Abstract
High cost of healthy foods could be a barrier to healthy eating. We aimed to examine the association between dietary cost and adherence to the Mediterranean diet in a non-Mediterranean country. We evaluated cross-sectional data from 12,417 adults in the UK Fenland Study. Responses to 130-item food frequency questionnaires were used to calculate a Mediterranean diet score (MDS). Dietary cost was estimated by matching food consumption data with retail prices of five major supermarkets. Using multivariable-adjusted linear regression, we examined the association of MDS and individual foods with dietary cost in absolute and relative scales. Subsequently, we assessed how much the association was explained by education, income, marital status, and occupation, by conducting mediation analysis and testing interaction by these variables. High compared to low MDS (top to bottom third) was associated with marginally higher cost by 5.4% (95% CI 4.4. 6.4%) or £0.20/day (£0.16, 0.25). Participants with high adherence had higher cost associated with the healthier components (e.g. vegetables, fruits, and fish), and lower cost associated with the unhealthy components (e.g. red meat, processed meat and sweets) (p<0.001 each for trend). 20.7% (14.3, 27.0%) of the MDS-cost association was explained by the selected socio-economic factors, and the MDS-cost association was of greater magnitude in lower socio-economic groups (p interaction<0.005). Overall, greater adherence to the Mediterranean diet was associated with marginally higher dietary cost, partly modified and explained by socio-economic status, but the potential economic barriers of high adherence might be offset by cost saving from reducing unhealthy food consumption.
Keywords: Mediterranean diet, dietary cost, socio-economic status
Introduction
The importance of healthy eating is widely recognised, but many individuals continue to make poor dietary choices(1,2), indicating that factors other than consideration of health and nutrition influence people’s dietary choice(3,4). Food cost is suggested to play an important role in determining people’s decisions regarding food purchase and consumption(3,4). Evidence indicates that healthy diets cost more than unhealthy diets(5–9). A recent meta-analysis reported that a diet rich in fruits, vegetables and nuts was on average USD$1.50 more expensive per day compared to a diet of processed foods, meats and refined grains(8). Dietary cost could thus be a barrier to adopting a healthy diet, particularly amongst individuals of lower socio-economic status(10). This socio-economic gradient in diet quality could in turn contribute to disparity in health amongst different socio-economic groups(11).
One example of a healthy diet is the Mediterranean diet, based on the traditional diets of Mediterranean regions(12). The Mediterranean diet is characterised by the use of olive oil as the main source of fat; high consumption of vegetables, legumes, fish; moderate consumption of fruits, cereals, nuts, eggs, dairy, white meat, wine; and low consumption of red meat, processed meat, potatoes and sweets(13). This dietary pattern has been associated with lower risk of many non-communicable diseases in both Mediterranean and non-Mediterranean countries(14–20). Based on the available evidence, some governmental and academic agencies recommend this dietary pattern to a general population for the primary and secondary prevention of non-communicable diseases(13,21,22). In addition, adherence to this dietary pattern has reportedly increased over the past decades in some non-Mediterranean countries(23).
Although the health benefits of adhering to the Mediterranean diet have been demonstrated, evidence of affordability or dietary cost associated with this diet is limited, especially in non-Mediterranean settings. Three population-based studies in Mediterranean countries(6,24,25) showed higher cost of the Mediterranean diet pattern; while two short-term small-scale trials showed conflicting results of greater cost in a Swedish trial(26), but not in a trial of healthy Canadian women(27). To our knowledge, no population-based study on the monetary cost of the Mediterranean diet has been published in non-Mediterranean countries. Moreover, evidence is lacking on whether there is a consistent association across different socio-economic strata, even though socio-economic status influences purchasing behaviours related to food prices(28,29). Therefore, we set two aims in this study. First, we aimed to examine the dietary cost associated with adhering to the Mediterranean diet in the UK. Second, we aimed to assess the extent to which this association is influenced by socio-economic factors.
Methods
Study population
The Fenland Study is a population based cohort study of 12,435 participants recruited from general practices in Cambridgeshire (Cambridge, Ely, Wisbech) from 2004 to 2015(30). The Fenland Study was designed to investigate genetic and environmental factors that interact to determine obesity, type 2 diabetes and related metabolic traits. For recruitment into the Fenland Study, participants were eligible if born between 1950 and 1975 (age 30 to 65 years at recruitment), and exclusion criteria included pregnancy, known diabetes, an inability to walk unaided, psychosis and terminal illness. Participants visited one of the three study centres for a health visit during which they completed a food frequency questionnaire (FFQ) and a general health and lifestyle questionnaire. Trained staff collected blood samples and anthropometric measures. The study was approved by the Health Research Authority NRES Committee East of England-Cambridge Central and all participants gave written informed consent.
Dietary assessment
Dietary assessment was based on a 130-item semi-quantitative FFQ, which asked about dietary intake over the past year. Participants reported intake frequencies of dietary consumption in a standard food portion, ranging from “never or less than once/month” to “6+ per day” across 9 categories. Further questions elicited information regarding milk intake, type of breakfast cereal, type of fat most often used for cooking, and dietary habits including use of dietary supplements. Information from the FFQ was processed to estimate daily intakes based on standard portion sizes and the UK food composition database using the FETA software(31). The FFQ has been previously validated against 16-day weighed records, 24-hour recall and selected biomarkers(32). Dietary intakes were adjusted to 2000 kcal/day (8.37 MJ/day) using the residual method, to reduce confounding by total energy intake and to examine diet quality independent of quantity(33).
We assessed adherence to the Mediterranean diet using a Mediterranean diet score (MDS) which we derived based on recommendations (the Mediterranean diet pyramid) by the Mediterranean Diet Foundation(13). High adherence to this MDS has been shown to be associated with lower risk of cardiovascular diseases in a UK population, and details of the scoring criteria have been described previously(20). Briefly, we derived fifteen dietary components from the recommendations (vegetables, legumes, fruits, nuts, cereals, dairy, fish, red meat, processed meat, white meat, egg, potatoes, sweets, olive oil and alcohol); and assigned scores of 0 to 1 for each component according to the participant’s level of adherence with each recommended intake. The MDS has a possible range of 0 to 15, and measures Mediterranean diet adherence with adjustment to a 2000 kcal/day (8.37 MJ/day) diet.
Dietary cost
Dietary cost of Fenland participants was estimated by attaching a food price variable to each of the 290 food codes in the FFQ’s food and nutrient database, using previously described methods(34–37). Briefly, retail prices were matched in June 2012 using prices on MySupermarket.co.uk, a website for comparing prices across UK supermarkets. Five supermarkets were represented (Tesco, Sainsbury’s, Asda, Waitrose, Ocado) on the website at the time of data collection, which together had 68% of the market share in 2012(35). The lowest, non-sale price listed on the website was matched for each item in the FFQ database, which was subsequently adjusted for preparation and waste to yield an adjusted food price (£) per 100g of the edible portion, using established methods(36–38). Similar to dietary intake, dietary cost was adjusted to a 2000kcal/day diet (8.37MJ/day) using the residual method(33). Total daily dietary cost and cost for each Mediterranean diet component were then summarised for each participant. Cost for adhering to the Mediterranean diet was also summarised, which was defined as the combined cost of the fifteen food components of the MDS. Additionally, cost of the rest of the diet was defined as the total daily dietary cost minus cost for adhering to the Mediterranean diet.
