Abstract
Objective
To identify how family advocates and clinicians describe disparities in NICU quality of care in narrative accounts.
Study design
Qualitative analysis of a survey requesting disparity stories at the 2016 VON Quality Congress. Accounts (324) were from a sample of RNs (n = 114, 35%), MDs (n = 109, 34%), NNPs (n = 55, 17%), RN other (n = 4, 1%), clinical other (n = 25, 7%), family advocates (n = 16, 5%), and unspecified (n = 1, <1%).
Results
Accounts (324) addressed non-exclusive disparities: 151 (47%) language; 97 (30%) culture or ethnicity; 72 (22%) race; 41 (13%) SES; 28 (8%) drug use; 18 (5%) immigration status or nationality; 16 (4%) sexual orientation or family status; 14 (4%) gender; 10 (3%) disability. We identified three types of disparate care: neglectful care 85 (26%), judgmental care 85 (26%), or systemic barriers to care 139 (44%).
Conclusions
Nearly all accounts described differential care toward families, suggesting the lack of equitable family-centered care.
Introduction
Quality-of-care delivery across neonatal intensive care units (NICUs) varies greatly [1], and vulnerable populations may be at risk for receiving suboptimal care, translating into suboptimal outcomes. We recently demonstrated statistically significant racial/ethnic variations in quality of care both between NICUs and within NICUs [2]. These findings reflect multiple mechanisms that create overall disparity. First, minority infants may be more likely to receive care in poor quality NICUs [1–7]. Very low birth weight (VLBW) infants born in high-black concentration hospitals have higher rates of infection, discharge without breast milk, and nurse understaffing [3] and these structural barriers likely translate to higher risk-adjusted VLBW infant mortality and morbidity rates [4–6]. Second, minority infants may be more likely to receive suboptimal care within a given NICU [2, 8–10]. Hispanic mothers have been found to be less likely than whites to receive antenatal steroids [9] and human breast milk feeding [10] at discharge within a given institution. Further, qualitative research [8] found that black non-Hispanic women have reported limited breastfeeding education and support in the NICU. However, breastfeeding at discharge may be a complex measure of NICU quality, given that non-NICU factors such as social support networks are key in establishing breastfeeding at NICU discharge [11].
The breastfeeding example highlights that the quality of NICU care is intricately linked to how NICU clinicians engage with families and their social attributes. However, little is known regarding the interactional and systemic factors that contribute to disparities in care delivery. The objective of this study was to understand these factors through personal experiences from NICU clinicians and family advocates of observed racial/ethnic disparities in neonatal care. We sought to understand how disparities in NICU care emerge in the course of family–clinician interactions or as a result of other barriers to quality care. Our primary interest was in racial/ethnic disparities in care. However, because race is just one of multiple and intersecting sources of inequality that can affect an individual’s or family’s experience in health care [12], the accounts discussed here reflect the interaction of race with other family-level and hospital-level factors and provide a unique lens with which to view clinician–patient encounters.
Methods
We surveyed a convenience sample of neonatal clinicians and family advocates during a plenary presentation at the 2016 Vermont Oxford Network (VON) Annual Quality Congress. VON is a collaboration of health-care professionals representing >1000 NICUs from around the world that submit their data with a shared goal of improving the quality and safety of medical care for newborn infants and families. [13]. The Annual Quality Congress is among the main meetings for neonatal providers and family advocates who are engaged in quality improvement activities. Plenary attendees were asked to submit an account of an observed racial/ethnic disparity in NICU care via a real-time Qualtrics electronic survey on their mobile devices. In separate fields, the survey also collected the presumed race/ethnicity of the patient (American Indian or Native American, Asian, black or African American, Hispanic or Latino, and white), the length of time since the event occurred (<6 months ago, 6–12 months ago, 12–24 months ago, >24 months ago), as well as respondent’s position (physician (MD), neonatal nurse practitioner (NNP), registered nurse (RN), respiratory therapist (RT), parent, or other—specify).
There were an estimated 1275 attendees at the plenary presentation and we obtained 336 surveys. Twelve surveys were excluded for non-completion of the disparity story, leaving 324 narrative accounts for analysis. Informed consent was obtained and the study was approved by the Stanford Institutional Review Board.
