Abstract
Background: Food prices influence food choices. Purchasing foods with higher nutritional quality for their price may help improve the diet quality of socioeconomically disadvantaged individuals.
Objective: This study aimed to describe the co-construction and evaluation of the Opticourses prevention program, which promotes healthy eating among participants in socioeconomically deprived situations by improving the nutritional quality of their household food purchases with no additional cost.
Methods: Individuals were recruited in poor districts of Marseille, France. The intervention and evaluation tools and protocols were co-constructed with 96 individuals. Then, 93 adults willing to participate in a standardized intervention comprising 5 participative workshops on diet and budget were enrolled. Impact on food purchases was estimated with experimental economics: 2-d experimental food purchase intents were observed at baseline and endline for workshop participants (WPs, n = 35) and controls (n = 23), with the use of monetary incentives to limit social-desirability bias. Changes in food and nutrient content and energy cost (expressed in €/2000 kcal) of experimental purchases were assessed.
Results: The co-constructed participative workshops included playful activities around food purchase practices and the nutritional quality, taste, and price of foods. Experimental purchases contained a large amount of energy at baseline for both WPs and controls (5114 and 4523 kcal ⋅ d−1 ⋅ person−1, respectively). For WPs only, the mean energy content decreased between baseline and endline (−1729 kcal ⋅ d−1 ⋅ person−1; P < 0.01; medium effect size: Cohen's d = 0.5), and the percentage of energy from free sugars and from foods high in fat, sugar, and salt also decreased (both P < 0.05 and medium effect sizes), whereas energy cost remained unchanged. No significant changes between baseline and endline were observed for the controls.
Conclusions: After the intervention, the energy content of participants' experimental purchases was closer to their needs, suggesting that the workshops helped them plan and rationalize their food purchases better. The nutritional quality of the experimental purchases increased but energy cost did not, showing that the co-constructed Opticourses prevention program can favorably change food purchasing behaviors of socioeconomically disadvantaged individuals with no additional cost. This trial was registered at clinicaltrials.gov as NCT02383875.
Keywords: intervention, low-income, diet, nutritional quality, food purchasing behavior, experimental economics, cost, food prices
Introduction
The diets of the most socially disadvantaged individuals in industrialized countries are characterized by low intakes of fruit and vegetables and by poorer nutritional quality overall (1). This is partly explained by the high price-per-calorie ratio of fruits and vegetables compared with that of high-fat and high-sugar products (2, 3). Socially disadvantaged individuals perceive food prices as a barrier to adopting healthier diets (4, 5). It is especially important for these populations to develop strategies to achieve good nutritional quality with a small budget. An intervention targeting socially disadvantaged populations must take into account their actual beliefs and expectations. A co-construction approach is thus recommended, involving participants at each step of the intervention to maximize its impact (6, 7).
It is more difficult to have a balanced diet with a low food budget (8), and a minimal food budget (estimated at ∼3.5€ ⋅ d−1 ⋅ person−1 in France) is strictly needed to design diets that are both nutritious and socially acceptable (9, 10). When the food budget is low but above this critical threshold, designing a balanced diet involves favoring a selection of foods with good nutritional quality for their price (11). In addition, for a given food product, replacing national brands with generic products can lower cost without impairing nutritional quality. Previous studies show that branded products are 2–4 times more costly than generic products with equivalent nutritional contents (12, 13).
Experimental economics is a powerful method for evaluating the impact of a public policy. The principle of experimental economics is to bring participants revealing their real choices by using incentive-compatible mechanisms (14). In nutrition, experimental economics has been used for ex ante evaluations of policies such as taxes and subsidies or nutritional labeling systems (15–18).
Evaluating the impact of an intervention is a key step that must be rigorous, feasible, and controlled (19, 20). However, the methodology generally used to evaluate nutrition prevention interventions has limitations as a result of declarative and social desirability bias (21–23). To reduce such bias, this study implemented a framed field experiment (24) to evaluate the impact of the intervention on food purchasing behavior.
The Opticourses project is multifactorial, territorial, and participative. Opticourses was implemented in disadvantaged neighborhoods in Marseille, France, with the aim to improve the nutritional quality of food purchases in populations with budgetary constraints (25, 26). The project addressed both the supply side, through an in-store intervention (27), and the demand side, through a prevention program based on participatory workshops. By focusing on household food supply (a daily activity that most adults are familiar with and feel able to handle), the Opticourses program is engaging and pragmatic, in accordance with the principles of health promotion (28). In the present study, the objectives were to describe the co-construction of the Opticourses program with participants in deprived social situations and, based on experimental economics, to evaluate its impact on the nutritional quality and cost of household food purchases.
Methods
Population characteristics
Socioeconomically disadvantaged individuals were recruited from community centers (n = 9) and health and care centers (n = 2) whose staff showed interest in the intervention and motivation for involvement. All of the facilities were located in socioeconomically deprived districts of Marseille, France. Participants volunteered to take part in an intervention that included a set of five 2-h workshops on diet and budget. Inclusion criteria were as follows: voluntary consent to participate in the study, residence in a socioeconomically deprived district of Marseille (13th, 14th, or 15th district), involvement in household food purchases, and financial difficulties as assessed by social workers. All participants gave written informed consent to participate in the study. No institutional review board approval was required for this research, as stated by the French South-Mediterranean Ethical Research Committee (Comité de Protection des Personnes Sud-Méditerranée), which reviewed the Opticourses intervention protocol. This trial was registered at clinicaltrials.gov as NCT02383875.
Co-construction of the protocol and tools
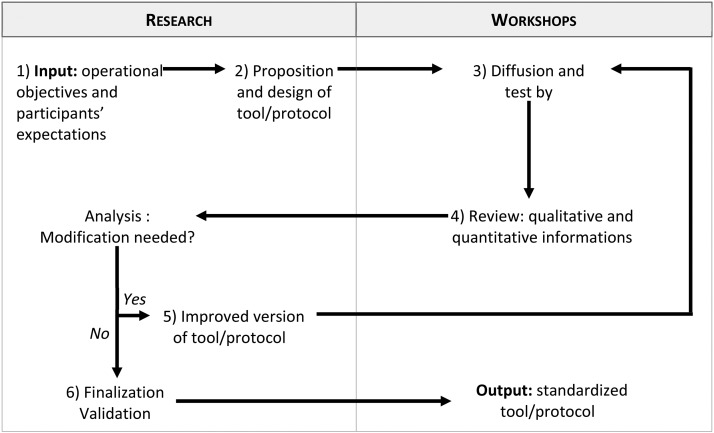
To maximize its effectiveness, the intervention was designed on the basis of the principles of co-construction and participative research. Participants were involved in the elaboration of the intervention, in order to implement a nonbinding, playful intervention tailored to the target population. This co-construction approach integrates the principles of health promotion (28) and social cognitive theory (29) and was applied to develop the protocol and the tools of the intervention and evaluation process. The intervention tools were developed through an iterative process as follows (Figure 1): 1) initial proposition of a tool by the research team, based on operational objectives, participants' expectations expressed in early workshops, estimated feasibility, and cost; 2) design of a first version by the research team; 3) testing of the first version by the participants during the workshops; 4) collection of both qualitative (understanding, participants' opinion, and time of use) and quantitative (test answers and consistency of results) information; 5) development of improved versions that were retested; and 6) validation and finalization. Different versions of the intervention protocol were also tested in the co-construction stage. The standardized tools and protocol were then used in the intervention stage.
