Abstract
Background
With new data supporting the efficacy of bracing, the role of school screening for early detection of moderate scoliosis curves has been revisited. Due to a high rate of false positive screening and cost concerns, a comprehensive county-wide school screening program was discontinued in 2004. We aim to determine the impact of a comprehensive school screening program on curve magnitude at presentation and initial scoliosis treatment for all local county patients presenting to a pediatric orthopedics clinic from all referral sources.
Methods
Between 1994 to 2014, 761 county patients presented to a pediatric orthopedic clinic for new scoliosis evaluation. Curve magnitude and recommended treatment were recorded. Treatment indications for bracing, surgery, and observation were consistent over the study period.
Results
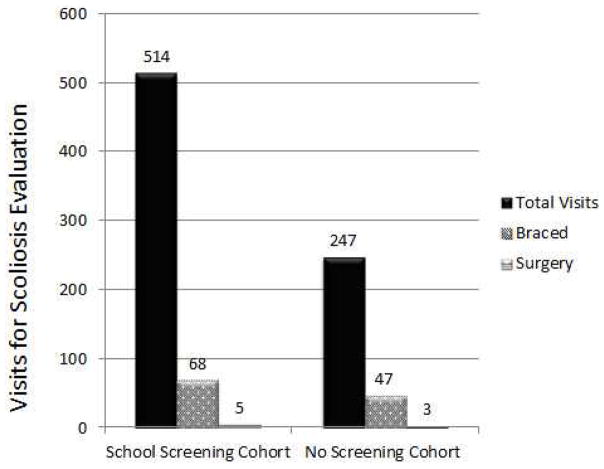
From January 1994–July 2004 (school screening period), 514 children were seen by a pediatric orthopedist specialist for scoliosis evaluation compared to 247 patients from August 2004–December 2014 (no school screening). There was a 48% decrease in the number of county children who were evaluated for idiopathic scoliosis by pediatric orthopedics once school screening was discontinued. Mean maximal Cobb angle at presentation increased from 20° (range,4°–65°) to 23° (range, 7°–57°). At presentation, 5/514 (0.97%) patients in the screened group required surgery and 68/514 (13.2%) required bracing, compared to 3 out of 247 (1.2%) patients in the non-screened group requiring surgery and 47/247 (19%) requiring bracing (p>0.05, p=0.04, respectively).
Conclusion
After school screening was discontinued, mean curve magnitude and rates of bracing at presentation statistically increased in county patients evaluated for new scoliosis, although the clinical significance is unclear. After school screening was discontinued, there were fewer patients referrals, braces prescribed, and unnecessary evaluations (patients discharged at first visit). This study provides data to evaluate the role of school screening for children with regular access to healthcare.
Level of Evidence
3
Introduction
Adolescent idiopathic scoliosis is the most common spinal deformity in children, affecting up to one in 300 individuals. The role and utility of school screening to detect scoliosis early in the disease course is debated in the literature (1–4). The goal of scoliosis school screening is to detect curves when they are moderate and amenable to bracing so as to prevent progression to surgical management (5). Those opposed to screening state that such programs consume valuable resources, cause worry to families and children (6), and result in unnecessary x-rays and radiation exposure for individuals who have false positive screening results (7). While many U.S school districts adopted a practice of universal scoliosis school screening, budgetary pressures and the lack of data proving the efficacy of brace treatment led to the discontinuation of screening programs in many regions. With recent studies conclusively demonstrating that bracing can prevent curve progression, there is renewed interest in the value of school screening for scoliosis (8, 9).
Our investigation evaluates the role of school screening on all new scoliosis referrals to pediatric orthopedics from county residents in one U.S. county. The total population of the county was 137,521 in 2006 and includes a city of 92,000 people where our pediatric orthopedic center is located. The radius of the county is approximately 20 miles. Children attend school at one of 5 public school districts and a variety of private schools. Earlier studies have established that our county experience provides a reasonable estimation for incidence rates of most diseases (10). A survey of county residents indicated that 95% or more receive their medical care at one of the two health care centers, of which only our center provides pediatric orthopedic care (11). Referral patterns did not significantly change during this study period. The nearest neighboring pediatric orthopedic center/spine surgeon is 70 miles away. Our pediatric orthopedic center accepts all major local insurance types including public assistance, and there is a low number of undocumented children in our region.
