Abstract
The current investigation examined if changes in youth internalizing problems as a result of a Family Group Cognitive-Behavioral (FGCB) preventive intervention for families with a parent with a history of depression had a cascade effect on youth social problems over 24 months and the bidirectional nature of these effects. One hundred and eighty families with a parent with a history of MDD (Mage = 41.96; 88.9% mothers) and a youth in the age range of 9-to-15 years (49.4% females; Mage = 11.46) participated. Findings from a panel model indicated that, compared to a minimum intervention condition, the FGCB intervention significantly reduced youth internalizing problems at 12 months which, in turn, were associated with lower levels of social problems at 18 months. Similarly, the FGCB intervention reduced internalizing problems at 18 months, which were associated with fewer social problems at 24 months. Changes in social problems were not related to reductions in subsequent internalizing problems. Findings suggest that reductions in youth internalizing problems can lead to lower levels of social problems. Youth social problems are difficult to change; therefore, targeting internalizing problems may be an effective way to reduce the social problems of children of parents with a history of depression.
Keywords: Parental depression, prevention, internalizing, social problems
Children of Parents with a History of Depression: The Impact of a Preventive Intervention on Youth Social Problems through Reductions in Internalizing Problems
Parental depression can have a widespread impact on children's psychological, behavioral, and social functioning (see Goodman, Rouse, Connell, Broth, Hall, & Heyward, 2011; Goodman & Tulley, 2006 for reviews). Given that an estimated 15 million youth in the United States live with a depressed parent, parental depression stands as a significant public health concern (England & Sim, 2009). In fact, having a parent with depression portends a three to four times greater risk for developing depression (England & Sim, 2009) and is one of the biggest risk factors for a first episode of major depressive disorder (MDD) in children and adolescents (Beardslee, Gladstone, & O'Connor, 2011). Furthermore, parents with a history of depression continue to exhibit difficulties that contribute to a stressful family environment for their children even when they are not in an episode of depression (Seifer, Dickstein, Sameroff, Magee, & Hayden, 2001). Recent preventative research suggests that both the parenting of parents with a history of depression and children's coping can be altered and these changes, in turn, can lead to lower youth internalizing problems (Compas et al., 2010). However, research is needed to elucidate some of the more distal outcomes of preventative programs that may have profound effects on youth functioning such as youth social problems (e.g., does not get along well with peers) as well as the cascading effects of the problems of these youth over time.
Research indicates that children of depressed parents (Goodman & Tulley, 2006) and children with internalizing problems (e.g., Hoglund & Chisholm, 2014; Kochel, Ladd, & Rudolph, 2012) tend to have significant problems in peer relationships (e.g., conflict, rejection). In addition, previous research indicates that problems in the peer group (e.g., exclusion) are related to increases in internalizing problems over time (e.g., Hoglund & Chisholm, 2014; Reijntjes, Kamphuis, Prinzie, & Telch, 2010). However, to our knowledge, no research to date has explored if internalizing problems of youth living in families with a history of depression play a role in youth social problems nor if changes in the social problems of these youth are related to changes in internalizing problems. Thus, the current study utilized an intervention framework to determine if reductions in youth internalizing problems as a result of a prevention program for families with a parent with a history of depression (Compas et al., 2009, 2011, 2015) had a cascading effect on youth social problems over 24 months and if changes in youth social problems altered youth internalizing problems over this same time period. Because this was the first investigation into the proposed model, a global definition of social problems was adopted in the current study. This broad definition of social problems includes the behavioral indicators (e.g., not liked, not getting along with others), antecedents (e.g., clumsiness, speech problems), and consequences (e.g., appears lonely) of rejection as well as social interaction style (e.g., dependent, prefers younger children).
This Family Group Cognitive-Behavioral (FGCB) preventive intervention targeted families with a mother or father with a history of MDD and included components to teach parenting skills rooted in behavioral parent training (e.g., praise for appropriate behavior; McMahon & Forehand, 2003) and youth coping skills (e.g., engaging in fun activities and positive thinking). Prior research has demonstrated that, relative to a minimum intervention comparison condition (i.e., written information condition), the youth in the preventive intervention program displayed decreased internalizing problems at 6-month, 12-month, 18-month, and 24-month follow-ups (Compas et al., 2009, 2011, 2015). An important continued area of inquiry is if the changes in the more proximal outcomes (e.g., internalizing problems) targeted by this cognitive-behavioral program have cascading effects on other areas of these youths’ lives. An area of particular importance is the social problems of children of depressed parents. Research suggests that children of depressed parents have more chronic and severe problems in relationships and interactions with peers compared to their peers who live with non-depressed parents (e.g., rejection, problems in social interactions; Feurer, Hammen, & Gibb, 2016; Goodman & Tulley, 2006; Weissman et al., 1997). Furthermore, research with depressed children of depressed mothers indicated that these youth were not simply impaired in all domains (e.g., academic functioning), but were impaired in the interpersonal domain specifically (Hammen & Brennan, 2001).
Researchers have theorized that some children of depressed parents struggle interpersonally because they observe, and learn from, the social interactions of their depressed parent who may have a wide variety of relationship difficulties him or herself (Hammen & Brennan, 2001). These youth may also suffer socially due to an unwillingness or inability of their depressed parent to manage and support their child's interpersonal activities and skills, therefore hindering their opportunities to develop positive peer relationships (Dodge, 1990; Zahn-Waxler, Cummings, Iannotti, R. J., & Radke-Yarrow, 1984).
However, there may be multiple pathways through which parental depression impacts youth social problems. One such pathway is through internalizing problems. Extant research indicates that children with internalizing problems experience higher levels of rejection (Agoston & Rudolph, 2013; Hoglund & Chisholm, 2014), lower social acceptance (Brendgen, Vitaro, Turgeon, & Poulin, 2002; Henricsson & Rydell, 2006; Kochel et al., 2012), and other related social problems (e.g., victimization; Hoglund & Chisholm, 2014; Leadbeater & Hoglund, 2009; Kochel et al., 2012; Reijntjes et al., 2010; Snyder et al., 2003). In fact, Rudolph, Flynn, and Abaied (2008) suggest that not only can early family disruption (e.g., parental depression) impact youth social problems by hindering the development of adaptive social behaviors via direct socialization, but the accompanying increased vulnerability (e.g., genetic, modelling) for internalizing problems may also directly impact social problems. Specifically, the impairment and stable characteristics of youth with internalizing problems (e.g., negative bias toward peers, reassurance seeking, ineffective coping) induce a stressful interpersonal context for the youth, therefore placing them at further risk for psychopathology. For example, the behavioral tendencies of youth with internalizing problems (e.g., cries a lot, too fearful or anxious, withdrawn) may provoke negative responses (e.g., rejection) from peers who view these youth as too sensitive to play with or as unattractive social partners (Hoglund & Chisholm, 2014; Morrow, Hubbard, McAuliffe, Rubin, & Dearing, 2006; Pedersen, Vitaro, Barker, & Borge, 2007; Van Lier & Koot, 2010). These children may also show little enjoyment when interacting with peers or may have difficulty successfully joining into peer activities (Hoglund & Chishold, 2014). As another example, internalizing problems may also be associated with aggressive behaviors (Angold et al., 1999; Crick & Grotpeter, 1995), perhaps because the internalizing-associated irritability of these youth leads to defensive and hostile interactions with peers (Agoston & Rudolph, 2013). As such, this aggression may then lead to increased problems in the peer group (e.g., rejection; Agoston & Rudolph, 2013).
These peer difficulties, in turn, have been shown to perpetuate risk for future internalizing problems (e.g., Hoglund & Chisholm, 2014; Schleider, Ginsburg, & Drake, 2017), perhaps because such experiences reinforce the negative self-evaluations of these youth (Reijntjes et al., 2010). A strength of Rudolph and colleagues' (2007) developmentally-based interpersonal model of youth depression lies in the fact that the bidirectional nature of the relation between internalizing and social problems is emphasized. These relations are transactional in nature and may help explain the continuity of internalizing problems across the lifespan (Hoglund & Chisholm, 2014). Additionally, social problems (e.g., rejection) amplify risk for aggression and delinquency (Coie & Dodge, 1998), which are related to a host of other negative outcomes (e.g., criminality; Simons, Wu, Conger, & Lorenz, 1994). Therefore, youth social problems are integrally important to understanding the psychopathology often observed in children of depressed parents that may have an impact at both individual (e.g., depression) and societal (e.g., crime) levels.
