Abstract
Objective
To offer primary care providers a comprehensive summary of breast reconstruction options and complications.
Quality of evidence
A literature search was conducted in PubMed with no time restriction using the search terms breast reconstruction, summary, review, complications, and options. Levels of evidence range from I to III.
Main message
As breast cancer survival rates increase, the focus of breast cancer management must shift to include the restoration of a patient’s quality of life after cancer. Breast reconstruction plays a crucial role in the restoration of normality for these women. Women who undergo mastectomy often suffer from challenges related to body image, self-esteem, and a decrease in quality of life scores. Cancer Care Ontario’s Breast Cancer Treatment Pathway Map mandates that all women diagnosed with breast cancer who might require mastectomy be referred to a plastic surgeon to discuss reconstructive options before surgery.
Conclusion
The knowledge and guidance of primary care providers is critical to effectively guiding and supporting patients who might undergo breast reconstruction in their decision-making processes. A thorough understanding of patient selection factors, modern options for breast reconstruction, and expected outcomes is essential.
Breast cancer continues to be the most common form of cancer affecting women in Canada (1 in 9 women).1 Certain women (with genetic mutations like BRCA1, BRCA2, and TP53) have a greater likelihood of developing the disease. Diagnostic and treatment improvements have increased survival to 87%,2,3 leading to a need to focus on restoration of quality of life after cancer. Studies show that women who undergo mastectomy often suffer from challenges related to body image, self-esteem, and a decrease in quality-of-life scores.4,5 Postmastectomy breast reconstruction can offset or reverse these negative sequelae of prophylactic or oncologic mastectomies. It has been shown to be one of the most important determinants of functional and psychosocial well-being, long-term health, and patient satisfaction compared with patients who have undergone mastectomy without reconstruction.6,7 However, rates of breast reconstruction in Canada continue to be low, approaching 2.7% to 18.5%.8 While not all women will be candidates or have a desire to undergo breast reconstruction, 100% of women should be given the option and feel that they were appropriately counseled to make a confident decision. The key to this lofty goal is complete engagement of the entire health care team.
In 2015, Cancer Care Ontario (CCO) released a Breast Cancer Treatment Pathway Map,9 which mandated that all women diagnosed with operable breast cancer requiring mastectomy be referred to a plastic surgeon to discuss reconstructive options before their scheduled mastectomies. The algorithm also outlines appropriate treatment and reconstructive options for individual patients.
Quality of evidence
A PubMed literature search was conducted with no time restriction using breast reconstruction, summary, review, complications, and options. Guidelines published by national cancer-related organizations were also reviewed. A supplemental search of references from selected articles and reference lists of guidelines was also performed. Finally, expert experience from key opinion leaders in Canadian breast reconstruction was included to provide the most up-to-date and comprehensive review of modern options for reconstruction. Levels of evidence range from I to III.
Main message
The knowledge and guidance of the primary care physician (PCP) is critical during the time of diagnosis and decision making. As one of the patient’s most valuable resources during the journey through breast cancer treatment, the PCP must understand and support decision making around modern reconstructive options. Unfortunately, the most recent comprehensive review we found written specifically with PCPs in mind comes from more than 35 years ago10 and much has changed. The purpose of this review is to provide a modern update on reconstructive options that offers PCPs a framework for discussion with and support of women who are candidates for breast reconstruction.
Dispelling false beliefs.
An unfortunate number of patient and health care provider beliefs around breast reconstruction are outdated and false. Patients often think they are too old,11 feel vanity in their desire to undergo reconstruction, worry that reconstruction will interfere with cancer treatment, or believe that breast reconstruction is dangerous and fraught with complications.
The reality is that there are no absolute contraindications to breast reconstruction. Certainly, the patients’ general health and the type and grade of malignancy must be considered. Certain factors such as morbid obesity and smoking considerably limit options. In most cases, however, health- and tumour-related factors will influence the type and timing of reconstruction but not whether or not reconstruction is an option. Breast reconstruction itself does not lead to an increase in recurrence nor increased difficulty in surveillance.
Timing of breast reconstruction.
Immediate breast reconstruction, performed during the same procedure as oncologic resection, has the distinct advantages of decreasing the total number of surgeries, providing improved psychological benefit, and preserving much of the native breast skin and potentially the nipple. Delayed reconstruction might be recommended for patients with advanced disease, those for whom there are uncertainties about disease control, or those not interested in or prepared to make a reconstructive decision at the time of their oncologic procedure (Table 1).