FIGURE 1.
Principles of the co-construction approach.
Intervention
The Opticourses workshops aimed to guide participants toward household food purchases of good nutritional quality at no additional cost, building on better knowledge of food groups and nutritional quality of foods, awareness of foods combining good nutritional quality with a “fair price,” knowledge and know-how sharing among participants (discussions on “tips and tricks,” beliefs about food, recipes, etc.), collection of all of the household food supply over a month (26), and advice based on the analysis of actual participants' food purchase practices.
The standardized protocol resulting from the co-construction stage took the form of five 2-h workshops held every 2 wk, except for the last workshop (mainly dedicated to evaluation), which was held 1 mo after the fourth workshop. Workshops comprised group sessions (6–12 participants) organized in the community or health and care centers and were led by a professional (C Dubois, A Maidon, and MS Sangolo-Gaubard) in health promotion and nutrition and dietetics. An assistant (A Lesturgeon) took charge of data collection and helped conduct the workshops. The workshops were built on real food purchases, including participants' household purchase receipts that they collected over a month. Complete information on the Opticourses program content was provided during the first workshop, so that individuals who were not interested could decide whether to attend the subsequent workshops. Workshop participants engaged in several activities. For example, they discussed food purchase strategies and played a food group categorization game that shared information on characteristics of food groups. Participants also received information on the nutritional quality of foods by playing a game in which foods were classified into 4 nutritional quality classes based on the SAIN,LIM (score of nutritional adequacy of individual foods, limited nutrient score) nutrient profile system (30). An overview of the notion of nutritional quality for price (NQP) based on 2 tools: a list of foods with both good nutritional quality and a low price within each food group, and a “fair price booklet” tool (31), which included a list of foods with good nutritional quality and the price below which the product could be considered as relatively inexpensive. Participants analyzed real food purchases by playing a game in which they classified food expenditures by food groups. Finally, participants worked on their beliefs about food by playing a tasting game in which they blindly compared the taste of commonly consumed foods of equivalent nutritional quality but of different prices and brands. During the fourth workshop, the research team analyzed participants' monthly household food receipts and then provided individual feedback on the nutritional quality of participants' food purchases and the contribution of each food group to total food expenditure, and provided advice to participants on how to improve the nutritional quality of their food purchases at no additional cost.
Quantitative evaluation
Evaluating the impact of the intervention on knowledge.
Two tools were developed to evaluate the intervention's impact on participants' knowledge: the food group test and the NQP test. Participants took both tests voluntarily before and after the intervention. In the food group test, participants were asked to assign a color code (e.g., green for fruit and vegetables, blue for dairy products, etc.) to 14 food pictures. In the NQP test, 10 pairs of foods were presented to participants and each pair comprised foods that differed in their NQP. Each pair was composed of similar foods with a similar price but different nutritional content (e.g., whole-grain sliced bread at 1.75€/kg or white sliced bread at 1.73€/kg), foods belonging to the same food group with similar prices and different nutritional quality (e.g., canned chickpeas at 1.62€/kg or frozen fried potatoes at 1.64€/kg), foods with similar nutritional quality but different prices [e.g., 2 types of potato flakes at 3.90€/kg (national brand) or 1.78€/kg (discount version)], or 2 different foods (i.e., of different nutritional quality) that were consumed similarly during meals (e.g., sweet flan at 2.60€/kg or fruit compote at 2.75€/kg). Participants were instructed to pick the food in each pair that they would advise a friend to buy when the friend wants to balance his or her food purchases with a limited budget. For both tests, a global score was computed as the total points obtained from correct answers (wrong or nonresponses were ignored).
Evaluating the impact of the intervention on food purchasing behavior by using experimental economics.
A catalog of 300 food items (http://www.opticourses.fr/node/24) was specifically developed for this study, based on prices and pictures of foods collected a few months before the intervention from a supermarket located in the participants' neighborhood. Each page displayed pictures of the front of the food packages, unit prices (expressed in €), and prices per kilo, as done in supermarket advertising catalogs. Use of the same catalog ensured that participants were faced with the same supply and diversity of foods throughout the study. Foods were grouped in the catalog according to a retail-based categorization (22 categories; Supplemental Table 1). Participants then selected foods for the next 2 d for their household, based on food items featured in the catalog. This selection constituted a food purchase intent. Similar to their regular shopping, participants were free to choose the nature and amount of food they wanted to select. To avoid potential bias related to the declarative nature of these purchase intents, the task was made incentive compatible by informing participants that they could earn a 10€ coupon if their next food purchases in a real store reflected their purchase intent during the experiment. They were thus prompted to shop in the experiment as they would in a real food store. At the subsequent workshop, participants' shopping receipts for their real food purchases were compared with their experimental food purchases. To obtain the coupon, participants' shopping receipts had to feature ≥6 items corresponding to the experimental purchase intents. This incentive aimed to assess true changes in food purchasing behaviors by limiting the effects of social desirability (i.e., when participants direct their choices to please or impress the workshop facilitator). Workshop participants (intervention group) took part in 2 experimental sessions (at the first and last workshops), and changes in their experimental purchases were compared between baseline and endline. In addition, to assess whether having already performed the test affects the experimental purchases of the subsequent session, a control group composed of 23 participants who were recruited in the same community centers but did not participate in the workshops also took part in 2 experimental sessions of food purchase intents at 3-wk intervals (baseline and endline), based on the same instructions and protocol as workshop participants (i.e., using the catalog and incentive with coupon).
