Summary:
Nipple-sparing mastectomy (NSM) and reconstruction is challenging in ptotic patients with additional risk factors. Here, these problems are addressed with a staged strategy that extends NSM and reconstruction to patients with grade 3 ptosis and additional risk factors of diabetes, obesity, and macromastia. Three stages are used to perform a mastectomy, reposition the nipple, and reduce the skin envelope using the Wise pattern. This is followed by definitive implant placement in a final fourth stage. All patients successfully completed their reconstructions without a single instance of implant loss. Using a staged approach, NSM and reconstruction in high-risk ptotic patients is feasible. This is facilitated by using multiple surgical delays and insuring a well-healed skin envelope and optimal nipple position before any prosthetic device is placed.
INTRODUCTION
NSM in patients with significant ptosis and macromastia is not routinely performed. These patients are at high risk for vascular compromise and unpredictable final positioning of the nipple areola complex (NAC), flap necrosis, a skin envelope that poorly accommodates the prosthetic and implant loss.1,2 For these patients, a first-stage mastectomy through Wise incisions has been shown to facilitate a reliable second-stage repositioning of the NAC, retailoring of the skin envelope and placement of a subpectoral tissue expander with the first-stage presumably serving as a surgical delay.3
Patients with grade 3 ptosis and additional risk factors of obesity [body mass index (BMI) > 35], diabetes, and macromastia (> 1,000 g) are at even greater risk for complications1,2 and require additional measures to prevent nipple and flap necrosis and implant loss. In these higher risk patients, mastectomy through a full Wise pattern can result in immediate nipple and flap necrosis. In addition, simultaneous repositioning of the nipple, retailoring of the skin envelope, and prosthetic placement has a high rate of implant loss.2
To avoid these complications, a new approach was devised that utilizes only a portion of the lateral half of the Wise pattern at the time of mastectomy. This minimizes the chances for immediate nipple and flap necrosis. The remaining Wise incisions (preserving the inferior pedicle) are made in a short office procedure 10 days later after the patient has healed from the mastectomy. These additional incisions further delay the nipple and skin flaps preparing them for safe Wise-pattern skin retailoring and nipple repositioning.
The NAC is then repositioned and skin retailored without prosthetic placement in a third surgery. This strategy establishes an ideal skin envelope and nipple position in preparation for definitive implant placement in a final surgery. This multi-stage approach allows for safe nipple-sparing reconstructions and more reliable healing of the mastectomy flaps in a greater number of higher risk patients with more severe ptosis and other risk factors. Initial outcomes from 10 consecutive high-risk patients with either isolated grade 3 ptosis or grade 2 ptosis and an additional risk factor (diabetes, mastectomy weight > 1,000 g, BMI > 35 or prepectoral breast reconstruction) are presented.
Surgical Technique
The patient is marked using a standard Wise pattern in the standing position (Fig. 1). The NSM is performed through the smallest portion possible of the lateral half of the Wise pattern and closed. Ten day later, after the nipple and mastectomy flaps are confirmed to be viable, the remainder of the Wise incisions are made in the office under local anesthesia to further delay the flaps and nipples (Fig. 2). The inframammary fold (IMF) is never violated as this would disrupt the dermal vasculature to the NAC. At a minimum of 10 days after our delay procedure in the office, we proceed with repositioning of the NAC on an intact inferior pedicle of dermis and fat and retailoring of the skin envelope using a standard Wise pattern closure (Fig. 3). Three months later, a definitive subpectoral or prepectoral implant (we cover all our prepectoral implants with an acellular dermal matrix) is placed through an inframammary incision to complete the reconstruction (Fig. 4).