Analysis
Results were analyzed using Dedoose (Version 7.5.14, SocioCultural Research Consultants, LLC), a mixed-methods software platform. We employed grounded theory methods in coding the data, which allows themes to emerge [14]. We coded accounts according to the patient-level characteristics invoked by respondents in their description of observed disparities in care. The vast majority (312, 96%) of accounts implied that care was suboptimal as a result of the disparate treatment of families, and a small number implied that care was privileged. We use the term “care” here in a broad sense to encompass treatment, interactions, and perceptions of the overall experience. Care, as used in this analysis, does not necessarily imply outcomes or lack/presence of a specific type of clinical intervention. We identified three types of suboptimal care—neglectful care, judgmental care, and systemic barriers to care. These types were identified as the coding scheme developed via the constant comparison method and memo writing [14]. The salience of overlapping dimensions of differences emerged from this analytic process, of which race and ethnicity were just two. A significant number of accounts included language barriers experienced by non-native English-speaking families, cutting across the race and ethnicity dimensions. The small number of accounts that implied better care as a result of disparate treatment were analyzed separately and memos were written to compare these accounts with the larger sample. A second analyst checked the coding scheme against all accounts, and disagreements were resolved by the two primary analysts. As memos were written, analysts conferred on the coding scheme, emerging themes, and coherence of the data against the analytic framework. In this way, the process generated novel analysis based on new insights [15, 16].
Results
Table 1 describes the participant roles in the study. The majority of participants were clinicians and the minority family advocates. Table 2 displays story characteristics, including infant race/ethnicity as presumed by respondent and length of time since the event. Accounts were distributed across presumed racial/ethnic groups, with Hispanic/Latino making up the largest group (120, 37%). Over half of the accounts occurred within the prior 6 months (169, 52%).
Table 1.
Study participant roles
| Estimated VON attendees | 1275 | |
| Total survey respondents | 324 | 100% |
| Nurses | 173 | 53% |
| Registered nurse | 114 | 35% |
| Neonatal nurse practitioner | 55 | 17% |
| RN Other (nurse educator, nurse technician) | 4 | 1% |
| Medical doctor | 109 | 34% |
| Clinical other (RD, PT, PA, Pharm) | 22 | 7% |
| Respiratory therapist | 6 | 2% |
| Administrator | 6 | 2% |
| Lactation consultant | 3 | 1% |
| Physiotherapist | 2 | <1% |
| Social worker | 2 | <1% |
| Registered dietitian | 1 | <1% |
| Physician assistant | 1 | <1% |
| Pharmacist | 1 | <1% |
| Family advocates | 16 | 5% |
| Not specified | 4 | 1% |
Table 2.
Racial/ethnic characteristics of infants as presumed by respondent and timing of story
| Race/ethnicity of patient in story | ||
| Total respondents | 324 | 100% |
| Hispanic or Latino | 120 | 37% |
| Black or African American | 73 | 23% |
| Asian | 62 | 19% |
| White | 57 | 18% |
| No data provided | 7 | 2% |
| American Indian or Native | 5 | 2% |
| Timing of story | ||
| <6 months ago | 169 | 52% |
| 6–12 months ago | 63 | 19% |
| 12–24 months ago | 37 | 11% |
| >24 months ago | 24 | 6% |
| Not specified | 2 | 1% |
Accounts predominantly described how families, rather than their babies, were treated differently. Accounts were for the most part told from the perspective of an observer, rather than that of a clinician involved in a particular case. The survey question on the patient’s race/ethnicity did not fully encapsulate relevant disparity dimensions described in the accounts. Table 3 shows the family factors as described in the accounts. We conceptualized these factors as dimensions of difference that rendered families vulnerable to suboptimal care. The most frequent dimension of difference concerned non-native English-speaking families and resultant language barriers. Because some accounts exhibited multiple dimensions, the total exceeds 100%.
Table 3.
