Abstract
Introduction and objectives:
Understanding the details of one individual's experience with pain, opioid use and withdrawal may generate insights into possible relationships between opioid-induced hyperalgesia and withdrawal-associated injury site pain (WISP).
Methods:
This case study was extracted from a mixed methods study that characterized WISP. In 2014, the individual was recruited from a primary care clinic that prescribes opioid agonist therapy. In an interview, she completed a 35-item survey and elaborated on her own experience. Follow-up contact was made in June of 2017.
Results:
This 34-year-old white woman had several twisting injuries of her right knee between ages 13 and 15. The pain resolved each time in a few days, and she was pain free for 15 years. Around age 30, she initiated illicit oxycodone recreationally (not for pain) and developed an opioid use disorder. On detoxification, she experienced severe knee pain for 6 weeks that resolved postdetoxification but returned after subsequent oxycodone use and withdrawal episodes along with generalized skin sensitivity. This experience of WISP became a barrier to opioid cessation. Although nonsteroidal anti-inflammatories and gabapentin relieved WISP and methadone therapy assisted her opioid use disorder, an eventual change to sublingual buprenorphine/naloxone provided superior control of both.
Conclusion:
This case report illustrates that both opioid use and withdrawal can reactivate injury site pain, which can increase with dose escalation and repeated withdrawal events. The timing, trajectory, and neuropathic features of WISP reported here are consistent with those previously reported for the development of opioid-induced hyperalgesia, possibly linking these phenomena.
Keywords: Opioids, Drug dependence, Pain, Hyperalgesia, Withdrawal syndrome
1. Introduction
As the opioid crisis continues in North America, clinicians and researchers need to understand factors that perpetuate opioid use and barriers to detoxification.2,4,19,32,33 There is a growing body of evidence that opioids can provide a pronociceptive force both centrally and peripherally, resulting in opioid-induced hyperalgesia (OIH).13,20,21,28 When regular opioid use is stopped, some people experience a temporary return of pain at old healed injury sites, a phenomenon that we have documented and termed withdrawal-associated injury site pain (WISP).27 The current case study is the first to detail one individual's pain experience with opioid use and withdrawal to shed light on the possible relationship between OIH and WISP, as well as to provide a case example to assist in the identification of this phenomenon.
2. Methods
This case study was extracted from our mixed methods study that characterized WISP.27 The participant was recruited in 2014 from a primary care clinic providing methadone treatment in Vancouver, Canada. She provided written informed consent. She screened positive for WISP as per the published protocol and completed the 35-question survey as well as elaborated on her own experience in an in-depth interview, which was recorded and transcribed. The initial study protocol was approved by the Behavioral Research Ethics Board at the University of British Columbia and the Vancouver Coastal Health Research Ethics Board. In June of 2017, the participant was contacted again. She endorsed a draft of this case report provided to her, and through email and text provided a brief update of her pain and treatment experience in the intervening 3 years.
3. Results
A 34-year-old white woman (pseudonym “Alice”) reported experiencing several twisting injuries of her right knee playing sports between the ages of 12 and 15. The original injury site pain (recalled as 4/10 on a 0–10 scale) associated with these injuries resolved in 2 to 3 days each time. She reported no knee pain, although an occasional click, for the subsequent 15 years and was medication free. At age 30, Alice began insufflating illicit oxycodone recreationally (not for pain) and developed an opioid use disorder (OUD).
In 2012, at age 32, she abruptly stopped the use of oxycodone 150 mg/d, morphine equivalent daily dose (MEDD) 225 mg (1:1.5 oral dose conversion chosen because of conflicting information regarding intranasal bioavailability).18,22,30 Alice reported experiencing moderate generalized withdrawal symptoms along with severe right knee pain (ie, WISP intensity 8/10 for 30 days, then 4/10 for 15 days). Subsequently, she reported being pain free for 7 months while opioid abstinent. Alice then reinitiated oxycodone insufflation and found that her right knee pain returned. She perceived escalation of injury site pain as her dose of opioids increased and attributed the etiology of the pain to a presumed chronic knee problem but wondered whether oxycodone was playing a role. Notably, each subsequent attempt at opioid cessation produced even greater right knee WISP (intensity 10/10) and generalized skin sensitivity, towards which she developed fear and aversion. By contrast, opioid withdrawal pain in the contralateral knee was mild (intensity 2/10) and not always present when opioids were stopped.