In 2004, 4 out of 5 public school districts and all private schools in our county discontinued school screening, which was previously provided by the county health department. Prior to this, there was a strong, standardized school screening program in place in both county public and private schools which was run by the county (7). We sought to compare the number of county patients seen by the pediatric orthopedic practice for school screening, and the curve magnitude and recommended treatment at initial presentation for new patients seen between 1994–2004 (during school screening) to 2004–2014 (after school screening) for evaluation of scoliosis. We hypothesized that patients presenting from 2004–2014 would have larger magnitude curves compared to patients presenting prior to 2004 and would more frequently require immediate bracing or surgery.
Materials and Methods
Our research team contacted our county schools to verify the years and timing of school screening and when it had been discontinued. Prior to 2004, school screening for scoliosis throughout the county was performed by a school public health nurse (LPN level or higher). Students were screened in grades 5, 7, and 8. If the student did not meet screening parameters (clinical suspicion or scoliometer reading of 6° or more), a second nurse examined the child. If there was still concern, the patient’s parent was called and a letter was sent. There was no direct referral to pediatric orthopedics via the school screening process. Rather, the school simply requested communication as to whether the scoliosis had been assessed by a medical professional. Screening in 4 out of 5 county public school districts and all the private schools was stopped in 2004. The remaining public school district did not have complete records, but stated that no screening had been done after 2007. Thus, county patients presenting to pediatric orthopedics between 1994 and August 2004 were considered the School Screening Cohort. Patients presenting to pediatric orthopedics between September 2004 and September 2014 were considered the No Screening Cohort. We hypothesized that curve magnitude at presentation would be increased in the No Screening Cohort. Patients in both cohorts were either self-referred or referred by their primary care provider for an orthopedic evaluation. During the study period, there was no pathway for schools or the health department to directly refer patients to an orthopedic surgeon for scoliosis care. During the study period, a stable pediatric orthopedic practice existed in our county with four surgeons, several nurse practitioners, and one physician assistant providing consistent care.
During the study period, no other orthopedic surgeons or neurosurgeons are known to offer pediatric scoliosis care within a 70 mile radius, and no specific training was provided to primary physicians that may have affected referral patterns. Standards for initiating bracing (skeletally immaturity, curve > 20–25 degrees), and surgery (curve > 45–50 degrees for skeletally immature patient and > 50 degrees for skeletally mature patient) were consistent over the study period.
We also assessed whether other healthcare providers were managing scoliosis bracing or surgery in the region. There is only one orthotics office within a 70 mile radius which manufactures scoliosis braces. They had not received a prescription for a scoliosis brace for anyone other than from the pediatric orthopedic providers included in this analysis. We surveyed 13 regional chiropractors to see if they had prescribed braces for adolescent idiopathic scoliosis treatment. Many stated that they would treat children with scoliosis but would refer for moderate or severe scoliosis and would not prescribe a brace.
Medical records for all new county patients presenting to the pediatric orthopedic practice for scoliosis from 1994–2014 were reviewed. Patients with neuromuscular scoliosis or diagnoses other than idiopathic scoliosis were excluded. Patients who moved to the county area with scoliosis treatment already provided at another center were excluded. All county residents between age 8 and 18 presenting to pediatric orthopedics for new scoliosis evaluation were included. We have noted that some patients present for scoliosis evaluation at age 8 or 9, are followed, and ultimately diagnosed with adolescent idiopathic scoliosis. Thus, we included 8 and 9 years old in the study. Curve magnitude at initial presentation to pediatric orthopedics was measured. Initial prescribed treatment was recorded, including bracing, surgery, observation, or no further follow-up. Need for subsequent surgery or bracing was also recorded over the follow-up period.
