Abstract
Background:Shared medical appointments (SMAs) are utilized across health care systems to improve access and quality of care, with limited evidence to support the use of SMAs to improve clinical outcomes and medication adherence among hypertensive patients. Objective: Improve access and quality of care provided within a Veterans Affairs health care system via implementation of a hypertension SMA to improve clinical outcomes and medication adherence. Methods: Veterans were eligible for enrollment in the SMA if they received care within the health care system, were aged ≥18 years, were receiving at least 2 antihypertensive medications, and had systolic blood pressure (SBP) >140 mm Hg or diastolic blood pressure (DBP) >90 mm Hg. A pre/post cohort design was used to evaluate the improvement in antihypertensive medication adherence as well as the change in SBP and DBP for all Veterans who attended at least 2 SMAs. Results: Twenty-one Veterans participated in at least 2 SMAs and were included in the analysis; 76.2% had a reduction in SBP with an overall average decrease of −8.3 mm Hg (P = .02). The proportion of Veterans considered to have controlled blood pressure (BP; <140/90 mm Hg) increased from 14.3% at baseline to 42.9% during the SMA period (P = .03). There was no significant difference found for the proportion of Veterans considered adherent to their prescribed antihypertensive medications (95.2% vs 85.7%, respectively; P = .50). Conclusions: SBP significantly improved for patients enrolled in a pharmacist-led SMA at a VA health care system, and the proportion of patients considered to have controlled BP increased significantly.
Keywords: adherence, antihypertensives, hypertension, pharmacist/physician issues, ambulatory care
Background
Cardiovascular disease is the leading cause of death in the United States, with more than 610 000 deaths attributed to heart disease annually.1 Hypertension is a primary risk factor for cardiovascular disease, contributing to the death of 410 000 Americans in 2014.2 Currently, more than one third of Americans are living with hypertension and fewer than half of those diagnosed have achieved adequate blood pressure (BP) control.3 Additionally, uncontrolled hypertension is the single most important modifiable risk factor for the development of heart failure.4 Medication nonadherence is often regarded as a key factor contributing to uncontrolled hypertension.5
Shared medical appointments (SMAs) are used within health care systems across the nation to improve clinical outcomes and access to health care, and are common practice within the Department of Veterans Affairs. SMAs are a redesigned system of health care delivery in which a medical provider (ie, physician, pharmacist, advanced nurse practitioner, and/or physician’s assistant) encounters several patients at one time in a group setting. Usually consisting of 10 to 15 patients with the same medical condition, these groups receive disease state education prior to a one-on-one provider-patient encounter allowing individualized education and medication management. SMAs are utilized across health systems to expand access to care, improve health literacy, increase patient participation in a team-based approach to care, and provide peer support to elicit and sustain health behavior change.6
SMAs are widely utilized for the management of diabetes mellitus, with fewer groups designed to improve BP control among patients with hypertension. One systematic review seeking to provide a summary of the effects of group medical visits on staff, patients, and economic outcomes concluded that SMAs improve clinical outcomes for patients with type 2 diabetes mellitus; however, the authors suggest that further studies are needed to support the use of SMAs as an intervention to improve clinical outcomes of other chronic conditions, including hypertension.6 While data on the impact of SMAs on BP control in patients with hypertension is lacking, so is the availability of data on the impact of SMAs on medication adherence.
The results of a population analysis conducted to determine blood pressure control and adherence to prescribed antihypertensive therapy among central Alabama Veterans are published elsewhere.7 After review of that analysis, we implemented pharmacist-led SMAs targeting Veterans with uncontrolled hypertension as part of a quality improvement project within a Veterans Affairs health care system.
Objective
The purpose of this quality improvement project was to improve access and quality of health care for Veterans with hypertension within our health care system through implementation of pharmacist-led SMAs. The aims of the project were to improve hypertension control across our Veteran population by reduction of systolic and diastolic blood pressures and improved adherence to prescribed antihypertensive medications. Primary objectives were to assess the difference in the proportion of Veterans considered adherent to prescribed antihypertensive medications and with adequately controlled BP from the baseline period throughout the intervention period. Secondary objectives included determining the mean changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP) from the baseline period throughout the intervention period as well as the number of pharmacist interventions made throughout the intervention period.
