD) | Mean (SD) | |
|
| |||
| Age | 15.4 (2.5) | 15.8 (1.4) | 15.6 (1.4) |
| Socioeconomic Status (class 1-5) | 3.6 (1.2) | 3.7 (1.2) | 3.6 (1.2) |
| Age of Depression Onset | 10.9 (2.5) | 11.9 (2.7) | 11.4 (2.7) |
| Age of Hypo/Mania Onset | 11.3 (3.2) | 12.3 (3.6) | 11.7 (3.4) |
| Percentage of weeks in a depressive episode | 22.2 (26.4) | 27.2 (24.5) | 24.9 (25.6) |
| Percentage of weeks in a (hypo)manic episode | 30.0 (33.7) | 11.8 (18.2) | 21.7 (29.1) |
| Depression Instability Score (rMSSD) | .93 (.66) | 1.2 (.6) | 1 (.6) |
| Baseline Hypo/Mania Instability Score (rMSSD)a | 1.4 (.8) | 1.3 (.7) | 1.3 (.8) |
| CGASb score | 37.6 (7.5) | 44.0 (6.9) | 40.6 (7.9) |
root mean square successive difference.
CGAS = Children’s Global Assessment Scale
Figure 1.
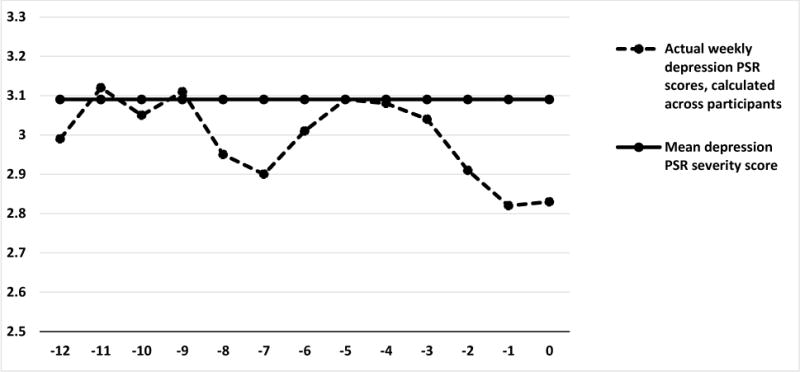
Comparison between overall 3-month mean depression Psychiatric Status Ratings (PSRs; sum of 12 weekly PSRs divided by 12 weeks) and actual weekly PSR scores, calculated across adolescents with bipolar disorder.
12 Weeks Prior to Initial Assessment Psychiatric Status Ratings (PSRs) for Depression
Figure 2.
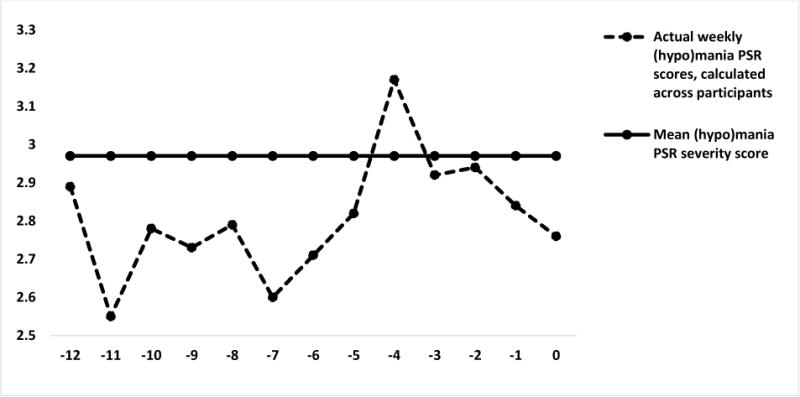
Comparison between overall 3-month mean (hypo)mania Psychiatric Status Ratings (PSRs; sum of 12 weekly PSRs divided by 12 weeks) and actual weekly PSR scores, calculated across adolescents with bipolar disorder.