Family factors that were salient dimensions of difference in accounts of disparity
| Language | 151 | 47% |
| Culture or ethnicity | 97 | 30% |
| Race | 72 | 22% |
| SES | 41 | 13% |
| Drug use | 28 | 8% |
| Sexual orientation or family status | 16 | 4% |
| Immigration status | 18 | 5% |
| Gender | 14 | 4% |
| Disability | 10 | 3% |
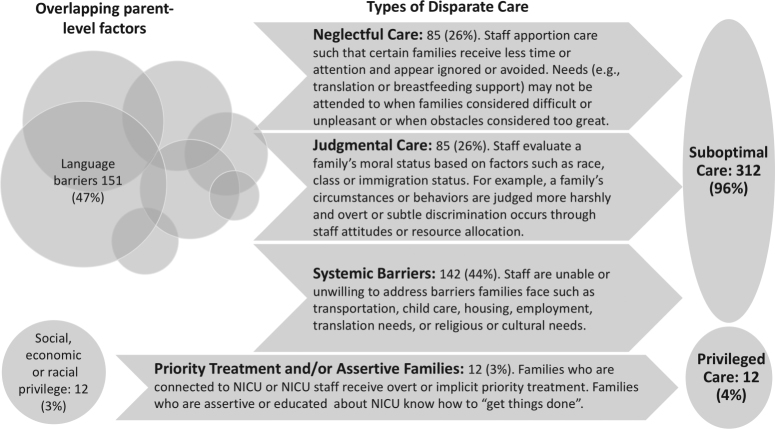
Nearly all accounts (312, 96%) implied that disparate treatment resulted in suboptimal care. We identified three major types of suboptimal care in the accounts: neglectful care (85), judgmental care (85), and systemic barriers to care (139). See Fig. 1 for representation of the types and Table 4 for illustrative accounts. Many accounts recounted by family advocates poignantly described judgmental care, emphasizing perceived racist or otherwise offensive provider attitudes. Just 12 (4%) accounts focused on privileged care.
Fig. 1.
Types of disparities in care. Accounts described neglectful care, judgmental care, and systemic barriers to care leading to suboptimal care or priority treatment or assertive families leading to better care Overlapping family-level factors led to suboptimal care, whereas social, economic, or racial privilege let to better care.
Table 4.
Illustrative accounts of implied worse care
| Neglectful care |
| A family in the NICU was from the Middle East and the mom had a language barrier. The dad was an engineer and very demanding and in extreme denial of his infant’s outcome. Staff avoided going to the room, especially when dad was present. I started to notice that the medical team avoided rounding at the bedside when dad was present and this just widened the gap in care for this infant.—NNP regarding family identified as Asian |
| A Spanish-speaking mother of a 23-week infant was not provided with a translator before, during, or after delivery to explain what has happening with her baby. I asked for an interpreter to come in to the hospital to help with this special situation and faced push back because it was late at night. The L&D staff thought a translator phone should be sufficient. I felt that the situation would not have been met with such a lack of empathy had the mother been of a different ethnicity.—MD regarding family identified as Hispanic or Latino |
| A mom approached her infant in an open crib, picked her up, and began trying to put her to breast. Mom’s position was not optimal and the infant wasn’t latching well. The RN approached and was quick to try and convert the breastfeeding attempt to a bottle feeding probably due to the extra time needed related to language barrier and getting lactation help.—RN regarding family identified as Asian |
| Judgmental care |
| I see this all the time… the way we treat black moms is definitely different than how we treat white moms. And age plays a factor too—young moms are judged very unfairly. One black mom was judged very harshly for being late for a feeding even though she had a long and challenging transit ride to get to the hospital. A white mother who was late on the same day was greeted with sympathy. A small example but I see moments like this every single day. Also, young black moms who might well have a very good reason for being wary with authority figures (based on years of being treated badly in the system) are judged harshly for “showing attitude”. – Family advocate regarding family identified as black or African American |
| Our front-line staff (greeter-unit secretaries) react very differently to black families than they do to the traditional white married families. Sometimes they can’t even make eye contact. There is a big need for diversity training.—Nurse Technician (RN Other) regarding family identified as black or African American |
| Mother in recovery shared the judgement and unkindness she experienced as being labeled a “drug mom” and her daughter a “drug baby” as she was NAS from methadone treatment. She was 4 years clean and sober and still wanted to hide in guilt and shame from the feeling of being an outsider among the others in the unit.—Director (Clinical Other) regarding family identified as Native or American Indian |
| Systemic barriers to care |
| I see disparity based on resources and home support for families to be able to visit their babies and partake in their care—this includes many different races and based more on socioeconomic status, but often is black families. These families are limited by care for other children, transportation, etc.—MD regarding family identified as black or African American |