There is reason to suspect that the hypothesized bidirectional relations between internalizing and social problems would be moderated by youth gender. First, girls have higher rates of internalizing problems than boys, beginning in early adolescence (Crick & Zahn-Waxler, 2003). Second, girls’ relationships are characterized by more intimacy, self-disclosure, and emotional support than those of boys (Rudolph, 2002). Because of these relationship characteristics, threats to interpersonal relationships (e.g., rejection) are particularly harmful for girls and are specifically related to internalizing problems (see also Taylor et al., 2000). Third, research by Rudolph, Ladd, and Dinella (2007) found that internalizing problems were related to social problems (i.e., fewer reciprocal friendships, reductions in friendship quality) in girls but not in boys. They theorized that, because the intimate nature of girls’ relationships requires heightened emotional energy, the symptoms of girls with internalizing problems (e.g., fatigue, lack of motivation, difficulties with emotion regulation, social disengagement) may interfere with successful navigation of peer relationships. In contrast, boys generally demand less emotional support from their male peers; as such, male peer relationships may be less impacted by the impairments associated with internalizing difficulties. Therefore, it is possible that social problems are more salient predictors of cascading problems in multiple domains for girls than for boys (Goodman & Tulley, 2006).
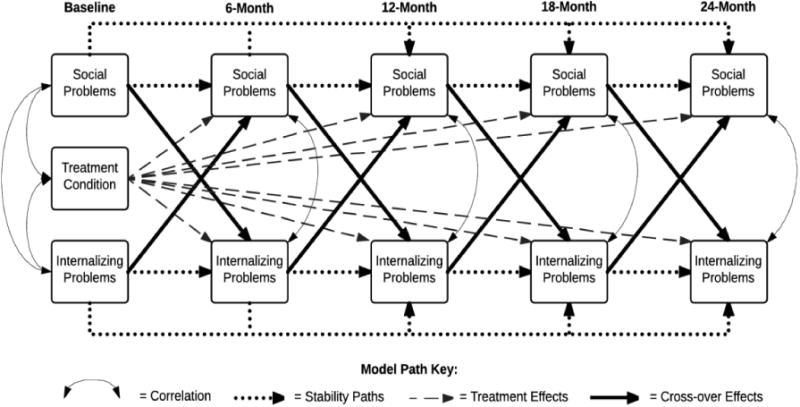
In summary, research suggests that children of depressed parents have elevated internalizing problems and higher rates of social problems, internalizing problems are associated with increases in social problems (e.g., Hoglund & Chisholm, 2014), and social problems are associated with increases in internalizing problems (Reijntjes et al., 2010). However, it remains to be investigated if reducing youth internalizing problems has a meaningful impact on social problems and if this has a cascade effect on future internalizing problems. Thus, the primary goal of the current study was to utilize an intervention framework to examine if changes in internalizing problems of youth living with a parent with a history of depression resulting from a cognitive-behavioral prevention (Bettis, Forehand, Sterba, Preacher, & Compas, in press; Compas et al., 2009, 2011, 2015) had a cascade effect on youth social problems and if changes in social problems had an impact on youth internalizing problems. Developmental cascades reflect the processes through which functioning in one domain has an impact on other areas of functioning over time; these cascades are also known as spill-over effects, chain reactions, and amplification effects (Masten & Cicchetti, 2010). In intervention designs, cascade models demonstrate that targeted change in one area of functioning (e.g., internalizing problems) can lead to change in other domains (e.g., social problems). The testing of cascade models requires longitudinal data, repeated assessment (i.e., at least three time points), and accounting for the stability of variables over time (Masten & Cicchetti, 2010). The current study was uniquely equipped to investigate if the attempted alteration (i.e., FGCB intervention) of internalizing problems had a cascade effect on social problems and subsequent internalizing problems over time using longitudinal, repeated assessments, and rigorous statistical methodology. See Figure 1 for an overview of the within-wave correlation, stability, treatment, and cascade effect pathways examined in the current study.
Figure 1. Overview of within-wave correlation, stability, treatment, and cascade effect pathways examined in the current study.
The selected age range (9-15 years old) for this intervention program is particularly well-suited for an investigation of both internalizing and social problems. Internalizing problems tend to escalate in early adolescence, especially in girls (e.g., Nolen-Hoeksema, 2001). This program represents a “well-timed” intervention (Masten & Cicchetti, 2010) in that it sought to prevent the emergence and/or escalation of internalizing problems at a time when these symptoms often increase. In addition, youth begin to spend more time with peers and place greater importance on acceptance within the peer group during this time period (Brown, Clasen, & Eicher, 1986). As such, a reduction in social problems during this developmental period would reflect an improvement in a domain that is particularly salient and meaningful for preadolescent and adolescent youth.
Prior research on this intervention indicates that, relative to those in the minimum intervention condition, youth of families in the cognitive-behavioral intervention exhibit a significant decrease in internalizing problems at the 6, 12, 18, and 24-month follow-ups (see Compas et al., 2015). We hypothesized that reductions in internalizing problems would lead to reductions in social problems over 24 months. We also predicted that these reductions in social problems would be associated with further reductions in internalizing problems. In other words, we expected that the cognitive-behavioral preventive intervention would have a cascade effect on youth social problems and internalizing problems due to initial reductions in internalizing problems over and above direct treatment effects and stability of social problems over time. Finally, we expected that gender would moderate any significant effect in our model such that the pathway would be stronger for girls than for boys.
Method
Participants
One hundred and eighty families, all of which had at least one caregiver with a history of MDD and one child in the target age range of 9 to 15 (49.4% [89] females; Mage = 11.46; SD = 2.00), were recruited from the larger Burlington, Vermont, and Nashville, Tennessee, communities and included in current analyses. The majority of the target parents (i.e., those identified as having a history of MDD) were mothers (88.9%; 160), married (61.7%), and were educated at the high school level (31.7% with 4-year college degree; 23.3% with graduate education) at baseline. Although participant ethnic composition was primarily Caucasian, with 25.6% of youth identifying as racial/ethnic minorities (12.8% Black or African American, 3.3% Asian, 1.7% Latino or Hispanic, 0.6% American Indian or Alaska Native, and 7.2% mixed race), the ethnic makeup of participants was, according to 2000 US Census data, representative of the regions from which they were drawn. Forty-eight participants (27%) were in a current episode of depression at the baseline assessment.
Procedure
Families were recruited via flyers, newspaper and radio advertisements, and referrals from physicians. Interested parents were initially screened over the telephone, followed by an in-person visit to determine eligibility. Participating parents were compensated $40 per participating child at four assessments and $15 for the 18-month assessment which required less effort. Each participating youth was similarly compensated.
Inclusion criteria for parents consisted of a history of MDD during the lifetime of the target child(ren) based on the Structured Clinical Interview for DSM (SCID; First, Spitzer, Gibbon, & Williams, 2001). Parental exclusion consisted of a history of bipolar I disorder, schizophrenia, or schizoaffective disorder. These exclusionary criteria were utilized to form a sample whose primary diagnostic history was depression.
Youth in the age range of 9-15 years old were eligible based on the Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime Version (Kaufman et al., 1997) if they were free of lifetime diagnoses of autism spectrum disorders, mental retardation, bipolar I disorder, and schizophrenia, and if they did not currently meet criteria for conduct disorder or alcohol/substance use disorders These exclusionary criteria were utilized to form an at-risk (i.e., due to parental history of depression) sample that did not meet criteria for diagnoses that may limit the preventive intervention. The current sample included 16.7% of youth with a history of depression.
Eligible families were deferred for later assessment if the parent was currently suicidal with a Global Assessment of Functioning score of ≤50 on the SCID, if the parent had a current alcohol/substance abuse or dependence with a Global Assessment of Functioning score of ≤50 on the SCID, and/or if the youth met criteria for current depression at screening. These families were assisted in obtaining appropriate mental health services in the community. Deferred families were re-screened every two (if reason for deferral was suicidality or youth depression) or six (if reason for deferral was alcohol/drug problems) months until they screened eligible and could be invited to the next stage of recruitment.