Alice cited WISP as a barrier to detoxification and opioid cessation. Despite many attempts at opioid cessation in the previous 2 years, she was able to go beyond the full 6 weeks of WISP symptoms only 3 times. On each of these 3 occasions, her right knee pain resolved completely. General withdrawal symptoms were a contributor to reinitiation of opioid use but were typically less intense (4/10) and somewhat shorter than WISP (30 days).
Alice reported that naproxen, ibuprofen, gabapentin, acetaminophen, and phenobarbital all diminished WISP somewhat during acute detoxification. She eventually tried detoxification with prescribed methadone (ie, 30-mg initial dose, then tapered by 5 mg/d), which eased WISP compared with withdrawal with no medication. At the time of the initial interview in 2014 at age 34, she was embarking on methadone maintenance treatment and had recently achieved a dose of 85 mg/d. Yet, she continued to use oxycodone for knee pain approximately 20 to 40 mg/d, ostensibly until her methadone dose could be further increased. At that point, the MEDD was 436 mg (1:4.6 conversion methadone to morphine and 1:1.5 oxycodone to morphine).22
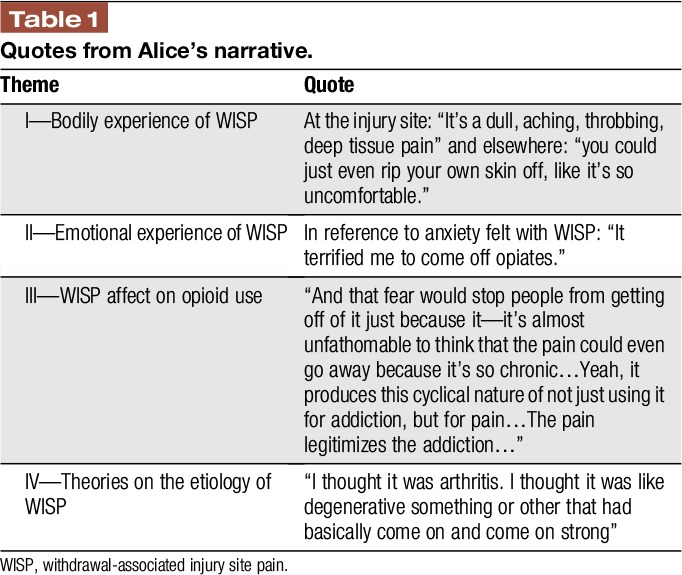
Alice's key individual quotes related to her clinical presentation are found in Table 1.
Table 1.
Quotes from Alice's narrative.
In follow-up at age 37, Alice related that her methadone had gone as high as 200 mg per day in the past year (MEDD 920 mg).22 Although methadone had helped her not use illicit opioids, it had been overly sedating and never managed her knee pain well. So, in the previous months, she had tapered down on methadone to 30 mg/d (MEDD 138 mg) and then switched over to sublingual buprenorphine/naloxone (although did not state her dose). Alice reported feeling very well on this medication; she had no drug cravings, was clear minded, and had no knee pain. Alice had never heard of nor been offered naltrexone.
Alice recognized that knowledge of WISP might have helped her. She said “I think it would have made it a lot easier… [knowing] that it'll actually go away.”
4. Discussion
This case study illustrates that both opioid use and withdrawal can activate old healed injury site pain, which can increase with dose escalation and repeated withdrawal events. The timing and trajectory of WISP in this case is consistent with those of the development and resolution of OIH, which has also been shown to be both opioid dose dependent and withdrawal episode dependent.6,12,14,15 Also, the pronociceptive changes that occur in OIH combined with catecholamine release and other factors has been linked with withdrawal-induced hyperalgesia, which in turn has been shown to last weeks to months in those with OUDs or on long-term opioid therapy for chronic noncancer pain.5,26,31,34 For Alice, she displayed generalized skin sensitivity, indicating she may have developed OIH revealed during withdrawal because allodynia can comanifest with hyperalgesia. It is possible that this pain-sensitive state then uncovered peripheral or central sensitization that resulted from the original injury but was quiescent under normal circumstances.27,35 Given that Alice experienced occasional clicking in her knee, it is possible that she had underlying pathology that was pain free under normal circumstances.