12 Weeks Prior to Initial Assessment Psychiatric Status Ratings (PSRs) for (Hypo) mania
3.2. Effects of Demographic Variables on Mood Instability
Females had greater baseline (hypo)mania instability scores than males (F(1, 144) = 5.43, p = .02) but there were no sex differences on depression instability. Therefore, sex was included as a covariate for the (hypo)mania instability regression models. There were no between-group differences among racial, ethnic, or SES groups on baseline depression or (hypo)mania instability. Age was not found to be significantly correlated with either baseline depression or (hypo)mania instability.
3.3. Diagnostic Subtype and Mood Instability
Baseline depression instability significantly distinguished between BD I and BD II participants, Wald X2=4.56, OR = 1.85 (95% CI [1.05 – 3.24]), p = .03: when baseline depression instability scores increased by 1 point (indicating greater instability), adolescents were 85% more likely to have BD II. Neither covariate in the model (baseline percent of weeks depressed and treatment group) was significant in distinguishing bipolar I and II subtypes.
Baseline (hypo)mania instability significantly distinguished between BD I and BD II participants, Wald X2=4.77, OR = .57 (95% CI [.34 - 95]), p = .03: when baseline (hypo)mania instability scores increased by 1 point (greater instability), adolescents were 75% more likely to have BD I than BD II. Patients who had BD I also spent more weeks in (hypo)manic states at baseline than patients with BD II (p < .001). The covariates, treatment group and sex, were not significant in this model.
3.4. Depression Instability as a Predictor of Clinical Outcomes
To examine the stability of depression instability over time, a multiple regression analysis was conducted to test whether baseline depression instability predicted follow-up depression instability, while controlling for treatment group and baseline percentage of weeks depressed. The overall regression model was significant, F(3, 110) = 5.22, p < .01, with an adjusted R2 = .10. Greater baseline depression instability scores (more instability) predicted greater follow-up depression instability, b = .33, t(110) = 3.54, p < .01. The covariates in the model, treatment group and baseline percentage of weeks depressed were not significant.
Next, we examined whether baseline depression instability would predict follow-up percent of weeks depressed, controlling for baseline percent of weeks depressed and treatment group. The overall regression model was significant, F(3, 110) = 6.04, p < .01, with an adjusted R2 = .12. Greater baseline depression instability scores predicted greater follow-up percent of weeks depressed, b = .18, t(110) = 1.98, p = .05. Additionally, baseline percent of weeks depressed was associated with follow-up percent of weeks depressed, b = .29, t(110) = 3.77, p < .001. The effect of treatment group was not significant.
3.5. (Hypo)Mania Instability as a Predictor of Clinical Outcomes
To examine the stability of (hypo)mania instability over time, a multiple regression analysis was conducted. This analysis evaluated whether baseline (hypo)mania instability predicted follow-up (hypo)mania instability, while controlling for treatment group and baseline percentage of weeks (hypo)manic. The overall regression model was not significant. However, greater baseline (hypo)mania instability scores (more instability) predicted greater follow-up (hypo)mania instability, b = .18, t(110) = 2.10, p = .04. The covariates, treatment group, sex, and baseline percentage of (hypo)manic weeks were not significant in this model.
The overall regression model using baseline (hypo)mania instability to predict follow-up percentage of weeks (hypo)manic was significant, F(3, 110) = 2.80, p = .03, with an adjusted R2 = .06. Baseline (hypo)mania instability scores did not significantly predict follow-up percentage of weeks (hypo)manic. However, baseline percentage of weeks (hypo)manic significantly predicted follow-up weeks (hypo)manic, b = .17, t(110) = 2.97, p < .01. Treatment group and sex were not significant in this model.
3.6. Mood Instability and Global Functioning
A multiple regression analysis was conducted to determine whether baseline depression instability predicted follow-up global functioning, while controlling for treatment group and baseline percentage of weeks depressed. The overall regression model was significant, F(3, 103) = 3.96, p = .01, with an adjusted R2 = .08. Greater baseline depression instability scores (more instability) were significantly associated with lower follow-up CGAS scores (poorer global functioning), b = −5.17, t(103) = −2.80, p = .01. The covariate, baseline percent of weeks depressed was significant, b = −.10, t(03) = −2.25, p = .03; treatment group was not significant.