Our hypothesis was that workshops could help improve the balance of food purchases (and consequently, their nutrient content), with no additional cost. Thus, the nutritional characteristics of the experimental purchases were assessed at both the food group and nutrient levels. For that purpose, each food in the catalog was associated with a nutritional composition for 100 g of food as consumed based on the French Centre d'Information sur la Qualité des Aliments database (https://pro.anses.fr/tableciqual/index.htm), which lists the nutritional composition and edible portion of French food products. Total weight (expressed in g ⋅ d−1 ⋅ person−1) and total energy content (expressed in kcal ⋅ d−1 ⋅ person−1) were estimated for each experimental purchase by summing the weight (as consumed) and energy content of all of the foods and drinks selected and dividing it by the number of household members and days for which purchases were planned. In addition to the classification into 22 categories relevant to the retail environment, as mentioned previously, all foods in the catalog were classified into the following 8 groups derived from the French National Nutrition and Health Program: 1) starch, 2) fruits and vegetables, 3) meat, fish, and eggs, 4) dairy products, 5) fats, 6) foods high in fat, salt, and sugar (HFSSs), 7) mixed dishes, and 8) juices and soft drinks (32). The contribution of these 8 food groups to total food purchases was estimated in weight and energy. Water was excluded from all analyses because participants consumed mainly tap water.
We used the mean adequacy ratio and the solid energy density (SED) to assess the nutritional quality of the experimental food purchases, as previously described by Vieux et al. (33). In addition, 3 nutrients to be limited were also assessed (namely sodium, SFAs, and free sugars). The nutritional quality assessment methodology is fully described in the Supplemental Methods and Supplemental Table 2.
Based on experimental food purchases selected by the participants and food prices from the catalog, we estimated the total expenditure (expressed in € ⋅ d−1 ⋅ person−1) and energy cost (expressed in €/2000 kcal) for each experimental food purchase.
Qualitative evaluation
How participants perceived the impact of the workshops on their food purchases was assessed by a qualitative evaluation. An external evaluator conducted individual semidirected interviews and one group interview 1 mo after the intervention, using an interview grid that included questions about the modification of food purchases. These interviews were proposed to participants coming from the different community or health centers, yielding a subsample of 19 interviews. Interviews were recorded using field notes and were transcribed. Interview transcripts were analyzed using conventional content analysis (34) and categorized thematically.
Statistical analysis
Descriptive and statistical analyses were performed using SAS software (version 9.4; SAS Institute). Sociodemographic characteristics were compared between workshop participants who performed the experimental economics quantitative evaluation (evaluated intervention group) and those who did not (nonevaluated intervention group) and between the intervention and control groups using the nonparametric chi-square test for qualitative variables and the Mann-Whitney test for continuous variables. Within the evaluated intervention group, the food group test scores, NQP test scores, and nutritional characteristics and food composition of the experimental purchases were compared between baseline and endline (i.e., before and after the intervention) using a paired t test and a generalized linear mixed model for repeated measures (with a compound symmetry covariance matrix) adjusted for age, sex, financial situation, number of individuals in the household, and number of children. Within the control group, the nutritional characteristics and food composition of experimental food purchases were compared between the first and second sessions of experimental food purchases (i.e., baseline and endline) using paired t tests and a generalized linear mixed model for repeated measures adjusted for age, sex, financial situation, and number of individuals. Effect sizes (d) for dependent groups (35) were computed for significant variables. Significance was set at 5% (P < 0.05) for all tests.
Results
Population characteristics
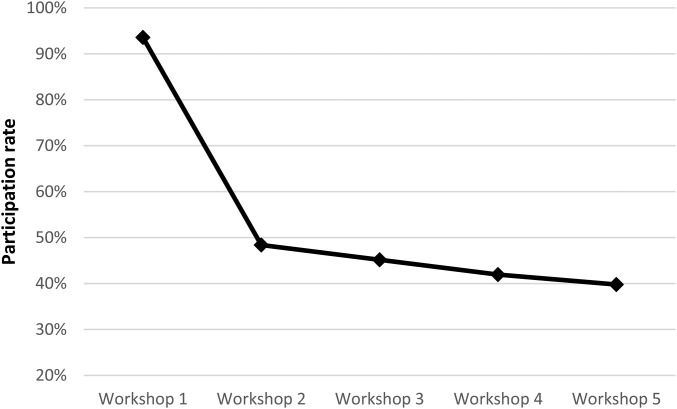
In all, 96 individuals (9 groups, 8 centers) participated in the co-construction stage (from September 2012 to April 2013), and 93 people (14 groups, 7 centers) then took part in the intervention stage. The site 1 intervention started in April 2013 and the site 7 intervention ended in June 2014. Thirty-five people took part in the evaluation of knowledge and in the food purchase experiment (i.e., 38% of the intervention participants); 23 other individuals (3 sites) also took part in the food purchase experiments but did not participate in the workshops (control group) (Supplemental Figure 1). Sociodemographic characteristics were not significantly different between the workshop participants who completed the evaluation and those who did not (Table 1). Evaluated workshop participants were mainly women (77%; mean age: 51 y; mean number of household members: 3.1 including 1.3 children); 44% declared severe financial difficulties (Table 1). Sociodemographic characteristics were not significantly different between evaluated workshop participants and the control group, except for age, which was significantly lower in the control group (45.4 compared with 50.9 y; P = 0.038) (Table 1). Participation rates in the 5 workshops varied (Figure 2): 94% of intervention participants attended the first workshop, and the participation rate then remained relatively stable (40–48%) over the other 4 workshops.
TABLE 1.
Population characteristics1
| Intervention (n = 93) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Co-construction (n = 96) | Evaluated (n = 35) | Nonevaluated (n = 58) | Control (n = 23) | |||||||
| Characteristic | Value | n | Value | n | Value | n | P 2 | Value | n | P 3 |
| Age, y | 48.4 ± 7.7 | 67 | 50.9 ± 11.2 | 34 | 47.0 ± 13.0 | 27 | 0.094 | 45.4 ± 9.6 | 23 | 0.038 |
| Total in household, n | 3.7 ± 2.0 | 62 | 3.1 ± 1.8 | 35 | 2.3 ± 1.4 | 25 | 0.080 | 3.3 ± 1.6 | 23 | 0.186 |
| Children, n | 2.0 ± 1.7 | 59 | 1.3 ± 1.5 | 35 | 1.2 ± 1.4 | 22 | 0.941 | 1.6 ± 1.3 | 23 | 0.135 |
| Women | 80.0 | 96 | 77.1 | 35 | 70.7 | 58 | 0.496 | 91.3 | 23 | 0.163 |
| Financial situation | 48 | 34 | 17 | 23 | ||||||
| Stable | 12.5 | 11.8 | 17.7 | 0.770 | 13.0 | 0.932 | ||||
| Precarious | 52.1 | 44.1 | 47.1 | 47.8 | ||||||
| Severe difficulties | 35.4 | 44.1 | 35.3 | 39.1 | ||||||
Values are means ± SDs or percentages unless otherwise indicated.
