Abstract
DYSIS II CHD was a longitudinal, observational study in 6794 patients from 18 countries. They were attending an outpatient physician appointment for coronary heart disease (CHD). 6370 patients (93.8%) were on active lipid lowering therapy (LLT). The mean atorvastatin dose equivalent was 25 mg per day and 10.5% received ezetimibe in combination with a statin. The mean low-density lipoprotein cholesterol (LDL-C) level was 88 mg/dL, with 29.4% of patients displaying a level below the 70 mg/dL target for very high-risk subjects.
Conclusion
While more than 90% of patients with CHD were on lipid lowering drugs, only three out of ten patients achieved their LDL-C target value.
Keywords: Low-density lipoprotein cholesterol, Treatment target, Global, Region, Statins
Specifications table
| Subject area | Biology |
| More specific subject area | Dyslipidemia and cardiovascular risk |
| Type of data | Tables and Figures |
| How data was acquired | Worldwide survey |
| Data format | Analyzed |
| Experimental factors | Observational, longitudinal registry |
| Experimental features | Comparison of lipid lowering therapies administered in patients with coronary heart disease, as well as LDL-C target achievement. |
| Data source location | Institut für Herzinfarktforschung, Ludwigshafen, Germany |
| Data accessibility | Data are included in this article |
Value of the data
-
•
These data have been collected under real life conditions across the world.
-
•
Stratification per country can help to facilitate a scientific dialogue for the benefit of coronary patients in these countries, but also help to compare treatment standards between geographies of the world.
-
•
The data presented can help to guide treatment decisions for novel lipid lowering agents.
1. Data
See Fig. 1 and Table 1, Table 2.
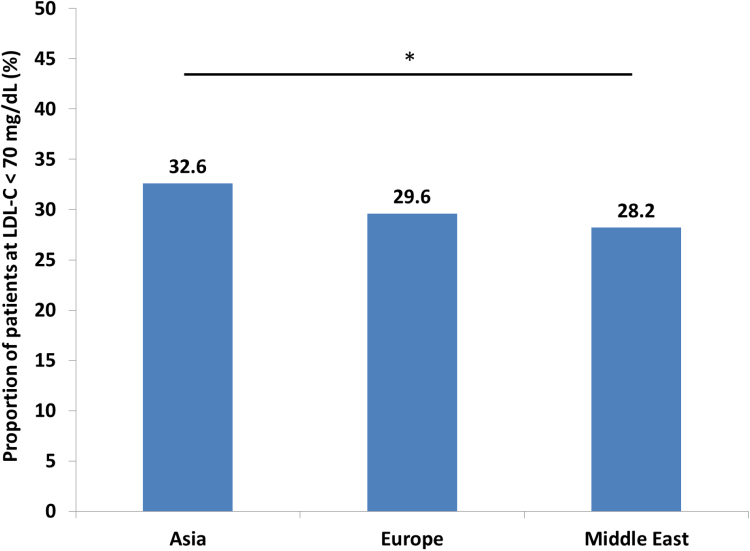
Fig. 1.
LDL-C target attainment for LLT-treated patients by region Legend: *p<0.05 for overall comparison.
Table 1.
Predictors of LDL-C target value attainment among treated CHD patients.
| Full model |
Stepwise model |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age >70 years | 1.09 | 0.97–1.23 | 0.166 | – | – | – |
| Female | 0.72 | 0.62–0.83 | <0.001 | 0.72 | 0.63–0.84 | <0.001 |
| BMI >30 kg/m2 | 0.83 | 0.72–0.95 | 0.007 | 0.82 | 0.71–0.94 | 0.004 |
| Current smoking | 0.82 | 0.69–0.99 | 0.035 | 0.81 | 0.68–0.97 | 0.022 |
| Sedentary lifestyle | 0.86 | 0.76–0.97 | 0.011 | 0.86 | 0.76–0.97 | 0.012 |
| Stable angina | 0.88 | 0.77–0.99 | 0.041 | 0.88 | 0.77–0.99 | 0.040 |
| Chronic kidney disease | 1.20 | 0.98–1.46 | 0.076 | – | – | – |
| Type 2 diabetes mellitus | 1.70 | 1.51–1.92 | <0.001 | 1.72 | 1.53–1.93 | <0.001 |
| History of chronic heart failure | 0.87 | 0.73–1.04 | 0.133 | – | – | – |
| Hypertension | 0.81 | 0.71–0.92 | 0.001 | 0.82 | 0.72–0.93 | 0.002 |
| Statin dose (>20 mg/day atorvastatin dose equivalent) | 1.010 | 1.007–1.013 | <0.001 | 1.010 | 1.007–1.013 | <0.001 |
Legend: BMI, body mass index; CI, confidence interval; OR, odds ratio.