| Parent was shamed by physician and social worker for “not being at bedside appropriate amount of time”. Parents spoke limited English and had no understanding of the social service protocols or resources. The team essentially was expressing discomfort that the hospital was funding a stay at our local hospitality house but family wasn’t present “enough” at the bedside. But, we had provided no guidance about what was “enough” or “expected”. Family felt shamed and embarrassed that they had not been living up to care team’s UNSPOKEN expectations.—Family advocate regarding family identified as Asian |
| We cared for a baby whose mother was Asian. She was unable to visit her baby for about a month because of cultural beliefs that she needed to be indoors following delivery. We did not have the capacity to provide a room for her to stay in after discharge for this extended length of time. I believe this interfered with initiation of breastfeeding and maternal-infant bonding. It was also difficult for staff to understand her need to comply with these cultural practices.—MD regarding family identified as Asian |
| Overlapping language barriers to care |
| “I have so many stories—I work at a hospital that is mainly black and Hispanic. A critical issue is language! Let’s face it, parents that speak English are always updated more frequently and more engaged in the care of their infant—and we have incredible translator services”.—MD regarding family identified as Hispanic or Latino |
| “Because this family couldn’t speak English this family wasn’t offered video connection because it took too long to get the interpreter and was considered to be basically a “pain”. This mom didn’t get to see the baby before she died”.—RT regarding family identified as Hispanic or Latino |
| “There was a delay for the parents to hold their baby of about 4 days because of language barrier. Parents did not understand that they could visit, hold and even get involved in the care such as feeding, bathing, their baby despite using a language line to explain what was going on. We realized the initial interpreter used a different dialect—so these parents didn’t simply understand.”—MD regarding family identified as black or African American |
| Illustrative stories of implied better care |
|---|
| Privilege and elite care |
| A physician’s baby was transferred into our unit. Baby was given special treatment, room preference. Attending generally change every two weeks, yet this patient kept the same attending as well as given patent updates privately by the attending. It’s not how we treat every patient.—RN regarding family identified as white |
| We have a “friends and family” program where people who have donated or affiliated to our hospital executives or board members are enrolled in a special program where they get priority treatment for scheduling doctor appointments and if hospitalized are visited by this department to assist in anyway. Often rules are not applicable to this group. They receive preferential treatment from the organization.—RN regarding identified as white |
Neglectful care
Accounts of neglectful care (85, 26%) described NICU staff using their discretion to apportion care resulting in certain families receiving less time or attention than they needed or in staff showing an unwillingness to go the extra mile for certain families. We define neglectful care as paying less attention to certain families, not as providing no attention to those families. These accounts described components missing in the clinician–family interactions, often attention, resources, or timely responsiveness that amounted to differences in care. Clinicians were described as strategically paying less attention to certain families to account for time or resources constraints. A typical story of neglectful care described families who were perceived as difficult or with unrealistically high needs and staff apportioning their efforts accordingly, to the families’ detriment.
Many accounts highlighted families not being updated or educated as often or as thoroughly as others and experiencing less optimal staffing (e.g., primary nursing care) or other resources that required additional staff (e.g., translation services, breastfeeding support, video conferencing, attendance at rounds, or accommodating cultural needs). Accounts stressed the potential harms of neglectful care (particularly parental isolation or distrust) while stating that such harms are often invisible to clinicians, given the need to allocate resources and how neglectful care can be institutionalized in a workplace culture. We found a cluster of accounts referencing nurses routinely “ignoring” families who didn’t speak English and not using translators regularly such that families were isolated and left wondering how their babies were doing. Other accounts of unmet (or misunderstood) cultural needs where language and socio-economic status simultaneously accounted for why families received suboptimal care.