Family group intervention
As demonstrated in Figure 2, 180 eligible families were randomized to the FGCB intervention (50% of current sample) or to a written information (WI; 50% of current sample) comparison condition. The FGCB condition included eight weekly group meetings and four monthly follow-up sessions with several other families. This program was designed such that both parents and youth were active participants; in the majority of sessions, parent and youth groups met separately. Both parents and youth received psychoeducation about depression and its effect on the family. Parents learned about effective parenting skills (i.e., praise, positive time with youth, encouragement of youth coping skills, structure, and consequences for problematic youth behavior). Youth sessions involved learning skills for coping with their parents’ depression. Specifically, youth learned secondary coping skills summarized by the acronym ADAPT: Acceptance, Distraction, Activities, and Positive Thinking. See Compas et al., 2009 and 2011 for more details about this intervention.
Figure 2. Participant screening and randomization.
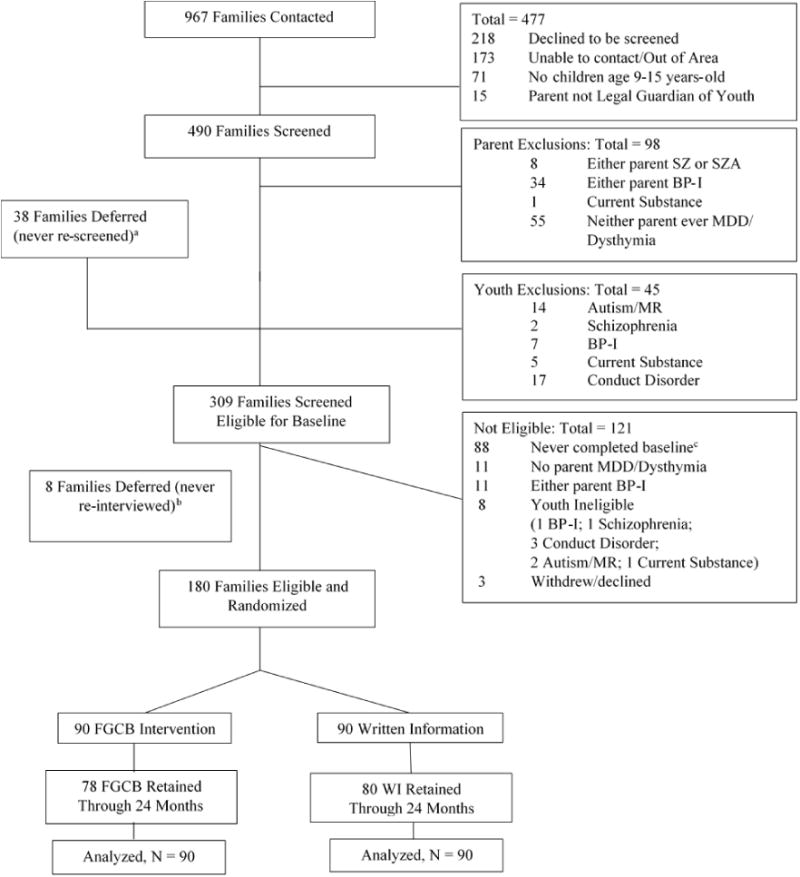
a = 15 families deferred due to youth MDE; b = 5 families deferred due to youth MDE; c = 8 youth not interested; 56 parent not interested; 3 families moved; 1 parent not legal guardian; 19 not reachable; 1contacted study after enrollment closed
Sessions were co-facilitated by one of three clinical social workers and one of nine doctoral-level clinical graduate students and were supervised by two Ph.D.-level clinical psychologists.
Treatment adherence and integrity
Treatment participation was adequate for families (parents and youth) randomized to the FGCB condition as demonstrated by the following: 1) the number of group sessions attended or made up after an absence by at least one family member averaged 7.9 sessions (out of 12), 2) for those who attended at least one session, the mean number of sessions attended or made up after an absence was 10.5 sessions, and 3) almost 70% of families attended more than one-half of the 12 sessions.
In order to evaluate the fidelity of the youth and parent group intervention sessions, a detailed list was made of the manualized content of each intervention session. Five individuals who were not involved in the delivery of the intervention were trained to code for the presence or absence of each content area. All sessions were audio recorded and 23% were selected for fidelity coding. There was a 92% agreement rate between the number of items that should have been covered in the sessions and the number that were actually covered. Additionally, 31% of the fidelity-coded tapes were selected for reliability coding; inter-rater agreement was 93%.
Written information self-study condition
Families in the WI self-study control condition (i.e., minimum intervention condition) were mailed three separate youth and parent packets of psychoeducational readings over an 8-week period regarding depression, signs of depression in youth, and effects of parental depression on families (for more detailed information about the readings, see Compas et al., 2009). Families were provided with a schedule for reading these materials but were otherwise left to engage with these materials on their own.
Retention
Families in both the FGCB and the WI conditions completed questionnaires at six time points, five of which were utilized in the current study (i.e., baseline, 6-month follow-up, 12-month follow-up, 18-month follow-up, and 24-month follow-up). Ninety-three percent of families (92% and 93% in FGCB and WI, respectively) remained enrolled at 18 months (i.e., 7% of families withdrew from the study), and eighty-eight percent of the families (87% and 89% in FGCB and WI, respectively) completed data collection through the 24-month follow-up, defined by the provision of data at any or all of the follow-ups. For families with more than one eligible child who participated in the study, the present analyses utilized one randomly selected child per family as determined by a random number generator.
Measures
Demographic information
Target parents provided demographic information about themselves (e.g., parental age, education) and their families (e.g., household income). Youth also reported demographic information (e.g., gender, age).
Youth internalizing and social problems
The Youth Self-Report for Ages 11-18 (YSR/11-18; Achenbach & Rescorla, 2001) is a widely-used, nationally-normed assessment of youth behavioral and emotional problems. The YSR consists of 118 items and has been found to generalize across 23 countries (Ivanova et al., 2007). Using a 0 (not true) to 2 (very or often true) scale, youth describe how well various statements describe their symptoms/behaviors over the past six months. Children as young as 7 years can complete the measure (Ebesutani, Bernstein, Martinez, Chorpita, & Weisz, 2011) and there is adequate internal consistency for the YSR scales among 9 and 10 year olds (i.e., all α ≥ .80; see Compas et al., 2009). See Table 1 for internal consistencies in current study1. Consistent with prior research (e.g., Compas et al., 2009, 2011), raw scores were utilized in analyses to maximize variance.
Table 1. Descriptive Statistics and Bivariate Correlations.
| M | S.D. | Skewness (S.E.) | α | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Condition | -- | -- | -- | -- | −.037 | −.019 | .137 | .132 | .233 | .123 | .153 | .086 | .089 | .110 |
| 2. Internalizing Baseline | 13.57 | 9.50 | .26 (.36) | .90 | -- | .779 | .554 | .472 | .427 | .336 | .414 | .374 | .377 | .348 |
| 3. Social Baseline | 4.45 | 3.57 | .84 (.36) | .72 | -- | .377 | .502 | .417 | .516 | .350 | .457 | .368 | .465 | |
| 4. Internalizing 6-month | 9.20 | 7.98 | 1.04 (.42) | .89 | -- | .723 | .717 | .508 | .755 | .604 | .588 | .420 | ||
| 5. Social 6-month | 3.54 | 3.11 | 1.76 (.42) | .82 | -- | .553 | .653 | .571 | .676 | .387 | .508 | |||
| 6. Internalizing 12-month | 9.62 | 8.79 | 3.86 (.43) | .92 | -- | .685 | .741 | .649 | .584 | .509 | ||||
| 7. Social 12-Month | 3.40 | 2.98 | .05 (.43) | .78 | -- | .601 | .727 | .430 | .622 | |||||
| 8. Internalizing 18-month | 8.61 | 8.00 | .62 (.45) | .89 | -- | .715 | .746 | .490 | ||||||
| 9. Social 18-month | 3.21 | 2.91 | 1.21 (.45) | .76 | -- | .431 | .590 | |||||||
| 10. Internalizing 24-month | 9.05 | 7.91 | 2.39 (.44) | .88 | -- | .685 | ||||||||
| 11. Social 24-month | 3.52 | 3.11 | .45 (.44) | .66 | -- |
Note: r ≥ .23 = p < .05
Youth internalizing problems
The broadband Internalizing Problems scale is compromised of the Anxious/Depressed (e.g., “I worry a lot”, “I feel worthless or inferior”), Withdrawn/Depressed (e.g., “I am unhappy, sad, or depressed”, “I keep from getting involved with others”), and Somatic Complaints (e.g., “I feel overtired without good reason”) narrowband subscales. The mean T score of internalizing problems averaged across participants in FGCB and WI groups on the YSR was 54.6 at baseline, indicating some elevated risk for the primary variable of interest in the current study.
