Abstract
Background
Fall injuries are common among the elderly. The aim of this study was to investigate whether blood-pressure patterns, as measured by 24-h ambulatory blood pressure monitoring (ABPM), or intensification of antihypertensive therapy following the 24-h ABPM, may be associated with fall injuries in hypertensive elderly patients.
Methods
In a retrospective study, community-based elderly patients (age ≥ 70 years) who were referred to 24-h ABPM were evaluated for fall injuries within one-year post-ABPM. We compared the clinical characteristics, 24-h ABPM patterns and the intensification of hypertensive therapy following 24-h ABPM, between patients with and without a fall injury.
Results
Overall 1032 hypertensive elderly patients were evaluated. Fifty-five (5.3%) had a fall injury episode in the year following ABPM. Patients with a fall injury were significantly older, and with higher rates of previous falls. Lower 24-h diastolic blood-pressure (67.3 ± 7.6 vs. 70.7 ± 8.8 mmHg; P < 0.005) and increased pulse-pressure (74.7 ± 14.3 vs. 68.3 ± 13.7 mmHg; P < 0.005), were found in the patients with a fall injury, compared to those without a fall injury. After adjustment for age, gender, diabetes mellitus and previous falls, lower diastolic blood-pressure and increased pulse-pressure were independent predictors of fall injury. Intensification of antihypertensive treatment following the 24-h ABPM was not associated with an increased rate of fall injury.
Conclusions
Low diastolic blood-pressure and increased pulse-pressure in 24-h ABPM were associated with an increased risk of fall injury in elderly hypertensive patients. Intensification of antihypertensive treatment following 24-h ABPM was not associated with an increased risk of fall injury.
Keywords: Ambulatory blood pressure monitoring, Hypertension, Falls
1. Introduction
Falls can lead to physical trauma and restriction of activity; this is a principal cause of morbidity in the elderly.[1] It was estimated that 30% of people over the age of 65 years who live in the community fall at least once per year, and this proportion increases strongly with age.[1] Roughly, half of all falls result in an injury.[1] The evidence is conflicting regarding a possible relationship between office blood-pressure, anti-hypertensive therapy and risk of falls among elderly hypertensive patients.[1]–[6] While several studies found an association between low blood-pressure patterns and the risk of fall injury, other studies failed to show any association between blood-pressure patterns and the risk of falls.
Twenty-four-hour ambulatory blood pressure monitoring (ABPM) is increasingly used in the routine clinical practice of blood pressure assessment. The risk of hypertensive cardiovascular complications may correlate more closely with 24-h ABPM than with office blood pressure measurements, both in the general population[7] and among the elderly.[8] It is currently unknown if blood-pressure parameters, as measured by 24-h ABPM, are associated with increased risk of fall injury in the elderly. In the current study, we aimed to investigate whether blood-pressure patterns, as measured by 24-h ABPM or intensification of antihypertensive therapy after 24-h ABPM, may be associated with fall injuries in hypertensive elderly patients. The hypothesis was that ABPM patterns and intensification of anti-hypertensive therapy increase the risk of fall injury.
2. Methods
This study was reviewed and approved by the Ethics Committee of the Kaplan Medical Center. Medical records were evaluated of a cohort of hypertensive elderly patients (age ≥ 70 years), who were tested with a 24-h ABPM in the Kaplan Medical Center and for whom one-year follow-up data were available after the ABPM test. The medical records were obtained from the OFEK Medical Record system of the largest health provider in Israel (Clalit Health Services).
Patients older than 70 year of age were included only if they fulfilled one of the two criteria for hypertension: (1) had known diagnosis of hypertension with anti-hypertensive treatment or (2) had evidence of hypertension in a 24-h ABPM, defined as blood-pressure above 130/80 mmHg.[9] For analysis, patients were divided to two groups: those who had a fall injury episode during the year after the 24-h ABPM, and those who did not have a fall injury during such time interval. Fall injury was defined as any fall that led to referral to an emergency ward or admission to a hospital due to bruises, hematomas, non-pathological fracture, dislocation of joints, pain or head injury. All records of patients with the diagnosis of falls based the International Classification of Diseases (ICD)-9 diagnosis codes were evaluated for the detailed description of the fall and its consequences.
For the analysis of the association between 24-h ABPM, anti-hypertensive medications and fall injury we excluded fall injury episodes that were directly attributed to medical or environmental causes, as described in the medical records (e.g., violent domestic events). For patients with more than one 24-h ABPM test over a one-year period, the most recent 24-h ABPM test for which there were one-year follow-up data was considered.
