Abstract.
Several in vitro and in vivo studies have established accelerated thrombolysis using ultrasound (US) induced microbubble (MB) cavitation. However, the mechanisms underlying MB mediated sonothrombolysis are still not completely elucidated. We performed three-dimensional (3-D) volumetric optical coherence tomography (OCT) imaging before and after the application of contrast US to thrombus. The most dramatic reduction in clot volume was observed with US + MB + recombinant tissue plasminogen activator (rt-PA). Thrombus surface erosion in this group on the side of the thrombus exposed to MB and ultrasound was evident on the OCT images. This technique may assist in clarifying the mechanisms underlying sonothrombolysis, especially regarding the importance of US transducer orientation on lytic efficacy and the effects of MB cavitation on thrombus structure.
Keywords: optical coherence tomography, sonothrombolysis, contrast ultrasound, microbubbles
1. Introduction
In vitro and in vivo studies have demonstrated enhancement of thrombolysis using ultrasound (US) with US contrast agents or microbubbles (MBs).1–5 At sufficient acoustic pressure, MBs will rupture, causing local fluid microjetting, which can result in pitting on solid surfaces, and may be responsible for enhancing thrombus fragmentation.6,7 Additionally, microstreaming resulting from MB oscillation in an US field may enhance the penetration of fibrinolytic enzymes such as rt-PA into the structure of the thrombus.8,9 Although these fundamental underlying theories have been generally accepted and partially demonstrated, the physical mechanisms responsible for MB-mediated thrombolysis remain poorly understood, as evidenced by variations in the published data,4–6,10 which may be partly due to limitations in current techniques for assessment of changes in thrombus size. Clot weight measurement2,4–6 can vary substantially depending on water content and does not allow for accurate evaluation of smaller thrombi. Microscopy1,10 cannot measure volume changes and surface contours. Histological sectioning4–6 cannot be used for assessment during treatment and requires tissue processing, which interferes with micron-scale changes.
In the present study, we employed optical coherence tomography (OCT)11 to precisely assess the efficacy of MB cavitation mediated clot lysis and elucidate the effects of MB cavitation on thrombus structure by generating high-resolution 3-D structural images of treated clots. OCT, which has the ability to visualize thrombus in vivo,12 is gaining use in clinical practice and offers important potential advantages over current methods for assessment of sonothrombolysis owing to its ability to capture high-resolution 3-D real-time volumetric images noninvasively with minimal sample manipulation.11,13 To our knowledge, there has been no report to date assessing MB-mediated thrombolysis using OCT.
2. Methods
An OCT optics engine (Bioptigen, Research Triangle, NC) was coupled with a high bandwidth superluminescent diode array (870-nm center wavelength, 200-nm bandwidth; model Q870, Superlum Ltd., Dublin, Ireland). The light source has a coherence length of 1.3 μm in tissue. The OCT scanner was installed in a scientific microscope (Zeiss Discovery V8, Carl Zeiss MicroImaging GmbH, Germany).
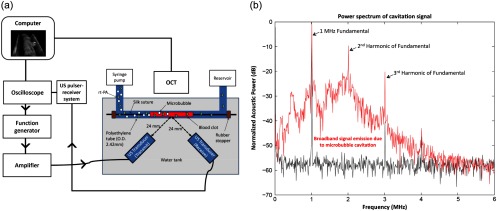
The flow system consisted of a syringe pump (Harvard Apparatus, Holliston, MA) delivering rt-PA (, Activase, Genentech, San Francisco, CA) and/or lipid MBs (, diameter )14 suspended in phosphate buffered saline (PBS) into an open loop polyethylene tubing system containing a cylindrical thrombus formed from whole porcine blood bound to a silk suture10 [Fig. 1(a)]. Two single-element transducers—an unfocused 1-MHz transducer for US delivery, and a focused 2.25-MHz transducer for detection of MB cavitation events (A303S and V306, Olympus NDT, Waltham, MA)—were mounted to a custom-built microscope stage with an acoustic chamber containing degassed water maintained at . The stage was designed for alignment of the two transducers, such that the focal area of the detection transducer overlapped with the center of the US treatment beam with the thrombus positioned at equal distance from the transducers. Target location was confirmed with US pulse/echo technique. MB cavitation was detected using the 2.25-MHz US transducer in passive receiving mode using amplifying and filtering (5073PR, Olympus, Waltham, MA) and a digital oscilloscope (6051A, Lecroy, Chestnut ridge, NY)4,5 [Fig. 1(b)].
Fig. 1.
