Abstract
Background:
Two-stage tissue expander (TE)/permanent implant (PI) breast reconstruction remains the most commonly performed technique in breast reconstruction. Predictions for the PI size preoperatively impact on the number and range of implants made available at TE exchange. This study aims to identify critical preoperative variables and create a predictive model for PI size.
Methods:
Patients who underwent 2-stage implant breast reconstruction from 2011 to 2017 were included in the study. Linear and multivariate regression analyses were used to identify significant preoperative variables for PI volume.
Results:
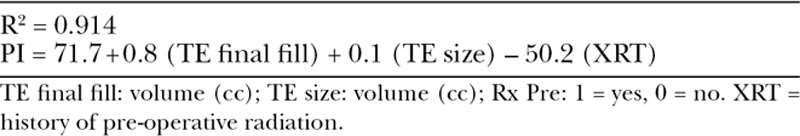
During the study period, 826 patients underwent 2-stage TE/PI breast reconstruction. Complete records were available for 226 breasts. Initial TE fill ranged from 0% to 102% with a mean final fill of 100.6% of TE volume. The majority of PIs were smooth round (98.2%), silicone (90%) implants. In a multivariate analysis, significant variables for predicting PI size were TE final fill volume (P < 0.0001), TE size (P = 0.03), and a history of preoperative radiation (P = 0.001). Relationships between these 3 variables were utilized to form a predictive model with a regression coefficient of R2 = 0.914.
Conclusions:
Significant variables for predicting PI volume were TE final fill volume, TE size, and a history of preoperative radiation. The ability to more accurately predict the PI volume can improve surgical planning, reduce consignment inventory, and simplify operating room workflow.
INTRODUCTION
Over 100,000 breast reconstructions are performed annually in the United States.1 Both the extirpative and reconstructive options for breast cancer have had technical advances, with 2-stage tissue expander (TE)/permanent implant (PI) breast reconstruction remaining the most commonly performed technique.2,3
First introduced by Radovan,4 TEs have undergone multiple modifications in design and technique. Major design changes have included an incorporated filling port within the expander, tabs to secure the expander, a textured surface, a modified shape to preferentially expand the inferior pole, acellular dermal matrix, and most recently a carbon dioxide–based, injection-free expansion.
Representing 72% of all breast reconstruction cases in 2016 alone, 2-stage implant reconstruction remains the most popular technique.2,3 Financially, breast reconstruction with TEs accounts for 45% of total care costs for all types of breast reconstruction according to some analyses.5 Determining the appropriate PI size during TE exchange is a multifactorial decision that depends on TE size, type and fill, skin envelope quality, patient preference, and surgeon judgment.
While 1–2 PIs are used for a unilateral or bilateral case, multiple PIs of varying type with accompanying implant sizers are ordered for a TE exchange surgery. The perioperative management of ordering, storing, tracking, and returning unused implants can deplete precious operating room storage space, complicate purchase order financial transactions, and create an inefficient workflow contributing to increased indirect costs.
Well-known predictive algorithms have been described for breast augmentation, and accurate volume analysis techniques are utilized for breast reduction.6–8 Developing a predictive model for PI size during TE exchange can simplify workflow and reduce the overall costs of breast reconstruction. This study retrospectively reviewed our experience at a large academic center with 2-stage implant breast reconstruction to identify the significant preoperative reconstructive variables when determining PI size.
PATIENTS AND METHODS
All patients who underwent mastectomy and 2-stage TE/PI breast reconstruction at Yale New Haven Hospital from 2011 to 2017 were included in the study. Medical records were reviewed retrospectively with approval from the institutional review board. Patients with incomplete medical records were excluded from the study. Patient demographics, medical history, surgical history, history of radiotherapy, operative details, and reconstructive outcomes were recorded.
After the mastectomy was performed by the breast surgeon, a TE was placed in a partial or complete submuscular plane.
TE size and profile were chosen based on preoperative base diameter measurement and final mastectomy weight. A TE size that matched the mastectomy weight was usually utilized unless there was an alternative patient preference. Postoperative drains were placed in all cases and maintained until 24-hour drain outputs were appropriately low. Patients returned for routine saline TE fills. Final TE fill volume and the size, type, and profile of the PI were a result of discussions between the patient and plastic surgeon.