Methods
Project Design and Setting
This quality improvement project was a prospective, pre/post design instituted at 2 primary care facilities, the Ft. Benning VA Clinic in Columbus, GA, and the Montgomery VA Clinic in Montgomery, AL, within the Central Alabama Veterans Health Care System. Baseline data for comparison was gathered for fiscal year 2015 (FY15; October 1, 2014, through September 30, 2015). Recruitment and enrollment occurred during September 2015 prior to the intervention period beginning in October 2015 and lasting until February 2016. After review of the project by the health care system’s leadership, it was determined to meet the guidelines for institutional review board review exemption as a quality improvement project.
Selection Criteria
Four primary care providers (PCPs) were identified and agreed to allow their patients to participate in the SMA with medication management performed by a Clinical Pharmacist Specialist. Veterans were eligible for SMA enrollment if they were enrolled to receive medical care in the previously described health care system, aged 18 years or older, prescribed 2 or more antihypertensive medications, and with an uncontrolled BP (SBP >140 mm Hg or DBP >90 mm Hg) documented in the electronic medical record (EMR) from the most recent clinic visit prior to the time of enrollment. Veterans were included in the pre/post analysis if they attended 2 or more SMAs. There were no defined exclusion criteria for this project. PCPs were provided with a list of Veterans under their care meeting the inclusion criteria, and each identified at least 15 potential participants.
SMA Design
Each Veteran was assigned to participate in the SMA created for their corresponding PCP, providing a total of 4 different SMAs meeting separately during the intervention period. Each group met once a month for a total of 4 meetings; the groups met for an hour and a half with the first 45 minutes dedicated to group education and the remaining time reserved for one-on-one encounters between the pharmacists and patients for individualized hypertension education and medication management. Each individual encounter between the patient and pharmacist may have included specific patient education regarding lifestyle modifications, such as weight management, dietary modifications, smoking cessation, and moderate alcohol consumption as determined necessary by the provider. On average, 2 pharmacists were present for each group meeting allowing approximately 10 to 15 minutes of time for each patient to spend in the one-on-one encounter with the pharmacist.
Over the 4-month period, Veterans received group and individual verbal and written education on hypertension as a disease state and the consequences of improperly managed blood pressure, their antihypertensive medications (including mechanisms of action, adverse effects, importance of adherence, etc), the Dietary Approaches to Stop Hypertension (DASH) eating plan, and stress management. Educational topics were presented by experts for each topic of discussion and included pharmacists, dietitians, psychologists, and social workers. The Clinical Pharmacist Specialists served as the provider for the Veterans enrolled in the SMA and designed drug therapy and monitoring plans in accordance with their defined scopes of practice. Dietitians, psychologists, and/or social workers attended 1 of the 4 group meetings to present information regarding the management of hypertension from their area of expertise. The PCP and nursing staff for each group were invited to attend the monthly meetings.
Medication organizers and blood pressure monitors were provided to Veterans, if they were not already being utilized, for the purposes of allowing self-monitoring of adherence and BP, respectively. During each SMA visit, 2 blood pressure measurements were obtained using an electronic, automatic inflatable blood pressure cuff (Welch Allyn Connex Vital Signs Monitor 6000 Series). One BP reading was taken approximately 10 minutes after arrival and one was taken just prior to the one-on-one encounter, and both were recorded in the EMR. All medication changes made by the Clinical Pharmacist Specialists were also documented in the EMR.
Outcomes
Primary outcomes included the proportion of Veterans considered adherent to their prescribed antihypertensive agents and the proportion of Veterans considered to have adequate BP control. Using the proportion of days covered (PDC) methodology endorsed by the Pharmacy Quality Alliance and National Quality Forum,8 adherence was determined for each Veteran during the 1-year baseline period and 4-month intervention period for the following medication classes: angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), beta-adrenergic receptor blockers (BBs), calcium channel blockers (CCBs), and thiazide diuretics (including thiazide and thiazide-like diuretics). Veterans were considered adherent to their prescribed antihypertensive medications if the PDC was ≥80% (ie, 80% of the days during the baseline and intervention periods were covered by at least one antihypertensive medication). The baseline and intervention period SBP and DBP were calculated for each Veteran using the average of the 3 most recent documented BPs during the specified time periods (FY15 and October 15 through February 16, respectively). Veterans were considered to have adequate BP control if the average BP was <140/90 mm Hg. The number of interventions made by pharmacists throughout the intervention period was determined by reviewing the progress notes in the EMR for each encounter. Other appointments that occurred during the intervention period were not considered, and interventions made by other members of the health care team (ie, PCP) were not tracked.