Youth social problems
The Social Problem subscale of the YSR was used to assess social problems in the current study. The YSR Social Problem subscale contains 11 items related to several areas of social functioning, including peer rejection (e.g., “I am not liked by other kids”, “I don’t get along with other kids”), social interaction style (e.g., “I’m too dependent on adults”, “I would rather be with younger kids than kids my own age”), the impact of peer rejection (e.g., “I feel lonely”), and behaviors that are associated with peer rejection (e.g., “I am poorly coordinated or clumsy”, “I have a speech problem”). Scores on this subscale are significantly related to cross-informant (i.e., parent, teacher) ratings of these behaviors (Achenbach & Rescorla, 2001) and to other indices of social maladjustment (i.e., peer victimization; McQuade, Breslend, & Groff, manuscript in preparation; Schwartz et al., 1999). Mean T scores averaged across participants in FGCB and WI groups on the Social Problem subscale was 57.7 at baseline, indicating elevated risk.
Data analytic plan
Evaluation of the cascade model
Path analysis was conducted utilizing Mplus 7.0 software (Muthén & Muthén, 2010) and used to test the hypothesized cascading effect panel model (see Figure 1). To account for skewed data, maximum likelihood estimation with robust standard errors (MLR) was used. When robust maximum likelihood estimation is implemented, standard errors and chi-square test statistics are statistically corrected to enhance the robustness of ML against departures from normality (Muthén & Muthén, 2010). Missing data for core variables was 2.2%, 27.2%, 31.7%, 37.2%, and 33.3% at baseline, 6-month, 12-month, 18-month, and 24-month follow-ups, respectively. Rates of missingness were similar for treatment and control conditions. The mechanism of missingness was treated as ignorable (missing completely at random, Little's MCAR test p > .05 for both treatment and control conditions) and full information maximum likelihood estimation techniques were used for inclusion of all available data and an intent-to-treat analysis. The following fit statistics were employed to evaluate model fit: Chi-square, χ2: p > .05 excellent, Comparative Fit Index (CFI; > .90 acceptable, > .95 excellent), Root Mean Square Error of Approximation (RMSEA; < .08 acceptable, < .05 excellent) and the Standardized Root Mean Square Residual (SRMR; < .08 acceptable, < .05 excellent) (Hu & Bentler, 1999). Additionally, to test the significance of the indirect effects, the Model Indirect command in Mplus was utilized to calculate a standardized indirect effect parameter and biased-corrected bootstrap confidence intervals.
Covariate and Youth Gender Analyses
Although not included in the proposed conceptual model, the effects of theoretically relevant demographic covariates (i.e., youth age, youth gender, and parent education as an indicator of family socioeconomic status) on the model were examined by running a multiple-indicator/multiple-cause (MIMIC; Muthén, 1989) model in which all major constructs of the final structural model were regressed on the covariates. If paths in the structural model remained significant and without substantial changes in effect size with the inclusion of these covariates, it was concluded that the demographic covariates did not influence the relationships among variables in the model. Additional checks were utilized for the influence of youth gender on the model such that for any significant treatment or cross-over effect in the model, an additional model included an interaction effect with youth gender to examine if gender moderated associations.
Results
Cascade effect model
A cascade effects model was tested with youth internalizing problems and youth social problems at baseline, 6-month, 12-month, 18-month, and 24-month follow-ups. Four different types of paths were modeled: within-wave correlation, stability, cross-over, and treatment effects (see Figure 1 for a depiction of each pathway type). For each follow-up wave of internalizing and social problems, stability pathways were estimated for the two previous waves (e.g., 12-month internalizing regressed on 6-month and baseline internalizing) to account for continuity of each problem behavior. In regard to treatment effects, each follow-up of internalizing and social problems was regressed on treatment assignment to account for direct treatment effects. Lastly, in regard to cross-over or cascade effect pathways, each follow-up of internalizing and social problems was regressed on the other variable in the previous wave (e.g., social problems at 24 months regressed on internalizing problems at 18 months) to examine if improvements in one domain led to improvements in another. Model testing proceeded in four steps: all hypothesized pathways estimated; nested model comparisons to validate cross-over effects; covariate sensitivity analyses; and finally gender moderation of key pathways.
The primary model (Figure 1) with all the above described effects demonstrated excellent fit, (χ2 [18, N = 178] = 17.76, p = .47, RMSEA = .00, 95% CI .000 to .066, CFI = 1.0, SRMR = .031). The standardized estimates of this final model are presented in Table 2 along with bias-corrected bootstrap confidence intervals. Figure 3 displays significant standardized estimates with non-significant pathways removed from the diagram. As hypothesized and consistent with previous outcome studies (Compas et al., 2015), youth randomized to the FGCB intervention reported lower levels of internalizing problems at the 6-month and 12-month follow-ups than those in the WI condition. To account for immediate and direct intervention effects on social problems, we tested the direct effect of intervention condition on social problems at each follow-up. A direct effect of intervention on 6-month social problems was observed such that youth randomized to the FGCB intervention reported lower levels of social problems at the 6-month follow-up relative to youth randomized to the WI condition. In support of hypotheses, youth-reported internalizing problems at 12 months significantly predicted youth social problems at 18 months such that youth who evidenced lower levels of internalizing problems at 12 months evidenced lower levels of social problems at the 18-month follow-up. Additionally, this crossover effect was also significant and in the same direction for the path from internalizing problems at 18 months to social problems at 24 months. However, contrary to expectations, reductions in social problems were not associated with further reductions in internalizing problems.
Table 2. Results from the Final Structural Model.
| β | p | 95% CI | p Value | |
|---|---|---|---|---|
| Internalizing 6-Month | ||||
|
| ||||
| ON Internalizing Baseline | .51 | .60 | .37, .83 | .000 |
| ON Treatment Condition | −2.47 | −.15 | −.29, -.02 | .023 |
| WITH Social 6-Month | 11.55 | .67 | .58, .77 | .000 |
| ON Social Baseline | −.12 | −.06 | −.32, .21 | .688 |
|
| ||||
| Social 6-Month | ||||
|
| ||||
| ON Social Baseline | .34 | .41 | .13, .68 | .003 |
| ON Treatment Condition | −.87 | −.14 | −.27, −.01 | .042 |
| ON Internalizing Baseline | .05 | .16 | −.06, .39 | .161 |
|
| ||||
| Internalizing 12-Month | ||||
|
| ||||
| ON Internalizing 6−Month | .66 | .60 | .39, .80 | .000 |
| ON Internalizing Baseline | .11 | .12 | −.04, .27 | .139 |
| ON Treatment Condition | −1.97 | −.11 | −.22, −.01 | .047 |
| WITH Social 12-Month | 7.20 | .55 | .40, .71 | .000 |
| ON Social 6-Month | .18 | .06 | −.11, .24 | .492 |
|
| ||||
| Social 12-Month | ||||
|
| ||||
| ON Social 6-Month | .46 | .49 | .26, .72 | .000 |
| ON Social Baseline | .16 | .19 | .03, .36 | .022 |
| ON Treatment Condition | −.11 | −.02 | −.15, .11 | .776 |
| ON Internalizing 6-Month | .03 | .08 | −.17, .32 | .531 |
|
| ||||
| Internalizing 18-Month | ||||
|
| ||||
| ON Internalizing 12-Month | .35 | .38 | .10, .65 | .007 |
| ON Internalizing 6-Month | .52 | .50 | .29, .72 | .000 |
| ON Treatment Condition | −.01 | −.01 | −.11, .11 | .988 |
| WITH Social 18-Month | 4.39 | .50 | .37, .64 | .000 |
| ON Social 12-Month | .01 | .01 | −.15, .16 | .950 |
|
| ||||
| Social 18-Month | ||||
|
| ||||
| ON Social 12-Month | .34 | .35 | .12, .57 | .003 |
| ON Social 6-Month | .30 | .33 | .15, .50 | .000 |
| ON Treatment Condition | −.22 | −.04 | −.16, .09 | .543 |
| ON Internalizing 12-Month | .07 | .22 | .02, .42 | .032 |
|
| ||||
| Internalizing 24-Month | ||||
|
| ||||
| ON Internalizing 18-Month | .76 | .77 | .59, .94 | .000 |
| ON Internalizing 12-Month | .15 | .17 | .01, .33 | .042 |
| ON Treatment Condition | −.13 | −.01 | −.12, .11 | .889 |
| WITH Social 24-Month | 6.69 | .61 | .49, .72 | .000 |
| ON Social 18-Month | −.41 | −.14 | −.32, .03 | .103 |
|
| ||||
| Social 24-Month | ||||
|
| ||||
| ON Social 18-Month | .28 | .26 | .01, .51 | .048 |
| ON Social 12-Month | .34 | .32 | .13, .52 | .001 |
| ON Treatment Condition | −.24 | −.04 | −.17, .10 | .577 |
| ON Internalizing 18-Month | .07 | .19 | −.002, .38 | .052 |
Figure 3. Final model with standardized estimates.