Judgmental care
Accounts of judgmental care (85, 26%) described NICU staff overtly or subtly evaluating families’ moral status, based on dimensions of difference (see Table 3). Many accounts of judgmental care were framed as incidents where families’ circumstances or behaviors were judged harshly, given their race/ethnicity, socioeconomic status, or history of drug use. Other accounts of judgmental care related NICU staff using offensive language reflecting racially or otherwise biased attitudes toward families and their circumstances. For example, staff were said to make fun of black sounding names, describing a single mom as having “made her bed” and a young father as a “baby daddy”. Other accounts revealed staff discomfort with non-white, non-heteronormative families. Many respondents noted that biased attitudes and offensive language likely result in vulnerable families spending less time in the unit with their babies or engaging less with NICU clinicians because of a lack of trust and rapor with clinicians. Further, many accounts suggested that this sort of biased treatment is common and goes unaddressed. We also noted several judgmental care accounts featuring African American or black families who were assumed to be violent, difficult, or at fault for their life circumstances, in contrast to white families who were given more leeway in displaying a variety of emotions and behaviors.
Systemic barriers to care
Nearly half of the accounts 139 (44%) focused on systemic organizational or cultural barriers to care. Systemic barriers identified by respondents included a variety of factors that made the families unable to be present in the NICU and/or to perform as expected by providers. Many accounts described barriers families faced that hindered their ability to be physically present in the NICU (e.g., poor transportation, poor housing, employment demands, or other children at home). Other accounts discussed rigid visiting, rounds, or consultation schedules or an inability/unwillingness to develop a therapeutic alliance with relatively absent families. In most cases, these accounts centered on families with low socio-economic status and other intersecting forms of disadvantage (prior premature birth or language issues) whose lives could not be put on hold to look after a preterm baby in the NICU or post discharge. Some accounts brought up the challenges of bringing a high needs infant into a home with minimal financial, familial, or neighborhood resources or unstable housing. These accounts illustrated how language or cultural barriers amplify systemic barriers, further distancing families from caring for their infants while hospitalized.
Other accounts pointed to systemic barriers to a family integration in the NICU as caregivers for their infants based on cultural conflicts. Here we use the term “cultural” not just to refer to the cultures of families but also the cultures of NICUs with an institutional culture of the way things are done [17]. As such, an NICU can impose expectations unknown to, or unable to be met by, families. Some accounts told of families who expected paternalistic care and/or were unaware of the demands put on them (e.g. being present in the NICU, making health-care decisions for their infant) until their fitness as families was called into question. Other accounts focused on families of color who lacked trust in health-care clinicians and institutions or families with low health literacy or literacy skills that affected their ability to participate fully in the NICU.
The accounts of systemic barriers to care presented a tangle of organizational and cultural barriers to care. For instance, we identified accounts of parents who were undocumented migrant workers who could not spend time in the NICU because of employment and transportation barriers and were simultaneously not comfortable making demands of the care team for fear of deportation. We found numerous accounts of Asian mothers who follow a traditional practice of remaining in bed (and thus not spending time in the NICU) after the birth of an infant. In these accounts, such mothers were not seen to be committed to the care of their infant by the NICU care team. See Table 4 for illustrative accounts.
Overlapping language barriers to care
Almost half of the accounts, 151 (47%), featured language barriers experienced by NICU families. These language barriers cut across, and were described as exacerbating, all three types of suboptimal care (neglectful care, judgmental care, and systemic barriers to care). Overall, language barriers implied that non-English speaking families are at a disadvantage by not being equally integrated in the care of their infants, even when translation services are available. When analyzed separately, these accounts described the isolation, delays, or missed opportunities for care that can occur when families are not fluent in English. Accounts of language barriers reflected on the isolation that non-English-speaking families can experience arising out of not adequately understanding their babies’ complex medical condition, not actively engaging in their infant’s care, and not receiving adequate emotional and social support. Often accounts specified how translation services, even when available, are incorrectly or inadequately used by NICU staff (e.g., specific dialects unavailable or wrongly identified, sign language unavailable, translation only available at certain times of day), and how this led to negative consequences for the infant. Some accounts commented on the important role clinical and support staff play who speak a second language have in supporting non-English families in the NICU. See Table 4 for illustrative accounts.
Privileged care
While the vast majority 312 (97%) of the accounts implied suboptimal care arose from disparate treatment, a small number (12, 3%) indicated that families with racial, financial, or social privilege received better care. Some accounts implied privilege because elite treatment for benefactors and employees was embedded within official NICU and hospital policy. In others, elite treatment occurred when families personally known to staff were treated preferentially. Finally, some accounts implied that parental assertiveness in communicating their needs and demands led to privileged care. Nearly all of these accounts featured white families.