Table 1.
Timing of breast reconstruction: Immediate versus delayed.
| TIMING | DEFINITION | IDEAL CANDIDATE | ADVANTAGES | DISADVANTAGES |
|---|---|---|---|---|
| Immediate | Reconstructive procedure is started during the same operation as the mastectomy or lumpectomy |
|
|
|
| Delayed | Reconstructive procedure occurs months to years after mastectomy or lumpectomy |
|
|
|
Mastectomy incisions.
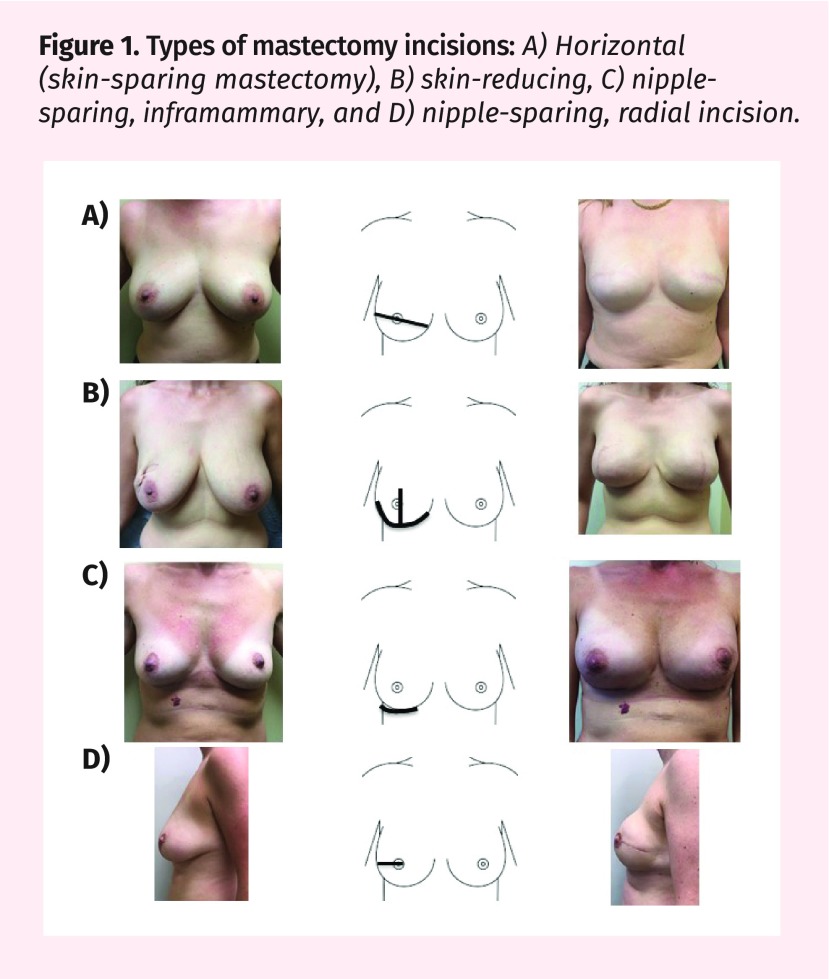
Before deciding on a reconstructive technique, a decision about which type of mastectomy is appropriate is made by the general surgeon, if possible in consultation with the plastic surgeon. When immediate reconstruction is not planned, a horizontal incision is made to remove excess skin with the mastectomy specimen and allow the remaining skin to close neatly, flat against the chest wall. When immediate reconstruction is planned, the incision is modified to preserve as much breast skin as possible. Traditionally, “skin-sparing” mastectomy involves nipple and areolar excision as an ellipse, leaving a horizontal scar and most native breast skin behind. Today, in appropriate patients, a “nipple-sparing” approach can be used. In these cases, surgeons will decide where to make the access incision for removal of the underlying breast tissue while preserving all overlying skin, nipple, and areola. A nipple-sparing approach can often be considered if these criteria are met:
the tumour does not involve the area around the nipple;
the patient has small- or medium-sized breasts (generally, A to a small C cup size); and
the patient has good native nipple position (minimal ptosis).
The various incisions types are shown in Figure 1.
Figure 1.
Types of mastectomy incisions: A) Horizontal (skin-sparing mastectomy), B) skin-reducing, C) nipple-sparing, inframammary, and D) nipple-sparing, radial incision.
Options for breast reconstruction.