Table 2.
Regional differences in lipid-lowering therapy.
| Asia (N=2562) | Europe (N=2777) | Middle East (N=1031) | P value | |
|---|---|---|---|---|
| Statin monotherapy | 86.2% | 79.8% | 79.6% | <0.001 |
| Statin+ezetimibe | 7.7% | 11.6% | 14.6% | <0.001 |
| Statin+other non-statin | 5.3% | 6.7% | 5.0% | 0.047 |
| Non-statin monotherapy | 0.8% | 2.0% | 0.7% | <0.001 |
| Atorvastatin dose equivalent (mean±SD mg/day)a | 20±15 | 27±20 | 30±18 | <0.0001 |
| Atorvastatin dose equivalent (median [IQR] mg/day)a | 20 (10, 20) | 20 (10, 40) | 20 (20, 40) |
SD, standard deviation; IQR, interquartile range.
In statin treated patients.
2. Experimental design, materials and methods
DYSIS II CHD was a multicenter, longitudinal, observational study that included 6794 patients from 18 countries in Europe, the Middle East, South-, Southeast- and East-Asia [1].
The study was approved by the relevant ethics committees and carried out in agreement with local laws.
Inclusion criteria were as follows: 1) provision of written informed consent, 2) aged ≥18, 3) attending an outpatient appointment for stable CHD 2012–2014, 4) availability of a full fasting or non fasting lipid profile from within the previous 12 months, and 5) not participating in a clinical trial.
The ESC/EAS dyslipidemia guidelines (2011) were used as a reference in order to determine target value attainment [2]. Low density lipoprotein (LDL-C) treatment target thus was <70 mg/dl. Use of LLT was documented, including use of statin and combination therapy. We also determined the statin dose administered, calculated as atorvastatin equivalent doses [3].
Data were collected in an electronic case report form and processed in a central web-based database at the Institut für Herzinfarktforschung, Ludwigshafen, Germany. It was used for both collection and storage of the data.
SAS version 9.3 (Cary, NC, USA) was used for performing the calculations. Data are presented as absolute numbers and percentages (n/N). Between-group differences were evaluated using a chi squared test. Multivariable logistic regression was used to calculate odds ratios for factors predictive of LDL-C target attainment. Both the results of the full model and a stepwise forward selection model are given.
Acknowledgments
The work was funded by Merck & Co., Inc., Kenilworth, NJ, USA. The authors of the present study would like to thank all DYSIS II CHD investigators for their contribution to the successful completion of this study.
Footnotes
Supplementary data associated with this article can be found in the online version at 10.1016/j.dib.2018.04.092.
Transparency document. Supplementary material
Supplementary material
.
References
- 1.Gitt A.K., Lautsch D., Ferrières J., De Ferrari G.M., Vyas A., Baxter C.A., Bash L.D., Ashton V., Horack M., Almahmeed W., Chiang F.T., Poh K.K., Brudi P., Ambegaonkar B. Cholesterol target value attainment and lipid-lowering therapy in patients with stable or acute coronary heart disease: results from the Dyslipidemia International Study II. Atherosclerosis. 2017;266:158–166. doi: 10.1016/j.atherosclerosis.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 2.European Association for Cardiovascular Prevention & Rehabilitation, Reiner Z., Catapano A.L., De Backer G., Graham I., Taskinen M.R., Wiklund O., Agewall S., Alegria E., Chapman M.J., Durrington P., Erdine S., Halcox J., Hobbs R., Kjekshus J., Filardi P.P., Riccardi G., Storey R.F., Wood D., Guidelines ESCCfP Committees ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) Eur. Heart J. 2011;32:1769–1818. doi: 10.1093/eurheartj/ehr158. [DOI] [PubMed] [Google Scholar]
- 3.Weng T.C., Yang Y.H., Lin S.J., Tai S.H. A systematic review and meta-analysis on the therapeutic equivalence of statins. J. Clin. Pharm. Ther. 2010;35:139–151. doi: 10.1111/j.1365-2710.2009.01085.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material