Patient characteristics were compared with descriptive statistics. Linear regression and multivariate analyses between final TE fill volume and PI size were performed while correcting for body mass index (BMI), breast cup size, surgeon, type of mastectomy, mastectomy weight, TE size, TE projection, presence of acellular dermal matrix (ADM), preoperative radiation, postoperative radiation, implant projection, and PI fill material.
Statistical significance was defined as P < 0.05. Significant and near-significant values were used to create a predictive equation for PI size. SPSS statistical software (IBM Corporation; Armonk, New York) was utilized for all statistical analyses.
RESULTS
Patients and Demographics
Eight-hundred twenty-six patients underwent 2-stage implant breast reconstruction from 2011 to 2017. Complete records were available for 140 patients for a total of 226 breasts. Patients’ mean age was 54 (range, 25–81) with a mean BMI of 27 (range, 16–44).
A total of 3.9% of breasts had a history of irradiation before mastectomy, whereas 8.8% of breasts received radiation therapy following mastectomy and before TE exchange. The majority of mastectomies were skin sparing (81.7%) with a smaller proportion of nipple-sparing mastectomies (11.6%) (Table 1).
Table 1.
Patient Demographics and Reconstructive Characteristics
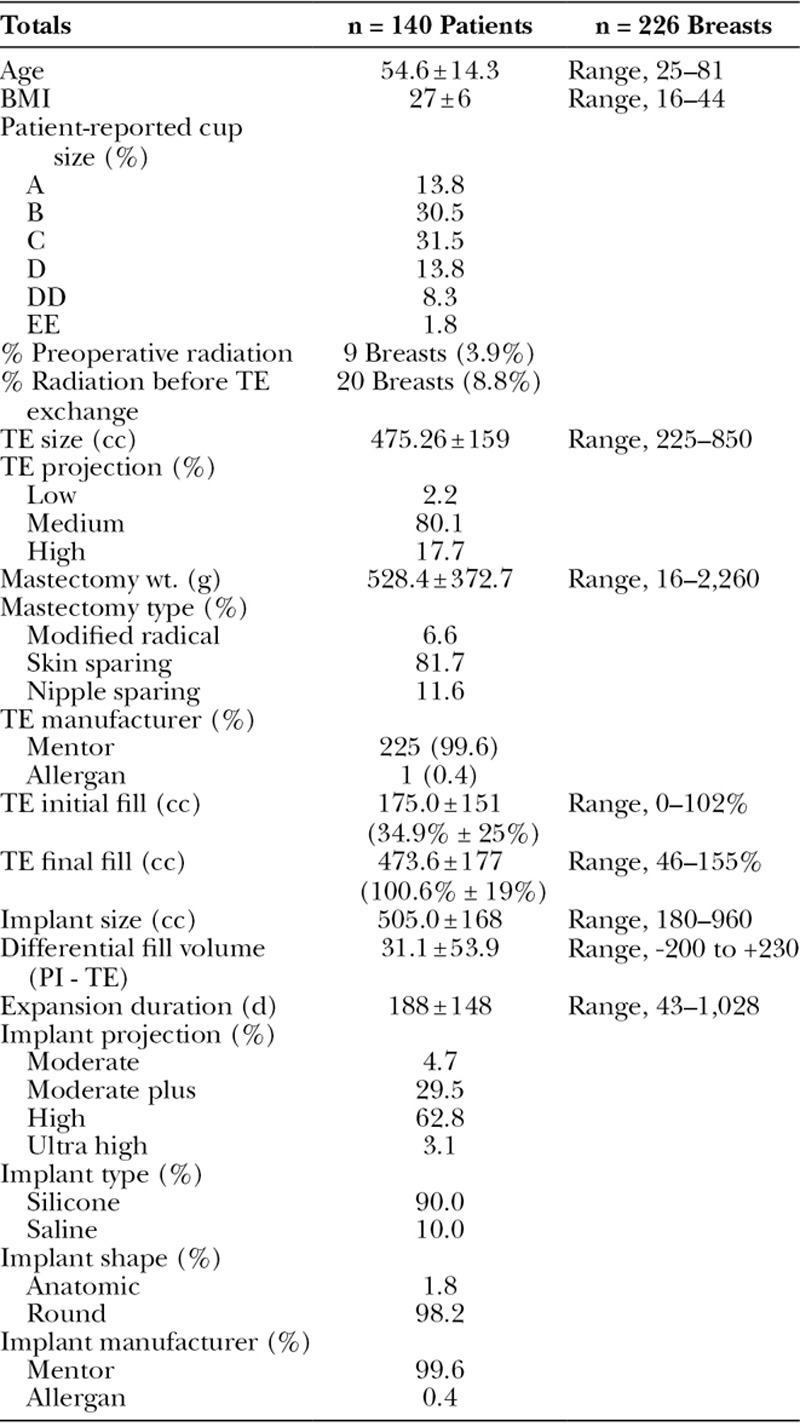