The overall regression model using baseline (hypo)mania instability to predict follow-up global functioning was not significant. Neither baseline (hypo)mania instability nor any of the covariates (i.e., baseline percent weeks (hypo)manic, treatment group, sex) predicted follow-up global functioning scores.
3.7. Effects of Baseline Medication Regimens on Instability Scores
To control for potential medication effects on baseline MI scores, we stratified the sample according to whether patients were or were not taking medications in the following classes: antidepressants, antipsychotics, lithium, anticonvulsants, and stimulants. One-way ANOVAs were conducted to examine the relationships between these medication classes and baseline depression and (hypo)mania instability scores. Adolescents with BD I or II who were taking antipsychotics (N = 92) were found to have significantly higher (hypo)mania instability scores than adolescents with BD I and II who were not taking antipsychotics (N = 53; F(1, 144) = 4.73, p= .03), but antipsychotic classification was unrelated to depression instability scores. There were no differences between patients taking or not taking antidepressants, lithium, anticonvulsants, and stimulants on baseline depression or (hypo)mania instability scores.
Next, baseline antipsychotics (prescribed vs. not) was included as a covariate in the multiple regression models in which baseline (hypo)mania instability was used to predict follow-up (hypo)mania instability scores, percentage of weeks (hypo)manic, and global functioning (CGAS) scores. Patients with bipolar I and II disorders still differed on (hypo)mania instability and percentage of weeks (hypo)manic (ps < .05) when antipsychotics were covaried. Results for the regression model using baseline (hypo)mania instability to predict follow-up global functioning remained non-significant when antipsychotics were covaried.
4. Discussion
This study examined the utility of MI in (a) distinguishing between BD I and BD II, (b) predicting outcomes (e.g., percentage of weeks depressed/(hypo)manic) over 3 months of treatment, and (c) predicting global functioning (CGAS scores) among adolescents with BD I or BD II. Our results indicate that MI is a relatively stable variable over a short-term follow-up and may be an important indicator of BD subtypes, as well as a predictor of clinical and functional outcomes.
MI has recently been shown to predict early-onset BD among depressed youth (Kochman et al., 2005). Our findings expand this work to suggest that MI may also help to distinguish between BD I vs. II subtypes in adolescents, who (on average) have a more severe and complicated course of illness than adult-onset BD (Birmaher and Axelson, 2006). Diagnosing subtypes of BD is usually determined by gathering a thorough history of mood episodes (depression/(hypo)mania), with the presence of mania as a hallmark determinant of BD type. However, distinguishing a manic episode from a hypomanic episode can be difficult, particularly with retrospective reports of symptoms (Hirschfeld et al., 2003). Using MI to inform diagnosis may improve overall accuracy and enhance prediction of course of illness in adolescents with BD. Future work in pediatric samples should examine whether MI can distinguish not only between BD subtypes but also between unipolar and bipolar presentations as has been shown in adults (Trull et al., 2008). Unfortunately, we did not include a subset of participants with BD NOS, which would have been useful given the difficulty clinicians have in distinguishing subthreshold versions of BD from its fully threshold variants.
Consistent with literature examining adults for up to 2 years (Clayton et al., 1994; Kochman et al., 2005; Strejilevich et al., 2013; Trull et al., 2008), our findings indicate that MI, particularly depression instability, predicts future MI, percentage of weeks in a depressed state, and global functioning among adolescents with BD over 3 months. Our findings are novel in suggesting that MI may be a stable trait of BD that predicts clinical course and functioning beyond what is predicted by prior percentage of weeks in a depressed or (hypo)manic state. Psychosocial impairments (i.e., poor academic performance, decreased quality of life) among adolescents with BD following acute mood episodes may, in part, reflect mood dysregulation at subthreshold levels (DelBello et al., 2007; Gitlin et al., 2011; Olsen et al., 2012). Traditional assessment and treatment of BD defines euthymic states as the absence of mood episodes. Our findings, however, indicate that MI provides unique additional variance in predicting course of illness. Treating adolescents until they achieve a persistent level of mood stability may help to ameliorate functional impairments during the post-episode period.