Assessment of socio-economic variables and lifestyle covariates
Social and economic characteristics of Fenland participants were ascertained from the general health and lifestyle questionnaire. Variables of interest included education level, marital status, occupation, and household income. Education level was assessed with questions regarding thirteen types of British education certificates, and responses were classified into three categories as compulsory, further, or higher education. Marital status was classified into single, married, or other. Occupation was assessed by eight possible occupation types and classified into two categories, managerial/professional and routine/technical/others. Equivalised household income for each Fenland participant was calculated based on their reported total household income, taking into account the number of people in the household using previously published methods(39,40). Test site location (Cambridge, Ely, Wisbech) at which the participants attended for the clinical visit was also considered as an area-based socio-economic status variable. Of the three sites, 41% of participants in Cambridge had an equivalised household income of the highest category (>£44,776), and the equivalent figures were 32% in Ely and 23% in Wisbech. Therefore, across the three sites, Cambridge was the least deprived, followed by Ely, and Wisbech was the most deprived.
Information on smoking behaviour was also collected in the same questionnaire. Physical activity energy expenditure was objectively assessed over six days using individually calibrated combined heart rate and movement sensing(41). Weight and height were measured following standardised procedures and used to calculate body-mass index (kg/m2, BMI).
Statistical Analyses
We used descriptive statistics to summarise the characteristics of participants by adherence to the Mediterranean diet, as assessed using the MDS. To assess the association of the MDS with total daily dietary cost, we estimated the linear association for per unit difference in dietary cost for thirds (tertiles) and per SD of the MDS. We adjusted for potential confounders including age, sex, socio-economic status (test site, education level, occupation, household income, marital status), physical activity, BMI and smoking. To check robustness of our result, we tested for the association using an alternative validated Mediterranean diet score (tMDS) with a possible range of 0 to 18(42). Furthermore, across the three categories of the MDS, we estimated the adjusted geometric means, absolute difference, and relative difference of total daily dietary cost and cost of each of the fifteen Mediterranean diet components. For these estimations, linear regressions were used for assessing total dietary cost, cost of adherence, and cost of rest of diet. In analysis of each of the fifteen dietary components, Poisson regression was used for estimating cost associated with each of the fifteen components to account for the positively skewed distribution of each variable.
To assess the extent to which socio-economic factors influenced the association between Mediterranean diet adherence and dietary cost, we compared β coefficients from two regression models between per SD of MDS and per unit (£/day) of dietary cost, without (as the reference model) and with socio-economic factors fitted (βreference and βreference+factor(s) of interest, respectively) as conducted elsewhere(43). In brief, we calculated the percentage attenuation between the two regression models as “100×(βreference – βreference +factor(s) of interest)/βreference”(43). 95% confidence intervals (CI) for the percentage attenuations were estimated by undertaking bootstrapping (n resampling=5000)(43,44). This analysis of attenuation was assumed to have no interaction between the variable of interest and MDS. We therefore tested interaction and stratified analyses of Mediterranean diet adherence and dietary cost, by strata of socio-economic variables by fitting a cross-product interaction term in multivariable-adjusted linear regression for each socio-economic variable (categorical) and MDS (continuous). For each variable showing a significant interaction, we assessed contribution of other socio-economic factors to the association of MDS and dietary cost by strata of the interacting variable.
Missing information on covariates was accounted for by conducting multiple imputation (10 imputed datasets) and pooling estimates with Rubin’s rule(45). The adjusted geometric means, absolute and relative difference, and mediation analysis involving bootstrapping used a single imputed dataset after confirming little difference between single- and multiple-imputation results. All analyses were performed in Stata 14.0 (Stata Corp, Texas, United States). P-values <0.05 were considered significant.
Results
Cohort characteristics
After excluding 18 participants without data from FFQ, 12,417 participants were included for analyses (mean±SD age, 48.6±7.5 years; 53.8% women). The participants’ characteristics and the MDS by strata of cohort characteristics are presented in Table 1. Dietary consumption levels (servings/day) of MDS components are presented in Supplementary Table 1. Mean±SD of MDS was 9.0±1.4. MDS was higher in participants who attended the Cambridge site, were women, more educated, had higher household income, of managerial or professional occupation, were not current smokers, not on antihypertensive medication or had low cardiovascular disease risk. Marital status was not related to the MDS.
Table 1.
Cohort characteristics and Mediterranean diet adherence in the Fenland Study (n=12,417).
| Cohort Characteristics | Mean (SD) or % | Mean (SD) of the Mediterranean diet score Overall: 9.0 (1.4) | % in top third of the score | P* |
|---|---|---|---|---|
| Test site (%)† | ||||
| Wisbech | 27.0 | 8.5 (1.4) | 20.9 | |
| Ely | 36.9 | 8.9 (1.4) | 30.5 | |
| Cambridge | 36.1 | 9.4 (1.4) | 45.5 | <0.001 |
| Age (years) | 48.6 (7.5) | - | - | 0.05 |
| Sex (%) | ||||
| Men | 46.2 | 8.7 (1.4) | 24.7 | |
| Women | 53.8 | 9.3 (1.4) | 40.8 | <0.001 |
| Education level (%)‡ | ||||
| Compulsory | 19.9 | 8.5 (1.4) | 19.2 | |
| Further | 46.2 | 8.8 (1.4) | 28.4 | |
| Higher | 33.9 | 9.6 (1.3) | 48.7 | <0.001 |
| Household income (%) | ||||
| ≤ £25,000 | 32.9 | 8.7 (1.4) | 25.6 | |
| £25,001 to £44,775 | 34.2 | 9.1 (1.4) | 34.8 | |
| ≥ £44,776 | 33.0 | 9.3 (1.4) | 40.9 | <0.001 |
| Marital status (%) | ||||
| Single | 9.1 | 9.1 (1.6) | 38.1 | |
| Married | 81.4 | 9.0 (1.4) | 33.8 | |
| Other§ | 9.5 | 9.1 (1.5) | 37.1 | 0.49 |
| Occupation (%)‖ | ||||
| Routine/Tech/Other | 41.5 | 8.6 (1.4) | 23.5 | |
| Manager/Professional | 58.5 | 9.3 (1.4) | 40.8 | <0.001 |
| Smoking status (%) | ||||
| Never | 54.5 | 9.1 (1.4) | 34.5 | |
| Former | 33.3 | 9.1 (1.4) | 35.6 | |
| Current | 12.2 | 8.4 (1.5) | 21.4 | <0.001 |
| Energy intake (kcal) | 1968 (689) | - | - | <0.001 |
| Energy expenditure (KJ/kg/day) | 53.6 (22.1) | - | - | 0.06 |
| BMI (kg/m2) | 26.9 (4.8) | - | - | <0.001 |
| Use of antihypertensive drug (%) | ||||
| No | 92.6 | 9.0 (1.4) | 33.9 | |
| Yes | 7.5 | 8.8 (1.4) | 26.3 | <0.001 |
| >10% of QRISK2¶ | ||||
| No | 95.4 | 9.0 (1.4) | 34.0 | |
| Yes | 4.6 | 8.5 (1.4) | 20.1 | <0.001 |
For all variables, P-values were estimated based on crude linear regression of Mediterranean diet score (fitted as continuous variable) and each cohort characteristic. For age, energy intake, energy expenditure, and BMI, the P-value represents significance of its association between Mediterranean diet adherence. For the other cohort characteristics, the P-value represents significance in heterogeneity of Mediterranean diet adherence across strata of cohort characteristics.