The majority of TEs were Mentor CPX4 (99.5%) and medium projection (80.1%) ranging in size from 225 to 850 cc (Fig. 1). Initial fill in the operating room at the time of TE placement ranged from 0 to 600 cc or 0–102% of the TE volume. Mean time between TE placement and exchange was 188 days (range, 43–1,028 days). Mean final fill volume percentage was 100.6% (range, 46–155%) of TE volume. The majority of PIs placed were high (63%) or moderate plus (26%) profile, smooth round (98%), silicone (90%) implants. Mean PI size was 505 cc with a range from 180 to 960 cc.
Fig. 1.
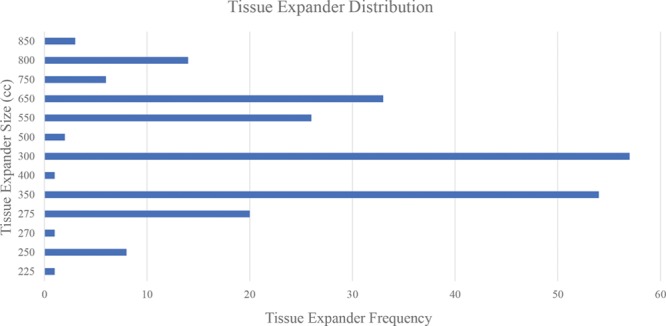
Range of TE sizes and profiles in the study. The 3 projection profiles included low (2.1%), medium (80.3%), and high (17.5%).
Reconstructive Outcomes
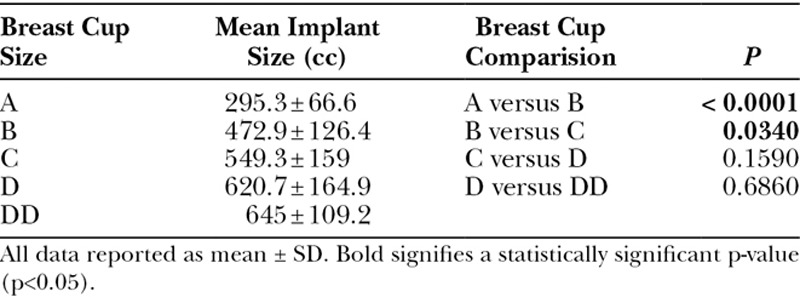
Mastectomy specimen weights were compared with preoperative self-reported breast cup size, TE size, and PI size. PI sizes were significantly different between patients with A cup versus B cup breasts (P < 0.0001) and B cup versus C cup breasts (P = 0.034), but differences were not significant between patients with breasts larger than C cup (Table 2).
Table 2.
Breast Cup Size and PI Size
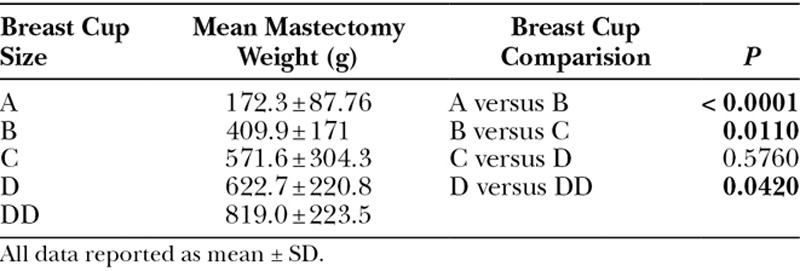
Similarly, the weight of the mastectomy specimen increased as self-reported breast cup size increased. There was a significant difference in mastectomy specimen weights between cup sizes A and B (P < 0.001), B and C (P = 0.011), and D and DD (P = 0.042; Table 3).