In vitro experimental setup and broadband signal emission. (a) A polyethylene tube containing a fixed blood clot was prepared and placed on a custom microscope stage with an acoustic chamber fitted with two ultrasound transducers. Optical coherence tomography was employed to image the thrombi over 30 min of ultrasound treatment. (b) The broadband signal emission, which indicates the occurrence of MB destruction, was evident when MBs were present in the perfusate (red, top) but not when ultrasound was applied without MBs (black, bottom).
During flow through the system shown in Fig. 1(a), clots treated with US were exposed to US pulses (1 MHz, 100 cycles, 1.0 MPa) that cause MB rupture in the US focus for 30 min.6 Pulses were delivered every 5 s to allow complete MB replenishment between pulses. OCT images were captured from the same location before and after treatment with one of three regimens: 1) PBS only; 2) rt-PA; or 3) US + MBs + rt-PA.
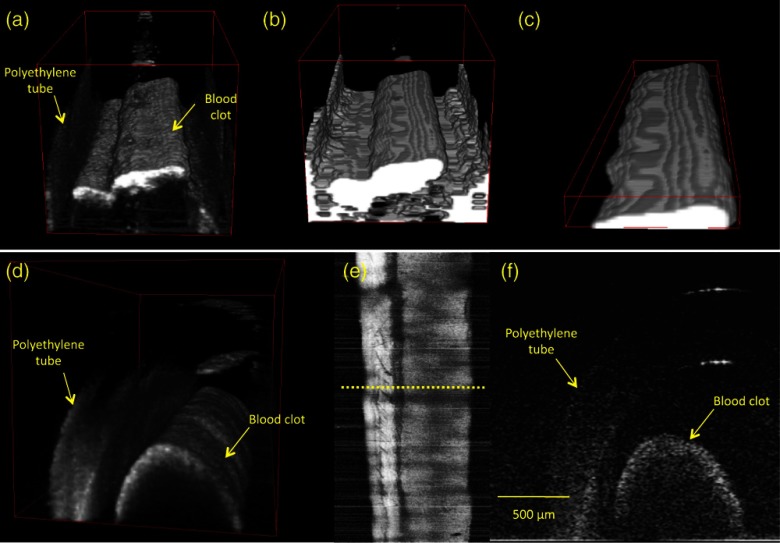
A single 3-D OCT acquisition consisted of a sampling of a volume centered on the portion of the blood clot exposed to the US treatment with each of these scans acquired four times and averaged. Each scan was acquired in 5.7 s. The degree of clot lysis was assessed by determining the clot volume pre- and post-treatment by thresholding the pixel intensity of each cross-sectional OCT image using a custom-made semi-automatic segmentation plug-in for ImageJ image processing software.15 Figure 2 (top panels) displays typical 3-D rendered OCT datasets of raw [Fig. 2(a)], thresholded [Fig. 2(b)] and cropped volumes [Fig. 2(c)].
Fig. 2.
Example of blood clot volume derivation from an optical coherence tomography (OCT) scan and 3-D rendering of thrombus. A raw OCT image (a) was thresholded using the image’s mean intensity value to form a binary image (b) The portion of the image that demonstrated a clear boundary was then segmented (c) for volume assessment by pixel counting. A 3-D rendering of an OCT scan is shown (d) with a projected image [(e), top view], and a B-mode image [(f), cross-section] along the dotted yellow line in (e).