Research from the Course and Outcome of Bipolar Youth study demonstrates that adolescents with BD spend more time in depressive episodes than in manic or mixed episodes (Birmaher et al., 2009b). Possibly, depressive MI is a marker of vulnerability to persistent depressive symptoms over time, unless interrupted by effective treatment. Future research examining the interplay between ongoing depression instability and depressive episode severity among adolescents with BD I versus BD II may clarify this relationship.
MI has been identified as a core component of borderline personality disorder and neuroticism given the defining features of frequent fluctuations in mood (e.g., anxiety, anger, sadness) and strong reactivity to environmental stimuli (Henry et al., 2001; Marwaha et al., 2013; Miller and Pilkonis, 2006; Trull et al., 2008). Our findings that MI is a stable feature of BD among adolescents indicates that MI may overlap with personality traits such as neuroticism. Future studies assessing the relationship between personality traits and MI – especially studies that clarify whether MI is a feature of comorbid personality disorder or BD – are certainly warranted. Measures of MI including both the presence (i.e., frequency, intensity) of mood shifts as well as the ability to regulate mood changes are necessary (Marwaha et al., 2013).
5. Limitations
The sample was primarily Caucasian, from middle to upper class homes (mean Hollingshead-Redlich status of 3.64 + 1.20; (Hollingshead and Redlich, 1958) and all families were seeking treatment for the adolescent’s BD. Therefore, results obtained from this study may not generalize to the broader population of adolescents with BD in lower SES environments or those who are less motivated for psychosocial treatment. Participants in this study were randomized into two treatment groups, FFT-A and EC. Although the first 3 months of the study involved psychoeducational sessions in both groups, one group received these sessions weekly for 3 months, whereas the other group received a total of 3 family sessions in the first month. Further, there was variability in medication regimens over the first 3 months. We did not include physician’s or patient’s ratings of medication adherence, variables that may have affected short-term symptomatic outcome (Delbello et al., 2007).
There were limitations related to the clinical measure used to determine symptom severity and MI. These variables were based on PSRs, an ordinal scale with retrospective reports of participants and parents over 3 months. Further research examining the relationships between MI and symptom severity using a daily measure such as moment-to-moment mood ratings may reduce the burden on recall (Ebner-Priemer and Trull, 2009).
Next, the percentage of weeks meeting clinical threshold, the symptom severity variables used in this study, did not capture the subthreshold symptoms that we know affect clinical and functional outcomes in patients with BD. Future use of a continuous measure such as the Children’s Depression Rating Scale would capture both threshold and subthreshold symptoms, providing an even greater understanding of MI as a predictor of outcomes.
The ALIFE was used to create scores for both MI and symptom severity, suggesting another possible limitation. However, the two variables, baseline depression instability and baseline percentage of weeks in a depressed state, were not significantly correlated (p>.05). There was a weak, negative correlation between baseline (hypo)mania instability and baseline percentage of weeks in a (hypo)manic state (r=−.30, p<.001). This suggests that, despite using the same assessment tool, the constructs measured captured different features of BD.
MI is a feature of borderline personality disorder and neuroticism as well as BD (Bowen et al., 2012; Marwaha et al., 2014; Trull et al., 2008). This study did not assess personality traits and/or personality disorders due to the uncertainty regarding diagnoses of personality disorders in adolescents (ages 13-18; Bondurant et al., 2004). Furthermore, it was recently found that detection of personality disorders among adults with BD is dependent on their assessment during depressive episodes only (Post et al., 2018). This suggests accurate detection of personality disorders would have been compromised in this study for those displaying a non-depressive mood state during the baseline assessment. Nonetheless, it is possible that including data on the presence or absence of impulsive personality traits would have explained some of the variability in moods over the study intervals, although determining the cause/effect relationship between personality and mood variables in this sample would have been challenging.