Options for breast reconstruction are divided into alloplastic (implant-based) or autologous (tissue-based) reconstruction (Table 2). Implant-based reconstruction is currently the most common type of breast reconstruction performed in North America.12 Substantial improvements made in both implant technology and techniques have allowed for aesthetically pleasing, efficient, and safe reconstruction in most breast cancer patients. Likewise, advances, particularly in the field of microsurgery, have provided options for transfer of tissue from various body areas with minimal donor-site morbidity. Both categories of breast reconstruction can be performed in an immediate or delayed fashion.
Table 2.
Types of breast reconstruction: Alloplastic versus autologous.
| TYPE | IDEAL CANDIDATE | ADVANTAGES | DISADVANTAGES | COMPLICATIONS |
|---|---|---|---|---|
| Alloplastic (implant-based) |
|
|
|
|
| Autologous (tissue-based) |
|
|
|
|
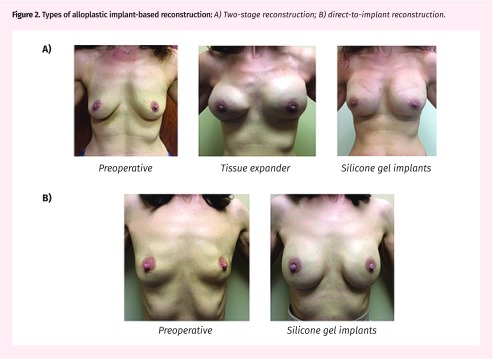
Alloplastic implant-based reconstruction: Alloplastic reconstruction (Figure 2) is traditionally performed in 2 stages involving insertion of a tissue expander followed by implant exchange. A “direct-to-implant” approach allows reconstruction with the permanent implant at time of mastectomy. Table 3 provides guidance for deciding between these approaches. Alloplastic reconstruction involves shorter surgeries with easier recovery but with the possible need for ongoing implant monitoring or adjustment in the future. Surgery can take 1 to 2 hours per side, and return to normal activity is expected within 2 to 3 weeks. Exercise and heavy lifting are restricted for 6 weeks.
Figure 2.
Types of alloplastic implant-based reconstruction: A) Two-stage reconstruction; B) direct-to-implant reconstruction.
Table 3.
Types of alloplastic (implant-based) reconstruction
| TYPE | DEFINITION | TECHNICAL DETAILS | ADVANTAGES | DISADVANTAGES |
|---|---|---|---|---|
| Two stage | Performed in 2 stages:
|
|
|
|
| Direct to implant | Final implant inserted at time of mastectomy |
|
|
|
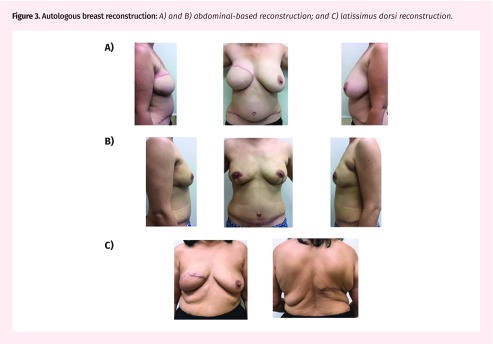
Autologous tissue reconstruction: Autologous reconstruction (Figure 3) uses the patient’s own skin, fat, and muscle to reconstruct the breast mound. Broadly, autologous reconstruction is divided into pedicled versus free flap. The advantages and disadvantages of each are described in Table 4. Pedicled flaps originate from tissue close to the breast and use native blood supply to vascularize the breast mound. Examples of pedicled flaps include the latissimus dorsi flap and the pedicled TRAM (transverse rectus abdominis myocutaneous) flap. Alternatively, free flaps can be taken from close or remote areas. They are disconnected from their native blood supply and reconnected in the breast area via specialized microvascular techniques. The most commonly used example is the DIEP (deep inferior epigastric artery perforator) flap, which uses skin and subcutaneous tissue of the abdomen supplied by the DIEP blood vessels to create the breast mound. Common autologous breast reconstruction types are described in Table 5.
Figure 3.
Autologous breast reconstruction: A) and B) abdominal-based reconstruction; and C) latissimus dorsi reconstruction.
Table 4.
Advantages and disadvantages of autologous breast reconstruction: Pedicled versus free flap.
| AUTOLOGOUS BREAST RECONSTRUCTION | ADVANTAGES | DISADVANTAGES |
|---|---|---|
| Pedicled flap |
|
|
| Free flap |
|
|
TRAM—transverse rectus abdominis myocutaneous.