Table 3.
Breast Cup Size and Mastectomy Weight
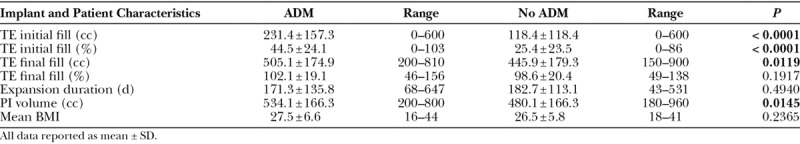
When ADM was used, patients had larger initial TE fill volume (P < 0.0001), final TE fill volume (P = 0.012), and PI size (P = 0.015; Table 4). Time between TE placement and TE exchange was not significantly different with ADM (P = 0.494). Higher intraoperative initial TE fill from use of ADM did not have a statistically significant impact on postoperative complications such as mastectomy flap necrosis, infection, or implant explantation.
Table 4.
The Effect of ADM on TE Fill, Duration of Expansion, and PI Size
The linear regression between mastectomy weight and TE final fill volume and PI size had correlation coefficients of 0.43 and 0.40, respectively (Fig. 2).
Fig. 2.
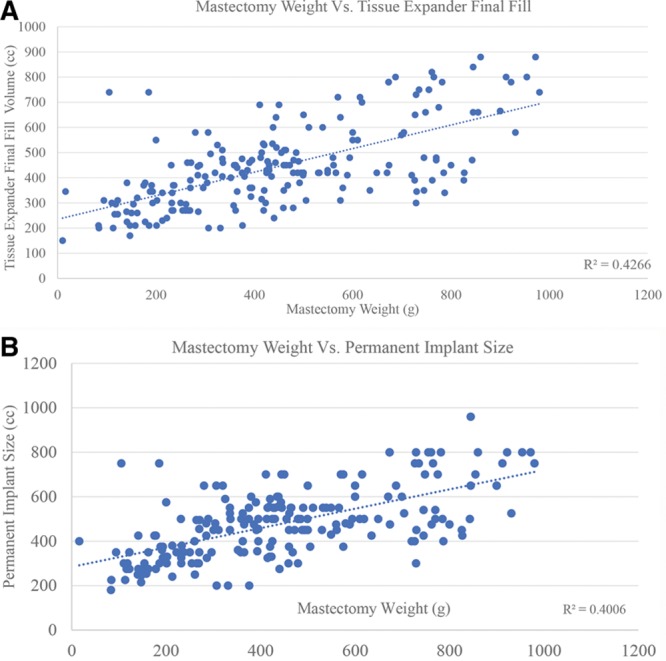
A, Linear regression model between the mastectomy specimen weight (g) and associated TE final fill volume (cc) (R2 = 0.43). B, Linear regression model comparing mastectomy specimen weight (g) to PI size (cc) (R2 = 0.40).
Difference in volume between the PI and final TE fill volume was calculated for each breast (Fig. 3). With respect to PI and TE volumes, 73.2% of breasts had greater PI volume than TE final fill volume, whereas 8.3% had matching PI volume to TE final fill volumes, and 18.4% of breasts had a smaller PI than TE final fill volume. TEs were grouped into categorical variables for final TE fill volume ranges, and mean PI volumes were compared within each TE size grouping yielding no overlapping 95% confidence intervals between any group.
Fig. 3.
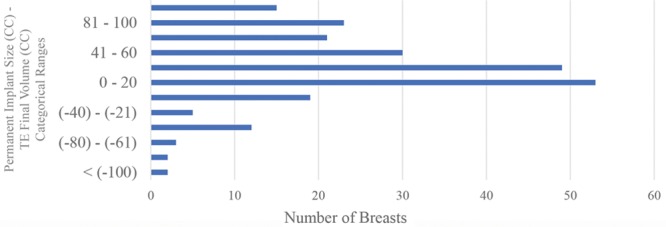
Differential between PI volume and final TE fill volume derived by subtracting the PI size (cc) from the TE final fill volume (cc).