P values were determined from a chi-square test of homogeneity for qualitative variables and a Mann-Whitney test for continuous variables to test differences between participants who did and did not complete the evaluation.
P values were determined from a chi-square test of homogeneity for qualitative variables and Mann-Whitney test for continuous variables to test difference between evaluated intervention participants and controls.
FIGURE 2.
Participation rate at each workshop during the intervention stage (n = 93).
Impact on knowledge
Food group test scores were significantly higher after the participative workshops than those obtained before the intervention (13.2 ± 1.8 and 12.1 ± 1.9 respectively; P < 0.01). NQP test scores were not significantly different before and after the intervention (6.6 ± 1.4 and 6.9 ± 1.6, respectively; P = 0.30).
Impact on food purchasing behavior: experimental economics evaluation
Table 2 shows the nutritional characteristics and cost of experimental food purchases of workshop participants before and after the intervention. The energy content of the experimental food purchases significantly decreased by 38% after the participative workshops (5114 compared with 3385 kcal ⋅ d−1 ⋅ person−1; crude and adjusted P < 0.01), as did food expenditures (9.73 compared with 7.22€ ⋅ d−1 ⋅ person−1; crude and adjusted P < 0.01). However, energy cost remained unchanged. The SED decreased from 128 kcal/100 g to 119 kcal/100 g after the intervention (crude P < 0.04; i.e., a reduction of 7.6%), but the significance was lost after adjustment. The mean adequacy ratio did not change significantly. The energy contribution of free sugars decreased significantly from 8.5% to 5.8% (crude and adjusted P < 0.01), whereas that of SFA and sodium content expressed for 2000 kcal remained similar. The contribution of food groups to the total energy of the experimental purchases was significantly different at baseline and endline (Table 2). The percentage of energy from the HFSS group was halved (from 11.0% to 5.5%; crude and adjusted P < 0.01). In parallel, a decrease occurred in the energy contribution from fruit and vegetables (from 10.1% to 13.6% of total energy; crude P = 0.03) and from meat, fish, and eggs (from 15.8% to 21.1% of total energy; crude P = 0.02), but the statistical significance of those changes was lost after adjustment (adjusted P = 0.06 for both food groups). Based on the classification proposed by Cohen (36), the calculated effect sizes were medium for energy content (d = 0.5) and energy contributions from proteins (d = 0.6), free sugars (d = 0.5), HFSSs (d = 0.5), and meat, fish, and eggs (d = 0.5). Effect sizes were small for food expenditure (d = 0.4), SED (d = 0.3), and energy contribution from fruits and vegetables (d = 0.4) (Table 2).
TABLE 2.
Nutritional and cost characteristics of experimental food purchases of workshop participants (n = 35) before (baseline) and after (endline) the intervention1
| Characteristic | Baseline | Endline | P 2 | Adjusted P3 | Effect size4 |
|---|---|---|---|---|---|
| Energy, kcal ⋅ d−1 ⋅ person−1 | 5114 ± 3883 | 3385 ± 2374 | <0.01 | <0.01 | 0.5 |
| Expenditure, € ⋅ d−1 ⋅ person−1 | 9.73 ± 7.10 | 7.22 ± 4.78 | <0.01 | <0.01 | 0.4 |
| Energy cost, €/2000 kcal | 3.03 ± 1.45 | 3.44 ± 2.00 | 0.30 | 0.36 | |
| Solid energy density, kcal/100 g | 128.4 ± 25.5 | 118.7 ± 30.1 | 0.04 | 0.10 | 0.3 |
| Mean adequacy ratio, % adequacy/2000 kcal | 81.3 ± 8.5 | 82.1 ± 7.4 | 0.56 | 0.42 | |
| Proteins, % of total energy | 18.7 ± 4.3 | 21.5 ± 5.6 | <0.01 | 0.02 | 0.6 |
| Carbohydrates, % of total energy | 52.7 ± 9.7 | 49.7 ± 10.7 | 0.11 | 0.08 | |
| Free sugars, % of total energy | 8.5 ± 6.0 | 5.8 ± 6.1 | <0.01 | <0.01 | 0.5 |
| Fats, % of total energy | 25.5 ± 7.1 | 25.4 ± 8.1 | 0.94 | 0.65 | |
| SFAs, % of total energy | 10.7 ± 3.9 | 10.6 ± 4.2 | 0.95 | 0.72 | |
| Sodium, mg/2000 kcal | 2038 ± 430 | 2182 ± 754 | 0.20 | 0.13 | |
| Food group, % of total energy | |||||
| Fruits and vegetables | 10.1 ± 5.8 | 13.6 ± 10.0 | 0.03 | 0.06 | 0.4 |
| Starch | 43.4 ± 19.7 | 40.8 ± 19.0 | 0.44 | 0.47 | |
| Meat, fish, and eggs | 15.8 ± 9.1 | 20.1 ± 9.6 | 0.02 | 0.06 | 0.5 |
| Mixed dishes | 1.9 ± 3.3 | 2.6 ± 4.8 | 0.29 | 0.13 | |
| Dairy products | 12.3 ± 7.7 | 13.2 ± 9.2 | 0.56 | 0.43 | |
| Foods high in fat, sugar, and salt | 11.0 ± 12.0 | 5.5 ± 11.0 | <0.01 | 0.01 | 0.5 |
| Drinks | 3.9 ± 3.8 | 2.9 ± 4.1 | 0.11 | 0.15 | |
| Fats | 1.6 ± 2.3 | 1.3 ± 2.5 | 0.55 | 0.63 |
Values are means ± SDs or percentages.
P values were determined from a paired t test.
Adjusted P values were determined from a mixed model adjusted for age, sex, financial situation, number in household, and number of children.
Calculation of the effect size (Cohen's d) for dependent samples was described elsewhere (35).
In the control group, none of the characteristics of experimental food purchases were significantly different between the 2 sessions (all P > 0.05; Table 3). In particular, the mean energy content was 4523 and 4711 kcal ⋅ d−1 ⋅ person−1 at baseline and endline, respectively (P = 0.71).
TABLE 3.