Of the three sites, Cambridge was the least deprived, followed by Ely, and Wisbech was the most deprived.
Compulsory includes ‘school leaving certificate’, ‘CSE’, ‘GCE O level or GCSE’; Further includes ‘matriculation’, ‘GCE A level, AS level, highers’, ‘technical college exams, city & guilds’, ‘HND GNVQ’, ‘completed apprenticeship’, ‘secretarial college exams’, ‘teaching diploma, HNC, NVQ’, ‘trade certificates’; Higher includes ‘university degree’.
Other included widowed, separated or divorced.
Routine/Tech/Others included clerical, technical, semi-routine and routine jobs; Manager/Professional included modern professional, senior manager, middle management and traditional professional jobs.
Cardiovascular risk score for 10 year risk of cardiovascular diseases.
Association of Mediterranean diet and dietary cost
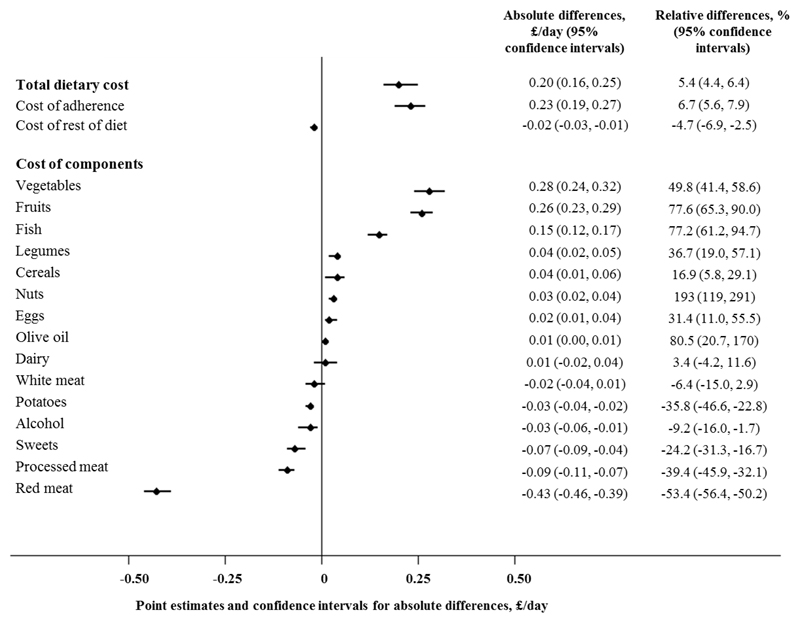
High adherence to the Mediterranean diet was associated with higher dietary cost, and results were similar across all levels of adjustment (Table 2, Supplementary Figure 1). On average, high Mediterranean diet adherence (adjusted mean dietary cost: £4.47, 95% CI 4.44, 4.49) was associated with a £0.20 price difference per day (95% CI 0.16, 0.24) compared to low adherence (£4.26, 95% CI 4.23, 4.29) in the most adjusted model, equivalent to 5.4% (95% CI 4.4. 6.4%) in relative terms (Figure 1). Results were similar when we used an alternative Mediterranean diet score (tMDS)(42), which showed an adjusted mean dietary cost of £4.69 (95% CI 4.66, 4.71) for high adherence compared to £4.08 (95% CI 4.05, 4.11) for low adherence.
Table 2.
Difference (£/day) in dietary cost by Mediterranean diet adherence in the Fenland Study (n=12,417).*
| Mediterranean diet score based on dietary pyramid (0-15) | Model 1† | Model 2† | Model 3† | Adjusted means of dietary cost, £/day (95% CI)† |
|---|---|---|---|---|
| Low (3.3-8.4) | Reference | Reference | Reference | 4.26 (4.23, 4.29) |
| Medium (8.4-9.6) | 0.18 (0.14, 0.22) | 0.15 (0.11, 0.19) | 0.16 (0.12, 0.20) | 4.42 (4.39, 4.45) |
| High (9.6-14.0) | 0.24 (0.20, 0.28) | 0.19 (0.15, 0.24) | 0.20 (0.16, 0.24) | 4.47 (4.44, 4.49) |
| p-trend | <0.001 | <0.001 | <0.001 | |
| Per SD difference | 0.11 (0.09, 0.13) | 0.09 (0.07, 0.11) | 0.10 (0.08, 0.11) |
Daily dietary cost and dietary intake adjusted to a 2000 kcal/day diet using the residual method. Estimates shown are β coefficients from linear regression estimated based on 10 multiple imputations.
Model 1 is adjusted for age and sex; Model 2 is additionally adjusted for test site, education level, occupation, household income, marital status; Model 3 is additionally adjusted for BMI, objectively measured physical activity (energy expenditure) and smoking status. Adjusted means of dietary cost estimated based on model 3 and on single imputed dataset, after confirming no difference in beta coefficients between single and multiple (10) imputations.
Figure 1. Absolute and relative differences in cost of total diet and dietary components comparing high (top third) and low adherence (bottom third) to the Mediterranean diet in the Fenland Study.
Point estimates and confidence intervals shown are for absolute differences. All estimates based on single imputed dataset, after confirming no difference in beta coefficients between single and multiple (10) imputations. Cost of adherence refers to total cost for all components included in the score of adherence to the Mediterranean diet (i.e. sum of dietary components listed); cost of rest of diet refers to any food items not included in the adherence score.
At the cohort level, participants who had a high MDS had higher dietary cost associated with consumption of food components representative of the Mediterranean diet, including vegetables, legumes, fruits, nuts, fish, eggs, cereals and olive oil. The largest absolute cost difference when comparing extreme thirds was associated with vegetables (£0.28 per day, 95% CI 0.24, 0.32) and fruit consumption (£0.26, 95% CI 0.23, 0.29). On the other hand, high Mediterranean diet adherence was also associated with lower diet cost relating to consumption of red meat, processed meat, potatoes, alcoholic beverages and sweets, with the biggest negative cost difference attributed to red meat consumption (-£0.43, 95% CI -0.46, -0.39). No statistically significant cost difference in dairy or white meat consumption was found between high and low adherence to a Mediterranean diet. Multivariable adjusted dietary cost of the overall Mediterranean diet and individual dietary component by thirds of MDS are presented in Supplementary table 2.