Student’s t-test was used to compare continuous variables between the two time periods (Cobb angle at presentation). Pearson’s chi square test was used to compare discrete variables (number bracing or surgery). Statistical significance was set at p<0.05. Institutional Review Board approval was obtained for all aspects of this study.
Results
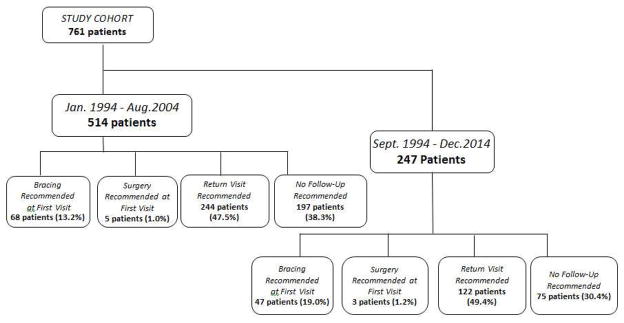
Between 1994 and 2014, a total of 761 county patients were seen by a pediatric orthopedist for the new diagnosis of scoliosis (Figure 1). 514 were seen while school screening was present, and 247 children were seen after screenings were discontinued (Table 1). The average age at presentation in both groups was 13 years old (p>0.05). In the screening years, 197 of the 514 patients (38.3%) were seen for a one-time visit and discharged due to skeletal maturity or small curve magnitude. For those whose initial recommended treatment was bracing (68 patients, 13.2%), surgery (5 patients, 1.0%), or observation (244 patients 47.5%), mean follow-up was 2.7 years. In the non-screening years, 75 patients (30.4%) were seen for a one-time visit and were not recommended to have any follow-up. Thus, ending school screening decreased the number of unnecessary visits from 38% down to 30% of all new patient scoliosis evaluations. 47 patients (19.0%) presented at the first visit with a curve large enough to warrant bracing immediately (Figure 2). Three patients (1.2%) required surgery upon first evaluation by pediatric orthopedics (Table 2). Of the 172 that were treated for scoliosis, mean follow up was 2.4 years. There was no difference in follow up time between the two groups.
Figure 1.
Study cohort. At the first visit to the pediatric orthopedic clinic, bracing, surgery, or additional follow-up visits were recommended. Some patients were discharged from the clinic and no follow-up was recommended.
Table 1.
| Parameter | School Screening Cohort (Seen by Peds Ortho During 1994–2004) | No School Screening Cohort (Seen by Peds Ortho 2004–2014) | P-Value |
|---|---|---|---|
| Number of Patients | 514 | 247 | |
| Age | 13 (Range, 8–18) | 13 (Range,8–18) | 0.35 |
| Gender | 364 Females 150 Males |
188 Females 79 Males |
0.13 |
Figure 2.
There were fewer scoliosis visits from county patients after discontinuation of school screening.
Table 2.
| Parameter | School Screening Cohort (n=514, Seen by Peds Ortho During 1994–2004) | No School Screening Cohort (n=247, Seen by Peds Ortho 2004–2014) | P-Value |
|---|---|---|---|
| Mean Thoracic Cobb at Presentation | 18° (Range, 4°–65°) | 21° (Range,4°–57°) | 0.003* |
| Mean Lumbar Curve at Presentation | 18° (Range, 4°–56°) | 20° (Range, 7°–51°) | 0.09 |
| Max Curve at Presentation | 20° (Range,4°–65°) | 23° (Range, 7°–57°) | 0.001* |
| Patients Never Requiring Treatment | |||
| Patients Requiring Bracing at Presentation | 68 (13.2%) | 47 (19.0%) | 0.04* |
| Patients Requiring Spine Fusion at Presentation | 5 | 3 | 0.8 |
| Patients Requiring Spinal Fusion for AIS | 21 (3.9%) | 12 (4.6%) |
Statistically significant result.