3. Results
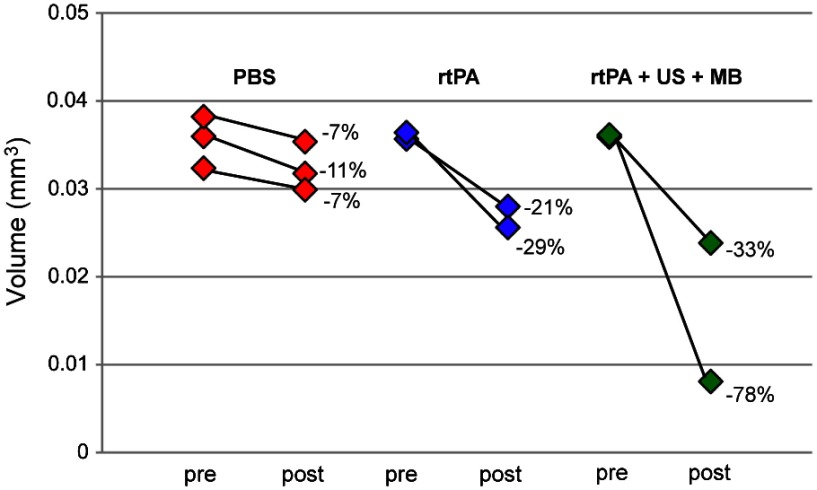
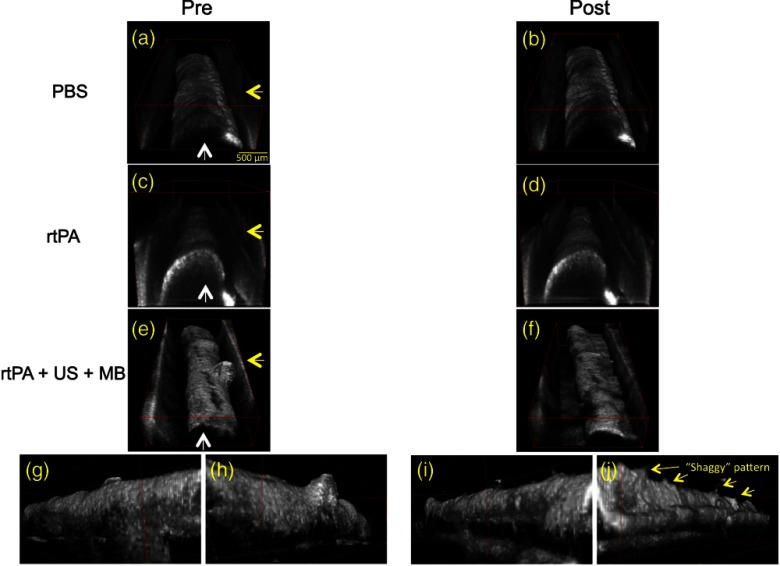
Seven experiments were performed (three control; two rt-PA; two US + MB + rt-PA). A 3-D OCT rendering of a thrombus is shown in Fig. 2(d) with a projected image [Fig. 2(e)], and a cross-sectional image [Fig. 2(f)] along the dotted yellow line in Fig. 2(e). Figure 3 shows clot volume changes between pre- and post-scans. After 30 min of treatment, the mean clot volume in the control group decreased by 8.9% (), while the rt-PA group showed a 25.6% () decrease in volume, and the US+ MB + rt-PA showed a 55.7% () decrease in volume. Figure 4 shows an example of pre- (left panels) and post- (right panels) treatment 3-D OCT images from the three groups. The effect of treatment was clearly seen in the US + MB + rt-PA group between pre- [Fig. 4(e)] and post- [Fig. 4(f)] treatment images. Interestingly, both trials of US + MB + rt-PA treatment resulted in erosion and the formation of an irregular clot surface contour with numerous fine projections emanating from the clot. This “shaggy” pattern was only visible on the surfaces of treated clots, which were facing the transducer [Fig. 4(j)]; the surfaces of the clots facing away from the US beam [Fig. 4(i)], further from the US source, retained their relatively smooth contour.
Fig. 3.
Clot volume changes from sonothrombolysis measured with optical coherence tomography (OCT). Clot volumes were measured by analyzing 3-D OCT images using a semi-automated thresholding method for volume quantification. Treatment with rt-PA resulted in a moderate reduction in clot volume while rt-PA + US + MBs resulted in a larger volume reduction.
Fig. 4.
3-D optical coherence tomography (OCT) volume renderings. Pre- (left panels) and post-(right panels) treatment: control [(a) and (b)], recombinant tissue plasminogen activator [rt-PA, (c) and (d)], and ultrasound (US) + microbubbles (MB) + rt-PA [(e) and (f)]. The difference in pre- and post- volumes was most clear after US + MB + rt-PA treatment [(e) and (f)]; note the dissolution of the protuberance from the clot surface. Direction of flow is indicated with white arrows; transducer orientation is indicated with yellow arrows. Surface of clot shown in (e) facing away from (g) and toward (h) transducer before treatment. Surface of clot shown in (f) facing away from (i) and toward (j) transducer after treatment. The clot surface after treatment became shaggy, especially on the surface facing the transducer (j).
4. Discussion
We have successfully measured micron scale volume changes due to sonothrombolysis in blood clots using OCT. The US + MB + rt-PA treatment showed higher lytic efficacy than rt-PA treatment alone, which is consistent with the reports of others.4–6,10 Interestingly, clots exposed to US + MB + rt-PA demonstrated an irregular “shaggy” pattern on their surface after treatment, which was not evident after administration of rt-PA alone. This pattern was more pronounced on the surface of the clot closest to the transducer and exposed to the highest “dose” of US [Fig. (4)], suggesting that the orientation of the US transducer may be critical for optimal MB mediated thrombolysis. Our study was limited to a single set of acoustic conditions that were tested and use of a non-physiological pefusate (PBS). This, however, allowed us to consider the relatively pure mechanical effects of the US-MB interaction on clot volume.