Statistical Analysis
The proportion of participants with controlled blood pressure and proportion considered adherent to prescribed antihypertensive medications were compared between baseline and intervention periods by McNemar’s exact test for matched pairs of the repeated sample. Differences in mean SBP and mean DBP were evaluated with a paired, 2-tailed t test. For all statistical tests, significance was set at P < .05 and analyses performed using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Results
Enrollment and Demographics
A total of 74 Veterans were selected by their PCP to participate in the SMA. Of the 74 contacted for enrollment, 47 (63.5%) Veterans agreed to participate in the SMA. Out of the 47 Veterans enrolled, 34 (72.3%) Veterans attended at least one group meeting and 21 (44.7%) Veterans met the criteria for inclusion in the project analysis by attending 2 or more SMAs (Figure 1). Of the 21 included in the analysis, 57.1% (n = 12) attended all 4 meetings and 81.0% (n = 17) attended at least 3 of the 4 meetings.
Figure 1.
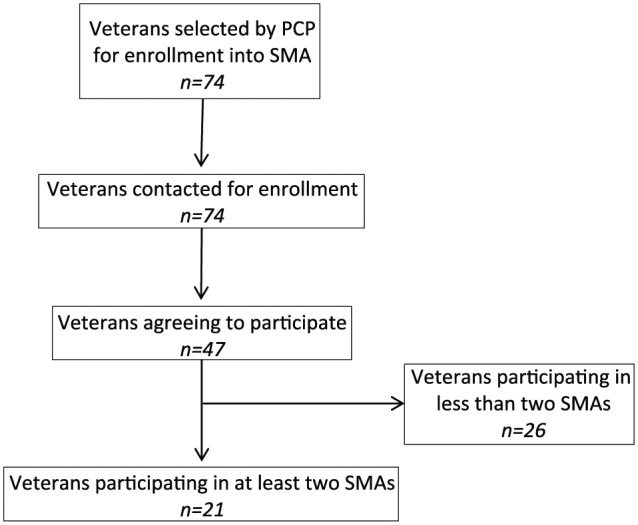
Project flow diagram from Veteran enrollment to project analysis.
For the Veterans included in the analysis, the average age was 61.8 years (range 46-78). The majority of Veterans in the analysis were African American (n = 17; 81.0%); other races represented in the population included Caucasians (n = 3; 14.3%). Race data were unavailable for one Veteran. All 21 of the Veterans included in the final analysis were male. Demographic data are summarized in Table 1.
Table 1.
Characteristics of Veterans Participating in Shared Medical Appointments for Hypertension Education (N = 21).
| Age, years (range) | 61.8 (range 46-78) |
| Race | |
| African American | 17 (81.0%) |
| White | 3 (14.3%) |
| Unknown | 1 (4.8%) |
| Gender | |
| Male | 21 (100%) |
Project Outcomes
There was no significant difference found for the proportion of Veterans considered adherent to their prescribed antihypertensive medications between the baseline and intervention periods (95.2% vs 85.7%, respectively; P = .50). However, the proportion of Veterans with adequately controlled BP increased significantly from the baseline period throughout the intervention period (14.3% vs 42.9%, respectively; P = .03).
Reductions for both SBP and DBP were observed between the baseline and intervention periods. SBP decreased for 76.2% of enrolled Veterans between the baseline and intervention periods with an overall average of −8.3 mm Hg (95% confidence interval = −15.3 to −1.3; P = .02). DBP decreased for 52.4% of enrolled Veterans between the baseline and intervention periods by an overall average of −1.5 mm Hg (95% confidence interval = −4.7 to 1.8; P = .36). The results of the primary and secondary outcomes are summarized in Table 2.
Table 2.
Blood Pressure Change, BP Control, and Antihypertensive Medication Adherence Among Veterans Participating in Shared Medical Appointments for Hypertension Education (N = 21).
| Outcomes | Baseline | Intervention | P |
|---|---|---|---|
| Primary | |||
| Proportion of patients considered adherent to BP medications (PDC ≥80%) | 95.2% | 85.7% | .5 |
| Proportion of patients considered to have controlled BP (<140/90 mm Hg) | 14.3% | 42.9% | .03 |
| Secondary | |||
| Mean change in SBP (mm Hg) | — | −8.3 (95% CI = −15.3 to −1.3) | .02 |
| Mean change in DBP (mm Hg) | — | −1.5 (95% CI = −4.7 to 1.8) | .36 |
Abbreviations: BP, blood pressure; PDC, proportion of days covered; SBP, systolic blood pressure; DBP, diastolic blood pressure; CI, confidence interval.