Table 5.
Common types of autologous (tissue-based) breast reconstruction
| TYPES | DEFINITION | IDEAL CANDIDATE |
|---|---|---|
| Pedicled flap | ||
|
|
|
|
|
|
| Free flap | ||
|
|
|
|
|
|
|
|
DIEP—deep inferior epigastric artery perforator, SGAP—superior gluteal artery perforator, TRAM—transverse rectus abdominis myocutaneous, TUG—transverse upper gracilis.
Autologous reconstruction involves longer surgery with donor- and recipient-site involvement. For this reason, return to sedentary activity (eg, walking or sitting for prolonged duration) is usually 2 weeks, but with restriction in many activities for up to 8 weeks. A hospital stay of 1 to 4 days is generally required.
Fat grafting in breast reconstruction: Autologous fat grafting (Figure 4) involves harvesting fat from a remote body area via liposuction followed by injection with small cannulas into the breast area. Most commonly, it is used for refinement and optimization, as an adjunct for both types of breast reconstruction,13 or to fill partial mastectomy defects.14 It is currently being used in select cases as the primary method for whole-breast reconstruction. As a filler material it is favourable owing to its availability, ease of harvest, and biocompatibility.13 The abundance of adipose-derived stem cells within the transferred fat also gives the fat great potential to repair breast tissues damaged from surgical trauma or radiation. This technique has extended the options of reconstruction in many patients who would have previously been poor candidates. It has been shown in many studies to be safe and compatible with surveillance imaging15 and it does not influence the risk of cancer recurrence.16,17
Figure 4.
Fat grafting for lumpectomy defect reconstruction
Lumpectomy defect reconstruction: As an alternative to mastectomy, many women undergo breast conservation therapy (BCT). Breast conservation therapy includes lumpectomy followed by radiation and provides equivalent long-term survival compared with mastectomy.18,19 While this approach leaves most of the breast intact, up to 40% of patients can have unsightly and deforming breast abnormalities following BCT.20–23 The new field of oncoplastic surgery combines the lumpectomy with immediate rearrangement of adjacent tissues to preserve the ideal breast shape. In many cases, the contralateral breast will be balanced at the same time through breast reduction or lift (Figure 5). Although possible through autologous fat grafting, transfer of autologous tissue flaps, or local tissue rearrangement,24 reconstructing these defects in a delayed manner is far more difficult. This highlights the need to consider plastic surgery involvement early in the decision to undergo BCT when a large defect is possible.
Figure 5.
Oncoplastic breast reduction
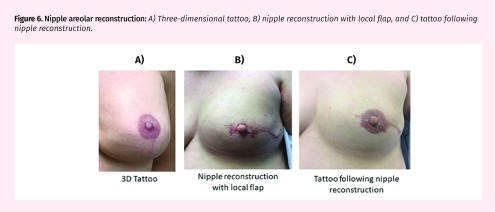
Nipple-areolar reconstruction: Reconstruction of the nipple-areolar complex (NAC) (Figure 6) is the last step of breast reconstruction and is usually undertaken when the breast mound has healed and settled in its final position. Restoration of the NAC includes reconstruction of the projecting nipple and pigmentation. For nipple reconstruction, local skin flaps can be designed and folded to produce a projecting nipple, a graft can be harvested from the contralateral nipple, or a 3-dimensional tattoo can be used to give the illusion of a projecting nipple. Pigmentation of the NAC can be obtained via tattoo or skin graft.25,26 Patients are generally very satisfied with NAC reconstruction, although a lack of long-term nipple projection is a common problem.27 These procedures are often completed under local anesthesia in an outpatient setting.
Figure 6.
Nipple areolar reconstruction: A) Three-dimensional tattoo, B) nipple reconstruction with local flap, and C) tattoo following nipple reconstruction.
Adjunct procedures: For many women, secondary procedures such as fat grafting, implant adjustments or replacements, or skin tightening procedures are required over time. In unilateral cases, balancing procedures such as contralateral breast reduction, augmentation, or mastopexy can be performed in the immediate or delayed setting to achieve appropriate symmetry.