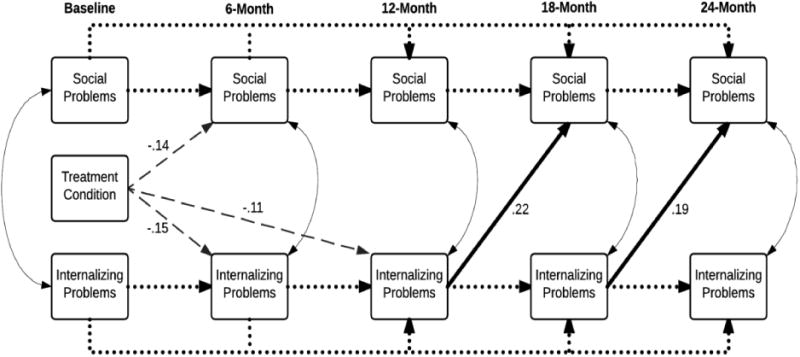
Note: Bolded solid lines are significant pathways of primary interest. Solid lines are statistically significant < .05.
Findings suggested that treatment condition had an indirect effect on youth social problems at 18 months (β = .044, 95% CI -.002 to .09, p = .058) through reductions in youth internalizing problems (i.e., total indirect effect). Individual indirect pathways that contributed to the total indirect effect included: (1) condition to 6-month internalizing to 12-month internalizing to 18-month social problems; and (2) condition to 12-month internalizing to 18-month social problems. Treatment condition also had an indirect effect on youth social problems at 24 months (β = .026, 95% CI .003 to .05, p = .024) through reductions in youth internalizing problems (i.e., total indirect effect). Individual indirect pathways that contributed to the total indirect effect included: (1) condition to 6-month internalizing to 12-month internalizing to 18-month internalizing to 24-month social problems; and (2) condition to 12-month internalizing to 18-month internalizing to 24-month social problems.
In line with previous research testing cascade models (e.g., Burt, Obradovic, Long, & Masten, 2008), we conducted a series of nested model comparisons to further validate cascade effects following estimation of the primary model that tested all hypotheses. The use of the MLR estimator required the use of a scaled chi-square difference test (Satorra, 2000) for making comparisons among nested models. The first nested model comparison was between the primary model presented above (Model 1, Figure 1) and a model that constrained all social problems to internalizing problem pathways to zero (Model 2) given that these effects were unsupported in primary results. Model fit did not significantly deteriorate with the exclusion of these paths (∆ scaled/2 [4] = .07, p = .999). Next, Model 2 was compared to a model that removed initial internalizing problem to social problem cross-over pathways at 6 and 12-month follow-ups (Model 3). Model fit was not affected by the exclusion of these paths (∆ χ2 [2] = 2.76, p = .251). Lastly, and of primary interest, Model 3 was compared to a model that removed all cascade pathways (Model 4, Stability and Treatment Only) to examine if a model with only direct treatment effects and continuity paths outperformed one with these distal follow-up cascade effects on social problems. Model fit significantly deteriorated with the exclusion of these cascade paths (∆ χ2 [2] = 6.37, p < .05). Thus, further supporting hypotheses, the cascade model with cross-over effects from internalizing problems at 12 and 18 months to social problems at 18 and 24-month follow-ups, respectively, was superior to a treatment effect continuity-only model.
Covariate and youth gender analyses
In regard to demographic covariates, MIMIC models tested the demographic effects of youth age, youth gender, youth race, and parent education level (as an indicator of SES) on the associations in the model. All follow-ups of internalizing and social problems were regressed on the covariates in a single model. All previously significant condition and cross-over paths in the structural model remained significant and effect sizes were largely unaffected by the inclusion of these control variables. The only difference between the original and MIMIC models was that the treatment effect on 6-month social problems was reduced to non-significance due to increased standard errors.
In order to more fully explore youth gender, the moderating effect of youth gender on each significant treatment and cross-over effect was tested. The gender by treatment interaction was not significant for internalizing problems at the 6-month (95% CI -.06 to .64), or 12-month (95% CI -.43 to .33) follow-ups and the gender by internalizing problems interaction was not significant for social problems at the 18-month (95% CI -.37 to .16) or 24-month (95% CI -.26 to .03) follow-ups. Lastly, we examined if gender moderated treatment effect paths to social problem outcomes and if gender moderated social problem to internalizing problem cross-over pathways. No support emerged for gender moderation of treatment paths to social problems at 6-month (95% CI -.54 to .19), 12-month (95% CI -.57 to .17), 18-month (95% CI -.48 to .17), or 24-month (95% CI -.43 to .28) follow-ups. Further, no support for gender moderation emerged for any of the cross-over pathways from social problems to internalizing problems at 12-month (95% CI -.48 to .14), 18-month (95% CI -.39 to .34), or 24-month (95% CI -.26 to .07) follow-ups. Together, it was concluded that youth gender and the other demographic control variables did not qualify the findings.
Discussion
Parental depression confers significant risk for the development of youth internalizing problems (Goodman et al., 2011). Children of depressed parents (Goodman & Tulley, 2006) and youth with internalizing problems (e.g., Hoglund & Chisholm, 2014; Kochel et al., 2012) tend to have significant problems in peer relationships. Furthermore, problems in the peer group (e.g., exclusion) are related to increases in internalizing problems over time (e.g., Hoglund & Chisholm, 2014; Reijntjes et al., 2010). However, the extent to which changes in more proximal youth outcomes (e.g., internalizing) cascade into other salient domains (e.g., social problems) of functioning for children of parents with a history of depression and the bidirectionality of these relations have been relatively unexplored. Therefore, the current study was conducted in order to determine if reductions in youth internalizing as a result of a prevention program for families with a parent with a history of depression (Compas et al., 2009, 2011, 2015) had a cascading effect on youth social problems over 24 months and if reductions in social problems predicted lower internalizing problems over the same time period.
As hypothesized and consistent with prior outcome studies (Compas et al., 2015), the FGCB intervention resulted in lower levels of youth internalizing at the 6-month and 12-month follow-ups. Interestingly, engagement in the FGCB intervention was also directly related to lower youth social problems at the 6-month follow-up. Also consistent with expectations, youth in the FGCB intervention displayed lower levels of internalizing problems at 12 months which then predicted lower social problems at 18 months. The same pattern emerged for internalizing problems at 18 months and youth social problems at 24 months. However, and inconsistent with the hypothesized bidirectional effects, social problems were not related to changes in internalizing problems at any of the subsequent waves of measurement. Finally, youth gender did not moderate any of the significant associations in the model.