Discussion
This study revealed that the primary “targets” of disparate care in NICUs are not the infants but families. We identified three types of disparate care: neglectful care, judgmental care, and systemic barriers to care. Intersectional dimensions of difference emerged across all types of suboptimal care but language barriers were an important dimension of difference cutting across all types of disparate care. Accounts of language barriers revealed the consequences of unmet translation needs (e.g., isolation and delays) as well as misuse of available translation services and inadequacy of available translation services to meet family needs. Together, the accounts suggest that families’ racial/ethnic, social, financial, cultural, and linguistic characteristics may influence interactions with NICU providers and that secondarily care for infants may suffer.
Overall, narratives portrayed the isolation of non-English speakers, lack of empathy for drug-using mothers or absentee families, lack of accommodation for cultural needs, and overt racist treatment of black families. We noted a cluster of judgmental care accounts featuring black families who were assumed to be violent, difficult, or at fault for their life circumstances, as opposed to white families who were given more leeway in displaying a variety of emotions and behaviors in the NICU. Overall, the 324 stories analyzed here support the view that unequal treatment and opportunity can exist in NICUs just as it does in other institutions and areas of society.
Our interpretation of the data may minimize the agency of families in navigating a health-care encounter. Theories of cultural health capital (CHC) [18] are useful to understand how families are active in the health-care interaction and “how broad social inequalities operate in patient-provider interactions, and shape the content and tone of health care encounters.” [18] (p.1). Shim defines CHC as “the repertoire of cultural skills, verbal and nonverbal competencies, attitudes and behaviors, and interactional styles, cultivated by patients and clinicians alike, that, when deployed, may result in more optimal health care relationships.” [18] (p.1). The disparity accounts in this analysis describe encounters where CHC has not been successfully exchanged. Families have differential access to clinically valuable resources—in this case, the skills and resources for parenting in the NICU—and clinicians have differential abilities and resources for optimizing a family’s CHC. Differential access to CHC can follow racial and socioeconomic lines [18] and other dimensions of difference identified here. Some accounts explicitly addressed differential access to CHC, while others revealed how disparities arise from clinician implicit bias around CHC via clinicians valuing or de-valuing specific culturally mediated ways of parenting or being a family. This point is similar to observations made over 20 years ago by Anspach [19] about the types of family behaviors that are valued in the NICU.
Family-centered care, “an approach to health care that is respectful of and responsive to individual families’ needs and values” has been identified as a critical factor for ICUs to improve outcomes for patients and their caregivers [20]. Guidelines for best practices for family-centered care in the ICU have recently been developed; however, evidence for their role in addressing health-care disparities remains weak [20]. Additional focus on family-centered care measure development would be an important mechanism for tracking disparities in the NICU, given the way they are described in our accounts. Instituting a standard for family-centered care could potentially particularly benefit affluent, white, English-speaking families and maybe even increase disparity if the interactional and cultural issues we found in this study are not attended to in standard development and implementation, as is the case with other quality improvement work in the area of racial disparities [21]. Further research needs to be sensitive to this tension by engaging the perspectives of diverse families with the awareness that clinicians have the ability to empower or disempower families in deploying CHC [18].
Roberts has argued that there are two primary inadequate analyses of racial disparities in health: equating race with socioeconomic status or equating race with genetics [22]. We think that our focus on the perspectives of clinicians and families, along with our analysis on the multiple dimensions of difference these perspectives raise, avoids these pitfalls. Feagin and Bennefield [23] urge analysts to address systemic racism in U.S. health care rather than narrowly limiting analyses to bias, stigma, or stereotypes. These accounts of disparate care suggest us to address the systemic aspects of NICUs that maintain unequal treatment.