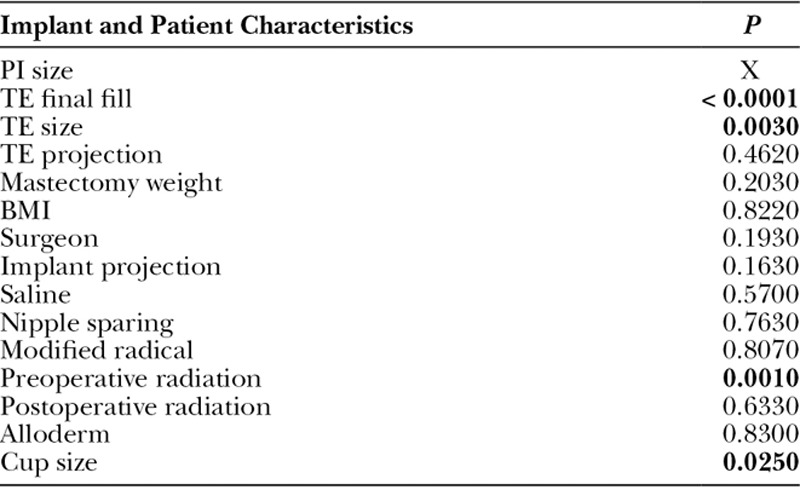
A multivariate analysis was used to evaluate the relationship between TE final fill volume and PI size. Variables were evaluated both independently and simultaneously (Table 5). Significant variables included TE final fill volume (P < 0.0001), TE size (P = 0.003), history of preoperative radiation (P = 0.001), and breast cup size (P = 0.031). On simultaneous multivariate analysis, modified radical mastectomy also achieved significance (P = 0.034).
Table 5.
Independent Regression Model for Predicting PI Size
A predictive equation for PI size during TE exchange was calculated using final TE fill volume, TE size, and whether the patient had a history of preoperative breast radiation with an R2 of 0.914:
TE size and TE final fill volume are reported in milliliters and preoperative radiation is represented as a binary value (1 = yes, 0 = no; Table 6). Although a modified radical mastectomy was statistically significant, its regression coefficient of 1 lacked clinical significance to justify inclusion in the formula. Preoperative breast cup size was only significant between A to B and B to C cup breasts and, therefore, excluded from the formula. TE and PI projection were not statistically significant, P = 0.074 and P = 0.163, respectively.
Table 6.
A Predictive Equation for Preoperatively Estimating PI Size
DISCUSSION
We retrospectively reviewed our multi-year institutional experience with 2-stage implant breast reconstruction. Multivariate regression analysis compared the significant variables for PI size during TE exchange. A predictive equation for PI size incorporating TE size, TE final fill volume, and history of radiation therapy was developed with a regression coefficient of 0.914. Although many centers have implants on consignment, the full range of implant sizes and quantities are not always available. Other institutions order implants per case, returning unused implants and generating significant back end workflow with regard to purchase orders.
Implant sizers and PIs of varying volume are ordered for each TE exchange. With growing experience, surgeons’ ability to predict final PI size improves. Developing a predictive model for PI sizing enables improved estimation of the final PI size.
The 3 significant variables for predicting final PI size were TE final fill volume, TE size, and history of preoperative radiation. Although TE fill volume and size are correlated, including both in the final formula yielded a higher overall regression coefficient. Preoperative radiation was associated with a 50 cc decrease in PI size regardless of TE fill volume. As expected, a history of preoperative radiation resulted in lower final implant volumes likely related to reduced soft-tissue compliance. The high complication risk associated with implant reconstruction in the setting of irradiated breasts has been well documented, but to our knowledge, no studies exist evaluating the impact of radiation on final PI size.9
The introduction of ADM in breast implant reconstruction represented a major and controversial development in breast reconstruction.10 Our study demonstrates that ADM use increases initial and final TE fill volume and PI size. Although ADM use may theoretically reduce the total number of fills required by increasing intraoperative fill volumes, it did not impact on time between TE placement and exchange as likely surgical timing was independent of completion of TE expansion alone.3,11,12
The relationships between self-reported bra cup size, mastectomy weight, and implant size were insightful findings. PI size increased with self-reported breast cup size, but above a C cup there was no statistically significant difference. The largest silicone and saline implants in the United States are 800 cc and 960 cc, respectively. At the larger end of breast sizes, there may not be adequately sized breast implants to replace mastectomy volumes. Furthermore, multiple studies have documented incorrect bra sizing in up to 70% of women and bra cup size variability by style, fabric, padding, and elastics.13,14 In contrast, the relationship between increasing bra cup size and mastectomy weights was more consistent at higher bra cup sizes. The relationships between bra size, mastectomy weight, and implant size are intuitive to plastic surgeons performing reconstruction. However, quantifying the relationship offers objective confirmation.