There was a marked decrease in the number of patients seen with a new diagnosis of scoliosis over the study period with a 48% decrease in patients seen between the two groups (541 vs. 265). County patients seen per year changed from 47 per year during the screening period (Figure 3), to 23 visits per year after screening was discontinued (p<0.001). County school enrollment, including public, private, charter and homeschooled students, increased 13% over the study period from 18,247 in 1994 to 20,621 in 2014. There was no known change in appointment availability or access to care, and in fact, the pediatric orthopedic group added a 4th full-time surgeon in 2007.
Figure 3.
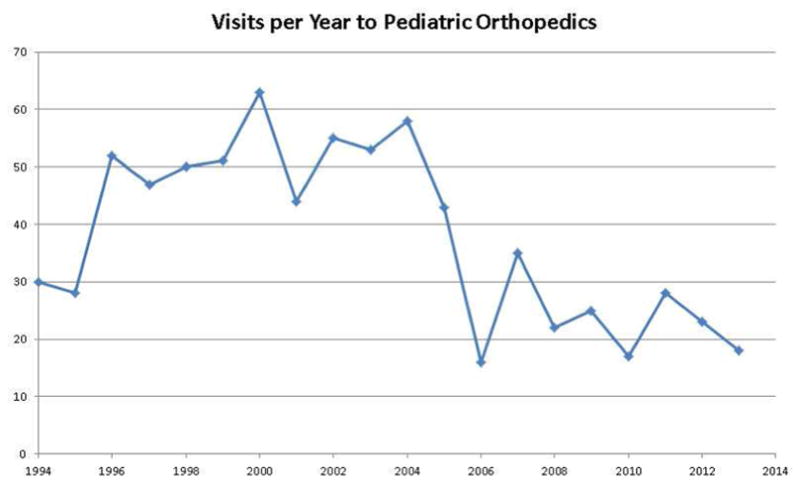
Number of new patient evaluations per year for suspected scoliosis at the pediatric orthopedic clinic over the study period. School screening was discontinued in 2004.
Mean maximum Cobb angle at presentation was significantly higher in the No Screening Cohort compared to the Screening Cohort (Table 2, p=0.001). It is unclear if this difference is clinically significant. The mean thoracic curve magnitude in the Screening Cohort was 18°; the mean magnitude in the No Screening Cohort was 21° (p=0.03). The mean lumbar curve magnitude measured 18° in the Screening Cohort and 20° in the No Screening Cohort, with no significant difference between the two groups (p>0.05). The percentage of patients prescribed a brace at the first visit increased after school screening was discontinued (Table 2), but the number of braces prescribed decreased from 68 to 47. There was no difference in the percentage of patients who were recommended to have surgery at the first visit.
Of those patients who participated in scoliosis screenings, ultimately 21/514 required surgery (4.1%). Of patients seen after school screening, 12/247 of the non-screened patients required surgery (4.5%). There was no change in the percentage of patients eventually requiring bracing or fusion surgery for the overall course of treatment between the School Screening and No Screening Cohorts (p>0.05).
Discussion
Previous studies have found school screening to be effective (12–14). Others have found school screening results in unnecessary visits for patients with minimal curves that do not require treatment (7, 15, 16). In our study, we sought to evaluate how a county-wide discontinuation of school screening would affect our local referrals for new scoliosis evaluation only including patients who live in our county. The most marked change was a significant decrease in the number of county patients being seen by the pediatric orthopedic practice for a new diagnosis of scoliosis, despite increased numbers of students enrolled in school.
Fewer county patients were seen by pediatric orthopedic subspecialists after school screening was discontinued. The number of patients who had no follow-up scheduled decreased from 38% of the cohort down to 30% of the cohort after school screening was discontinued, relieving these patients from potentially unnecessary visits and radiation exposure. Observation with radiographic/clinical follow-up was recommended for 47% (244/514) of the School Screening cohort, compared to 49% of the No School Screening cohort. It is unclear how many of those patients eventually needed bracing or surgery, since many of these patients were lost to follow-up. Given that fewer braces were prescribed during the No School Screening period of the study, but the student population increased, there may be more patients with undetected moderate scoliosis in the community after school screening has been discontinued. It is possible that some of those patients had significant curves and would have benefited treatment. The mean magnitude of scoliosis curve at presentation modestly increased during the study period. There may be patients with surgical magnitude curves living the community unaware of their condition. Evaluation of the presence of undiagnosed moderate or severe scoliosis in the community was beyond the scope of this study.