Outcomes and complications
Outcomes: Many recent studies have looked at outcomes, complications, and satisfaction rates after breast reconstruction. Regardless of procedure type, most women find an improvement in quality of life and psychological and emotional well-being, with an improvement in body image, symmetry, and balance. Studies repeatedly demonstrate that, when asked, women who have undergone breast reconstruction indicate they would make the same decision again and would recommend reconstruction to a friend who was facing this decision.4–7
Complications: Complications specific to breast reconstruction depend on the reconstructive option chosen (Table 6).28 Complications of implant-based reconstruction include capsular contracture (hardening of the internal breast capsule), malposition (improper or changed positioning of the implant), implant rippling or edge visibility, and an unnatural look or feel. Complications more specific to autologous reconstruction include donor-site complications such as wound healing delay, abdominal bulge or hernia, and occasionally donor-site weakness. Difficulties in obtaining good shape, appropriate size, and good symmetry are problems with both implant- and tissue-based reconstruction.
Table 6.
Complications associated with breast reconstruction
| COMPLICATION | ALLOPLASTIC | AUTOLOGOUS |
|---|---|---|
| Surgical site infections | 0.37 times more likely | ... |
| Hematoma or seroma formation | 0.56 times more likely | ... |
| Skin or soft tissue necrosis | ... | 2.79 times more likely |
| Wound dehiscence | No difference | No difference |
| Reconstructive failure | 0.14 times more likely | ... |
| Deep vein thrombosis | No difference | No difference |
| Pulmonary embolism | No difference | No difference |
Data from Tsoi et al.28
Surveillance following breast reconstruction.
There are no data to support the value of routine screening mammography after mastectomy and reconstruction. Further, there are no data to suggest breast reconstruction hides local recurrence or affects survival.29,30 The goal of mastectomy is to remove all breast tissue, and if there is a small amount of residual breast tissue it is almost always under the breast skin. Therefore, local recurrences after mastectomy usually present as skin recurrence, as the skin is physically separated from the chest wall by breast reconstruction.31,32 Clinical examination of the chest wall and reconstructed breast can detect skin recurrences and should be performed during breast cancer survivorship follow-up appointments.29,33 Cancer Care Ontario recommends diagnostic imaging (such as mammography, ultrasound, and magnetic resonance imaging) primarily for reconstructed breasts of symptomatic patients.9,34
Funding.
In Canada, most provinces offer postmastectomy breast reconstruction coverage. Refer to the relevant schedule of benefits for more information.35–43
Patient education.
Many educational resources exist to help patients better understand their options for breast reconstruction. Online and print resources are available from the CCO44 and the Canadian Cancer Society45 web-sites. An international campaign for breast reconstruction awareness takes place on the third Wednesday of October every year. Additionally, BRA (Breast Reconstruction Awareness) Day events are an excellent resource for patients to learn about options and improve access to breast reconstruction. Education and event information are available online.46
Behavioural change.
Given that there are no absolute contraindications for breast reconstruction, surgical optimization can be achieved for women thinking about undergoing the procedure with the support of their PCPs. Strong examples in this realm include smoking cessation and weight loss.
Conclusion
All breast cancer patients should receive education about breast reconstruction as soon as operative management is considered, as reflected in CCO’s breast cancer treatment guidelines47 and other similar guidelines worldwide. Currently, many effective options are available for breast reconstruction, making virtually all cancer patients candidates. These include both implant-based and tissue-based options that each can be performed in either the immediate or the delayed setting.
While some women will choose not to undergo breast reconstruction, all women should receive the appropriate education and support to allow for informed decision making. The PCP remains one of the most valuable resources for women embarking on the breast cancer treatment journey. As such, it is important to stay up to date on the options available to these women.
Editor’s key points
▸ Breast cancer continues to be the most common form of cancer affecting women in Canada (1 in 9 women), but diagnostic and treatment improvements have increased survival to 87%. Breast reconstruction can improve quality of life for patients who undergo mastectomy, but rates of reconstruction in Canada continue to be low. Many effective options are available for reconstruction, making almost all patients who require mastectomy candidates.
▸ Cancer Care Ontario recommends that all women diagnosed with operable breast cancer requiring mastectomy be referred to a plastic surgeon to discuss reconstructive options before their scheduled mastectomies.
▸ This article outlines the options for reconstruction, outcomes, and complications, and provides guidance that can be used to help patients decide among the various options. While some women will choose not to undergo breast reconstruction, all women should receive the appropriate education and support to allow for informed decision making.
Footnotes
Contributors
All authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de juin 2018 à la page e255.