Nutritional and cost characteristics of experimental food purchases of the control group (n = 23) during the first session (baseline) and the second session (endline)1
| Characteristic | Baseline | Endline | P value2 | Adjusted P value3 |
| Energy, kcal ⋅ d−1 ⋅ person−1 | 4523 ± 2924 | 4711 ± 2747 | 0.71 | 0.63 |
| Expenditure, € ⋅ d−1 ⋅ person−1 | 8.75 ± 5.13 | 8.84 ± 4.43 | 0.90 | 0.94 |
| Energy cost, €/2000 kcal | 3.17 ± 1.38 | 3.06 ± 1.36 | 0.77 | 0.71 |
| Solid energy density, kcal/100 g | 136.8 ± 23.9 | 136.3 ± 20.3 | 0.91 | 0.90 |
| Mean adequacy ratio, % adequacy/2000 kcal | 80.2 ± 7.2 | 80.9 ± 6.2 | 0.56 | 0.77 |
| Proteins, % energy | 17.1 ± 4.8 | 17.5 ± 3.2 | 0.61 | 0.91 |
| Carbohydrates, % energy | 49.9 ± 8.0 | 50.6 ± 7.4 | 0.74 | 0.56 |
| Fats, % energy | 30.2 ± 5.8 | 29.2 ± 5.9 | 0.55 | 0.61 |
| Free sugars, % energy | 11.4 ± 4.5 | 11.7 ± 5.1 | 0.79 | 0.74 |
| SFAs, % energy | 13.6 ± 3.6 | 12.9 ± 2.9 | 0.43 | 0.79 |
| Sodium, mg/2000 kcal | 1976 ± 460 | 1887 ± 310 | 0.23 | 0.55 |
| Food group, % of total energy | ||||
| Fruits and vegetables | 8.7 ± 6.0 | 8.0 ± 5.3 | 0.39 | 0.39 |
| Starch | 34.3 ± 10.4 | 35.2 ± 13.5 | 0.82 | 0.82 |
| Meat, fish, and eggs | 11.4 ± 7.7 | 12.2 ± 7.2 | 0.51 | 0.51 |
| Mixed dishes | 3.3 ± 3.5 | 3.4 ± 3.0 | 0.93 | 0.93 |
| Dairy products | 15.3 ± 5.1 | 16.3 ± 5.0 | 0.52 | 0.52 |
| Foods high in fat, sugar, and salt | 18.4 ± 8.7 | 17.0 ± 11.2 | 0.56 | 0.56 |
| Drinks | 5.7 ± 3.1 | 5.6 ± 3.6 | 0.79 | 0.79 |
| Fats | 2.9 ± 2.5 | 2.4 ± 2.4 | 0.44 | 0.44 |
Values are means ± SDs or percentages.
P values were determined from a paired t test.
Adjusted P values were determined from a mixed model adjusted for age, sex, financial situation, number in household, and number of children.
Qualitative evaluation
Analysis of participants' declarations highlighted their improved knowledge about the nutritional quality of foods (e.g., the difference in nutritional quality between potatoes and vegetables, and between sweet dairy desserts and yogurts) and their awareness of the share of their food budget allocated to the different food groups. Of the 19 participants interviewed 1 mo after the intervention, 15 gave concrete examples indicating how they had modified their food purchasing behavior. The analysis of participants' declarations identified 3 types of modification: changes in the type of foods purchased, changes in purchasing attitudes and strategies, and changes in culinary practices. Among changes in the type of foods purchased, soft drinks were the most frequently cited: 1 person in 3 declared that he or she had reduced or even stopped purchases of sodas or replaced purchases of fruit “nectars” (i.e., sugared fruit juices) with fruit juices. Other modifications of foods purchased were expressed in terms of quantity (e.g., increased purchases of legumes or fruits and vegetables) and quality (e.g., substitution of white bread with whole-grain bread). The changes in purchasing attitudes and strategies included more attention paid to labeled information (product composition and price per kilo), changes or diversification of purchasing points, improved opinion of cheaper brand products, retrieval and purchases of these products, and better control of the food budget. Changes in culinary practices included cooking at home or cooking differently (e.g., less fat, more vegetables). The following synthesis of transcripts illustrates the different modifications to food purchasing behaviors:
51-y-old woman: Now, after shopping for food, I still keep the receipts. They help me check if I've managed my budget well. I look at the price per kilo of foods and don't get confused with orange juices anymore (sugar and fruit). I've bought canned fish, and several times I've prepared some lovely dishes with raw vegetables and sardines. When I'm cooking starches, I add some fresh vegetables. I shared the tips and tricks with my friends who by the way have noticed that I've changed the way I cook.
46-y-old woman: I buy too much fat, I've cut back a bit. I buy more fruit and vegetables, it doesn't get too expensive for me, I do my shopping at Noailles [very popular market in the center of the town]. I already used to, but I wasn't buying much fruit and legumes. I also buy more legumes (red beans and lentils). I used to shop at Dia or Simply markets and now I go to Carrefour, the other participants told me it's less expensive and it's true. I pay more attention to labels and especially the price per kilo.
51-y-old woman: I buy cheaper brand products, before I never did because I thought they were poorer quality. I know how to tell the real juices from the ones with only sugar: I buy the real ones and I don't buy sodas anymore. I buy whole-grain bread instead of white bread. For minced meat, I look and I take no more than 12% fat, 5% I can't, it's too expensive. I've changed many things, I spend 330€ (per month) instead of 360€ before, so it's a bit cheaper and I'm purchasing better things. I use more different oils, I like canola oil, I blend them. I also try to add less salt. I used to buy a lot of sweet products. I buy a bit more fish, beef and chicken and less pork. I diversify shops a bit (Aldi, Leader Price) but I don't have a car, it's not easy.
Participants were able to analyze their own food purchases and identify ways to improve them, as supported by several transcripts:
Group interview: I realized the burden of sweet products in my food budget.
59-y-old woman: For me it's easy since I save money and it's a true motivation.
Group interview: Now I look at what I purchase, I used not to necessarily.
42-y-old woman: I look differently when I do my shopping.
53-y-old woman: I look at labels more carefully, especially the price per kilo.