Although bracing fabrication techniques changed somewhat over the course of our study period, our primary outcome measure was curve magnitude at presentation, which would not be affected by specific bracing practices. The treatment indications for surgical or bracing treatment did not change over the study period. It is encouraging that there was not an increased number of surgeries recommended at first presentation. Our study may have been underpowered to detect a change in the rate of surgery following the discontinuation of school screening.
Current literature reports conflicting information as to the value of scoliosis school screening. A recent study from Denmark without school screening reported median curve magnitude at time of referral from a general practitioner to be 35°, and surgery was recommended in 160 out of 460 (35%) patients at the time of initial referral to an orthopedic surgeon over a 5 year period. There was no comparison cohort of patients who had received school screening (4). Also, routine pediatric screenings end at age 5 in Denmark, whereas children in the U.S. frequently require regular physician physicals well into teenage years for clearance in sports and other extra-curricular activities. School screening may hold additional benefits for children and adolescents who are not regularly seen by a primary care as described in Denmark. Additional studies have concluded that closing school screening programs was associated with increased curve magnitude upon initial presentation to a physician and increased incidence of surgical correction (1, 3). The results of our study are considerably different than the Denmark study, with much smaller curve magnitudes at presentation (21° vs. 35°) and lower surgical rates among patients presenting for evaluation (4.5% vs. 35%).
In two different publications, one in 1995 and one in 2004, the U.S. Preventative Services Task force challenged the effectiveness of performing scoliosis screening (15), and gave routine screening a D recommendation in 2004, discouraging the use of this service (17). Jakubowski et al. (18) concluded that money and time could be better spent in schools by eliminating school screenings and instead focusing on overall health education. However, it is difficult to make a firm decision on the benefit of school screening. Surgeons and families are very disappointed when patients present with severe curves requiring surgery which may have been amenable to bracing treatment had the curve been diagnosed earlier in the course of the disease. This highlights the need for further study to optimize scoliosis screening such that no child’s scoliosis is missed but prevents unnecessary radiographic screening of large numbers of patients.
Other studies conclude that there is not enough evidence either way to come to a conclusion regarding the benefit of school scoliosis screening, and that further evidence is needed before drawing conclusions (5, 13, 19–21). Our paper provides similar indeterminate findings regarding the benefit of school screening. With improvement in screening methods, some suggest that screenings could be successfully implemented (2, 22). Regional variation in medical practice and frequency of contact with primary care providers may make school scoliosis screening beneficial in one area while redundant and ineffective in another healthcare system.
Our pediatric orthopedic clinic is located in the county, which is home to two large medical centers. Residents of the county have more ready access to medical care than is typical in most areas of the world. This may increase the detection of scoliosis by regular interaction with medical providers, obviating the need for school scoliosis screening. It is possible that our findings simply reflect a temporal decline in referrals to the pediatric orthopedic clinic rather than a result of school screening discontinuation. Patients seen for scoliosis by primary care physicians or in other health centers will be the focus of future investigation.
Other limitations of our study include the retrospective design and limited patient numbers. Although we did not perform a formal power analysis, our patient numbers are likely too few to detect a difference in surgical rates between the Screening and No Screening Cohorts. Further, we cannot exclude the possibility that after the discontinuation of school screening some children have scoliosis that was not detected. In this study, we only evaluated patients presenting to a pediatric orthopedic specialist; thus, no conclusions regarding the incidence of scoliosis in our region can be determined.