Perceived intensity and emotional fear of WISP acted as a barrier to opioid detoxification for Alice. This is in keeping with other studies showing that anxiety and fear can influence inflammation and pain perception.23,29
Alice initially presumed that she had a chronic pain condition, when instead she had WISP and opioid lowering, detoxification or rotation was needed for the pain to resolve, as can be the case in OIH.1,3,20 Nonsteroidal anti-inflammatories and gabapentin were among the medications that subjectively helped relieve her symptoms of WISP consistent with medications found to relieve WISP and OIH in other studies.1,3,8,27 Pain during and immediately after opioid detoxification has been shown by other authors to be a risk factor for reinitiation of opioid use.24
At the time of the first interview, Alice had decided to initiate methadone treatment, which has been shown to be equally efficacious to buprenorphine/naltrexone in the treatment of OUD in noninjection opioid analgesia users.25 Despite methadone being a racemic mixture in which one enantiomer is a mu opioid receptor agonist and one an NMDAr antagonist, OIH can still develop.7 Interestingly, a high proportion of people with OUDs report having what they presume is chronic pain, even after conversion to methadone.7,10,11 Ultimately for Alice, the methadone could not control her right knee pain, although helped her OUD. In her view, Alice benefitted from once daily oral buprenorphine/naloxone therapy. Both her pain and her addiction were managed. This is consistent with another study showing a fifty percent drop in pain when converted from high-dose pharmaceutical grade opioids to buprenorphine, but is in contrast to a report of patients with previous heroin use still displaying OIH on buprenorphine.7,9 One is patient self-report, and the other an experimentally elicited response, which may account for the difference.
Alice had never been offered naltrexone, which is a reminder for clinicians to discuss all medication options with patients. Naltrexone is an antagonist at both mu opioid receptor and toll-like receptor 4 on microglial cells, which shows mixed results in preclinical trials to treat OIH, as well as being a treatment for OUD.1,16,17
Limitations of this study include Alice's omission of her buprenorphine/naloxone dose for comparison. Also, it is unknown if Alice may build symptoms of OIH and WISP overtime on buprenorphine/naloxone.
5. Conclusion
We present the first detailed description of a case in which both opioid use and withdrawal could reactivate injury site pain. This woman's experience illustrates that the timing, trajectory, and neuropathic features of WISP reported here are consistent with those previously reported for the development and resolution of OIH, possibly linking these phenomena.
Disclosures
The authors have no conflict of interest to declare.
L.M. Rieb received funding through the Clinical Scholars Program, Department of Family Practice, University of British Columbia, and the College of Family Physicians of BC and was supported by a US National Institute of Drug Abuse (NIDA) sponsored Canadian Addiction Medicine Research Fellowship through St. Paul's Hospital (R25 DA037756-02). W.V. Norman is supported with a Chair in Applied Public Health Research from the Canadian Institutes for Health Research (CIHR) and the Public Health Agency of Canada (CPP137903) and as a Scholar of the Michael Smith Foundation for Health Research (MSFHR). E. Wood is supported in part by a Tier 1 Canada Research Chair in Inner-City Medicine award. M.-J. Milloy is supported in part by the United States National Institutes of Health (R01-DA051525) and from the University of British Columbia by an unstructured gift from NG Biomed. R. McNeil is supported by a Canadian Institutes of Health Research New Investigator Award and Michael Smith Foundation for Health Research Scholar Award, as well as funding from the United States National Institutes of Health (NIH, R01DA044181). M.-J. Milloy is supported in part by the NIH (U01-DA021525), a Scholar Award from MSFHR and a New Investigator award from CIHR. The funders had no role in the design and conduct of this study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
M.-J. Milloy's institution has received an unstructured gift from NG Biomed Ltd, a private firm seeking a licence to produce medical cannabis, to support him.