Notably, the plastic surgeon did not impact on the predictive equation for PI volume. Implant projection and mastectomy type did not have a clinically significant impact on final PI size either. Limitations to the study include its retrospective nature. The majority of the mastectomies were skin-sparing with predominantly smooth, round silicone implants used. Generalizability of results would be limited to smooth, round silicone implants, and the CPX4 Mentor TEs or their equivalent for Allergan and Sientra. Patient-reported outcomes to assess patient satisfaction using this formula were not available and are planned in an upcoming study.
Our equation for determining PI size has a high predictive value. With better presurgical implant planning, there is an opportunity to reduce the range of PIs required for each TE exchange. Application of the formula has the opportunity to simplify workflow, decrease implant storage space in the operating room, and simplify purchase orders and indirect costs of breast reconstruction. Future research directions include a prospective trial utilizing the predictive formula combined with a financial analysis to determine direct and indirect cost savings.
Footnotes
Published online 21 May 2018.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.2016 Plastic surgery statistics report. Available at: https://www.plasticsurgery.org/news/plastic-surgery-statistics. Accessed July 1, 2017.
- 2.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23.. [DOI] [PubMed] [Google Scholar]
- 3.Qureshi AA, Broderick K, Funk S, et al. Direct hospital cost of outcome pathways in implant-based reconstruction with acellular dermal matrices. Plast Reconstr Surg Glob Open. 2016;4:e831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 1982;69:195–208.. [DOI] [PubMed] [Google Scholar]
- 5.Fitzpatrick AM, Gao LL, Smith BL, et al. Cost and outcome analysis of breast reconstruction paradigm shift. Ann Plast Surg. 2014;73:141–149.. [DOI] [PubMed] [Google Scholar]
- 6.Qiao Q, Zhou G, Ling Y. Breast volume measurement in young Chinese women and clinical applications. Aesthetic Plast Surg. 1997;21:362–368.. [DOI] [PubMed] [Google Scholar]
- 7.Longo B, Farcomeni A, Ferri G, et al. The BREAST-V: a unifying predictive formula for volume assessment in small, medium, and large breasts. Plast Reconstr Surg. 2013;132:1e–7e.. [DOI] [PubMed] [Google Scholar]
- 8.Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2006;118:35S–45S.. [DOI] [PubMed] [Google Scholar]
- 9.Fischer LH, Nguyen D. Double-chamber tissue expanders optimize lower pole expansion in immediate breast reconstruction requiring adjuvant radiation therapy. Ann Plast Surg. 2016;76:S171–S174.. [DOI] [PubMed] [Google Scholar]
- 10.Breuing KH, Colwell AS. Immediate breast tissue expander-implant reconstruction with inferolateral AlloDerm hammock and postoperative radiation: a preliminary report. Eplasty. 2009;9:e16. [PMC free article] [PubMed] [Google Scholar]
- 11.Sbitany H, Serletti JM. Acellular dermis-assisted prosthetic breast reconstruction: a systematic and critical review of efficacy and associated morbidity. Plast Reconstr Surg. 2011;128:1162–1169.. [DOI] [PubMed] [Google Scholar]
- 12.Pannucci CJ, Antony AK, Wilkins EG. The impact of acellular dermal matrix on tissue expander/implant loss in breast reconstruction: an analysis of the tracking outcomes and operations in plastic surgery database. Plast Reconstr Surg. 2013;132:1–10.. [DOI] [PubMed] [Google Scholar]
- 13.Pechter EA. A new method for determining bra size and predicting postaugmentation breast size. Plast Reconstr Surg. 1998;102:1259–1265.. [DOI] [PubMed] [Google Scholar]
- 14.Bengtson BP, Glicksman CA. The standardization of bra cup measurements: redefining bra sizing language. Clin Plast Surg. 2015;42:405–411.. [DOI] [PubMed] [Google Scholar]