Parents with a history of depression likely confer biological (i.e., genetic heritability, dysfunctional neuroregulatory mechanisms) and environmental (i.e., exposure to negative parental cognitions, emotions, and behaviors; exposure to contextual stressors) (Goodman & Gotlib, 1999; Rudolph et al., 2008) risk for internalizing problems in their children. Internalizing problems, in turn, may make it difficult for these children to navigate social spheres and meet appropriate developmental tasks in the peer group (e.g., Hoglund & Chishold, 2014; Rudolph et al., 2008). For example, they may have trouble successfully joining into peer activities due to their internalizing problems (e.g., anxious, sad), limiting further opportunities for interaction with peers and making it more difficult to develop as an appropriate social partner (e.g., Hoglund & Chishold, 2014; Morrow et al., 2006; Pederson et al., 2007; Van Lier & Koot, 2010). In addition, they may engage in behaviors (e.g., excessive reassurance seeking, negative bias toward peers, withdrawal, and aggression) that make them unattractive as social partners (Rudolph et al., 2008). Our findings are an important contribution to the growing literature on the role that internalizing problems play in the development of peer problems (e.g., victimization; Hoglund & Chisholm, 2014). The findings also increase our understanding of how parental depression can set in motion processes that impact multiple areas of youth functioning. In order to ascertain the relation between youth internalizing problems and interpersonal functioning, it is necessary to conduct prospective longitudinal research (Rudolph et al., 2008); as such, the current study addressed an important gap in current research and adds to the growing support of Rudolph and colleagues' (2008) developmentally-based interpersonal model of youth depression.
Identifying distal outcomes (e.g., social problems) associated with engagement in a cognitive-behavioral preventive intervention and the mechanisms responsible for this relation may lead to more innovative approaches to intervention with youth with social problems (e.g., seeking to reduce internalizing problems). Indeed, optimally timed interventions may effectively interrupt the progression of negative developmental cascades by reducing problems in areas that often cause problems in other domains (Masten & Cicchetti, 2010). By mapping the pathways to maladjustment for youth with a parent with a history of depression, we may begin to fully understand the substantial ways that youth living with this contextual stressor are impacted in psychological, behavior, and social domains. Perhaps more importantly, we may begin to understand why these youth fare so poorly in multiple domains and target areas for intervention. Youth social problems and social status are difficult to change and the effectiveness of child-focused interventions has been limited (e.g., Hoza et al., 2005; Moote, Smith, & Wodarski, 1999). In fact, interventions that specifically target social skills often raise the social status of youth only minimally (Asher & Hymel, 1986), and oftentimes youth are still rejected, just somewhat less so (e.g., Conduct Problems Prevention Research Group, 1999). There are many plausible reasons for these continued difficulties in the peer group such as a lack of access to socially skilled peers who can reinforce optimal social skills (e.g., Boivin & Hymel, 1997) or the persistence of classroom norms that reinforce the continued mistreatment of a few, selected youth (e.g., Serdiouk et al., 2015). Nevertheless, creative intervention techniques are sorely needed. The findings from the current study suggest that reducing internalizing problems by implementing a program which effectively changes parenting and child coping (Compas et al., 2010) in families with a parent with a history of depression might be a unique, yet effective, way to reduce the social problems of these youth.
Interestingly, findings do not support the existence of a bidirectional relation between internalizing problems and social problems in these youth. In fact, there was no evidence that changes in youth social problems were related to changes in youth internalizing problems across any waves of measurement. These findings are in contrast to previous research (e.g., Hoglund & Chisholm, 2014). However, much of this past research investigated how victimization is related to changes in internalizing problems (Schleider et al., 2017) whereas the current study focused on indicators of rejection. Many researchers view peer rejection as a precursor to peer victimization (e.g., Serdiouk et al., 2013); in fact, some research suggests that victimization helps explain the link between rejection and increased internalizing problems (e.g., Buhs & Ladd, 2001). As such, it is possible that we did not see the hypothesized link between reductions in social problems and reductions in internalizing problems because rejection is less of a predictor of internalizing problems than is peer maltreatment (e.g., victimization). Therefore, future work will benefit from investigating if changes in social problems as measured in the current study (i.e., rejection) are related to changes in peer victimization in order to more fully understand the nature of this complex relation with internalizing problems.
In the current model, gender did not moderate any of the significant pathways. This suggests that reductions in internalizing problems are similarly related to lower social problems for both boys and girls in the current sample. There are several plausible explanations for this finding. First, it is possible that internalizing problems do indeed relate to lower social problems similarly across gender and that the randomized control design of this study mitigated any artefactual gender moderation that may have otherwise emerged. This would be in line with past research that did not find a gender difference in the association between depressive symptoms and perceived peer acceptance (Rudolph et al., 2007). Second, it is possible that this null finding is accurate, but perhaps only for this unique population of at-risk youth. Third, this may be a result of the fact that the social problems in this study focused around peer rejection. Perhaps if social problems that were more strongly related to one gender (e.g., relational victimization; e.g., Cullerton-Sen & Crick, 2005; Kawabata, Crick, & Hamaguchi, 2010) were utilized, significant gender moderation would have emerged.
Limitations and Strengths
The current study was limited in several important ways. First, although the sample was representative of the regions from which it was drawn, it was composed of primarily Caucasian mothers. Future work should seek to include a more racially and socioeconomically diverse sample. Second, parent and/or youth were excluded based on other psychiatric diagnoses (e.g. Bipolar I, schizophrenia). Youth were also excluded if they met criteria for current MDD or conduct disorder. Consequently, the sample is not entirely representative of parents with a history of depression or their children. As such, the incidence of youths’ maladjustment may be underestimated. Therefore, the interpretation of these findings are limited to at-risk youth (i.e., exclusion of some types of youth psychopathology) in families with parents without significant psychopathological comorbidity. Third, the current study did not assess the psychopathology of the second parent unless the parent elected to participate in the intervention. Future research will benefit from collecting systematic data on both parents in the context of a targeted intervention such as this one.
Fourth, we elected to use a broad assessment of social problems in this initial investigation of the processes linking engagement in a prevention program for children of parents with a history of depression to youth social problems. The Social Problem subscale of the YSR focuses primarily on the behavioral indicators, antecedents, and consequences of rejection (although social interaction style is also included). Other negative social interactions that have a detrimental impact on youths’ quality of life should also be investigated (e.g., physical victimization, relational victimization, friendship conflict). By focusing on more specific problems in the peer domain, we may continue to develop and refine targeted prevention and intervention efforts. Additionally, it will be important to examine which aspects of social functioning (e.g., victimization, rejection) are most relevant at different developmental periods and how that relates to the findings from the current study. Fifth, likely due to the nature of the sample (i.e., at-risk) and the efficacy of the intervention in preventing youths’ problems, the sample was low on clinical levels of internalizing problems. In addition, there currently is no definitive way of understanding a clinically meaningful reduction or prevention of social problems. Future research would benefit from examining these processes in typical and clinical samples and should seek to understand the potency of these changes over time.
Sixth, the current study only utilized youth report of problems. Youth are arguably the best reporters of their own internal experiences as well as their social experiences that occur primarily outside of the context of the home. There is also evidence to suggest that parents’ ratings of their child's mental health is substantially impacted by their own anxiety and depression such that they report their child's functioning is worse than is observed and reported by others (i.e., maternal psychopathology-distortion hypothesis; Müller, Achtergarde, & Furniss, 2011). Given the history of depression in all of the caregivers in the current study, it is likely that the use of the youth self-report was the best choice. However, there is also evidence to suggest that depressed mood may lead youth to have negative views about their peer acceptance (Rudolph et al., 2007), dwell on negative aspects of their social experiences (e.g., Lyubomirsky, Caldwell, & Nolen-Hoeksema, 1998), and underestimate their social competence (e.g., Pomerantz & Rudolph, 2003). Therefore, future research should seek to investigate the relations among constructs in this study using other reporters (e.g., teacher) and other modes of measurement (e.g., observations).
Despite these limitations, the current study also has several notable strengths. First, this study was the first to utilize an intervention framework to examine if internalizing problems of youth living with a parent with a history of depression has a cascade effect on youths’ social problems and the bidirectional nature of this relation. In the tradition of cascade models (e.g., Masten & Cicchetti, 2010), the findings from this study provide valuable evidence as to one relatively unexplored domain in which children of depressed parents may be negatively impacted and how (i.e., through internalizing problems).