Acknowledgements
The authors thank the study participant for her contribution to the research.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
References
- [1].Arout CA, Edens E, Petrakis IL, Sofuoglu M. Targeting opioid-induced hyperalgesia in clinical treatment: neurobiological considerations. CNS Drugs 2015;29:465–86. [DOI] [PubMed] [Google Scholar]
- [2].Ballantyne JC. Opioid therapy in chronic pain. Phys Med Rehabil Clin N Am 2015;26:201–18. [DOI] [PubMed] [Google Scholar]
- [3].Bannister K. Opioid-induced hyperalgesia: where are we now? Curr 2015;9:116–21. [DOI] [PubMed] [Google Scholar]
- [4].Berna C, Kulich RJ, Rathmell JP. Tapering long-term opioid therapy in chronic noncancer pain: evidence and recommendations for everyday practice. Mayo Clinic Proc 2015;90:828–42. [DOI] [PubMed] [Google Scholar]
- [5].Bie B, Fields HL, Williams JT, Pan ZZ. Roles of alpha1- and alpha2-adrenoceptors in the nucleus raphe magnus in opioid analgesia and opioid abstinence-induced hyperalgesia. J Neurosci 2003;23:7950–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Celerier E, Laulin JP, Corcuff JB, Le Moal M, Simonnet G. Progressive enhancement of delayed hyperalgesia induced by repeated heroin administration: a sensitization process. J Neurosci 2001;21:4074–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Compton P, Canamar CP, Hillhouse M, Ling W. Hyperalgesia in heroin dependent patients and the effects of opioid substitution therapy. J Pain 2012;13:401–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Compton P, Kehoe P, Sinha K, Torrington MA, Ling W. Gabapentin improves cold-pressor pain responses in methadone-maintained patients. Drug Alcohol Depend 2010;109:213–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Daitch D, Daitch J, Novinson D, Frey M, Mitnick C, Pergolizzi J. Conversion from high-dose full-opioid agonists to sublingual buprenorphine reduces pain scores and improves quality of life for chronic pain patients. Pain Med 2014;15:2087–94. [DOI] [PubMed] [Google Scholar]
- [10].Dennis BB, Bawor M, Naji L, Chan CK, Varenbut J, Paul J, Varenbut M, Daiter J, Plater C, Pare G, Marsh DC, Worster A, Desai D, Thabane L, Samaan Z. Impact of chronic pain on treatment prognosis for patients with opioid use disorder: a systematic review and meta-analysis. Subst Abuse 2015;9:59–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dennis BB, Samaan MC, Bawor M, Paul J, Plater C, Pare G, Worster A, Varenbut M, Daiter J, Marsh DC, Desai D, Thabane L, Samaan Z. Evaluation of clinical and inflammatory profile in opioid addiction patients with comorbid pain: results from a multicenter investigation. Neuropsychiatr Dis Treat 2014;10:2239–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dunbar SA, Pulai IJ. Repetitive opioid abstinence causes progressive hyperalgesia sensitive to N-methyl-D-aspartate receptor blockade in the rat. J Pharmacol Exp Ther 1998;284:678–86. [PubMed] [Google Scholar]
- [13].Grace PM, Hutchinson MR, Maier SF, Watkins LR. Pathological pain and the neuroimmune interface. Nat Rev Immunol 2014;14:217–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hooten WM, Lamer TJ, Twyner C. Opioid-induced hyperalgesia in community-dwelling adults with chronic pain. PAIN 2015;156:1145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hooten WM, Mantilla CB, Sandroni P, Townsend CO. Associations between heat pain perception and opioid dose among patients with chronic pain undergoing opioid tapering. Pain Med 2010;11:1587–98. [DOI] [PubMed] [Google Scholar]