We evaluated the time interval from a 24-h ABPM to a fall injury, and the time interval from a 24-h ABPM to intensification of antihypertensive medication. The date of antihypertensive medication intensification was considered as the day that a new antihypertensive medication was purchased or the date of increasing dosage of an antihypertensive medication that was already prescribed in the past. We defined antihypertensive therapy as treatment with any medication on the list of available antihypertensive medications in our health system organization.
Data were presented as mean ± SD for continuous variables, and as frequency and percentage for categorical variables. Differences in continuous variables were determined by the Mann-Whitney U test. Differences in categorical variables were determined by the Pearson's chi-squared test. For predicting fall injury, we performed a logistic regression and adjusted for factors that were included in the regression model. The factors were based on parameters that were previously associated with an increased risk of falls. All statistical analyses were two-tailed tests and significance was set at 5%. Results were analyzed using SPSS 23.0 (SSPS Inc., Chicago, Ill., USA).
3. Results
3.1. Patient characteristics
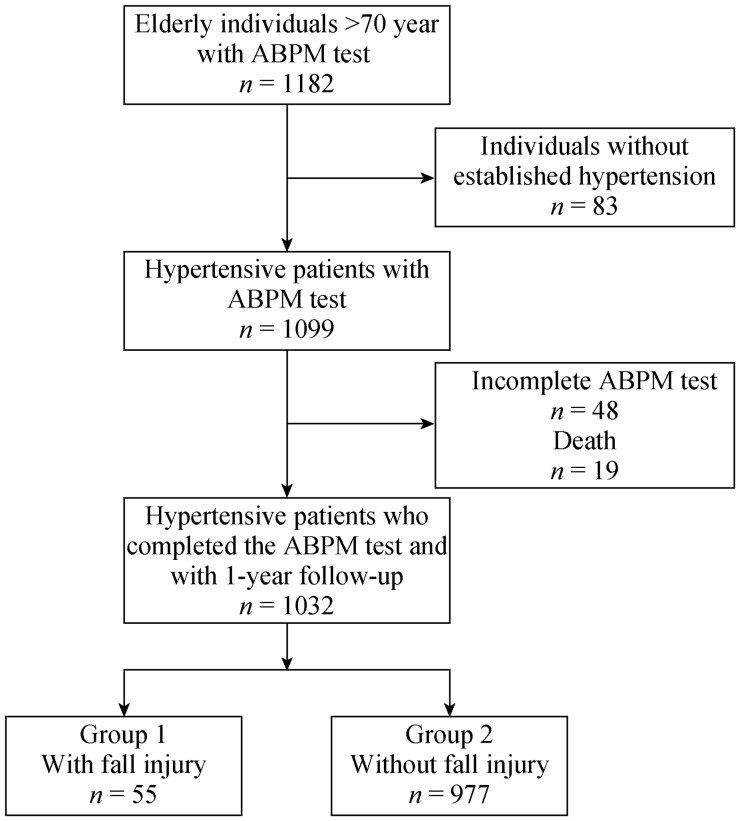
Overall, 1032 elderly hypertensive patients completed a 24-h ABPM and were included in the cohort (Figure 1). Of the 1032 patients, 55 (5.3%) had a fall injury episode in the following year (Figure 1). Patient baseline characteristics, according to fall injury are summarized in Table 1. Patients with a fall injury episode were significantly older (78.2 ± 4.4 vs. 76.3 ± 5.1 years; P < 0.005) compared to patients without a fall injury episode. Patients with a fall injury episode also had higher rates of previous fall injuries [20/55 (36%) vs. 199/977 (20%) patients; P < 0.05] compared to patients without a fall injury episode. Distributions of gender, diabetes mellitus, dementia and the use of antihypertensive therapy did not differ significantly between the two groups.
Figure 1. Study flow diagram.
ABPM: ambulatory blood pressure monitoring.