A total of 37 interventions were performed by the Clinical Pharmacist Specialists across all 4 groups, not including the general education on disease state and drug therapy provided at each encounter; this corresponds to approximately 1.8 interventions performed per patient. The types of interventions detailed in Table 3 include dose titrations (40.5%) and initiation of a new medication (24.3%).
Table 3.
Type of Pharmacist Interventions Performed During the Shared Medical Appointments (Excludes Disease State and Drug Therapy Education).
| Total interventions performed | 37 |
| Dose titration | 15 (40.5%) |
| Blood pressure monitor provided | 9 (24.3%) |
| Initiation of new medication | 9 (24.3%) |
| Discontinuation of medication | 3 (8.1%) |
| Dose taper | 1 (2.7%) |
Discussion
When compared to the baseline data, participants in a pharmacist-led SMA had significant improvements in the attainment of goal BP targets with significant reductions in SBP. The improvement in the number of patients achieving BP targets is likely attributable to a number of factors, including improved patient understanding and involvement in health care decision making, increased accessibility to multiple practitioners of the health care team, consideration of pharmacological as well as nonpharmacological methods to control BP, and improved evidence-based prescribing for the management of hypertension.9 These significant improvements in the number of Veterans achieving goal BP targets were found despite 14.3% of patients being considered to have controlled BP at baseline. This was due to Veterans being referred to the SMA by their PCP based on their most recent clinic BP reading in the EMR being uncontrolled, but then having controlled BP based on the average of the 3 most recent clinic BP readings in FY15.
BP targets for defined BP was set at <140/90 mm Hg for each Veteran during the analysis. However, using the most recent clinical practice guidelines for blood pressure management, a goal BP of <150/90 mm Hg can be considered for patients ≥60 years old without diabetes or renal disease.10 Therefore, it is possible that the current analysis underestimated the actual number of Veterans that may have achieved their patient-specific BP goal, as we did not account for these individualized BP targets in the analysis.
While improvements in SBP and the number of patients achieving BP goals improved significantly, medication adherence did not differ significantly among patients when comparing usual care with SMA participation. However, data from both the baseline and intervention period reflect that an overwhelming majority of patients were considered adherent to their prescribed antihypertensive medications. There are a number of factors that might contribute to this high rate of adherence in the Veteran population, with the most likely being the ease with which Veterans refill their medications via the online refill ordering system as well as the consolidated mail outpatient pharmacy, which allows Veterans to receive refills of their medication by mail several weeks in advance of exhausting their current supply. Additionally, providers may renew or refill all medication orders when Veterans are seen for clinic visits without determining the patients’ actual need for these medications. These factors may artificially inflate the measures of adherence in this population.
The results of our project are consistent with the findings reported by Cohen et al in a similar study designed to assess whether a pharmacist-led SMA could improve attainment of targets for hypertension, hyperglycemia, hyperlipidemia, and tobacco use in patients with type 2 diabetes.11 The researchers found that participants in the SMA achieved target goals for SBP (<130 mm Hg) after 6 months of intervention at significantly greater rates as compared with usual care (58% vs 32.7%, respectively; P = .015), with a mean reduction in SBP of −9.19 mm Hg (95% confidence interval = −14.95 to −3.43). Also similar to the findings of our project, they report that medication possession ratios (another surrogate marker of adherence) did not differ significantly between the usual care and intervention group (0.83 vs 0.87, respectively; P = .193).11
The nonsignificant change in adherence between the baseline and intervention periods is possibly a result of inadequate sample size to detect a difference in adherence during this project, but might also be related to the following limitations. First, the adherence for the intervention period was only measured during a 4-month period of time compared to 12 months for the baseline analysis. Additionally, consideration must be given to the fact that most prescriptions dispensed in the VA are 90-day supplies, which may cause further discrepancies in the determination of adherence when the analysis is over such a short time period. Second, adherence for only first- and second-line medications for the management of hypertension (ie, ACEIs, ARBs, CCBs, thiazide diuretics, and BBs) were included in the evaluation. Some patients presenting to the SMAs were receiving antihypertensive medications that were not included in our analysis, such as hydralazine, clonidine, or spironolactone. Exclusion of these medications may have resulted in an inability to capture a true measure of each patient’s adherence to all prescribed antihypertensive medications. Last, there were several instances of medication discontinuation or dose reduction by the Clinical Pharmacist Specialists for the Veterans who participated in the SMA. Therefore, our method of determining medication adherence may have appeared lower for these patients than their true medication adherence.