References
- 1.Canadian Cancer Society . Breast cancer in Canada, 2016. Toronto, ON: Canadian Cancer Society; 2017. Available from: www.cbcf.org/ontario/AboutBreastCancerMain/FactsStats/Pages/Breast-Cancer-Canada.aspx. Accessed 2017 Mar 1. [Google Scholar]
- 2.Canadian Cancer Society . Breast cancer statistics. Toronto, ON: Canadian Cancer Society; Available from: www.cancer.ca/en/cancer-information/cancer-type/breast/statistics/?region=bc. Accessed 2015 Oct 1. [Google Scholar]
- 3.Halls S. Breast cancer incidence and mortality rates worldwide: Canada, U.K., U.S.A. Camrose, AB: Moose & Doc Breast Cancer; 2017. Available from: breast-cancer.ca/mortratings. Accessed 2017 Mar 1. [Google Scholar]
- 4.Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer. 2000;36(15):1938–43. doi: 10.1016/s0959-8049(00)00197-0. [DOI] [PubMed] [Google Scholar]
- 5.Serletti JM, Fosnot J, Nelson JA, Disa JJ, Bucky LP. Breast reconstruction after breast cancer. Plast Reconstr Surg. 2011;127(6):124e–35e. doi: 10.1097/PRS.0b013e318213a2e6. [DOI] [PubMed] [Google Scholar]
- 6.Baildam AD. Oncoplastic surgery for breast cancer. Br J Surg. 2008;95(1):4–5. doi: 10.1002/bjs.6098. [DOI] [PubMed] [Google Scholar]
- 7.Schain WS. Breast reconstruction. Update of psychosocial and pragmatic concerns. Cancer. 1991;68(5 Suppl):1170–5. doi: 10.1002/1097-0142(19910901)68:5+<1170::aid-cncr2820681309>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 8.Zhong T, Fernandes KA, Saskin R, Sutradhar R, Platt J, Beber BA, et al. Barriers to immediate breast reconstruction in the Canadian universal health care system. J Clin Oncol. 2014;32(20):2133–41. doi: 10.1200/JCO.2013.53.0774. [DOI] [PubMed] [Google Scholar]
- 9.Cancer Care Ontario . Breast cancer treatment pathway map. Version 2015.11. Toronto, ON: Cancer Care Ontario; 2015. Available from: www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=349036. Accessed 2016 Sep 1. [Google Scholar]
- 10.Mendelson BC, Woods JE. Breast reconstruction after mastectomy. Aust Fam Physician. 1979;8(6):646–7. 651–3. [PubMed] [Google Scholar]
- 11.Platt J, Baxter N, Zhong T. Breast reconstruction after mastectomy for breast cancer. CMAJ. 2011;183(18):2109–16. doi: 10.1503/cmaj.110513. Epub 2011 Nov 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Clearinghouse of Plastic Surgery Procedural Statistics . 2014 Plastic surgery statistics report. Arlington Heights, IL: American Society of Plastic Surgeons; 2015. Available from: https://www.plasticsurgery.org/documents/News/Statistics/2014/plastic-surgery-statistics-full-report-2014.pdf. Accessed 2018 Apr 23. [Google Scholar]
- 13.Gabriel A, Champaneria MC, Maxwell GP. Fat grafting and breast reconstruction: tips for ensuring predictability. Gland Surg. 2015;4(3):232–43. doi: 10.3978/j.issn.2227-684X.2015.04.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoy E. State of the art: reconstructing partial mastectomy defects with autologous fat grafting. Del Med J. 2016;88(1):20–3. [PubMed] [Google Scholar]
- 15.Lindegren A, Chantereau MW, Bygdeson M, Azavedo W, Schultz I. Autologous fat transplantation to the reconstructed breast does not hinder assessment of mammography and ultrasound: a cohort study. World J Surg. 2016;40(5):1104–11. doi: 10.1007/s00268-015-3385-x. [DOI] [PubMed] [Google Scholar]
- 16.Silva-Vergara C, Fontdevila J, Descarrega J, Burdio F, Yoon TS, Grande L. Oncological outcomes of lipofilling breast reconstruction: 195 consecutive cases and literature review. J Plast Reconstr Aesthet Surg. 2016;69(4):475–81. doi: 10.1016/j.bjps.2015.12.029. Epub 2016 Feb 3. [DOI] [PubMed] [Google Scholar]
- 17.Kronowitz SJ, Lam C, Terefe W, Hunt KK, Kuerer HM, Valero V, et al. A multidisciplinary protocol for planned skin-preserving delayed breast reconstruction for patients with locally advanced breast cancer requiring postmastectomy radiation therapy: 3-year follow-up. Plast Reconstr Surg. 2011;127(6):2154–66. doi: 10.1097/PRS.0b013e3182131b8e. [DOI] [PubMed] [Google Scholar]