Table 1. Patient baseline characteristics.
| With fall injury (n = 55) | Without fall injury (n = 977) | |
| Age, yrs | 78.2 ± 4.4 | 76.3 ± 5.1 |
| Female gender | 37 (67%) | 635 (65%) |
| Diabetes mellitus | 18 (33%) | 263 (27%) |
| Dementia | 1 (1.8%) | 6 (0.6%) |
| Previous fall injury | 20 (36%) | 199 (20%) |
| Antihypertensive therapy | 53 (96%) | 966 (99%) |
| ACEI/ARBs | 27 (51%) | 463 (48%) |
| Diuretics | 22 (41%) | 425 (44%) |
| CCBs | 28 (52%) | 541 (56%) |
| Beta-blockers | 21 (40%) | 377 (39%) |
| Alpha-blockers | 3 (6%) | 91 (9%) |
| Central-acting | 4 (8%) | 77 (8%) |
Data were presented as mean ± SD or n (%). ACEI: angiotensin converting enzyme inhibitor; ARBs: angiotensin receptor blockers; CCBs: calcium channel blockers.
3.2. Blood-pressure patterns in a 24-h ABPM and fall injury
24-h ABPM patterns for the two groups are summarized in Table 2. Ambulatory systolic blood-pressure measurements (24-h, awake and sleep periods) did not differ significantly between the groups. Patients with a fall injury episode had a significantly lower 24-h diastolic blood-pressure (67.3 ± 7.6 vs. 70.7 ± 8.8 mmHg; P < 0.005) and a higher 24-h pulse-pressure (74.7 ± 14.3 vs. 68.3 ± 13.7 mmHg; P < 0.005), compared to patients who did not have a fall injury. Both awake and sleep diastolic blood-pressure were significantly lower in patients with a fall injury episode compared to those who did not have a fall injury. The awake and sleep pulse-pressure measurements were significantly increased in patients with a fall injury episode compared to those who did not have a fall injury. Heart rate was one beat per minute lower in those who fell, but this difference was not statistically significant between the groups (Table 2). Logistic regression analysis, with adjustment for age, gender, diabetes mellitus and previous falls showed that lower diastolic blood-pressure (24-h, awake and sleep) and increased pulse-pressure (24-h, awake and sleep) were predictive of a fall injury in the following year post-ABPM (Table 3A). For 1 mmHg increase in diastolic blood-pressure, there was a 6% decrease in the probability of having a fall injury. For each 1 mmHg increase in pulse-pressure, there was a 3% increase in the probability of having a fall injury (Table 3A). A logistic regression analysis model with adjustment for age, gender, diabetes mellitus, previous falls, systolic blood-pressure, and diastolic blood-pressure showed that both high systolic blood-pressure and low diastolic blood-pressure (24-h, awake and sleep) were predictive of a fall injury during the year following ABPM (Table 3B).
Table 2. 24-h ABPM in hypertensive elderly patients with or without a fall injury within one year.
| ABPM parameter | With fall injury (n = 55) | Without fall injury (n = 977) | P value |
| 24-h systolic, mmHg | 140.9 ± 15.2 | 139.0 ± 15.1 | 0.1 |
| 24-h diastolic, mmHg | 67.3 ± 7.6 | 70.7 ± 8.8 | < 0.005 |
| 24-h pulse pressure, mmHg | 74.7 ± 14.3 | 68.3 ± 13.7 | < 0.005 |
| 24-hr heart rate, beats/minute | 64.7 ± 8.6 | 65.9 ± 8.9 | 0.05 |
| Awake systolic, mmHg | 142.9 ± 16.2 | 141.0 ± 15.2 | 0.2 |
| Awake diastolic, mmHg | 68.2 ± 8.0 | 71.3 ± 9.4 | < 0.005 |
| Awake pulse pressure, mmHg | 74.8 ± 14.9 | 68.7 ± 13.7 | < 0.005 |
| Awake heart rate, beats/minute | 66.4 ± 9.9 | 67.5 ± 9.4 | 0.06 |
| Sleep systolic, mmHg | 135.5 ± 17.8 | 132.8 ± 19.6 | 0.1 |
| Sleep diastolic, mmHg | 62.5 ± 10.0 | 65.3 ± 8.2 | < 0.05 |
| Sleep pulse pressure, mmHg | 73.3 ± 16.0 | 67.3 ± 15.7 | < 0.005 |
| Sleep heart rate, beats/minute | 59.9 ± 8.7 | 60.2 ± 8.8 | 0.08 |
ABPM: ambulatory blood-pressure monitoring.