In assessing the influence of socio-economic variables, education, income, marital status and occupation were found to partially explain the observed association between Mediterranean diet adherence and dietary cost (Table 3). Among the individual variables, occupation explained the greatest variation in the observed association (15.8%, 95% CI 11.5, 20.5%), followed by income (15.0%, 95% CI 11.4, 18.6%). All tested variables collectively explained 20.7% (95% CI 14.3, 27.0%) of the observed association.
Table 3.
Contribution of socio-economic factors in explaining the association between Mediterranean diet adherence and daily dietary cost in the Fenland Study (n=12,417).
| Difference in daily dietary cost (95% CI), (£/day)* | % variation (95% CI)† | |
|---|---|---|
| Reference model‡ | 0.12 (0.10,0.14) | |
| + adjusted for test site | 0.12 (0.10,0.13) | 2.21 (-1.30, 5.73) |
| + adjusted for education level | 0.11 (0.09,0.13) | 9.93 (5.51, 14.3) |
| + adjusted for income | 0.10 (0.09,0.12) | 15.0 (11.4, 18.6) |
| + adjusted for marital status | 0.12 (0.10,0.14) | -1.34 (-2.30, -0.40) |
| + adjusted for occupation | 0.10 (0.08,0.12) | 15.8 (11.5, 20.2) |
| + adjusted for all socio-economic factors | 0.10 (0.08,0.11) | 20.7 (14.3, 27.0) |
β coefficients from linear regression for daily dietary cost (£/day) per SD of Mediterranean diet score estimated based on 10 imputations.
Percentage difference in β coefficients comparing tested model to reference model (estimated from 5000 bootstrap samples) based on one of the 10 imputations. A positive value indicates attenuation.
Adjusted for age, sex, objectively measured physical activity (energy expenditure), smoking status and BMI.
In assessing potential interaction between MDS and socio-economic variables, significant interaction was observed for test site, education, income and occupation (p for interaction<0.005 for each) (Table 4). No significant association between MDS and dietary cost was observed among population groups that were the most highly educated or not married (i.e. single or others, including widowed, separated or divorced), and a lower magnitude of association was observed among those who visited the Cambridge test site, had the highest household income, or of managerial or professional occupations. The contribution of socio-economic factors in explaining the association between MDS and dietary cost by strata of the interacting socio-economic variables are presented in Supplementary table 3.
Table 4.
Association between adherence to the Mediterranean diet and dietary cost by socio-economic characteristics in the Fenland Study (n=12,417).*
| % of adults | Difference in daily dietary cost (95% CI) (£/day) by adherence to the Mediterranean dietary pyramid | p for interaction† | ||||
|---|---|---|---|---|---|---|
| Low (3.3-8.4) | Medium (8.4-9.6) | High (9.6-14.0) | per SD difference | |||
| Test site‡ | ||||||
| Wisbech | 27.0 | Reference | 0.21 (0.14,0.28) | 0.32 (0.23,0.40) | 0.15 (0.12,0.19) | |
| Ely | 36.9 | Reference | 0.16 (0.09,0.22) | 0.22 (0.15,0.29) | 0.10 (0.08,0.13) | |
| Cambridge | 36.1 | Reference | 0.08 (0.01,0.16) | 0.10 (0.02,0.17) | 0.04 (0.02,0.07) | <0.001 |
| Education level§ | ||||||
| Compulsory | 19.9 | Reference | 0.15 (0.06,0.23) | 0.32 (0.22,0.42) | 0.14 (0.10,0.18) | |
| Further | 46.2 | Reference | 0.18 (0.13,0.24) | 0.27 (0.20,0.33) | 0.12 (0.09,0.14) | |
| Higher | 33.9 | Reference | 0.06 (-0.02,0.14) | 0.03 (-0.04,0.11) | 0.03 (-0.00,0.06) | <0.001 |
| Household income | ||||||
| ≤ £25,000 | 32.9 | Reference | 0.16 (0.09,0.23) | 0.27 (0.19,0.35) | 0.12 (0.09,0.15) | |
| £25,001 to £44,775 | 34.2 | Reference | 0.13 (0.06,0.20) | 0.18 (0.11,0.26) | 0.09 (0.06,0.12) | |
| ≥ £44,776 | 33.0 | Reference | 0.16 (0.09,0.24) | 0.13 (0.06,0.21) | 0.06 (0.03,0.09) | 0.005 |
| Marital status | ||||||
| Single | 9.1 | Reference | -0.00 (-0.17,0.16) | 0.16 (-0.01,0.33) | 0.06 (-0.01,0.13) | |
| Married | 81.4 | Reference | 0.16 (0.12,0.21) | 0.18 (0.13,0.23) | 0.09 (0.07,0.12) | |
| Other‖ | 9.5 | Reference | 0.11 (-0.06,0.28) | 0.17 (-0.01,0.35) | 0.05 (-0.02,0.12) | 0.22 |
| Occupation¶ | ||||||
| Routine/Tech/Other | 41.5 | Reference | 0.17 (0.11,0.23) | 0.28 (0.21,0.35) | 0.13 (0.10,0.15) | |
| Manager/Professional | 58.5 | Reference | 0.13 (0.07,0.18) | 0.13 (0.08,0.19) | 0.06 (0.04,0.09) | 0.002 |
β coefficients from linear regression for daily dietary cost (£/day) by adherence to the Mediterranean dietary pyramid estimated based on 10 imputations. Daily dietary cost and dietary intake were adjusted to a 2000 kcal/day diet using the residual method. All estimates were adjusted for age, sex, objectively measured physical activity (energy expenditure), smoking status and BMI, and for socio-economic variables including education level, household income, marital status, test site and occupation, with exception for the stratified variable. Strata were defined based on non-imputed data.
p for interaction based on Mediterranean diet adherence modelled as a continuous variable and socio-economic variables modelled as categorical variables. Estimation was based on one of the 10 imputed datasets after confirming little difference across datasets.
Of the three sites, Cambridge was the least deprived, followed by Ely, and Wisbech was the most deprived.
Compulsory includes ‘school leaving certificate’, ‘CSE’, ‘GCE O level or GCSE’; Further includes ‘matriculation’, ‘GCE A level, AS level, highers’, ‘technical college exams, city & guilds’, ‘HND, GNVQ’, ‘completed apprenticeship’, ‘secretarial college exams’, ‘teaching diploma, HNC, NVQ’, ‘trade certificates’; Higher includes ‘university degree’.
‘Other’ marital status included widowed, separated or divorced.
Routine/Tech/Others included clerical, technical, semi-routine and routine jobs; Manager/Professional included modern professional, senior manager, middle management, traditional professional jobs.