- [16].Hutchinson MR, Bland ST, Johnson KW, Rice KC, Maier SF, Watkins LR. Opioid-induced glial activation: mechanisms of activation and implications for opioid analgesia, dependence, and reward. ScientificWorldJournal 2007;7:98–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lee JD, Friedmann PD, Kinlock TW, Nunes EV, Boney TY, Hoskinson RA, Jr, Wilson D, McDonald R, Rotrosen J, Gourevitch MN, Gordon M, Fishman M, Chen DT, Bonnie RJ, Cornish JW, Murphy SM, O'Brien CP. Extended-release naltrexone to prevent opioid relapse in criminal justice offenders. N Engl J Med 2016;374:1232–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lofwall MR, Moody DE, Fang WB, Nuzzo PA, Walsh SL. Pharmacokinetics of intranasal crushed OxyContin and intravenous oxycodone in nondependent prescription opioid abusers. J Clin Pharmacol 2012;52:600–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Manchikanti L, Helm S, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States. Pain Physician 2012;15:ES9–38. [PubMed] [Google Scholar]
- [20].Mao J. Opioid-induced abnormal pain sensitivity: implications in clinical opioid therapy. PAIN 2002;100:213–17. [DOI] [PubMed] [Google Scholar]
- [21].Mao J. Opioid-induced abnormal pain sensitivity. Curr Pain Headache Rep 2006;10:67–70. [DOI] [PubMed] [Google Scholar]
- [22].Nielsen S, Degenhardt L, Hoban B, Gisev N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf 2016;25:733–7. [DOI] [PubMed] [Google Scholar]
- [23].Pongratz G, Straub RH. The sympathetic nervous response in inflammation. Arthritis Res Ther 2014;16:504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Potter JS, Chakrabarti A, Domier CP, Hillhouse MP, Weiss RD, Ling W. Pain and continued opioid use in individuals receiving buprenorphine-naloxone for opioid detoxification: secondary analyses from the Clinical Trials Network. J Subst Abuse Treat 2010;38:S80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Potter JS, Marino EN, Hillhouse MP, Nielsen S, Wiest K, Canamar CP, Martin JA, Ang A, Baker R, Saxon AJ, Ling W. Buprenorphine/naloxone and methadone maintenance treatment outcomes for opioid analgesic, heroin, and combined users: findings from starting treatment with agonist replacement therapies (START). J Stud Alcohol Drugs 2013;74:605–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Prosser JM, Steinfeld M, Cohen LJ, Derbyshire S, Eisenberg DP, Cruciani RA, Galynker II. Abnormal heat and pain perception in remitted heroin dependence months after detoxification from methadone-maintenance. Drug Alcohol Depend 2008;95:237–44. [DOI] [PubMed] [Google Scholar]
- [27].Rieb LM, Norman WV, Martin RE, Berkowitz J, Wood E, McNeil R, Milloy MJ. Withdrawal-associated injury site pain (WISP): a descriptive case series of an opioid cessation phenomenon. PAIN 2016;157:2865–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Rivat C, Ballantyne J. The dark side of opioids in pain management: basic science explains clinical observation. Pain Rep 2016;1:e570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Salim S, Chugh G, Asghar M. Inflammation in anxiety. Adv Protein Chem Struct Biol 2012;88:1–25. [DOI] [PubMed] [Google Scholar]
- [30].Takala A, Kaasalainen V, Seppala T, Kalso E, Olkkola KT. Pharmacokinetic comparison of intravenous and intranasal administration of oxycodone. Acta Anaesthesiologica Scand 1997;41:309–12. [DOI] [PubMed] [Google Scholar]
- [31].Treister R, Eisenberg E, Lawental E, Pud D. Is opioid-induced hyperalgesia reversible? A study on active and former opioid addicts and drug naive controls. J Opioid Manag 2012;8:343–9. [DOI] [PubMed] [Google Scholar]
- [32].United Nations Office on Drugs and Crime. World Drug Report 2017. ISBN: 978-92-1-148291-1, eISBN: 978-92-1-060623-3, United Nations Pubilication, Sales No. E.17.XI.6.
- [33].Volkow ND, McLellan AT. Opioid Abuse in chronic pain–misconceptions and mitigation strategies. N Engl J Med 2016;374:1253–63. [DOI] [PubMed] [Google Scholar]
- [34].Wang H, Akbar M, Weinsheimer N, Gantz S, Schiltenwolf M. Longitudinal observation of changes in pain sensitivity during opioid tapering in patients with chronic low-back pain. Pain Med 2011;12:1720–6. [DOI] [PubMed] [Google Scholar]
- [35].Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. PAIN 2011;152:S2–15. [DOI] [PMC free article] [PubMed] [Google Scholar]