Additional limitations of our project include our lack of ability to report more detailed baseline demographics of the patient population, including their comorbid disease states, the number and type of antihypertensive each patient was receiving at baseline, as well as their baseline SBP and DBP. Also, our study did not include the use of a control group and may have included selection bias considering the providers and patients selected to participate in the SMA were not selected using a blinded process. Safety outcomes were not evaluated, which may have been useful in determining patient harms that resulted during the intervention period. Consideration should also be given to the fact that we did not evaluate interventions made by other health care providers outside the SMA model that may have contributed to improved BP control in our population.
Finding high medication adherence with poor control at baseline followed by significantly improved control with medication therapy management during the SMA period suggests that adherence to inappropriate antihypertensive medication(s) or inappropriate doses can lead to poor control of blood pressure. For this reason, efforts to improve evidence-based prescribing of antihypertensive and other medications for the management of hypertension and other disease states in health care systems like ours will likely result in improved outcomes, leading to better patient satisfaction, possible cost containment, and avoidance of complications of poorly controlled blood pressure.12 The development of evidence-based treatment algorithms, among other opportunities to improve provider adherence to clinical practice guidelines within health care systems, may lead to improvements in evidence-based prescribing.12 Additionally, we feel the results of this project demonstrate that both patient education as well as medication management of disease states that is readily achievable via the SMA model have the potential to improve clinical outcomes for chronic diseases, such as hypertension.
Conclusion
The results of this quality improvement project demonstrate that pharmacist-led SMAs improve blood pressure control among patients in a Veterans Affairs health care system. Implementation of pharmacist-led SMAs has the potential to decrease adverse outcomes of poorly controlled hypertension. Investigating the impact of SMAs on medication adherence in a larger population of patients over a longer period of time is warranted.
Acknowledgments
The authors would like to acknowledge the assistance of Emily Piercefield, MD, MPH; Lynsey Neighbors, PharmD, BCPS; and Addison Ragan, PharmD, BCPS, for their dedicated work on the pharmacist-led education project.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Centers for Disease Control and Prevention. Heart disease facts. http://www.cdc.gov/heartdisease/facts.htm. Accessed March 26, 2016.
- 2. Centers for Disease Control and Prevention. High blood pressure fact sheet. http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_bloodpressure.htm. Accessed March 26, 2016.
- 3. Centers for Disease Control and Prevention. Vital signs: Awareness and treatment of uncontrolled hypertension among adults—United States, 2003-2010. MMWR Morb Mortal Wkly Rep. 2012;61:703-709. [PubMed] [Google Scholar]
- 4. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240-e327. [DOI] [PubMed] [Google Scholar]
- 5. Mendis S, Salas M. Hypertension. In: Sabate E, ed. Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 6. Edelman D, McDuffie JR, Oddone E, Gierisch JM, Nagi A, Williams JW., Jr. Shared Medical Appointments for Chronic Medical Conditions: A Systematic Review (VAESP Project #09-010). Washington, DC: Department of Veteran Affairs; 2012. [PubMed] [Google Scholar]
- 7. Piercefield EW, Howard ME, Robinson MH, Kirk CE, Ragan AP, Reese SD. Antihypertensive medication adherence and blood pressure control among central Alabama veterans. J Clin Hypertens. 2017;19:543-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nau DP. Proportion of days covered (PDC) as a preferred method of measuring medication adherence. http://www.pqaalliance.org/images/uploads/files/PQA%20PDC%20vs%20%20MPR.pdf. Accessed May 31, 2016.
- 9. Fletcher RD, Amdur RL, Kolodner R, et al. Blood pressure control among US Veterans: a large multiyear analysis of blood pressure data from the Veterans Administration Health Data Repository. Circulation. 2012;125:2462-2468. [DOI] [PubMed] [Google Scholar]
- 10. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520. [DOI] [PubMed] [Google Scholar]
- 11. Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37:801-812. [DOI] [PubMed] [Google Scholar]
- 12. Kenefick H, Lee J, Fleishman V. Improving Physician Adherence to Clinical Practice Guidelines: Barriers and Strategies for Change. Cambridge, MA: New England Healthcare Institute; February 2008. [Google Scholar]