6. Conclusions
Targeting MI, particularly depressive symptoms, should be considered an adjunctive focus to the traditional methods of understanding BD, especially among adolescents with the disorder. Adolescents, in general, are faced with the challenge of managing periodic mood fluctuations within their daily lives (Stringaris and Goodman, 2009), and these challenges are magnified in BD. High levels of MI may be associated with the more severe consequences of adolescent BD, including psychosis, self-harm, or compromised psychosocial functioning (Birmaher et al., 2009a; Geller et al., 2000; Goldstein et al., 2012; Perlis et al., 2004; Propper et al., 2015). Developing a more nuanced understanding of the impact of MI on clinical and functional outcomes is essential for developing more effective interventions and providing a better quality of life for those with childhood-onset BD.
Highlights.
Examined whether MI was associated with bipolar subtype among adolescents with BD.
Examined whether MI was associated with mood symptoms and CGAS scores over 3 months.
Greater depression instability was associated with BD II.
Greater (hypo)mania instability was associated with BD I.
MI predicted mood severity and CGAS scores over 3 months among adolescents with BD.
Acknowledgments
The authors thank Adrine Biuckians, Ph.D., University of Colorado, Boulder, Jedediah Bopp, Ph.D., University of Colorado, Boulder, Victoria Cosgrove, Ph.D., Stanford University School of Medicine, L. Miriam Dickinson, Ph.D., University of Colorado, Boulder, Dana Elkun, M.A., M.F.A., University of Colorado, Boulder, Elizabeth George, Ph.D., University of Colorado, Boulder, Jessica Lunsford-Avery, Ph.D., Duke University School of Medicine, Chris Hawkey, M.A., University of Colorado, Boulder, Zachary Millman, B.A., University of Maryland, Baltimore Country, Aimee Sullivan, Ph.D., University of Colorado, Boulder, Dawn Taylor, Ph.D., University of Colorado, Boulder, Margaret M. Van de loo, University of California, Los Angeles, Marianne Wamboldt, M.D., University of Colorado, Boris Birmaher, M.D., University of Pittsburgh School of Medicine, and Melissa DelBello, M.D., University of Cincinnati Academic Health Center for their assistance.
Roles of the Funding Sources:
Financial Support was provided by National Institute of Mental Health (NIMH) grants R01 MH073871 and R34MH077856 to Dr. Miklowitz, grant R01MH073817 to Dr. Axelson, and grant R01MH074033 to Dr. Robert Kowatch. The sponsors named above did not have any role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Effectiveness of Family-Focused Treatment Plus Pharmacotherapy for Bipolar Disorder in Adolescents, http://clinicaltrials.gov identifier; NCT00332098
Conflicts of Interest
Drs. O’Donnell, Ellis, and Axelson have no conflicts of interest to declare. Dr. Stange is supported by the National Institute of Mental Health (K23MH112769) and has received research funding from the Brain and Behavior Research Foundation. Dr. Schneck has received research support from NIMH, the Crown Family Philanthropies, and the Ryan White HIV/AIDS Treatment Extension Act. Dr. Miklowitz has received research funding from the National Institute of Mental Health, Brain and Behavior Research Foundation, Attias Family Foundation, Danny Alberts Foundation, Carl and Roberta Deutsch Foundation, Kayne Family Foundation, and the American Foundation for Suicide Prevention and book royalties from Guilford Press and John Wiley & Sons.
Contributions:
Dr. O’Donnell contributed to the data analysis, data interpretation, and writing of the manuscript.
Dr. Ellis contributed to the data analysis, data interpretation, and writing of the manuscript.
Ms. Van de Loo contributed to the writing of the manuscript.
Dr. Stange contributed to the data analysis, data interpretation, and writing of the manuscript.
Dr. David Axelson directed two of the three study sites and contributed to the development of the protocol and writing of the manuscript
Dr. Chris Schneck was a primary physician for the study and managed patients’ pharmacotherapy, supervised other physicians, tabulated data on patients’ medication regimens and contributed to the writing of this manuscript.
Dr. Miklowitz directed the third study site, contributed to the development of the protocol, contributed to the data analysis, interpretation, and writing of the manuscript.