Table 3. Multi-variant regression analysis for fall-injury events.
| ABPM parameter | Odds ratio | 95% confidence Interval |
||
| Lower | Upper | |||
| A | ||||
| 24-h SBP | 1.01 | 0.989 | 1.026 | |
| 24-h DBP | 0.94** | 0.907 | 0.974 | |
| 24-h pulse pressure | 1.03** | 1.011 | 1.050 | |
| Awake SBP | 1.01 | 0.989 | 1.025 | |
| Awake DBP | 0.95** | 0.919 | 0.981 | |
| Awake pulse pressure | 1.03** | 1.009 | 1.048 | |
| Sleep SBP | 1.01 | 0.993 | 1.020 | |
| Sleep DBP | 0.96* | 0.937 | 0.995 | |
| Sleep pulse pressure | 1.02** | 1.005 | 1.037 | |
| B | ||||
| 24-h SBP | 1.03* | 1.005 | 1.045 | |
| 24-h DBP | 0.92** | 0.887 | 0.959 | |
| Awake SBP | 1.02* | 1.0 | 1.04 | |
| Awake DBP | 0.93** | 0.900 | 0.968 | |
| Sleep SBP | 1.02** | 1.006 | 1.040 | |
| Sleep DBP | 0.94** | 0.909 | 0.975 | |
A: adjusted variables: age, sex, previous falls, diabetes mellitus; B: adjusted variables: age, sex, previous falls, diabetes mellitus, systolic blood-pressure and diastolic blood-pressure. DBP: diastolic blood-pressure; SBP: systolic blood-pressure. *P < 0.05; **P < 0.01.
3.3. Intensification of antihypertensive therapy following a 24-h ABPM and fall injury
No difference was observed between the groups in terms of intensification of antihypertensive treatment before a fall injury (23/55 in patients with a fall injury vs. 390/977 in patients without a fall injury; P = 0.3). No statistically significant difference was found in the drug-classes used to intensify treatment, between patients with and without a fall injury (Table 4).
Table 4. Intensification of antihypertensive therapy after a 24-h ABPM.
| Antihypertensive therapy drug-class | With fall injury (n = 23) | Without fall injury (n = 390)* |
| ACE-I/ARBs | 9 (39%) | 131 (33%) |
| Diuretics | 7 (30%) | 101 (26%) |
| CCBs | 5 (22%) | 121 (31%) |
| Beta-blockers | 3 (13%) | 35 (9%) |
| Alpha-blockers | 4 (17%) | 85 (22%) |
| Central-acting | 2 (9%) | 11 (3%) |
Data are presented as n (%). ABPM: ambulatory blood pressure monitoring; ACEI: angiotensin converting enzyme inhibitor; ARBs: angiotensin receptor blockers; CCBs: calcium channel blockers. *P > 0.05 for all antihypertensive therapy drug-classes.
The interval between the 24-h ABPM and the intensification of antihypertensive therapy was similar in the two groups (36.2 ± 42.5 days in patients with a fall injury vs. 37.3 ± 42.8 days in patients without a fall injury; P = 0.6).
4. Discussion
In a cohort of community based elderly hypertensive patients, low diastolic blood-pressure and increased pulse-pressure in a 24-h ABPM were associated with an increased risk of fall injuries during the one-year following the 24-h ABPM. These associations remained significant in a multivariate analysis. To the best of our knowledge, this study is the first to evaluate a possible association between baseline blood-pressure measured by a 24-h ABPM and fall injuries in elderlies with hypertension. It suggests that the performance of a 24-h ABPM may aid in fall risk assessment for elderly patients with hypertension.
Fall injury rates increase with age and age-related changes in blood-pressure are observed even after the age of 80 years.[1],[10] It is therefore possible that the conflicting data about the association of office blood-pressure and falls in elderlies are related to continuous changes in blood-pressure patterns in this population. A retrospective study of 3544 community-dwelling adults ≥ 60 years of age found that increased systolic and diastolic blood-pressure were associated with a lower risk of self-reported falls among women, while low systolic or low diastolic blood-pressure were associated with an increased risk of falls in men.[4] On the other hand, in a prospective trial of 5236 hypertensive adults ≥ 65 years of age, a crude analysis showed that both low and high office diastolic blood-pressure were associated with an increased risk of serious fall injuries, but this association was no longer present after multivariable adjustment.[5] A study of Banach, et al.,[6] did not find an association between systolic blood-pressure and self-reported falls among elderly persons taking antihypertensive medication. Taken together, these conflicting results suggest that prospective trials in elderlies, with a 24-h ABPM, are needed to further investigate the possible association of ambulatory blood-pressure parameters and the risk of fall injuries.