Discussion
This study shows that co-constructed participative workshops based on recreational and entertaining activities around food purchase practices and nutritional quality and price of foods can favorably change the food purchasing behaviors of individuals in deprived social situations without significantly increasing their food expenditure. Interviews revealed 3 types of change in purchasing behaviors: changes in the type of foods purchased, changes in purchasing attitudes and strategies (attention paid to label information, purchasing points, and opinion on cheaper brand products), and changes in culinary practices. Quantitative evaluation of the intervention was performed on food purchase intents using experimental economics to limit social desirability bias. Unlike controls, workshop participants decreased the total energy of their experimental food purchases (toward more realistic energy levels), suggesting a better ability to assess the needs of their households for 2 d and adapt purchases accordingly. The evaluation also showed that the intervention improved food purchasing behaviors, as indicated by the decreased energy contribution from free sugars and from products high in fat, salt, and sugar and the nearly significantly increased energy contribution from fruit and vegetables (adjusted P = 0.06) at the endline in the intervention group only, and at no additional cost.
Similar reductions in the total number of calories purchased were previously observed in low-income families in the United States who received home-based nutrition education sessions (37). To our knowledge, most individual-directed interventions to promote healthy eating are based on activities around food consumption or cooking skills (38–40). Yet changing food consumption behavior implies changing food purchasing behavior. One strength of our study was the use of food purchases and prices as an entry point to address the question of a healthy diet with individuals in deprived social situations. Implementing workshops on food purchases (a major daily, tangible concern for this population), rather than on food intake, can induce stronger motivation among participants, which is a success factor for interventions in health education (6).
Many population-directed policies designed to improve the nutritional quality of food purchases rely on enhancing access to information (41). The underlying assumption is that people act rationally when making food choices. In economic terms, rationality means that consumers maximize their lifetime happiness when they allocate their scarce resources of time and money (42). Nonetheless, various studies have shown that the provision of nutritional information has moderate effects (41, 43–46). The main reason may be that consumers do not behave as homo economicus or “economic man,” i.e., a rational and self-interested agent who seek optimal, utility-maximizing outcomes (47). For instance, consumers have a limited capacity to process information and may even be distracted when provided with additional information (48). In that respect, the Opticourses workshops focused on tacit knowledge (know-how) rather than explicit knowledge (know-what). By sharing tips and tricks on food purchasing (fair price booklet, real purchase analyses), the intervention provided participants practical knowledge on how to build healthy diets. By doing so, the Opticourses workshops provide participants with the necessary tools for fast and frugal food decision making, allowing the construction of healthier diets despite bounded rationality (49).
Different reports and studies explored the levers for effective interventions on diet, particularly for socioeconomically disadvantaged populations (6, 7, 20, 38–40, 50, 51). A WHO report assessing the evidence on effective interventions on diet and physical activity (7) underlined that multicomponent interventions adapted to the local context and involving participants in the planning and implementation stages were found to be the most successful. Co-construction was a key component of the present study to engage participants, with specific attention given to the format of the intervention to make it playful with multiple, diversified activities and reachable goals. Empowerment is known to be a success factor in nutrition health promotion (50). This is particularly true for vulnerable populations, who are more prone to low self-esteem (20). The present workshops enabled participants to appropriate tools and knowledge to act favorably on their purchases, thus enhancing autoefficacy and self-esteem. Moreover, conducting the intervention in the form of group workshops has been identified as a key lever to improve the effectiveness of interventions promoting nutrition and physical activity among socioeconomically disadvantaged populations (51).
Interventions promoting healthy eating are generally evaluated through self-reported and thus potentially biased dietary intakes or behaviors (40, 52). The experimental economics approach has been used in public health and nutrition to assess food taxes (15) and labeling policies (17). To our knowledge, the present study is the first to implement this approach in an innovative way to evaluate the impact of a nutritional intervention in a real-world setting. Experimental economics limits social desirability bias and thus reveals true consumer preferences by using incentive mechanisms (53). In addition, placing participants in controlled conditions (as close as possible to those of the real world) ensured that the observed changes in purchasing behavior were not influenced by modifications in the purchasing environment (diversity and price of food supply, purchasing points, etc.). In addition, the conditions for implementing the evaluation method were tailored for a target population with potentially low literacy skills. Whereas questionnaires could be perceived as demanding, normative, and difficult to fill out, the food catalog and instructions given placed participants in a comfortable day-to-day activity that preserved their self-esteem. The main strength of this study is that it improved food purchasing behaviors despite the limited room for maneuvering in terms of economical means. Participants had a low budget for food, previously estimated at 3.65€ ⋅ d−1 ⋅ person−1 (26), which is very close to the lowest cost at which a nutritionally adequate diet can be achieved (∼3.5€ ⋅ d−1 ⋅ person−1) as estimated by Darmon et al. (9) and very close to the cost of 2000 kcal of experimental food purchases in the present study. The beneficial changes in food purchasing behaviors could be explained by the anticipation and rationalization of food purchasing, highlighted by the decrease in the total energy of experimental food purchases after the intervention. Workshop participants may have realized the importance of the act of purchase and of purchasing foods rationally rather than automatically or routinely.
The present study has limitations. In the intervention stage, the attrition rate was ∼50% after the first workshop. This was expected, because recruitment is known to be difficult in low-income populations (20, 54). The high attrition rate may reflect a sensible economic decision about the time:benefit ratio of attending the workshops (42). However, the participation rate in the subsequent workshops (once the participants understood and agreed with the format and contents of the intervention) remained stable, which highlights the importance of providing complete information and engaging people during the first workshop. Another limitation is that the quantitative evaluation was only performed by a subsample of intervention participants, was not randomized, and did not assess the long-term effect of the intervention. However, the participants who carried out the quantitative evaluation (n = 35) were not significantly different in terms of sociodemographic characteristics from those who did not (n = 58), the specificity of the observed changes was tested with a control group (n = 23), and the sample sizes were sufficient to highlight significant differences between the control and intervention groups. In addition, the endline experimental food purchases of the control group were assessed after a shorter interval of time (3 wk) than the intervention group (10 wk). This may have introduced a bias in the design but allowed us to limit the attrition rate that might have been higher in the control after 10 wk. In addition, the evaluation tools were new and not quantitatively validated, but face validity was assessed by researchers and participants who evaluated whether the items were relevant to assess the measured concept, and acceptability and feasibility were tested with the co-construction group. Finally, the effect size was medium or small. However, moderate effects were expected, because it is unlikely that an intervention on its own induces radical shifts in food purchasing behaviors. These moderate effects can support the idea that social desirability bias was limited and that participants revealed true choices.
This study shows that co-constructed participative workshops, based on actual food purchase practices, can guide individuals in deprived social situations toward household food purchases of better nutritional quality without increasing their food expenditure. This study also shows the relevance and feasibility of using experimental economics to evaluate the impact of a public health nutrition intervention conducted in a real-world setting on food purchasing behavior. The “game-like” aspect of the experimental economics approach enables participants to deliver unbiased evaluations while preserving their self-esteem.