In summary, we found mean maximal curve magnitude and rates of bracing at presentation significantly increased after the discontinuation of school screening in county patients presenting with a new diagnosis of scoliosis, although the clinical significance may not be large. Discontinuing school screening resulted in 48% fewer patient referrals and a decrease in the total number of patients treated. Patients who were discharged after the first visit decreased from 38% of all new patients seen during the school screening period to 30% of all new patients after school screening was discontinued. We did not detect a statistically significant increase in the rates of surgical treatment for scoliosis patients but our study likely was underpowered to evaluate this. This study provides data to evaluate the role of school screening for early detection of scoliosis and brace treatment in a population with regular access to healthcare.
Acknowledgments
ANL was supported by an NIH from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. (R03 AR 66342). Additional funding was provided by the Department of Orthopedic Surgery, Mayo Clinic.
Footnotes
Institutional review board approval was obtained for all aspects of this study (Mayo IRB #14-005455 and Olmsted Medical Center 006-OMC-15)
CONFLICT OF INTEREST: A. Noelle Larson received research grants from Orthopedic Research and Education Foundation and Scoliosis Research Society. A. Noelle Larson and Todd Milbrandt serve on board of Pediatric Orthopedic Society of North America.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Adobor RD, Riise RB, Sorensen R, Kibsgard TJ, Steen H, Brox JI. Scoliosis detection, patient characteristics, referral patterns and treatment in the absence of a screening program in Norway. Scoliosis. 2012;7(1):18. doi: 10.1186/1748-7161-7-18. Epub 2012/10/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fong DY, Cheung KM, Wong YW, Wan YY, Lee CF, Lam TP, Cheng JC, Ng BK, Luk KD. A population-based cohort study of 394,401 children followed for 10 years exhibits sustained effectiveness of scoliosis screening. The spine journal: official journal of the North American Spine Society. 2015;15(5):825–33. doi: 10.1016/j.spinee.2015.01.019. Epub 2015/01/24. [DOI] [PubMed] [Google Scholar]
- 3.Labelle H, Richards SB, De Kleuver M, Grivas TB, Luk KD, Wong HK, Thometz J, Beausejour M, Turgeon I, Fong DY. Screening for adolescent idiopathic scoliosis: an information statement by the scoliosis research society international task force. Scoliosis. 2013;8:17. doi: 10.1186/1748-7161-8-17. Epub 2013/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ohrt-Nissen S, Hallager DW, Henriksen JL, Gehrchen M, Dahl B. Curve Magnitude in Patients Referred for Evaluation of Adolescent Idiopathic Scoliosis: Five Years’ Experience From a System Without School Screening. Spine Deformity. 2016;4(2):120–4. doi: 10.1016/j.jspd.2015.10.001. doi: http://dx.doi.org/10.1016/j.jspd.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Richards BS, Vitale MG. Screening for Idiopathic Scoliosis in Adolescents. An Information Statement. 2008;90(1):195–8. doi: 10.2106/jbjs.g.01276. [DOI] [PubMed] [Google Scholar]
- 6.Hines T, Roland S, Nguyen D, Kennard B, Richard H, Hughes CW, McClintock SM, Ramo B, Herring T. School Scoliosis Screenings: Family Experiences and Potential Anxiety After Orthopaedic Referral. Spine. 2015;40(21):E1135–43. doi: 10.1097/brs.0000000000001040. Epub 2015/07/15. [DOI] [PubMed] [Google Scholar]
- 7.Yawn BP, Yawn RA, Hodge D, Kurland M, Shaughnessy WJ, Ilstrup D, Jacobsen SJ. A population-based study of school scoliosis screening. JAMA. 1999;282(15):1427–32. doi: 10.1001/jama.282.15.1427. Epub 1999/10/27. [DOI] [PubMed] [Google Scholar]