This study should be viewed in the context of its design. Our sample of NICU providers and family advocates may not easily generalize given VON’s longstanding focus on family-centered care and quality improvement. Although the VON quality congress is not limited to VON member sites, the vast majority of quality congress attendees come from VON member centers (95%) (Horbar J, Buus-Frank M. Personal Communication, 2017). While in some states NICUs are required to join VON, in most states, membership is voluntary. Responses may reflect higher-performing NICUs in this regard. Despite our study’s bias toward sampling from NICU providers who may be more focused on family-centered care and quality improvement, it should be noted that 90% of the VLBW infants in the US are in the VON database and cared for at VON data submitting centers (Horbar J, Buus-Frank M. Personal Communication, 2017). We note that family advocates at VON are not necessarily representative of NICU families in general. Parents who attend VON, termed “family advocates” or “family representatives” have been invited by quality improvement teams at their respective NICUs (Horbar J, Buus-Frank M. Personal Communication, 2017) and are thus families with the social and economic resources to commit to their participation.
Of an estimated 1275 attendees at the plenary presentation, we obtained 324 narrative accounts for analysis. This response rate may imply that the remaining audience members did not have a disparity account to share. However, because we did not ask respondents “do you have an account of disparate care?”, we cannot assume this. It may also be that non-responders were not comfortable writing on this topic, did not have a device on which to respond, or were not in attendance or otherwise able to participate. Our sample is thus biased toward those who have witnessed and were able and willing to describe disparate care for this study. Our intent was not to determine a rate or frequency of disparities in NICU care but rather to explore the mechanisms through which disparate care can occur. As such, we see the 324 accounts as revelatory of the dynamics of disparate care of families in NICUs. Similarly, the absolute frequency of types of disparate care or frequency of particular dimensions of difference should not be over-interpreted. For instance, our findings may be biased in that accounts about language barriers are generally easier to report than more egregious examples involving race. Had we known that non-responders did not have a disparity story, our interpretation of the collected stories would remain the same. However, we would wonder why certain clinicians or family advocates report disparate care, while others do not. Despite the low response rate, the ease with which respondents spontaneously recorded disparity accounts (52% occurred within the past 6 months) during a 3-min exercise in the midst of a lecture suggests that disparities in care are not uncommon occurrences. Indeed, several accounts included statements about recurring observations (as in “I see this all the time…”).
Our study may be used to generate hypotheses about the mechanisms and dynamics of disparities in clinical encounters. Specifically, our findings indicate that adverse consequences of disparate care for infants is mediated through adverse interactions with families more so than through direct differences in care to the infant. Accounts include delays in holding, delays in breastfeeding, lack of proper supports for under-resourced families, and lack of understanding or accommodating families’ wishes or circumstances, all of which may lead to suboptimal neonatal outcomes. All families should receive attentive and respectful care that addresses the organizational and cultural constraints of parenting in the NICU. A family’s diminished presence in the NICU or communication with clinicians likely impacts the health of the neonate through less kangaroo care, parental education, and breastfeeding at discharge.
Conclusion
This study suggests that vulnerable populations may be subject to disparate care in the NICU as they interact with their infants’ health-care team. These disparities are likely experienced by families across a variety of dimensions, including but not limited to race/ethnicity. These disparities appear to mirror general societal inequalities in vulnerable populations and exert their negative effects on patient care through suboptimal engagement with diverse families. Optimal care in the NICU requires family presence and trusting relationships between parents and clinicians. We see a need for standardization and implementation of family-centered care in the NICU to guarantee engagement with diverse families in the care of their neonates. We hope that this study can generate further investigation into the ways family-centered care is differentially experienced by families and spark interventions and strategies to improve care for all diverse families.
Electronic supplementary material
Acknowledgements
We would like to thank the Vermont Oxford Network for bringing together families and clinicians in a venue where we could conduct this survey. We are grateful to the families and clinicians who shared their accounts. We would also like to thank those who reviewed early drafts of this manuscript, especially Lelis Vernon and Marybeth Fry, and also Taylor Cruz, Kate Darling, Jeffrey Horbar, Natalie Ingraham, and Henry Lee.
Funding
All the authors are supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD083368-01, PI Profit).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Disclaimer:
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Change history
7/24/2018
The original HTML version of this Article incorrectly showed the copyright holder to be ‘Nature America, Inc., part of Springer Nature’, when the correct copyright holder is ‘The Authors 2018’. This has been corrected in the HTML version of the Article. The PDF version was correct from the time of publication.