Second, these relations were explored within the context of a randomized control trial; therefore, we were able to explore how reductions in youth internalizing problems were related to lower levels of youth social problems. This provides a unique view of not only the relations among these variables, but of how intervention and prevention efforts can be efficacious in impacting these more distal outcomes. Cicchetti and Hinshaw (2002) noted that interventions and preventions are particularly well-equipped to study developmental processes because they provide unique insights into the progression, continuity, and alteration of both normative and non-normative behaviors and symptomatology. The presence of a minimum treatment comparison condition strengthens conclusions regarding the mediating mechanisms because it helps account for any age or development related effects that might account for change in social and internalizing problems. In fact, more research should aim to utilize randomized control trails to investigate cascade models in order to identify creative, innovative intervention and prevention techniques.
Third, we assessed internalizing problems and social problems at different time points, a criterion important for examining mediation in intervention studies (Kraemer et al., 2008). Fourth, utilizing a sample of parents with a history of depression may have helped diminish floor effects that often occur when studying psychopathology in community samples.
Overall, findings indicated that engagement in this FGCB preventive intervention led to decreased internalizing problems at 12 months which, in turn, were associated with lower levels of social problems at 18 months. A similar pattern of findings emerged for 18-month internalizing problems and 24-month social problems. These findings suggest that prevention and intervention efforts with a proximal aim of decreasing youth internalizing problems may lead to reductions in problems in other domains and may serve as a unique way of targeting the social problems of these youth. By understanding the numerous domains in which children of depressed parents are impacted, interventionists may be better able to identify and reduce these negative consequences and improve the lives of these youth.
Acknowledgments
Funding for this research was supported by grants R01MH069940 (Compas, PI) and R01MH069928 (Forehand, PI) from the National Institute of Mental Health and gifts from the Ansbacher family (Forehand, PI) and Patricia and Rodes Hart (Compas, PI). Preparation of this article was also supported, in part, by NIMH R01MH100377 (Jones, PI) to the third author and NICHD grant F31HD082858 that funded the second author's (Parent's) training. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
In order to examine if youth age was related to the reliability of the measures, the sample was split into two age groups (9-11 and 12-15 years). Alpha coefficients across these two age groups were equivalent in interpretation.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA schoolage forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Agoston AM, Rudolph KD. Pathways from depressive symptoms to low social status. Journal of Abnormal Child Psychology. 2013;41(2):295–308. doi: 10.1007/s10802-012-9675-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. doi: 10.1111/1469-7610.00424. [DOI] [PubMed] [Google Scholar]
- Asher SR, Hymel S. Coaching in social skills for children who lack friends in school. Children & Schools. 1986;8(4):205–218. doi: 10.1093/cs/8.4.205. [DOI] [Google Scholar]
- Beardslee WR, Gladstone TR, O'Connor EE. Transmission and prevention of mood disorders among children of affectively ill parents: A review. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(11):1098–1109. doi: 10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- Bettis AH, Forehand R, Sterba SK, Preacher KJ, Compas BE. Anxiety and depression in children of depressed parents: Dynamics of change in a preventive intervention. Journal of Clinical Child and Adolescent Psychology. 2016:1–14. doi: 10.1080/15374416.2016.1225503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boivin M, Hymel S. Peer experiences and social self-perceptions: A sequential model. Developmental Psychology. 1997;33(1):135. doi: 10.1037/0012-1649.33.1.135. [DOI] [PubMed] [Google Scholar]
- Buhs ES, Ladd GW. Peer rejection as antecedent of young children's school adjustment: An examination of mediating processes. Developmental Psychology. 2001;37(4):550. doi: 10.1037/0012-1649.37.4.550. [DOI] [PubMed] [Google Scholar]
- Burt KB, Obradović J, Long JD, Masten AS. The interplay of social competence and psychopathology over 20 years: Testing transactional and cascade models. Child Development. 2008;79(2):359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Brendgen M, Vitaro F, Turgeon L, Poulin F. Assessing aggressive and depressed children's social relations with classmates and friends: A matter of perspective. Journal of Abnormal Child Psychology. 2002;30(6):609–624. doi: 10.1023/A:1020863730902. [DOI] [PubMed] [Google Scholar]
- Brown BB, Clasen DR, Eicher SA. Perceptions of peer pressure, peer conformity dispositions, and self-reported behavior among adolescents. Developmental Psychology. 1986;22(4):521–530. doi: 10.1037/0012-1649.22.4.521. [DOI] [Google Scholar]
- Cicchetti D, Hinshaw SP. Editorial: Prevention and intervention science: Contributions to developmental theory. Development and Psychopathology. 2002;14(04):667–671. doi: 10.1017/S0954579402004017. [DOI] [PubMed] [Google Scholar]
- Coie JD, Dodge KA. Aggression and antisocial behavior. In: William D, Eisenberg N, editors. Handbook of child psychology: Social, emotional, and personality development. Hoboken, NJ, U.S: John Wiley & Sons, Inc; 1998. pp. 779–862. [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Roberts L, et al. Coping and parenting: Mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology. 2010;78:623–634. doi: 10.1037/a0020459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Keller G, Champion JE, Rakow A, Reeslund KL, Cole DA, et al. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. 2009;77(6):1007–1020. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Thigpen J, Hardcastle E, Garai E, Sterba S, et al. Efficacy and moderators of a family cognitive behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. 2015;83(3):541–553. doi: 10.1037/a0039053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Thigpen JC, Keller G, Hardcastle EJ, Cole DA, Roberts L, et al. Family group cognitive–behavioral preventive intervention for families of depressed parents: 18- and 24-month outcomes. Journal of Consulting and Clinical Psychology. 2011;79(4):488–499. doi: 10.1037/a0024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group. Initial impact of the Fast Track prevention trial for conduct problems: II. Classroom effects. Journal of Consulting and Clinical psychology. 1999;67(5):648. [PMC free article] [PubMed] [Google Scholar]
- Crick NR, Grotpeter JK. Relational aggression, gender, and social-psychological adjustment. Child Development. 1995;66(3):710–722. doi: 10.1111/j.1467-8624.1995.tb00900.x. [DOI] [PubMed] [Google Scholar]
- Crick NR, Zahn-Waxler C. The development of psychopathology in females and males: Current progress and future challenges. Development and Psychopathology. 2003;15(3):719–742. doi: 10.1017/S095457940300035X. [DOI] [PubMed] [Google Scholar]
- Cullerton-Sen C, Crick NR. Understanding the effects of physical and relational victimization: The utility of multiple perspectives in predicting social-emotional adjustment. School Psychology Review. 2005;34(2):147–160. [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250(4988):1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- England MJ, Sim LJ, editors. Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Martinez JI, Chorpita BF, Weisz JR. The Youth Self-Report: Applicability and validity across younger and older youths. Journal of Clinical Child & Adolescent Psychology. 2011;40(2):338–346. doi: 10.1080/15374416.2011.546041. [DOI] [PubMed] [Google Scholar]
- Feurer C, Hammen CL, Gibb BE. Chronic and episodic stress in children of depressed mothers. Journal of Clinical Child & Adolescent Psychology. 2016;45(3):270–278. doi: 10.1080/15374416.2014.963859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR axis I disorders—non-patient edition. New York State Psychiatric Institute; New York: 2001. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106(3):458–490. doi: 10.1037/0033-295X.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Tully E. Depression in women who are mothers: An integrative model of risk for the development of psychopathology in their sons and daughters. In: Keyes CLM, Goodman SH, editors. Women and depression: A handbook for the social, behavioral, and biomedical sciences. Cambridge University Press; 2006. pp. 241–280. [Google Scholar]