OCT measurements can be taken noninvasively and serially in a functioning experimental or physiologic system without the need for fixation or tissue processing. As such, the observations gathered using OCT technology can offer unique insights into mechanical events that underlie thrombolysis in response to MB and US, facilitating future improvement for this approach. As demonstrated in this study, optimal orientation of the US transducer may be critical for achieving efficient sonothrombolysis. Further studies using OCT technology to investigate the effects of MB cavitation on thrombus structure as well as the response to varying US and MB parameters would be important. Intravascular thrombus detection has already been extensively demonstrated in vivo.12 If successful, this method may allow for a real-time feedback mechanism using OCT for assessment of sonothrombolysis during clinical application.
Acknowledgments
The Physician Scientist Training Program and Center for Ultrasound Molecular Imaging and Therapeutics, University of Pittsburgh School of Medicine (JE Leeman) and the postdoctoral fellowship in Ocular Tissue Engineering and Regenerative Ophthalmology, LJ Fox Center for Vision Restoration, UPMC (JS Kim). JS Schuman receives royalties for intellectual property licensed by Massachusetts Institute of Technology to Carl Zeiss Meditec.
References
- 1.Shaw G. J., et al. , “Tissue plasminogen activator concentration dependence of 120-kHz ultrasound-enhanced thrombolysis,” Ultra. Med. Bio. 34(11), 1783–1792 (2008). 10.1016/j.ultrasmedbio.2008.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Porter T. R., et al. , “Thrombolytic enhancement with perfluorocarbon-exposed sonicated dextrose albumin microbubbles,” Am. Heart J. 132(5), 964–968 (1996). 10.1016/S0002-8703(96)90006-X [DOI] [PubMed] [Google Scholar]
- 3.Xie F., et al. , “Diagnostic ultrasound combined with glycoprotein IIb/IIIa-targeted microbubbles improves microvascular recovery after acute coronary thrombotic occlusions,” Circulation 119(10), 1378–1385 (2009). 10.1161/CIRCULATIONAHA.108.825067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Datta S., et al. , “Correlation of cavitation with ultrasound enhancement of thrombolysis,” Ultra. Med. Bio. 32(8), 1257–1267 (2006). 10.1016/j.ultrasmedbio.2006.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Datta S., et al. , “Ultrasound-enhanced thrombolysis using definity as a cavitation nucleation agent,” Ultra. Med. Biol. 34(9), 1421–1433 (2008). 10.1016/j.ultrasmedbio.2008.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chuang Y. H., et al. , “Effects of ultrasound-induced inertial cavitation on enzymatic thrombolysis,” Ultra. Imag. 32(2), 81–90 (2010). [DOI] [PubMed] [Google Scholar]
- 7.Crum L. A., “Cavitation microjets as a contributory mechanism for renal calculi disintegration in ESWL,” J. Urol. 140(6), 1587–1590 (1988). [DOI] [PubMed] [Google Scholar]
- 8.Miller D. L., “Particle gathering and microstreaming near ultrasonically activated gas-filled micropores,” J. Acoust. Soc. Am. 84(4), 1378–1387 (1988). 10.1121/1.396636 [DOI] [PubMed] [Google Scholar]
- 9.Collis J., et al. , “Cavitation microstreaming and stress fields created by microbubbles,” Ultrasonics 50(2), 273–279 (2010). 10.1016/j.ultras.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 10.Meunier J. M., et al. , “Duty cycle dependence of ultrasound enhanced thrombolysis in a human clot model,” Ultra. Med. Biol. 33(4), 576–583 (2007). 10.1016/j.ultrasmedbio.2006.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang D., et al. , “Optical coherence tomography,” Science 254(5035), 1178–1181 (1991). 10.1126/science.1957169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prati F., et al. , “Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis,” Eur. Heart J. 31(4), 401–415 (2010). 10.1093/eurheartj/ehp433 [DOI] [PubMed] [Google Scholar]
- 13.Gabriele M. L., et al. , “Three dimensional optical coherence tomography imaging: advantages and advances,” Prog. Ret. Eye Res. 29(6), 556–579 (2010). 10.1016/j.preteyeres.2010.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weller G. E., et al. , “Modulating targeted adhesion of an ultrasound contrast agent to dysfunctional endothelium,” Annal. Biomed. Eng. 30(8), 1012–1019 (2002). 10.1114/1.1513565 [DOI] [PubMed] [Google Scholar]
- 15.Rasband W. S., ImageJ. Available at: http://rsb.info.nih.gov/ij/. Accessed (15 January 2011).