- 18.Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–32. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 19.Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 20.Al-Ghazal SK, Fallowfield L, Blamey RW. Does cosmetic outcome from treatment of primary breast cancer influence psychosocial morbidity? Eur J Surg Oncol. 1999;25(6):571–3. doi: 10.1053/ejso.1999.0708. [DOI] [PubMed] [Google Scholar]
- 21.Curran D, van Dongen JP, Aaronson NK, Kiebert G, Fentiman IS, Mignolet F, et al. Quality of life of early-stage breast cancer patients treated with radical mastectomy or breast-conserving procedures: results of EORTC Trial 10801. Eur J Cancer. 1998;34(3):307–14. doi: 10.1016/s0959-8049(97)00312-2. [DOI] [PubMed] [Google Scholar]
- 22.Sneeuw KC, Aaronson NK, Yarnold JR, Broderick M, Regan J, Ross G, et al. Cosmetic and functional outcomes of breast conserving treatment for early stage breast cancer. 2. Relationship with psychosocial functioning. Radiother Oncol. 1992;25(3):160–6. doi: 10.1016/0167-8140(92)90262-s. [DOI] [PubMed] [Google Scholar]
- 23.Waljee JF, Hu ES, Ubel PA, Smith DM, Newman LA, Alderman AK. Effect of esthetic outcome after breast-conserving surgery on psychosocial functioning and quality of life. J Clin Oncol. 2008;26(20):3331–7. doi: 10.1200/JCO.2007.13.1375. [DOI] [PubMed] [Google Scholar]
- 24.Loskem A, Pinell-White X, Hodges M, Egro FM. Evaluating outcomes after correction of the breast conservation therapy deformity. Ann Plast Surg. 2015;74(Suppl 4):S209–13. doi: 10.1097/SAP.0000000000000443. [DOI] [PubMed] [Google Scholar]
- 25.Liliav B, Loeb J, Hassid VJ, Antony AK. Single-stage nipple-areolar complex reconstruction technique, outcomes, and patient satisfaction. Ann Plast Surg. 2014;73(5):492–7. doi: 10.1097/SAP.0b013e318276dac0. [DOI] [PubMed] [Google Scholar]
- 26.Farhadi J, Maksvytyte GK, Schaefer DJ, Pierer G, Scheufler O. Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg. 2006;59(1):40–53. doi: 10.1016/j.bjps.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Goh SCJ, Martin NA, Pandya AN, Cutress RI. Patient satisfaction following nipple-areolar complex reconstruction and tattooing. J Plast Reconstr Aesthet Surg. 2011;64(3):360–3. doi: 10.1016/j.bjps.2010.05.010. Epub 2010 Jun 8. [DOI] [PubMed] [Google Scholar]
- 28.Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O’Reilly D, Goeree R. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg. 2014;133(2):234–49. doi: 10.1097/01.prs.0000436847.94408.11. [DOI] [PubMed] [Google Scholar]
- 29.Sim YT, Literland JC. The use of imaging in patients post breast reconstruction. Clin Radio. 2012;67(2):128–33. doi: 10.1016/j.crad.2011.07.050. Epub 2011 Sep 10. [DOI] [PubMed] [Google Scholar]
- 30.Zakhireh J, Fowbie B, Esserman LJ. Application of screening principles to the reconstructed breast. J Clin Oncol. 2010;28(1):173–80. doi: 10.1200/JCO.2008.21.7588. Epub 2009 Nov 2. [DOI] [PubMed] [Google Scholar]
- 31.Slavin SA, Love SM, Goldwyn RM. Recurrent breast cancer following immediate reconstruction with myocutaneous flaps. Plast Reconstr Surg. 1994;93(6):1191–204. doi: 10.1097/00006534-199405000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Kroll SS, Khoo A, Singletary SE, Ames FC, Wang BG, Reece GP, et al. Local recurrence risk after skin-sparing and conventional mastectomy: a 6 year follow up. Plast Reconstr Surg. 1999;104(2):421–5. doi: 10.1097/00006534-199908000-00015. [DOI] [PubMed] [Google Scholar]
- 33.Barnsley GP, Grunfeld E, Coyle D, Paszat L. Surveillance mammography following the treatment of primary breast cancer with breast reconstruction: a systematic review. Plast Reconstr Surg. 2007;120(5):1125–32. doi: 10.1097/01.prs.0000279143.66781.9a. [DOI] [PubMed] [Google Scholar]