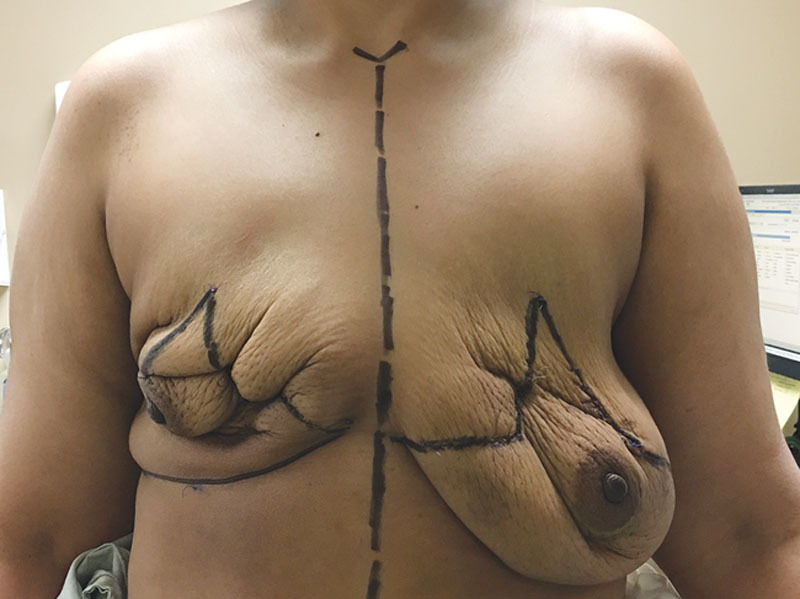
Fig. 1.

An obese (BMI, 33) 43-year-old female with grade 3 ptosis, macromastia (breast weight ~1,500 g) and a multi-centric right breast cancer involving 3 quadrants. Given her extensive disease, she is not a candidate for Spear’s approach of first-stage oncoplastic reduction. She is interested in a prepectoral breast reconstruction and nipple preservation. Given her excessive skin envelope and sternal notch to nipple distance of 37 cm, a staged approach was most appropriate. She underwent a bilateral total skin and nipple-preserving mastectomy through the extension from the lateral vertical limb to the IMF. Clearance of her cancer in confirmed on final pathology before proceeding to the next step. Complete healing is insured before proceeding with additional incisions to further delay the mastectomy flaps and NAC in the office. These additional incisions are not made at the initial surgery as they can result in significant upfront necrosis, which could immediately derail the reconstruction. This is a modification from our previous publication where all the Wise incisions were made at the initial surgery.3
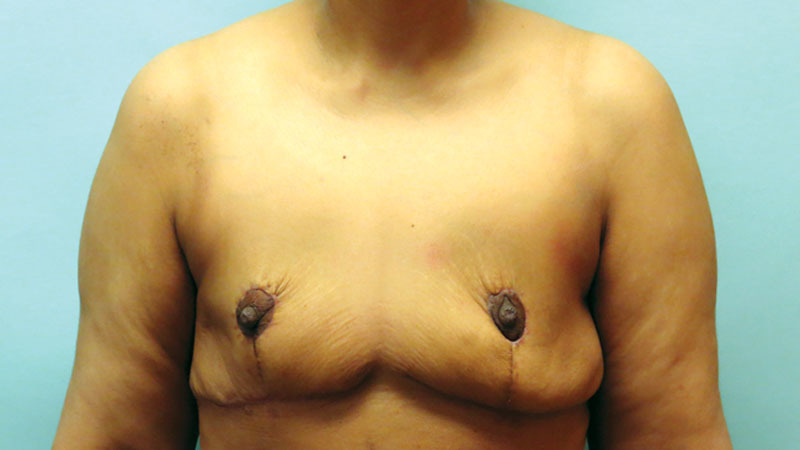
Fig. 2.
This photograph demonstrates our patient after she has recovered from the office procedure that further delays the Wise flaps and the NAC. This office procedure is done under local and is easily tolerated as the mastectomy flaps are virtually insensate. These are full thickness incisions through skin, dermis, and fat. The remainder of the lateral Wise pattern and the entirety of the medial Wise incisions are made while preserving the IMF. If the NAC can be bluntly dissected off the muscle, this is done to increase the stress of the delay.
Fig. 3.