- 8.Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92(6):1343–52. doi: 10.2106/JBJS.I.01142. Epub 2010/06/03. 92/6/1343 [pii] [DOI] [PubMed] [Google Scholar]
- 9.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. The New England journal of medicine. 2013;369(16):1512–21. doi: 10.1056/NEJMoa1307337. Epub 2013/09/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clinic proceedings. 2012;87(12):1202–13. doi: 10.1016/j.mayocp.2012.08.012. Epub 2012/12/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madhok R, Lewallen DG, Wallrichs SL, Ilstrup DM, Kurland RL, Melton LJ., 3rd Trends in the utilization of primary total hip arthroplasty, 1969 through 1990: a population-based study in Olmsted County, Minnesota. Mayo Clinic proceedings. 1993;68(1):11–8. doi: 10.1016/s0025-6196(12)60013-5. Epub 1993/01/01. [DOI] [PubMed] [Google Scholar]
- 12.Luk KD, Lee CF, Cheung KM, Cheng JC, Ng BK, Lam TP, Mak KH, Yip PS, Fong DY. Clinical effectiveness of school screening for adolescent idiopathic scoliosis: a large population-based retrospective cohort study. Spine (Phila Pa 1976) 2010;35(17):1607–14. doi: 10.1097/BRS.0b013e3181c7cb8c. [DOI] [PubMed] [Google Scholar]
- 13.Fong DY, Lee CF, Cheung KM, Cheng JC, Ng BK, Lam TP, Mak KH, Yip PS, Luk KD. A meta-analysis of the clinical effectiveness of school scoliosis screening. Spine (Phila Pa 1976) 2010;35(10):1061–71. doi: 10.1097/BRS.0b013e3181bcc835. [DOI] [PubMed] [Google Scholar]
- 14.Ohtsuka Y, Yamagata M, Arai S, Kitahara H, Minami S. School screening for scoliosis by the Chiba University Medical School screening program. Results of 1.24 million students over an 8-year period. Spine (Phila Pa 1976) 1988;13(11):1251–7. doi: 10.1097/00007632-198811000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg CJ, Dowling FE, Fogarty EE, Moore DP. School scoliosis screening and the United States Preventive Services Task Force. An examination of long-term results. Spine. 1995;20(12):1368–74. Epub 1995/06/15. [PubMed] [Google Scholar]
- 16.Morais T, Bernier M, Turcotte F. Age- and sex-specific prevalence of scoliosis and the value of school screening programs. Am J Public Health. 1985;75(12):1377–80. doi: 10.2105/ajph.75.12.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Calonge N. Screening for Idiopathic Scoliosis in Adolescents. 2004. [Google Scholar]
- 18.Jakubowski TL, Alexy EM. Does school scoliosis screening make the grade? NASN school nurse (Print) 2014;29(5):258–65. doi: 10.1177/1942602X14542131. Epub 2014/10/03. [DOI] [PubMed] [Google Scholar]
- 19.Adobor RD, Rimeslatten S, Steen H, Brox JI. School screening and point prevalence of adolescent idiopathic scoliosis in 4000 Norwegian children aged 12 years. Scoliosis. 2011;6:23. doi: 10.1186/1748-7161-6-23. Epub 2011/10/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plaszewski M, Bettany-Saltikov J. Are current scoliosis school screening recommendations evidence-based and up to date? A best evidence synthesis umbrella review. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2014;23(12):2572–85. doi: 10.1007/s00586-014-3307-x. Epub 2014/04/30. [DOI] [PubMed] [Google Scholar]
- 21.Yamamoto S, Shigematsu H, Kadono F, Tanaka Y, Tatematsu M, Okuda A, Iwata E, Koizumi M, Tanaka Y. Adolescent Scoliosis Screening in Nara City Schools: A 23-Year Retrospective Cross-Sectional Study. Asian spine journal. 2015;9(3):407–15. doi: 10.4184/asj.2015.9.3.407. Epub 2015/06/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grivas TB, Hresko MT, Labelle H, Price N, Kotwicki T, Maruyama T. The pendulum swings back to scoliosis screening: screening policies for early detection and treatment of idiopathic scoliosis - current concepts and recommendations. Scoliosis. 2013;8(1):16. doi: 10.1186/1748-7161-8-16. Epub 2013/10/30. [DOI] [PMC free article] [PubMed] [Google Scholar]