Low diastolic blood-pressure is common in the elderly hypertensive population and is associated with increased cardiovascular risk.[11] A recent study in a large cohort of treated hypertensive patients aged 80 years and older found that about 20% of the patients had hypotension in a 24-h ABPM (defined as systolic blood-pressure < 100 and/or diastolic blood-pressure < 60 mmHg) and 34% had hypotension in awake ABPM measurements (defined as systolic blood-pressure < 105 and/or diastolic blood-pressure < 65 mmHg). Interestingly, low diastolic blood-pressure was the cause of hypotension in more than 90% of the cases.[11] These results suggest that a 24-h ABPM is a useful examination to detect hypotensive episodes not diagnosed in office visits.
Lower diastolic blood-pressure and higher pulse-pressure in elderlies are associated with an increased risk of cardiovascular complications.[11],[12] Possible mechanisms for cardiovascular complication involve greater stress on arteries and endothelial dysfunction.[13] Data supporting an effect of low diastolic blood-pressure and increased pulse-pressure on falls are sparse. Non-cardiovascular mechanisms may be involved in the association between blood-pressure patterns and the risk of falls. Indeed, sarcopenia was found to be associated with increased pulse-pressure in older women,[14] and sarcopenia is also a risk factor for falls.[15]
We did not find an association between intensification of antihypertensive treatment following the 24-h ABPM and an increased risk of fall injuries. Data are conflicting in regard to associations between hypertension, antihypertensive therapy and the risk of fall injuries. A survey of 4961 community-living adults older than 70 years with hypertension found that moderate to high intensity antihypertensive treatment was associated with an increased risk of serious fall injuries, particularly among those with previous fall injuries.[16] Increased risk during the first 45 days following antihypertensive therapy initiation was found in a population-based self-controlled case series study of 543,572 new users of antihypertensive drugs, among community-dwelling elderly > 66 year of age.[2] Shimbo, et al.,[17] showed that initiation of antihypertensive therapy or intensification of antihypertensive therapy was associated with a short-term (change in medications less than 15 days before a fall injury), but not long-term increased risk of serious fall injuries among older adults. On the other hand, a meta-analysis of published studies did not find that administration of any of the five main antihypertensive drug classes affected the risk of fall injuries in the elderly (aged > 60 years).[18] Furthermore, among ambulatory adults aged 75 years or older, participating in The Systolic Blood-Pressure Intervention Trial (SPRINT) trial, intensified treatment to systolic blood-pressure target of less than 120 mmHg compared with target of less than 140 mmHg, resulted in a non-significantly lower rate of injurious falls.[19] In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, intensive antihypertensive treatment that lowered systolic blood-pressure below 120 mmHg, was not associated with an increased risk of falls in a subset of 3,099 diabetic participants aged 40–79 years.[20]
This study has several limitations. First and foremost, it is a retrospective observational study. Any association of 24-h ABPM results and fall injuries does not necessarily imply causality. The referral to a 24-h ABPM was mostly given by general practitioners, as well as hypertension specialists. Consequently, the clear indications for the 24-h ABPM test, in the majority of patients, are unknown and may vary between physicians. It is therefore impossible to conclude whether the referrals to 24-h ABPM were in agreement with the suggested indications for ABPM tests in consensus guidelines.[9] Importantly, there are no data regarding the diagnosis of orthostatic hypotension in this cohort. Indeed, suspicion of orthostatic or episodic hypotension (e.g., postprandial hypotension) is a possible indication for 24-h ABPM testing, and orthostatic hypotension is a potential risk factor for falls.[9],[21] There is also no frailty assessment for this cohort. Nevertheless, this study may reflect the “real world” since 24-h ABPM may aid in reassessing hypertension, specifically in the elderly population.[8],[22] Although the potential for misclassification does exist, all files of patients admitted to the emergency ward or hospital during the one-year following the 24-h ABPM test were analyzed to minimize this potential limitation. In that regard, the falls considered in this study are all those that led to referral to an emergency ward or hospitalization, regardless of the severity of the fall. Others have reported only events of serious fall injuries, including patients who were admitted to the hospital with non-pathological fractures, dislocations of joints, intractable pain or head injury.[16] Therefore, the associations found in this study may differ from those of patients with very severe fall injury.
In conclusion, low diastolic blood-pressure and increased pulse-pressure, as found by 24-h ABPM, were associated with an increased risk of fall injuries among elderly hypertensive patients. Strategies to reduce the risk of fall injury risk should be considered in this subset of elderly hypertensive patients.