Supplementary Material
Acknowledgments
We thank Célia Chischportich (expert in qualitative evaluation, Regards Santé), Gérard Coruble (expert in interventional research and public health, Regional Health Agency Provence Alpes Côte d'Azur Region), Flavie Ferrari (graphic designer, Maison des artistes), Valerie Leblanc (graphic designer, Maison des artistes), Audrey Lesturgeon [assistant, ‘Nutrition Obésité et Risque Thrombotique’ (NORT) research unit], Audrey Maidon (dietician, NORT research unit), Anne Meyer-Dutour (professor, NORT research unit), Jean de Pena (website designer, Maison des artistes), Malu-Séverine Sangolo-Gaubard (dietician, NORT research unit), Amir Rezzoug (conception and realization of the purchase catalogue, Maison des artistes), Maelle Robert (intership student, NORT research unit), and Joséphine Rohaut (internship student, NORT research unit). The authors' responsibilities were as follows—ND, CD, and HG: designed and conducted the intervention; MP, CD, and ND: interpreted the data and drafted the manuscript; MM and RG: analyzed the data; LM and BR: designed the experimental economic assessment and were involved in the interpretation of the results; and all authors: critically reviewed and read and approved the final manuscript.
Abbreviations
- HFSS
food high in fat, salt, and sugar
- NQP
nutritional quality for price
- SED
solid energy density
Footnotes
Supported by the Regional Health Agency in the Provence Alpes Côte d'Azur Region and the French National Cancer Institute. The funding bodies had no role in the protocol design, analysis or interpretation of the data, writing of the manuscript, or the decision to submit the manuscript for publication.
References
- 1. Darmon N, Drewnowski A.. Does social class predict diet quality? Am J Clin Nutr 2008;87:1107–17. [DOI] [PubMed] [Google Scholar]
- 2. Drewnowski A, Darmon N.. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82(1 Suppl):265S–73S. [DOI] [PubMed] [Google Scholar]
- 3. Maillot M, Darmon N, Darmon M, Lafay L, Drewnowski A.. Nutrient-dense food groups have high energy costs: an econometric approach to nutrient profiling. J Nutr 2007;137:1815–20. [DOI] [PubMed] [Google Scholar]
- 4. Beydoun MA, Wang Y.. How do socio-economic status, perceived economic barriers and nutritional benefits affect quality of dietary intake among US adults? Eur J Clin Nutr 2008;62:303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Waterlander WE, de Mul A, Schuit AJ, Seidell JC, Steenhuis IH.. Perceptions on the use of pricing strategies to stimulate healthy eating among residents of deprived neighbourhoods: a focus group study. Int J Behav Nutr Phys Act 2010;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Peters L, Molleman G, Hommels L, Ploeg M, Hosman C, Jané-Llopis E.. Outil de pilotage et d'analyse de l'efficacité attendue des interventions en promotion de la santé [A tool for steering and analyzing the expected effectiveness of health promotion interventions.]. Preffi 2.0. Guide explicatifs, les fondements de Preffi Woerden (Netherlands): Institut pour la Promotion de la Santé et pour la Prévention des Maladies (NIGZ); 2003. (in French). [Google Scholar]
- 7. World Health Organization Interventions on diet and physical activity: what works? Summary report. Geneva (Switzerland): World Health Organization; 2009. p. 1–48. [PubMed] [Google Scholar]
- 8. Darmon N, Drewnowski A.. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev 2015;73:643–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Darmon N, Ferguson EL, Briend A.. Impact of a cost constraint on nutritionally adequate food choices for French women: an analysis by linear programming. J Nutr Educ Behav 2006;38:82–90. [DOI] [PubMed] [Google Scholar]
- 10. Maillot M, Darmon N, Drewnowski A.. Are the lowest-cost healthful food plans culturally and socially acceptable? Public Health Nutr 2010;13:1178–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Maillot M, Ferguson EL, Drewnowski A, Darmon N.. Nutrient profiling can help identify foods of good nutritional quality for their price: a validation study with linear programming. J Nutr 2008;138:1107–13. [DOI] [PubMed] [Google Scholar]
- 12. Cooper S, Nelson M.. “Economy” line foods from four supermarkets and brand name equivalents: a comparison of their nutrient contents and costs. J Hum Nutr Diet 2003;16:339–47. [DOI] [PubMed] [Google Scholar]
- 13. Darmon N, Caillavet F, Joly C, Maillot M, Drewnowski A.. Low-cost foods: how do they compare with their brand name equivalents? A French study. Public Health Nutr 2009;12:808–15. [DOI] [PubMed] [Google Scholar]
- 14. Harrison GW.. Making choice studies incentive compatible. Kanninen BJ. editor. Valuing environmental amenities using stated choice studies Dordrecht (Netherlands: ): Springer; 2006. p. 67–110. [Google Scholar]
- 15. Darmon N, Lacroix A, Muller L, Ruffieux B.. Food price policies improve diet quality while increasing socioeconomic inequalities in nutrition. Int J Behav Nutr Phys Act 2014;11:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Crosetto P, Muller L, Ruffieux B.. Helping consumers with a front-of-pack label: numbers or colors? J Econ Psychol 2016;55:30–50. [Google Scholar]
- 17. Muller L, Ruffieux B.. Modification des achats en réponse à l'apposition de différents logos d'évaluation nutritionnelle sur la face avant des emballages. Cah Nutr Diététique 2012;47:171–82. [Google Scholar]
- 18. Crosetto P, Muller L, Ruffieux B.. Réponses des consommateurs à trois systèmes d'étiquetage nutritionnel face avant. Cah Nutr Diététique 2016;51:124–31. [Google Scholar]
- 19. Cambon L, Minary L, Ridde V, Alla F.. Transferability of interventions in health education: a review. BMC Public Health 2012;12:497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. French National Institute of Health and Medical Research [Social inequalities in health in relation to diet and physical activity.]. Paris: 2014; 731 p. [Google Scholar]
- 21. Fisher RJ.. Social desirability bias and the validity of indirect questioning. J Consum Res 1993;20:303–15. [Google Scholar]
- 22. Hebert JR, Clemow L, Pbert L, Ockene IS, Ockene JK.. Social desirability bias in dietary self-report may compromise the validity of dietary intake measures. Int J Epidemiol 1995;24:389–98. [DOI] [PubMed] [Google Scholar]
- 23. Norwood FB, Lusk JL.. Social desirability bias in real, hypothetical, and inferred valuation experiments. Am J Agric Econ 2011;93:528–34. [Google Scholar]
- 24. Harrison GW, List JA.. Field experiments. J Econ Lit 2004;42:1009–55. [Google Scholar]
- 25. Darmon N, Gaigi H, Dubois C. Opticourses [Internet]. [cited 2016 Jul 11]. Available from: http://www.opticourses.fr/.