References
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the kiddie schedule for affective disorders and schizophrenia for school-age children mania rating scale for children and adolescents. Journal of Child and Adolescent Psychopharmacology. 2003;13(4):463–70. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D. Course and outcome of bipolar spectrum disorder in children and adolescents: a review of the existing literature. Dev Psychopathol. 2006;18:1023–1035. doi: 10.1017/S0954579406060500. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry. 2009a;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Yang M, Ryan N, Goldstein B, Hunt J, Esposito-Smythers C, Iyengar S, et al. Comparison of manic and depressive symptoms between children and adolescents with bipolar spectrum disorders. Bipolar Disord. 2009b;11:52–62. doi: 10.1111/j.1399-5618.2008.00659.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Goldstein BI, Axelson DA, Monk K, Hickey MB, Fan J, Iyengar S, Ha W, Diler RS, Goldstein T, et al. Mood lability among offspring of parents with bipolar disorder and community controls. Bipolar Disord. 2013;15:253–263. doi: 10.1111/bdi.12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bondurant H, Greenfield B, Tse SM. Construct Validity of the Adolescent Borderline Personality Disorder: A Review. The Canadian Child and Adolescent Psychiatry Review. 2004;13(3):53–57. [PMC free article] [PubMed] [Google Scholar]
- Bonsall MB, Wallace-Hadrill SM, Geddes JR, Goodwin GM, Holmes EA. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc R Soc B The Royal Society. 2012:916–924. doi: 10.1098/rspb.2011.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen R. Mood Instability is the distinctive feature of neuroticism. Results from the British Health and Lifestyle Study (HALS) Personality and Individual Differences. 2012;53:896–900. [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch Gen Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Clayton PJ, Ernst C, Angst J. Premorbid personality traits of men who develop unipolar or bipolar disorders. Eur Arch Psychiatry Clin Neurosci. 1994;243:340–346. doi: 10.1007/BF02195728. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164:582–590. doi: 10.1176/ajp.2007.164.4.582. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer U, Trull TJ. Ecological momentary assessment of mood disorders and mood dysregulation. Psychol Assess. 2009;21:463–475. doi: 10.1037/a0017075. [DOI] [PubMed] [Google Scholar]
- Geller B, Bolhofner K, Craney JL, Williams M, DelBello MP, Gundersen K. Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry. 2000;39:1543–1548. doi: 10.1097/00004583-200012000-00018. [DOI] [PubMed] [Google Scholar]
- Gitlin MJ, Mintz J, Sokolski K, Hammen C, Altshuler LL. Subsyndromal depressive symptoms after symptomatic recovery from mania are associated with delayed functional recovery. J Clin Psychiatry. 2011;72:692–697. doi: 10.4088/JCP.09m05291gre. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Ha W, Axelson DA, Goldstein BI, Liao F, Gill MK, Ryan ND, Yen S, Hunt J, Hower H, et al. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Arch Gen Psychiatry. 2012;69:1113–1122. doi: 10.1001/archgenpsychiatry.2012.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafeman DM, Merranko J, Axelson D, Goldstein BI, Goldstein T, Monk K, Hickey MB, Sakolsky D, Diler R, Iyengar S, et al. Toward the definition of a bipolar prodrome: dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016;173:695–704. doi: 10.1176/appi.ajp.2015.15040414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry C, Mitropoulou V, New AS, Koenigsberg HW, Silverman J, Siever LJ. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35:307–312. doi: 10.1016/s0022-3956(01)00038-3. [DOI] [PubMed] [Google Scholar]
- Henry C, Van den Bulke D, Bellivier F, Roy I, Swendsen J, M’Baïlara K, Siever LJ, Leboyer M. Affective lability and affect intensity as core dimensions of bipolar disorders during euthymic period. Psychiatry Res. 2008;159:1–6. doi: 10.1016/j.psychres.2005.11.016. [DOI] [PubMed] [Google Scholar]
- Hirschfeld R, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003 [PubMed] [Google Scholar]