Postoperative photograph after nipple repositioning and skin retailoring without prosthetic placement. This is the ultimate breast reduction surgery that removes all breast tissue and optimizes the nipple position and skin envelope. We do not place a prosthetic at the same time as nipple repositioning and skin retailoring as we feel these patients are still at high risk for wound breakdown and implant loss. The NAC is kept alive on an inferior pedicle of dermis and fat only with no residual breast tissue. This NAC repositioning with no underlying residual breast tissue is only possible because of the vascular effects of the 2 previous surgical delays. We have demonstrated the feasibility of this NAC repositioning with no residual breast tissue in over 50 patients now.3,7 If the cancer requires sacrifice of a portion of the flap that might result in necrosis of the nipple, conversion to a free nipple graft is performed. We have the luxury of a final pathology report before involuting tissue that might require reexcision. Patients who initially were poor candidates for NSM mastectomy and reconstruction are now converted to ideal candidates. We previously placed a subpectoral expander during this stage, which resulted in reconstructive failure in a significant percentage of these higher risk patients.3,7
Fig. 4.

Three months after confirmation of complete healing and the all the edema has resolved, either prepectoral or subpectoral definitive implant placement is performed. We have delayed placement of the prosthetic until the very last step in these patients to insure minimal risk of implant loss as there is now minimal chance of wound breakdown. By waiting 3 months, we can proceed with a lateral inframammary incision with minimal risk of compromise to the NAC as there has been time for collaterals to develop. If circumstances demand that the prosthetic is placed sooner, one must consider dissecting the Wise flaps off the inferior pedicle to preserve blood flow. This is tedious and puts the implant and NAC at increased risk. Here, the patient undergoes prepectoral breast reconstruction with an acellular dermal matrix. The option of a subpectoral reconstruction without acellular dermal matrix is also available. To date, we have had no instances of implant loss if we delay implant placement for 3 months after the NACs have been repositioned and the skin has been retailored and allowed to heal as demonstrated here.
DISCUSSION
Multiple approaches have been described to facilitate nipple-sparing mastectomy (NSM) and reconstruction4 in the ptotic patient. The most accepted approach was proposed by Spear—an oncoplastic reduction in a first stage followed by subsequent NSM and reconstruction in a second stage.5 This strategy allows for repositioning of the nipple and retailoring of the skin envelope before NSM and reconstruction, which avoids the high risk of complications when performing these procedures simultaneously.2 There are difficulties with applying this strategy to extensive breast cancers that are not amenable to breast conservation and require upfront mastectomy. These patients are not candidates for a first-stage oncoplastic reduction as this operation would violate the basic tenets of surgical oncology.
These problems have been previously addressed using a strategy which involves a first-stage mastectomy through Wise incisions followed by second-stage repositioning of the NAC, retailoring of the skin envelope and subpectoral expander placement.3 In a third stage, a definitive implant is placed. This strategy effectively addresses the most extensive cancers and creates a hand-in-glove accommodation between the implant and skin envelope.
Although this strategy works well in patients with grade 2 ptosis and subpectoral reconstructions, complications arise in patients with grade 3 ptosis and significant skin excess and patients with grade 2 ptosis and additional risk factors (prepectoral reconstructions, diabetes, mastectomy weight > 1,000 g or BMI > 35). These patients often have significant rates of flap and nipple necrosis when incising the full Wise pattern at the time of the initial mastectomy (the IMF is always preserved). They are also at high risk for reconstructive failure when attempting to retailor the skin and reposition the nipple and place a prosthetic in the same setting.
To avoid immediate nipple and mastectomy flap necrosis, only the smallest portion possible of the lateral Wise pattern is now incised at the time of mastectomy. The remaining incisions are made in the office after confirmed viability of the nipple and mastectomy flaps. The third stage involves pure skin retailoring and nipple repositioning and transforms a high-risk patient with a nonideal breast into one with an ideal skin envelope and nipple position with no residual breast tissue. Subpectoral or prepectoral definitive implants are then placed 3 months later. This is the key change in approach that avoids reconstructive failure in these very high-risk patients—avoiding placement of a prosthetic with simultaneous significant skin retailoring and nipple repositioning.