- 34.Zhong T, Spithoff K, Kellett S, Boyd K, Brackstone M, Hanrahan R, et al. Breast cancer reconstruction surgery (immediate and delayed) across Ontario: patient indications and appropriate surgical options. Toronto, ON: Cancer Care Ontario; 2016. Available from: https://www.cancercareontario.ca/en/guidelines-advice/types-of-cancer/31721. Accessed 2018 Apr 25. [Google Scholar]
- 35.Medical Services Plan . MSC payment schedule index. Victoria, BC: Government of British Columbia; Available from: https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/medical-services-plan/msc-payment-schedule-december-2017.pdf. Accessed 2018 May 4. [Google Scholar]
- 36.Alberta Health . Schedule of medical benefits effective April 1, 2017. Edmonton, AB: Alberta Health; 2017. Available from: www.health.alberta.ca/professionals/SOMB.html. Accessed 2018 Apr 23. [Google Scholar]
- 37.Government of Saskatchewan . Payment schedules. Regina, SK: Government of Saskatchewan; Available from: www.saskatchewan.ca/government/health-care-administration-and-provider-resources/resources-for-health-care-businesses-and-career-development/physician-career-resources#physician-payment-schedules-newsletters-and-bulletins. Accessed 2016 Sep 9. [Google Scholar]
- 38.Manitoba Minister of Health . Manitoba physician’s manual. Winnipeg, MB: Government of Manitoba; 2018. Available from: www.gov.mb.ca/health/documents/physmanual.pdf. Accessed 2018 Apr 23. [Google Scholar]
- 39.Ontario Ministry of Health and Long-Term Care . Schedule of benefits. Physician services under the Health Insurance Act. Toronto, ON: Ontario Ministry of Health and Long-Term Care; 2015. Available from: www.health.gov.on.ca/english/providers/program/ohip/sob/physserv/sob_master20160406.pdf. Accessed 2016 Sep 9. [Google Scholar]
- 40.Régie de l’assurance maladie du Québec . Health insurance. Quebec city, QC: Régie de l’assurance maladie du Québec; Available from: www.ramq.gouv.qc.ca/en/citizens/health-insurance/healthcare/Pages/fees-billed-physician.aspx. Accessed 2016 Sep 9. [Google Scholar]
- 41.Government of New Brunswick . New Brunswick physicians’ manual. Fredericton, NB: Government of New Brunswick; 2015. Available from: www.gnb.ca/0394/pdf/2015/physician_manual-e.pdf. Accessed 2016 Sep 9. [Google Scholar]
- 42.Nova Scotia Medical Services Insurance . Physician’s manual. Halifax, NS: Nova Scotia Medical Services Insurance; 2014. Available from: www.medavie.bluecross.ca/static/MSI/PhysicianManual.pdf. Accessed 2016 Sep 9. [Google Scholar]
- 43.Newfoundland and Labrador Medical Care Plan . Medical payment schedule. St John’s, NL: Newfoundland and Labrador Medical Care Plan, Department of Health and Community Services; 2013. Available from: www.health.gov.nl.ca/health/mcp/providers/Full_MCP_Payment_Schedule-03_13_14.pdf. Accessed 2016 Sep 9. [Google Scholar]
- 44.Cancer Care Ontario . Recommended resources for patients and families. Toronto, ON: Cancer Care Ontario; Available from: https://www.cancercareontario.ca/en/resources-patients-and-families. Accessed 2018 Apr 25. [Google Scholar]
- 45.Canadian Cancer Society [website] What is breast cancer? Toronto, ON: Canadian Cancer Society; 2017. Available from: www.cancer.ca/en/cancer-information/cancer-type/breast/breast-cancer/?region=on. Accessed 2017 Mar 9. [Google Scholar]
- 46.Breast Reconstruction Awareness Day [website] Toronto, ON: Canadian Cancer Society; Available from: www.bra-day.com. Accessed 2017 Mar 9. [Google Scholar]
- 47.Cancer Care Ontario . Guidelines & advice. Breast cancer. Toronto, ON: Cancer Care Ontario; 2017. Available from: https://www.cancercare.on.ca/toolbox/qualityguidelines/diseasesite/breast-ebs/. Accessed 2017 Mar 9. [Google Scholar]