Acknowledgments
We wish to thank Mrs. Keren Levy for her assistance in the generating of the ABPM data. The authors declare no conflict of interest.
References
- 1.Phelan EA, Mahoney JE, Voit JC, Stevens JA. Assessment and management of fall risk in primary care settings. Med Clin North Am. 2015;99:281–293. doi: 10.1016/j.mcna.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butt DA, Mamdani M, Austin PC, et al. The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int. 2013;24:2649–2657. doi: 10.1007/s00198-013-2369-7. [DOI] [PubMed] [Google Scholar]
- 3.Bursztyn M, et al. Hypertension, its treatment, frailty, falls, and mortality. Hypertension. 2017;70:253–254. doi: 10.1161/HYPERTENSIONAHA.117.09689. [DOI] [PubMed] [Google Scholar]
- 4.Klein D, Nagel G, Kleiner A, et al. Blood pressure and falls in community-dwelling people aged 60 years and older in the VHM&PP cohort. BMC Geriatr. 2013;13:50. doi: 10.1186/1471-2318-13-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bromfield SG, Ngameni CA, Colantonio LD, et al. Blood pressure, antihypertensive polypharmacy, frailty, and risk for serious fall injuries among older treated adults with hypertension. Hypertension. 2017;70:259–266. doi: 10.1161/HYPERTENSIONAHA.116.09390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banach M, Bromfield S, Howard G, et al. Association of systolic blood pressure levels with cardiovascular events and all-cause mortality among older adults taking antihypertensive medication. Int J Cardiol. 2014;176:219–226. doi: 10.1016/j.ijcard.2014.07.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hansen TW, Jeppesen J, Rasmussen S, et al. Ambulatory blood pressure and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 8.Burr ML, Dolan E, O'Brien EW, et al. The value of ambulatory blood pressure in older adults: the Dublin outcome study. Age Ageing. 2008;37:201–206. doi: 10.1093/ageing/afm193. [DOI] [PubMed] [Google Scholar]
- 9.Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–1366. doi: 10.1097/HJH.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 10.Franklin SS, Gustin W, Wong ND, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96:308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 11.Divisón-Garrote JA, Ruilope LM, de la Sierra A, et al. Magnitude of hypotension based on office and ambulatory blood pressure monitoring: results from a cohort of 5066 treated hypertensive patients aged 80 years and older. J Am Med Dir Assoc. 2017;18:452.e1–452.e6. doi: 10.1016/j.jamda.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 13.Dart AM, Kingwell BA. Pulse pressure―a review of mechanisms and clinical relevance. J Am Coll Cardiol. 2001;15; 37:975–984. doi: 10.1016/s0735-1097(01)01108-1. [DOI] [PubMed] [Google Scholar]
- 14.Coelho Júnior HJ, Aguiar Sda S, et al. Sarcopenia is associated with high pulse pressure in older women. J Aging Res. 2015:109824. doi: 10.1155/2015/109824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Landi F, Liperoti R, Russo A, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012;31:652–568. doi: 10.1016/j.clnu.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–595. doi: 10.1001/jamainternmed.2013.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shimbo D, Barrett Bowling C, Levitan EB, et al. Short-term risk of serious fall injuries in older adults initiating and intensifying treatment with antihypertensive medication. Circ Cardiovasc Qual Outcomes. 2016;9:222–229. doi: 10.1161/CIRCOUTCOMES.115.002524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zang G. Antihypertensive drugs and the risk of fall injuries: a systematic review and meta-analysis. J Int Med Res. 2013;41:1408–1417. doi: 10.1177/0300060513497562. [DOI] [PubMed] [Google Scholar]
- 19.Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥ 75 years: a randomized clinical trial. JAMA. 2016;315:2673–2682. doi: 10.1001/jama.2016.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Margolis KL, Palermo L, Vittinghoff E, et al. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med. 2014;29:1599–1606. doi: 10.1007/s11606-014-2961-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120:841–847. doi: 10.1016/j.amjmed.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 22.Cappelleri C, Janoschka A, Berli R, et al. Twenty-four-hour ambulatory blood pressure monitoring in very elderly patients: comparison of in-hospital vs. home follow-up results. Medicine (Baltimore) 2017;96:e7692. doi: 10.1097/MD.0000000000007692. [DOI] [PMC free article] [PubMed] [Google Scholar]