Discussion
Key findings
In this large population-based Fenland study, high adherence to the Mediterranean diet was associated with a modest degree (5.4%) of higher dietary cost. Compared to low Mediterranean diet adherence, participants who had a high adherence typically had higher dietary cost associated with consumption of food components traditionally marked as healthy (e.g. vegetables, legumes, fruits, nuts, fish, cereals, and olive oil) in this dietary pattern, but lower dietary cost associated with food components traditionally marked as unhealthy (e.g red and processed meat, potatoes and sweets). For those dietary components for which moderate consumption was recommended, the difference in dietary cost comparing high to low adherence could be slightly higher (e.g. eggs), slightly lower (e.g. alcohol), or not significantly different (e.g. dairy, white meat). Socio-economic status partially explained the observed association between Mediterranean diet adherence and dietary cost, and significant interaction was observed between Mediterranean diet adherence and test site, education, income and occupation.
Comparison with other studies
While some previous studies examined the association between the Mediterranean diet and dietary cost, our study was the first to demonstrate the extent to which socio-economic factors contribute to this association. Our results were broadly consistent with some published studies on the Mediterranean diet and dietary cost(6,24–27). But, our estimate of cost difference by adherence to the diet was smaller than estimates on average in most of the previous studies. For example, estimates based on comparing high to low adherence to the Mediterranean diet in Spain was £0.5 per day or greater (crude percentage difference 18% and 28%)(6,24), while our estimate showed £0.2 per day (5.4%).
Outside of the Mediterranean region, a small (N=30) trial in Sweden compared between the daily 2000-kcal dietary costs of the Mediterranean diet and the usual Swedish diet(26). The authors reported that the average cost difference was €1.45 (SD 0.10) (24%, or equivalent to £1.29 as of 26 July 2017) per day(26). In contrast, a trial (n=73) among women in Canada reported no significant change in total daily dietary cost following a 12 week Mediterranean diet intervention: 8.61 CAN$ (£5.27) before intervention and 8.75 CAN$ (£5.36) after intervention (p=0.58)(27). Overall, there is inconsistency in existing evidence, study populations, and methods to assess the association or effect, as well as no prior evidence for the effect modified by underlying socio-economic diversity. Therefore, whether or not the Mediterranean diet costs more than a usual diet remains inconclusive.
Two studies of existing literature reported contribution of the components of the Mediterranean diet to dietary cost, and both were consistent with our findings. The trial of women in Canada found that the Mediterranean-diet intervention increased cost related to consumption of healthy components (e.g. vegetables, fish, nuts and seeds, canola or olive oil), and reduced cost related to consumption of unhealthy components (e.g. red meat, refined grains, fast food)(27). Similarly, the trial in Sweden found higher costs associated with consumption of fish, vegetable, and poultry and lower cost associated with the consumption of meat and desserts in the Mediterranean diet intervention group compared to the control group(26), and one observational study in Spain also showed similar results if adherence to the Mediterranean diet was higher(24).
The observed positive association between Mediterranean diet adherence and socio-economic status is consistent with other evidence from adult populations in both Mediterranean(46) and non-Mediterranean countries(47). With exception, a study in Portugal reported an inverse association in that people of higher socio-economic status had lower Mediterranean diet adherence(48). However, as the authors acknowledged, this is likely reflective of the current phase of the nutrition transition in Portugal, during which urbanisation and increased income levels are linked to higher intakes of animal products or processed foods(48,49). No study was found which simultaneously examined dietary cost of a Mediterranean diet and how this association varied by socio-economic status.
Interpretation of findings and implications
Our results indicate that in this non-Mediterranean cohort, high adherence to the Mediterranean diet, based on an MDS previously shown to be associated with lower cardiovascular disease risk(20), was associated with higher dietary cost, but the degree of cost difference was modest compared to previous studies(6,24,26). In addition, there was negligible difference in dietary cost associated with consumption of items not included in the Mediterranean diet score (i.e. cost of rest of diet: Figure 1 and Supplementary table 3). Therefore, the observed cost difference was mainly associated with differential costs across Mediterranean diet components. As discussed above, individuals with low adherence to the Mediterranean diet had higher cost associated with unhealthy food items such as red meat and processed meat. This gives rise to the possibility of increasing adherence to the Mediterranean diet on an individual level without increasing cost, by substituting spending on unhealthy items for more healthy items(50). The feasibility of this approach is supported by evidence from the trial in Canada(27). Moreover, although our work did not include details within each food group, increasing adherence to the Mediterranean diet might also be achieved by increasing consumption of the cheaper healthy components, or lower cost options of the more expensive components, such as by increasing consumption of pulses, legumes, dried fruit and canned fish(51). Overall, our results from this UK population suggest that adopting a Mediterranean diet could potentially be a financially feasible way of achieving a healthy diet. Methods of diet optimisation modelling or linear modelling could be employed to model possible ways of increasing Mediterranean diet adherence at any given cost(52–54).
Our results suggest that socio-economic factors explained about 22% of the association between Mediterranean diet adherence and dietary cost. This supports the hypothesis that socio-economic status could be related to both dietary behaviour and dietary spending habits(55). Results from our stratified analyses showed non-significant or lower magnitudes of associations between the dietary adherence and dietary cost among individuals with relatively high socio-economic status. This suggests that amongst people of a high socio-economic status, dietary cost is less likely to be associated with, or influence their adherence to a Mediterranean diet compared to people of lower socio-economic status. This in turn supports the notion that high dietary cost is more likely to be a barrier against adopting a healthy diet amongst people of lower socio-economic status(56,57).
Our observed difference by £0.20 per day (approximately equivalent to £6.10 (4.90, 7.30) cost difference per month or £73.20 (58.80, 87.60) per year) between extreme thirds of the adherence measure appears modest compared to both other studies on the Mediterranean diet as described, as well as other studies on alternative indexes of dietary quality in the UK(9,35), therefore suggesting that the Mediterranean dietary pattern may be a relatively affordable option of a healthy diet in this country. However, the relevance of this magnitude of difference to a real world setting deserves further discussion. In our analyses, we estimated the cost difference adjusted to a 2000 kcal/day diet, in order to assess the cost difference associated with a difference in diet quality independent of quantity(33,34). In this study, participants in the lowest third of adherence to a Mediterranean diet had an average calorie intake of 2,124 kcal/day, compared to 1,856 kcal/day among participants in the top third of adherence, which is in line with other evidence that healthier diets are less energy dense(58). Therefore, if an increased adherence to a Mediterranean diet is simultaneously associated with a decrease in total energy in a natural setting, the cost difference reported in this study may be an overestimation of the real cost difference(50). Also, the calculation of dietary cost in this study made the assumption that all meals were prepared and consumed at home, and did not factor in the higher costs associated with out-of-home meals. As a result, the true monetary value of a Mediterranean diet in the UK remains to be determined.