Electronic supplementary material
The online version of this article (10.1038/s41372-018-0057-3) contains supplementary material, which is available to authorized users.
References
- 1.Profit J, Zupancic JA, Gould JB, Pietz K, Kowalkowski MA, Draper D, et al. Correlation of neonatal intensive care unit performance across multiple measures of quality of care. JAMA Pediatr. 2013;167:47–54. doi: 10.1001/jamapediatrics.2013.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Profit J, Gould JB, Bennett M, Goldstein BA, Draper D, Phibbs CS, Lee, HC. Racial/Ethnic Disparity in NICU Quality of Care Delivery. Pediatrics 2017;140. [DOI] [PMC free article] [PubMed]
- 3.Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2014;50:374–97. doi: 10.1111/1475-6773.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morales LS, Staiger DO, Horbar JD, Carpenter J, Kenny M, Geppert J, et al. Mortality among very low-birthweight infants in hospitals serving minority populations. Am J Public Health. 2005;95:2206–12. doi: 10.2105/AJPH.2004.046730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lake ET, Staiger D, Horbar J, Cheung R, Kenny MJ, Patrick T, et al. Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307:1709–16. doi: 10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howell EA. Racial disparities in infant mortality: a quality of care perspective. Mt Sinai J Med. 2008;75:31–35. doi: 10.1002/msj.20018. [DOI] [PubMed] [Google Scholar]
- 7.Lee HC, Gould JB, Martin-Anderson S, Dudley RA. Breast-milk feeding of very low birth weight infants as a function of hospital demographics. J Perinatol. 2011;31:S82–S82. doi: 10.1038/jp.2010.179. [DOI] [Google Scholar]
- 8.Cricco-Lizza R. Black non-Hispanic mothers’ perceptions about the promotion of infant-feeding methods by nurses and physicians. J Obstet, Gynecol, Neonatal Nurs. 2006;35:173–80. doi: 10.1111/j.1552-6909.2006.00033.x. [DOI] [PubMed] [Google Scholar]
- 9.Lee HC, Lyndon A, Blumenfeld YJ, Dudley RA, Gould JB. Antenatal steroid administration for premature neonates in California. Obstet Gynecol. 2011;117:603–9. doi: 10.1097/AOG.0b013e31820c3c9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee HC, Gould JB. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J Pediatr. 2009;155:657–62. doi: 10.1016/j.jpeds.2009.04.064. [DOI] [PubMed] [Google Scholar]
- 11.Fleurant E, Schoeny M, Hoban R, Asiodu IV, Riley B, Meier PP, et al. Barriers to human milk feeding at discharge of very-low-birth-weight infants: maternal goal setting as a key social factor. Breastfeed Med. 2017;12:20–27. doi: 10.1089/bfm.2016.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smedley BD, Stith AY, Nelson AR, Institute of Medicine (U.S.). Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, D.C.: National Academy Press; 2003. [PubMed]
- 13.Vermont Oxford Network. Membership FAQs. [cited June 1, 2017]. Available from: https://public.vtoxford.org/how-to-become-a-member/membership-faqs/
- 14.Feagin J, Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. 2014;103:7–14. doi: 10.1016/j.socscimed.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- 16.Clarke A. Situational analysis: grounded theory after the postmodern turn. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]
- 17.Kaufman SR. And a time to die: how American hospitals shape the end of life. New York: Scribner; 2005. [Google Scholar]
- 18.Shim JK. Cultural health capital: a theoretical approach to understanding health care interactions and the dynamics of unequal treatment. J Health Soc Behav. 2010;51:1–15. doi: 10.1177/0022146509361185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anspach RR. Deciding who lives: fateful choices in the intensive-care nursery. Berkeley, CA: Univ of California Press; 1997.
- 20.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–28. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 21.Lion KC, Raphael JL. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135:354–61. doi: 10.1542/peds.2014-2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberts DE. Debating the cause of health disparities -- implications for bioethics and racial equality. Camb Q Healthc Ethics. 2012;21:332–41. doi: 10.1017/S0963180112000059. [DOI] [PubMed] [Google Scholar]
- 23.Schulz AJ, Mullings L. Gender, race, class, and health: intersectional approaches. San Francisco, CA: Jossey-Bass; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.