- 26. Marty L, Dubois C, Gaubard MS, Maidon A, Lesturgeon A, Gaigi H, Darmon N.. Higher nutritional quality at no additional cost among low-income households: insights from food purchases of “positive deviants.” Am J Clin Nutr 2015;102:190–8. [DOI] [PubMed] [Google Scholar]
- 27. Gamburzew A, Darcel N, Gazan R, Dubois C, Maillot M, Tomé D, Raffin S, Darmon N.. In-store marketing of inexpensive foods with good nutritional quality in disadvantaged neighborhoods: increased awareness, understanding, and purchasing. Int J Behav Nutr Phys Act 2016;13:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. WHO, Health and Welfare Canada, and Canadian Public Health Association Ottawa Charter for Health Promotion: An international conference on health promotion—the move towards a new public health, Nov. 17–21 1986, Ottawa. Geneva (Switzerland): WHO; 1986.
- 29. Bandura A.. Health promotion by social cognitive means. Health Educ Behav 2004;31:143–64. [DOI] [PubMed] [Google Scholar]
- 30. Darmon N, Vieux F, Maillot M, Volatier J-L, Martin A.. Nutrient profiles discriminate between foods according to their contribution to nutritionally adequate diets: a validation study using linear programming and the SAIN,LIM system. Am J Clin Nutr 2009;89:1227–36. [DOI] [PubMed] [Google Scholar]
- 31. Dubois C, Gaubard MS, Darmon N.. Identification des aliments de bon rapport qualité nutritionnelle/prix pour le projet de recherche interventionnelle OPTICOURSES. Inf Diététique 2015;2:21–33. [Google Scholar]
- 32. Hercberg S, Chat-Yung S, Chauliac M.. The French National Nutrition and Health Program: 2001-2006-2010. Int J Public Health 2008;53:68–77. [DOI] [PubMed] [Google Scholar]
- 33. Vieux F, Soler L-G, Touazi D, Darmon N.. High nutritional quality is not associated with low greenhouse gas emissions in self-selected diets of French adults. Am J Clin Nutr 2013;97:569–83. [DOI] [PubMed] [Google Scholar]
- 34. Hsieh H-F, Shannon SE.. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
- 35. Dunlap WP, Cortina JM, Vaslow JB, Burke MJ.. Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Methods 1996;1:170–7. [Google Scholar]
- 36. Cohen J.. Statistical power analysis for the behavioral sciences. Mahwah (NJ): Lawrence Erlbaum Associates; 1988. p. 567. [Google Scholar]
- 37. Cortés DE, Millán-ferro A, Schneider K, Vega RR, Caballero AE.. Food purchasing selection among low-income, Spanish-speaking Latinos. Am J Prev Med 2013;44:S267–73. [DOI] [PubMed] [Google Scholar]
- 38. McGill R, Anwar E, Orton L, Bromley H, Lloyd-Williams F, O'Flaherty M, Taylor-Robinson D, Guzman-Castillo M, Gillespie D, Moreira P, et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 2015;15:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Oldroyd J, Burns C, Lucas P, Haikerwal A, Waters E.. The effectiveness of nutrition interventions on dietary outcomes by relative social disadvantage: a systematic review. J Epidemiol Community Health 2008;62:573–9. [DOI] [PubMed] [Google Scholar]
- 40. Reicks M, Trofholz AC, Stang JS, Laska MN.. Impact of cooking and home food preparation interventions among adults: outcomes and implications for future programs. J Nutr Educ Behav 2014;46:259–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Downs JS, Loewenstein G, Wisdom J.. Strategies for promoting healthier food choices. Am Econ Rev 2009;99:159–64. [DOI] [PubMed] [Google Scholar]
- 42. Cawley J.. An economic framework for understanding physical activity and eating behaviors. Am J Prev Med 2004;27:117–25. [DOI] [PubMed] [Google Scholar]
- 43. Bassett MT, Dumanovsky T, Huang C, Silver LD, Young C, Nonas C, Matte TD, Chideya S, Frieden TR.. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health 2008;98:1457–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Burton S, Creyer EH, Kees J, Huggins K.. Attacking the obesity epidemic: the potential health benefits of providing nutrition information in restaurants. Am J Public Health 2006;96:1669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Finkelstein EA, Strombotne KL, Chan NL, Krieger J.. Mandatory menu labeling in one fast-food chain in King County, Washington. Am J Prev Med 2011;40:122–7. [DOI] [PubMed] [Google Scholar]
- 46. Harnack LJ, French SA, Oakes JM, Story MT, Jeffery RW, Rydell SA.. Effects of calorie labeling and value size pricing on fast food meal choices: results from an experimental trial. Int J Behav Nutr Phys Act 2008;5:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kahneman D.. Maps of bounded rationality: psychology for behavioral economics. Am Econ Rev 2003;93:1449–75. [Google Scholar]
- 48. Simon HA.. A behavioral model of rational choice. Q J Econ 1955;69:99–118. [Google Scholar]
- 49. Gigerenzer G.. Fast and frugal heuristics: the tools of bounded rationality Koehler D, Harvey N. editors. Blackwell handbook of judgment and decision making. Hoboken (NJ): John Wiley & Sons; 2004. p. 62–88. [Google Scholar]
- 50. Brandstetter S, Rüter J, Curbach J, Loss J.. A systematic review on empowerment for healthy nutrition in health promotion. Public Health Nutr 2015;18:3146–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ball K.. Traversing myths and mountains: addressing socioeconomic inequities in the promotion of nutrition and physical activity behaviours. Int J Behav Nutr Phys Act 2015;12:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pérez-Escamilla R, Hromi-Fiedler A, Vega-López S, Bermúdez-Millán A, Segura-Pérez S.. Impact of peer nutrition education on dietary behaviors and health outcomes among Latinos: a systematic literature review. J Nutr Educ Behav 2008;40:208–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Harrison GW, Rutström EE.. Experimental evidence on the existence of hypothetical bias in value elicitation methods (Chapter 81) Plott CR, Smith VL. editor. Handbook of experimental economics results Amsterdam (Netherlands): Elsevier; 2008. p. 752–67. [Google Scholar]
- 54. Corbie-Smith GM.. Minority recruitment and participation in health research. N C Med J 2004;65:385–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.