Regardless of the true cost difference, the greater magnitude of cost difference observed among people of lower socio-economic status could in turn accentuate the existing socio-economic disparity in health(59,60), but it remains unclear whether or not this magnitude of difference is meaningful for individuals or public health in the UK or elsewhere. Previous studies have shown that dietary interventions may be cost-effective strategies for reducing medical costs associated with non-communicable diseases(61,62). For the US and Canadian populations, cost-effectiveness of adherence to the Mediterranean diet has been supported by modelling the dietary adherence and medical expenditure due to cardiovascular diseases(63), and research from Australia(64) and France(65) also reported that a Mediterranean diet is cost-effective for prevention of diabetes and secondary prevention of myocardial infarction. Similar work in other countries is warranted accounting for cultural acceptance of the Mediterranean diet across different socio-economic groups, and population-specific burdens of various non-communicable diseases.
Apart from the overall dietary pattern, our work highlights the importance of focusing on individual food groups to achieve a healthy diet pattern in an economic context. There is a compelling case that public health policies should play key roles in controlling subsidies, taxation, and other strategies to improve diet quality(66,67), in particular for those with relatively low socio-economic status. The potential effectiveness of these policies can be justified by trial evidence which showed that price reduction on healthy dietary components increased consumption of these dietary components(68,69). Our work additionally raises the possibility that adherence to the Mediterranean diet could be improved without increases in dietary cost. Therefore, recommendation of and facilitating adherence to a Mediterranean diet may help improve public health at the population level by providing dietary guidelines on substituting healthy alternatives for unhealthy food items to overcome economic barriers.
Strengths and limitations
Our study has the advantage of being large, population-based, and it represents a contemporary cohort with price data collected during a matching period, which makes findings relevant to the current UK population. A healthy cohort bias could exist however, given the Fenland cohort has lower prevalence of smoking and obesity compared to the general UK population(70,71), and thus might limit the generalisability of findings. Since price data were derived from supermarket prices, this may not reflect real expenditure nor take into account any variation in prices due to region, time of year, or type of establishment from which the participants made their purchase(6). Additionally, because price data was collected at one time point in 2012 while food intake information was collected from between 2004 to 2015, we have not accounted for possible changes in dietary intake over the years as a result of inflation, or price changes associated with particular food items. Surrogate categorical variables of socio-economic status were also used in our analyses, which might not fully capture socio-economic variation in the population. Since both the MDS and dietary cost were derived from the same FFQ, we cannot rule out the possibility that some level of association might be artefactual. Due to the structure of the FFQ, details in dietary intake such as culinary methods (e.g. cooking or food preparation) or type of product consumed (e.g. cut of meat, or organic and non-organic products) was not captured, although such differences may be relevant to both Mediterranean diet adherence and dietary cost. Because this study adopted a cross-sectional design and entails residual confounding, we cannot infer any causal association between increasing Mediterranean diet adherence and dietary cost.
Conclusions
High adherence to the Mediterranean diet was associated with marginally higher dietary cost in a large UK population, although strength of association differed by socio-economic status. Our findings provide evidence that although higher cost associated with healthy diets could be a barrier against healthy eating, especially among people of lower socio-economic status, savings could be made by reducing consumption of food components not representative of the Mediterranean diet. These findings should prompt debate on public health interventions to help lower dietary costs associated with healthy diets and also to guide the public to recognise feasibility of improving certain dietary habits without substantial financial burden, which could in turn help improve overall dietary patterns and tackle the issues of socio-economic disparities in health.
Supplementary Material
Acknowledgements
The authors thank all the Fenland Study volunteers for their time and participation, as well as the Fenland Study Co-ordination team, the Field Epidemiology team, the data management team and the laboratory team.
Financial support: The Fenland Study is funded by the Medical Research Council. Support from Medical Research Council core programmes MC_UU_12015/1 and MC_UU_12015/5 is acknowledged.
Footnotes
Ethics approval and consent to participate: The Fenland Study was approved by the Health Research Authority NRES Committee East of England-Cambridge Central and all participants gave written informed consent.
Consent for publication: Not applicable.
Availability of data and material: Researchers with an institutional address seeking the analysis dataset for this work can submit a data request to the Fenland Study Committee by emailing fenlandstudy@mrc-epid.cam.ac.uk.
Conflict of interest: The authors declare that they have no conflict of interest.
Authorship: SB, NGF, SJG, and NJW acquired the data as Fenland Study principal investigators, with NJW as chief investigator. TYNT, FI, PM and NGF conceived and designed the research question. TYNT analysed the data and wrote the first draft of the manuscript, and FI, PM and NGF provided input on data analysis and interpretation of results. All authors revised the manuscript critically for important intellectual content, and read and approved the final manuscript.
References
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Imamura F, Micha R, Khatibzadeh S, et al. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob Heal. 2015;3(3):e132–42. doi: 10.1016/S2214-109X(14)70381-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glanz K, Basil M, Maibach E, et al. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc. 1998;98(10):1118–26. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 4.Kearney M, Kearney J, Dunne A, et al. Sociodemographic determinants of perceived influences on food choice in a nationally representative sample of Irish adults. Public Health Nutr. 2000;3(2):219–26. doi: 10.1017/s1368980000000252. [DOI] [PubMed] [Google Scholar]
- 5.Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr. 2010;92(5):1181–8. doi: 10.3945/ajcn.2010.29300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez CN, Martinez-Gonzalez MA, Sanchez-Villegas A, et al. Costs of Mediterranean and western dietary patterns in a Spanish cohort and their relationship with prospective weight change. J Epidemiol Community Health. 2009;63(11):920–7. doi: 10.1136/jech.2008.081208. [DOI] [PubMed] [Google Scholar]