- Hollingshead AB, Redlich FC. Social class and mental illness: Community study. 1958 doi: 10.2105/ajph.97.10.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychol Methods. 2008;13:354. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kochman FJ, Hantouche EG, Ferrari P, Lancrenon S, Bayart D, Akiskal HS. Cyclothymic temperament as a prospective predictor of bipolarity and suicidality in children and adolescents with major depressive disorder. J Affect Disord. 2005;85:181–189. doi: 10.1016/j.jad.2003.09.009. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW. Affective instability: toward an integration of neuroscience and psychological perspectives. J Personal Disord. 2010;24:60–82. doi: 10.1521/pedi.2010.24.1.60. https://doi.org/10.1521/pedi.2010.24.1.60. [DOI] [PubMed] [Google Scholar]
- Marwaha S, Broome MR, Bebbington PE, Kuipers E, Freeman D. Mood instability and psychosis: analyses of British national survey data. Schizophr Bull. 2013;40:269–277. doi: 10.1093/schbul/sbt149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marwaha S, He Z, Broome M, Singh SP, Scott J, Eyden J, Wolke D. How is affective instability defined and measured? A systematic review Psychol Med. 2014;44:1793–1808. doi: 10.1017/S0033291713002407. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Schneck CD, George EL, Taylor DO, Sugar CA, Birmaher B, Kowatch RA, DelBello MP, Axelson DA. Pharmacotherapy and family-focused treatment for adolescents with bipolar I and II disorders: a 2-year randomized trial. Am J Psychiatry. 2014;171:658–667. doi: 10.1176/appi.ajp.2014.13081130. https://doi.org/10.1176/appi.ajp.2014.13081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JD, Pilkonis PA. Neuroticism and affective instability: the same or different? Am J Psychiatry. 2006;163:839–845. doi: 10.1176/ajp.2006.163.5.839. [DOI] [PubMed] [Google Scholar]
- Olsen BT, Ganocy SJ, Bitter SM, Findling RL, Case M, Chang K, Tohen M, DelBello MP. Health-related quality of life as measured by the child health questionnaire in adolescents with bipolar disorder treated with olanzapine. Compr Psychiatry. 2012;53:1000–1005. doi: 10.1016/j.comppsych.2012.03.010. [DOI] [PubMed] [Google Scholar]
- Patel R, Lloyd T, Jackson R, Ball M, Shetty H, Broadbent M, Geddes JR, Stewart R, McGuire P, Taylor M. Mood instability is a common feature of mental health disorders and is associated with poor clinical outcomes. BMJ Open. 2015;5:e007504. doi: 10.1136/bmjopen-2014-007504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs GS, Nierenberg AA, STEP-BD Investigators Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biol Psychiatry. 2004;55:875–881. doi: 10.1016/j.biopsych.2004.01.022. [DOI] [PubMed] [Google Scholar]
- Post RM, Leverich GS, McElroy S, et al. Prevalence of axis II comorbidities in bipolar disorder: relationship to mood state. Bipolar Disorders. 2018;00:1–10. doi: 10.1111/bdi.12596. [DOI] [PubMed] [Google Scholar]
- Propper L, Ortiz A, Slaney C, Garnham J, Ruzickova M, Calkin CV, O’donovan C, Hajek T, Alda M. Early-onset and very-early-onset bipolar disorder: distinct or similar clinical conditions? Bipolar Disord. 2015;17:814–820. doi: 10.1111/bdi.12346. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children’s global assessment scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Stange JP, Kleiman EM, Sylvia LG, da Magalhães PVS, Berk M, Nierenberg AA, Deckersbach T. Specific Mood Symptoms Confer Risk For Subsequent Suicidal Ideation in Bipolar Disorder With and Without Suicide Attempt History: Multi-Wave Data From STEP-BD. Depress Anxiety. 2016;33:464–472. doi: 10.1002/da.22464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strejilevich SA, Martino DJ, Murru A, Teitelbaum J, Fassi G, Marengo E, Igoa A, Colom F. Mood instability and functional recovery in bipolar disorders. Acta Psychiatr Scand. 2013;128:194–202. doi: 10.1111/acps.12065. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Goodman R. Mood lability and psychopathology in youth. Psychol Med. 2009;39:1237–1245. doi: 10.1017/S0033291708004662. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, Watson D. Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. J Abnorm Psychol. 2008;117:647. doi: 10.1037/a0012532. [DOI] [PubMed] [Google Scholar]