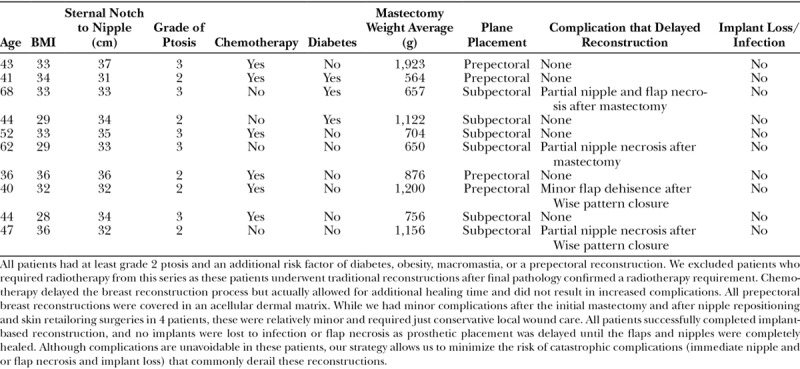
In our first 10 patients, 2 suffered partial nipple necrosis after initial mastectomy, which required wound care and debridement and 2 patients suffered wound healing issues after nipple repositioning and skin retailoring. These patients all recovered with conservative wound care. There were no implant-related complication, and all patients successfully completed their reconstructions (Table 1). At 1-year follow-up, there have been no instances of capsular contracture, significant malposition or complications requiring reoperation. The use of multiple stages allows us to safely extend NSM and reconstruction to a greater number of high risk ptotic patients who would not have previously been offered nipple preservation. Preliminary analysis from at least 25 patients now using a 13-item survey with a 5-point Likert-type scale to assess their experience with this new procedure indicates excellent satisfaction with their outcomes.6
Table 1.
Demographics for 10 Consecutive, Nipple-sparing, Implant-based Breast Reconstructions
SUMMARY
NSM and implant-based reconstruction in patients with significant ptosis and other risk factors is challenging. Nipple and flap necrosis, implant loss and reconstructive failure are common in these patients. Here, we present a 4-stage approach that allows us to avoid these complications. High-risk patients with nonideal and large skin envelopes and ptotic nipple positions have their mastectomies performed, skin envelopes reduced, and nipples repositioned in 2 surgeries and 1 office procedure. This is followed by delayed definitive implant placement in a fourth surgery. This multistage strategy minimizes the risk of reconstructive failure in ptotic, high-risk patients.
ACKNOWLEDGMENTS
The authors thank Dr. Piotr Skowronski for his assistance and thoughtful insight.
Footnotes
Published online 10 May 2018.
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
REFERENCES
- 1.McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg. 2008;121:1886–1892.. [DOI] [PubMed] [Google Scholar]
- 2.Munhoz AM, Montag E, Filassi JR, et al. Immediate nipple-areola-sparing mastectomy reconstruction: an update on oncological and reconstruction techniques. World J Clin Oncol. 2014;5:478–494.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz JD, Skowronksi PP. Improved outcomes with pedicled nipple-sparing mastectomies using a new surgical delay: mastectomy through wise incisions. Plast Reconstr Surg Glob Open. 2017;5:e1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karian LS, Therattil PJ, Wey PD, et al. Delay techniques for nipple-sparing mastectomy: a systematic review. J Plast Reconstr Aesthet Surg. 2017;70:236–242.. [DOI] [PubMed] [Google Scholar]
- 5.Spear SL, Rottman SJ, Seiboth LA, et al. Breast reconstruction using a staged nipple-sparing mastectomy following mastopexy or reduction. Plast Reconstr Surg. 2012;129:572–581.. [DOI] [PubMed] [Google Scholar]
- 6.Martin E, Schwartz JC. Patient satisfaction and experience with a four-stage procedure to facilitate extreme nipple sparing mastectomy and reconstruction. 2018, In: Proceedings of the American Society for Breast Surgeons 19th Annual Meeting; May 2–6, Orlando, FL Abstract. [Google Scholar]
- 7.Schwartz JD, Skowronski PP. Surgical delay facilitates pedicled nipple-sparing mastectomy and reconstruction in the ptotic patient. Plast Reconstr Surg Glob Open. 2016;4:e735. [DOI] [PMC free article] [PubMed] [Google Scholar]