- 7.Mhurchu CN. Food costs and healthful diets: the need for solution-oriented research and policies. Am J Cinical Nutr. 2010;92(5):1007–8. doi: 10.3945/ajcn.110.002717. [DOI] [PubMed] [Google Scholar]
- 8.Rao M, Afshin A, Singh G, et al. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ Open. 2013;3(12):e004277. doi: 10.1136/bmjopen-2013-004277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conklin AI, Monsivais P, Khaw K-T, et al. Dietary Diversity, Diet Cost, and Incidence of Type 2 Diabetes in the United Kingdom: A Prospective Cohort Study. PLoS Med. 2016;13(7):e1002085. doi: 10.1371/journal.pmed.1002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marmot M, Brunner E. Cohort Profile: the Whitehall II study. Int J Epidemiol. 2005;34(2):251–6. doi: 10.1093/ije/dyh372. [DOI] [PubMed] [Google Scholar]
- 11.Rehm CD, Monsivais P, Drewnowski A. Relation between diet cost and Healthy Eating Index 2010 scores among adults in the United States 2007-2010. Prev Med (Baltim) 2015;73:70–5. doi: 10.1016/j.ypmed.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Willett WC, Sacks F, Trichopoulou A, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6 Suppl):1402S–1406S. doi: 10.1093/ajcn/61.6.1402S. [DOI] [PubMed] [Google Scholar]
- 13.Bach-Faig A, Berry EM, Lairon D, et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011;14(12A):2274–84. doi: 10.1017/S1368980011002515. [DOI] [PubMed] [Google Scholar]
- 14.Sofi F, Macchi C, Abbate R, et al. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17(12):2769–82. doi: 10.1017/S1368980013003169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kastorini CM, Milionis HJ, Goudevenos JA, et al. Nutr Metab Cardiovasc Dis. 7. Vol. 20. Elsevier Ltd; 2010. Mediterranean diet and coronary heart disease: is obesity a link? - A systematic review; pp. 536–51. [DOI] [PubMed] [Google Scholar]
- 16.Psaltopoulou T, Sergentanis T, Panagiotakos D, et al. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann Neurol. 2013;74(4):580–91. doi: 10.1002/ana.23944. [DOI] [PubMed] [Google Scholar]
- 17.Schwingshackl L, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: A systematic review and meta-analysis of observational studies. Int J Cancer. 2014;135(8):1884–97. doi: 10.1002/ijc.28824. [DOI] [PubMed] [Google Scholar]
- 18.de Lorgeril M, Salen P, Martin J-LL, et al. Mediterranean Diet, Traditional Risk Factors, and the Rate of Cardiovascular Complications After Myocardial Infarction : Final Report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 19.Estruch R, Ros E, Salas-Salvadó J, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med. 2013;368(14):1279–90. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 20.Tong TYN, Wareham NJ, Khaw K-T, et al. BMC Med. 1. Vol. 14. BMC Medicine; 2016. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk study; p. 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Office of Disease Prevention and Health Promotion. Appendix 4. USDA Food Patterns: Healthy Mediterranean-Style Eating Pattern - 2015-2020 Dietary Guidelines - health.gov. [cited 2016 Apr 27];2015 [Internet] Available from: http://health.gov/dietaryguidelines/2015/guidelines/appendix-4/
- 22.National Health Service. What is a Mediterranean diet? - NHS Choices. Department of Health; 2013. [cited 2014 Mar 18]. [Internet]; Available from: http://www.nhs.uk/Livewell/Goodfood/Pages/what-is-a-Mediterranean-diet.aspx. [Google Scholar]
- 23.da Silva R, Bach-Faig A, Raido Quintana B, et al. Worldwide variation of adherence to the Mediterranean diet, in 1961-1965 and 2000-2003. Public Health Nutr. 2009;12(9A):1676–84. doi: 10.1017/S1368980009990541. [DOI] [PubMed] [Google Scholar]
- 24.Schröder H, Marrugat J, Covas MI. High monetary costs of dietary patterns associated with lower body mass index: a population-based study. Int J Obes. 2006;30(10):1574–9. doi: 10.1038/sj.ijo.0803308. [DOI] [PubMed] [Google Scholar]
- 25.Vlismas K, Panagiotakos DB, Pitsavos C, et al. Quality, but not cost, of diet is associated with 5-year incidence of CVD: the ATTICA study. Public Health Nutr. 2010;13(11):1890–7. doi: 10.1017/S1368980010000649. [DOI] [PubMed] [Google Scholar]
- 26.Rydén P, Sydner YM, Hagfors L. Counting the cost of healthy eating: a Swedish comparison of Mediterranean-style and ordinary diets. Int J Consum Stud. 2008;32(2):138–46. [Google Scholar]
- 27.Goulet J, Lamarche B, Lemieux S, et al. A nutritional intervention promoting a Mediterranean food pattern does not affect total daily dietary cost in North American women in free-living conditions. J Nutr. 2008;138(1):54–9. doi: 10.1093/jn/138.1.54. [DOI] [PubMed] [Google Scholar]
- 28.Monsivais P, Aggarwal A, Drewnowski A. Are socio-economic disparities in diet quality explained by diet cost? J Epidemiol Community Health. 2012;66(6):530–5. doi: 10.1136/jech.2010.122333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aggarwal A, Monsivais P, Cook A, et al. Does diet cost mediate the relation between socioeconomic position and diet quality? Eur J Clin Nutr. 2011;65(9):1059–66. doi: 10.1038/ejcn.2011.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Lucia Rolfe E, Loos RJF, Druet C, et al. Association between birth weight and visceral fat in adults. Am J Clin Nutr. 2010;92(2):347–52. doi: 10.3945/ajcn.2010.29247. [DOI] [PubMed] [Google Scholar]
- 31.Mulligan A, Luben RN, Bhaniani A, et al. A new tool for converting food frequency questionnaire data into nutrient and food group values: FETA research methods and availability. BMJ Open. 2014;4(3):e004503. doi: 10.1136/bmjopen-2013-004503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bingham SA, Gill C, Welch A, et al. Comparison of dietary assessment methods in nutritional epidemiology: weighed records v. 24 h recalls, food-frequency questionnaires and estimated-diet records. Br J Nutr. 1994;72(4):619. doi: 10.1079/bjn19940064. [DOI] [PubMed] [Google Scholar]
- 33.Hu FB, Stampfer MJ, Rimm E, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149(6):531–40. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 34.Monsivais P, Perrigue MM, Adams SL, et al. Measuring diet cost at the individual level: a comparison of three methods. Eur J Clin Nutr. 2013;67(11):1220–5. doi: 10.1038/ejcn.2013.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Monsivais P, Scarborough P, Lloyd T, et al. Greater accordance with the Dietary Approaches to Stop Hypertension dietary pattern is associated with lower diet-related greenhouse gas production but higher dietary costs in the United Kingdom. Am J Clin Nutr. 2015;102(1):138–45. doi: 10.3945/ajcn.114.090639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Monsivais P, Drewnowski A. Lower-energy-density diets are associated with higher monetary costs per kilocalorie and are consumed by women of higher socioeconomic status. J Am Diet Assoc. 2009;109(5):814–22. doi: 10.1016/j.jada.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Monsivais P, Drewnowski A. The Rising Cost of Low-Energy-Density Foods. J Am Diet Assoc. 2007;107(12):2071–6. doi: 10.1016/j.jada.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Monsivais P, Rehm CD, Drewnowski A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern Med. 2013;173(20):1922–4. doi: 10.1001/jamainternmed.2013.9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anyaegbu G. Using the OECD equivalence scale in taxes and benefits analysis. Labour Gaz. 2010;4(1):49–54. [Google Scholar]