- Hammen C, Brennan PA. Depressed adolescents of depressed and nondepressed mothers: tests of an interpersonal impairment hypothesis. Journal of Consulting and Clinical Psychology. 2001;69(2):284–294. doi: 10.1037/0022-006X.69.2.284. [DOI] [PubMed] [Google Scholar]
- Henricsson L, Rydell AM. Children with behaviour problems: The influence of social competence and social relations on problem stability, school achievement and peer acceptance across the first six years of school. Infant and Child Development. 2006;15(4):347–366. doi: 10.1002/icd.448. [DOI] [Google Scholar]
- Hoglund WL, Chisholm CA. Reciprocating risks of peer problems and aggression for children's internalizing problems. Developmental Psychology. 2014;50(2):586–599. doi: 10.1037/a0033617. [DOI] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Mrug S, Hinshaw SP, Bukowski WM, Gold JA, Greenhill LL, et al. Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2005;34(1):74–86. doi: 10.1207/s15374424jccp3401_7. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Ivanova MY, Achenbach TM, Rescorla LA, Dumenci L, Almqvist F, Bilenberg N, Erol N, et al. The generalizability of the Youth Self-Report syndrome structure in 23 societies. Journal of Consulting and Clinical Psychology. 2007;75(5):729. doi: 10.1037/0022-006X.75.5.729. [DOI] [PubMed] [Google Scholar]
- Kawabata Y, Crick NR, Hamaguchi Y. Forms of aggression, social-psychological adjustment, and peer victimization in a Japanese sample: The moderating role of positive and negative friendship quality. Journal of Abnormal Child Psychology. 2010;38(4):471–484. doi: 10.1007/s10802-010-9386-1. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children—present and lifetime version (K-SADSPL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021.. [DOI] [PubMed] [Google Scholar]
- Kochel KP, Ladd GW, Rudolph KD. Longitudinal associations among youth depressive symptoms, peer victimization, and low peer acceptance: An interpersonal process perspective. Child Development. 2012;83(2):637–650. doi: 10.1111/j.1467-8624.2011.01722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(2S):101–108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leadbeater BJ, Hoglund WL. The effects of peer victimization and physical aggression on changes in internalizing from first to third grade. Child Development. 2009;80(3):843–859. doi: 10.1111/j.1467-8624.2009.01301.x. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Caldwell ND, Nolen-Hoeksema S. Effects of ruminative and distracting responses to depressed mood on retrieval of autobiographical memories. Journal of Personality and Social Psychology. 1998;75(1):166. doi: 10.1037/0022-3514.75.1.166. [DOI] [PubMed] [Google Scholar]
- Masten AS, Cicchetti D. Developmental cascades. Development and Psychopathology. 2010;22(03):491–495. doi: 10.1017/S0954579410000222. [DOI] [PubMed] [Google Scholar]
- McMahon RJ, Forehand R. Helping the noncompliant child: A clinician's guide to effective parent training. New York: Guilford Press; 2003. [Google Scholar]
- McQuade J, Breslend NL, Groff D. (manuscript in preparation) Experiences of physical and relational victimization in children with ADHD: The role of social problems and aggression. doi: 10.1002/ab.21762. [DOI] [PubMed] [Google Scholar]
- Moote GT, Smyth NJ, Wodarski JS. Social skills training with youth in school settings: A review. Research on Social Work Practice. 1999;9(4):427–465. doi: 10.1177/104973159900900403. [DOI] [Google Scholar]
- Morrow MT, Hubbard JA, McAuliffe MD, Rubin RM, Dearing KF. Childhood aggression, depressive symptoms, and peer rejection: The mediational model revisited. International Journal of Behavioral Development. 2006;30(3):240–248. doi: 10.1177/0165025406066757. [DOI] [Google Scholar]
- Müller JM, Achtergarde S, Furniss T. The influence of maternal psychopathology on ratings of child psychiatric symptoms: an SEM analysis on cross-informant agreement. European Child & Adolescent Psychiatry. 2011;20(5):241–252. doi: 10.1007/s00787-011-0168-2. [DOI] [PubMed] [Google Scholar]
- Muthén BO. Latent variable modeling in heterogeneous populations. Psychometrika. 1989;54(4):557–585. doi: 10.1007/BF02296397. [DOI] [Google Scholar]
- Muthén L, Muthén BO. Mplus user's guide (6th ed.) 6th. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10(5):173–176. doi: 10.1111/1467-8721.00142. [DOI] [Google Scholar]
- Pedersen S, Vitaro F, Barker ED, Borge AI. The timing of middle-childhood peer rejection and friendship: Linking early behavior to early-adolescent adjustment. Child Development. 2007;78(4):1037–1051. doi: 10.1111/j.1467-8624.2007.01051.. [DOI] [PubMed] [Google Scholar]
- Pomerantz EM, Rudolph KD. What ensues from emotional distress? Implications for competence estimation. Child Development. 2003;74(2):329–345. doi: 10.1111/1467-8624.7402001. [DOI] [PubMed] [Google Scholar]
- Reijntjes A, Kamphuis JH, Prinzie P, Telch MJ. Peer victimization and internalizing problems in children: A meta-analysis of longitudinal studies. Child Abuse & Neglect. 2010;34(4):244–252. doi: 10.1016/j.chiabu.2009.07.009. [DOI] [PubMed] [Google Scholar]
- Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. Journal of Adolescent Health. 2002;30(4):3–13. doi: 10.1016/S1054-139X(01)00383-4. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Flynn M, Abaied JL. A developmental perspective on interpersonal theories of youth depression. In: Abela JRZ, Hankin BL, editors. Handbook of Depression in Children and Adolescents. NY, NY: The Guilford Press; 2008. pp. 79–102. [Google Scholar]
- Rudolph KD, Ladd G, Dinella L. Gender differences in the interpersonal consequences of early-onset depressive symptoms. Merrill-Palmer Quarterly. 2007;53(3):461–488. doi: 10.1353/mpq.2007.0020. [DOI] [Google Scholar]
- Satorra A. Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In: Heijmans RDH, Pollock DSG, Santorra A, editors. Innovations in multivariate statistical analysis. US: Springer; 2000. pp. 233–247. [Google Scholar]
- Schleider JL, Ginsburg GS, Drake K. Perceived peer victimization predicts anxiety outcomes in a prevention program for offspring of anxious parents. Journal of Clinical Child & Adolescent Psychology. 2017:1–9. doi: 10.1080/15374416.2016.1270831. [DOI] [PMC free article] [PubMed]
- Schwartz D, McFadyen-Ketchum S, Dodge KA, Pettit GS, Bates JE. Early behavior problems as a predictor of later peer group victimization: Moderators and mediators in the pathways of social risk. Journal of Abnormal Child Psychology. 1999;27:191–201. doi: 10.1023/A:1021948206165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifer R, Dickstein S, Sameroff AJ, Magee KD, Hayden LC. Infant mental health and variability of parental depression symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(12):1375–1382. doi: 10.1097/00004583-200112000-00007. [DOI] [PubMed] [Google Scholar]
- Serdiouk M, Rodkin P, Madill R, Logis H, Gest S. Rejection and victimization among elementary school children: The buffering role of classroom-level predictors. Journal of Abnormal Child Ps ychology. 2015;43(1):5–17. doi: 10.1007/s10802-013-9826-9. [DOI] [PubMed] [Google Scholar]
- Simons RL, WU CI, Conger RD, Lorenz FO. Two routes to delinquency: Differences between early and late starters in the impact of parenting and deviant peers. Criminology. 1994;32(2):247–276. [Google Scholar]
- Snyder J, Brooker M, Patrick MR, Snyder A, Schrepferman L, Stoolmiller M. Observed peer victimization during early elementary school: Continuity, growth, and relation to risk for child antisocial and depressive behavior. Child Development. 2003;74(6):1881–1898. doi: 10.1046/j.1467-8624.2003.00644.x. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, Updegraff JA. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychological Review. 2000;107(3):411. doi: 10.1037/0033-295X.107.3.411. [DOI] [PubMed] [Google Scholar]
- van Lier PA, Koot HM. Developmental cascades of peer relations and symptoms of externalizing and internalizing problems from kindergarten to fourth-grade elementary school. Development and Psychopathology. 2010;22(03):569–582. doi: 10.1017/S0954579410000283. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents: 10 years later. Archives of General Psychiatry. 1997;54(10):932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Cummings EM, Iannotti RJ, Radke-Yarrow M. Young children of depressed parents: A population at risk for affective problems. New Directions for Child and Adolescent Development 1984. 1984;26:81–105. doi: 10.1002/cd.23219842607. [DOI] [Google Scholar]