- 40.Maguire ER, Monsivais P. Socio-economic dietary inequalities in UK adults: an updated picture of key food groups and nutrients from national surveillance data. Br J Nutr. 2015;113(1):181–9. doi: 10.1017/S0007114514002621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brage S, Westgate K, Franks PW, et al. Estimation of Free-Living Energy Expenditure by Heart Rate and Movement Sensing: A Doubly-Labelled Water Study. Criscuolo F, editor. PLoS One. 2015;10(9):e0137206. doi: 10.1371/journal.pone.0137206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.The InterAct Consortium. Mediterranean Diet and Type 2 Diabetes Risk in the European Prospective Investigation Into Cancer and Nutrition (EPIC) Study: The InterAct project. Diabetes Care. 2011 Jul 27;34(9):1913–8. doi: 10.2337/dc11-0891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stringhini S, Tabak AG, Akbaraly TN, et al. Contribution of modifiable risk factors to social inequalities in type 2 diabetes: prospective Whitehall II cohort study. BMJ. 2012 Aug 21;345:e5452. doi: 10.1136/bmj.e5452. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Efron B. Ann Stat. 1. Vol. 7. Institute of Mathematical Statistics; 1979. Bootstrap Methods: Another Look at the Jackknife; pp. 1–26. [Google Scholar]
- 45.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 46.González CA, Argilaga S, Agudo A, et al. [Sociodemographic differences in adherence to the Mediterranean dietary pattern in Spanish populations] Gac Sanit. 2002;16(3):214–21. doi: 10.1016/s0213-9111(02)71664-6. [DOI] [PubMed] [Google Scholar]
- 47.Marques-Vidal P, Waeber G, Vollenweider P, et al. Sociodemographic and behavioural determinants of a healthy diet in Switzerland. Ann Nutr Metab. 2015;67(2):87–95. doi: 10.1159/000437393. [DOI] [PubMed] [Google Scholar]
- 48.Rodrigues SSP, Caraher M, Trichopoulou A, et al. Portuguese households’ diet quality (adherence to Mediterranean food pattern and compliance with WHO population dietary goals): trends, regional disparities and socioeconomic determinants. Eur J Clin Nutr. 2008;62(11):1263–72. doi: 10.1038/sj.ejcn.1602852. [DOI] [PubMed] [Google Scholar]
- 49.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84(2):289–98. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 50.Jones NRV, Tong TYN, Monsivais P. Meeting UK dietary recommendations is associated with higher estimated consumer food costs: An analysis using the National Diet and Nutrition Survey and consumer expenditure data, 2008-12. Public Health Nutr. 2017 doi: 10.1017/S1368980017003275. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Drewnowski A, Eichelsdoerfer P. The Mediterranean diet: does it have to cost more? Public Health Nutr. 2009;12(9A):1621–8. doi: 10.1017/S1368980009990462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maillot M, Drewnowski A. Energy allowances for solid fats and added sugars in nutritionally adequate U.S. diets estimated at 17-33% by a linear programming model. J Nutr. 2011;141(2):333–40. doi: 10.3945/jn.110.131920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Masset G, Monsivais P, Maillot M, et al. Diet optimization methods can help translate dietary guidelines into a cancer prevention food plan. J Nutr. 2009;139(8):1541–8. doi: 10.3945/jn.109.104398. [DOI] [PubMed] [Google Scholar]
- 54.Wilson N, Nhung N, Mhurchu CN, et al. Foods and Dietary Patterns That Are Healthy, Low-Cost, and Environmentally Sustainable: A Case Study of Optimization Modeling for New Zealand. PLoS One. 2013;8(3):e59648. doi: 10.1371/journal.pone.0059648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pechey R, Monsivais P. Prev Med (Baltim) Vol. 88. The Authors; 2016. Socioeconomic inequalities in the healthiness of food choices: Exploring the contributions of food expenditures; pp. 203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mackenbach JD, Brage S, Forouhi NG, et al. Does the importance of dietary costs for fruit and vegetable intake vary by socioeconomic position? Br J Nutr. 2015;114(9):1464–70. doi: 10.1017/S0007114515003025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Green R, Cornelsen L, Dangour AD, et al. The effect of rising food prices on food consumption: systematic review with meta-regression. BMJ. 2013 Jun 17;346:f3703. doi: 10.1136/bmj.f3703. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murakami K, Livingstone MBE. Energy density of meals and snacks in the British diet in relation to overall diet quality, BMI and waist circumference: findings from the National Diet and Nutrition Survey. Br J Nutr. 2016;116(8):1479–89. doi: 10.1017/S0007114516003573. [DOI] [PubMed] [Google Scholar]
- 59.Dalstra Jaa, Kunst aE, Borell C, et al. Socioeconomic differences in the prevalence of common chronic diseases: An overview of eight European countries. Int J Epidemiol. 2005;34(2):316–26. doi: 10.1093/ije/dyh386. [DOI] [PubMed] [Google Scholar]
- 60.Elgar FJ, Pförtner TK, Moor I, et al. Socioeconomic inequalities in adolescent health 2002-2010: A time-series analysis of 34 countries participating in the Health Behaviour in School-aged Children study. Lancet. 2015;385(9982):2088–95. doi: 10.1016/S0140-6736(14)61460-4. [DOI] [PubMed] [Google Scholar]
- 61.Zhang D, Cogswell ME, Wang G, et al. Evidence of Dietary Improvement and Preventable Costs of Cardiovascular Disease. Am J Cardiol. 2017 doi: 10.1016/j.amjcard.2017.07.068. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 62.Saulle R, Semyonov L, La Torre G. Cost and Cost-Effectiveness of the Mediterranean Diet: Results of a Systematic Review. Nutrients. 2013;5(11):4566–86. doi: 10.3390/nu5114566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abdullah MMH, Jones JPH, Jones PJH. Economic benefits of the Mediterranean-style diet consumption in Canada and the United States. Food Nutr Res. 2015;59:1–10. doi: 10.3402/fnr.v59.27541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dalziel K, Segal L. Time to give nutrition interventions a higher profile: cost-effectiveness of 10 nutrition interventions. Health Promot Int. 2007;22(4):271–83. doi: 10.1093/heapro/dam027. [DOI] [PubMed] [Google Scholar]
- 65.Dalziel K, Segal L, de Lorgeril M. A Mediterranean diet is cost-effective in patients with previous myocardial infarction. J Nutr. 2006;136(7):1879–85. doi: 10.1093/jn/136.7.1879. [DOI] [PubMed] [Google Scholar]
- 66.Eyles H, Ni Mhurchu C, Nghiem N, et al. Food pricing strategies, population diets, and non-communicable disease: a systematic review of simulation studies. PLoS Med. 2012;9(12):e1001353. doi: 10.1371/journal.pmed.1001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Powell LM, Chriqui JF, Khan T, et al. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obes Rev. 2013;14(2):110–28. doi: 10.1111/obr.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.French SA, Story M, Jeffery RW, et al. Pricing strategy to promote fruit and vegetable purchase in high school cafeterias. J Am Diet Assoc. 1997;97(9):1008–10. doi: 10.1016/S0002-8223(97)00242-3. [DOI] [PubMed] [Google Scholar]
- 69.French SA, Jeffery RW, Story M, et al. Pricing and promotion effects on low-fat vending snack purchases: The CHIPS study. Am J Public Health. 2001;91(1):112–7. doi: 10.2105/ajph.91.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lifestyle Statistics team. Health and Social Care Information Centre. Statistics on smoking England 2015. 2015.
- 71.Public Health England Obesity Knowledge and Intelligence Team. UK and Ireland prevalence and trends. [cited 2016 May 9];2016 [Internet] Available from: http://www.noo.org.uk/NOO_about_obesity/adult_obesity/UK_prevalence_and_trends.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.