Abstract
Identifying risk factors associated with overweight and obesity in HIV-infected patients.
A cross-sectional study analyzing data from patients attending an HIV outpatient unit. Overweight was defined as body mass index (BMI) ≥25 kg/m2; <30 kg/m2, obesity was ≥30 kg/m2. Patients’ characteristics contemporary to BMI assessment were collected. Multivariate logistic regression identified risk factors associated with overweight/obesity.
Eight hundred sixty-two patients, median age 51 years, 21.5 years of HIV infection follow-up, 585 (68%) male, 829 (96%) receiving combined antiretroviral therapy (cART) for median 16.7 years, 768 (91%) HIV load <40 copies/mL, 618 (73%) CD4+ ≥500 cells/mm3; 266 (31%) HCV+ serology, 110 (13%) had detectable HCV-RNA. Overweight affected 191 (22%) patients and obesity 46 (5%). Overweight and obesity were associated with age, HIV follow-up duration, and HIV transmission risk group. Overweight was also associated with gender and HCV status. In patients with substance use data, overweight was associated with alcohol and nonsmoking status. Obesity was associated with nonsmoking and ex-smoker status. Overweight/obesity were not found associated with cART or immune cell counts.
In HIV-infected people, aging, alcohol consumption, nonsmoking, and ex-smoker status, the absence of HCV coinfection and to have cleared HCV infection are associated with overweight and/or obesity. Clinicians should be aware of these trends and consider introducing weight management programs as part of routine HIV care.
Keywords: cleared HCV management, HIV, nutritional support, obesity, overweight, smoking cessation
1. Introduction
Highly active antiretroviral therapy has drastically reduced the number of deaths and AIDS-defining events among HIV-infected people, including wasting syndrome.[1] Nowadays, HIV-infected patients who receive combined antiretroviral therapy (cART) live longer but comorbidities emerge earlier and more frequently. Among them, metabolic and cardiovascular diseases are 2 leading causes of death for HIV-infected patients living in high-income countries.[2] Overweight and obesity are 2 risk factors for diabetes, hypertension, cardiovascular disease, and cancer in the general population[3,4] that increasingly affect HIV-infected people.[5–7] Moreover, obesity seems to have a detrimental effect on immune recovery after cART initiation.[8]
Few studies have investigated the factors associated with overweight and obesity in HIV-infected people, and the concomitant incidence of overweight/obesity and metabolic/cardiovascular diseases in this population. The aim of this study was to determine the risk factors associated with overweight and obesity in a large cohort of HIV-infected patients.
2. Methods
2.1. Patients and study design
This cross-sectional study was conducted in an HIV outpatient unit in France, using an electronic medical record for HIV, HBV- or HCV-infected adults.[9,10] Subjects provided written informed consent for the use of their medical records on NADIS. This electronic medical record was approved by the French Commission National Informatique et Liberté (Registration number: 2001/762876/nadiscnil.doc). Patient data were recorded during medical visits, and data quality was controlled systematically during capture, annual assessments, and ad hoc processes prior to analyses. We selected patients with body mass index (BMI, kg/m2) measured at least once between January 1, 2015 and December 31, 2015.
According to the World Health Organization, obesity was defined as a BMI ≥30 kg/m2, and overweight is BMI ≥25 and <30 kg/m2. Demographic characteristics, comorbidities (past or ongoing) including diabetes, hypertension, myocardial infarction/coronary artery disease, peripheral arteriopathy and stroke, CD4+ and CD8+ T cell count, HIV viral load (VL), cART exposure and regimen, and HCV/HBV serologies were collected at the time of BMI measurement. Behavioral factors such as alcohol and tobacco consumption were collected when available.
2.2. Statistical analysis
Patients’ characteristics by BMI groups were analyzed using the Kruskal–Wallis test for quantitative variables, and Pearson χ2 test or Fischer test for categorical variables.
We studied associations between BMI (dependent variable) in 3 classes (<25 kg/m2/overweight/obesity) and socio-demographic characteristic (gender, age); HIV-related variables (CDC stage C, HIV transmission risk group, duration of HIV infection follow-up, CD4+ (cells/mm3 and <350 cells/mm3; yes/no) and CD8+ T cell count and %, nadir CD4+, HIV-VL, duration of HIV suppression, cART exposure and status (naive, ongoing, previous), cART regimen and cumulative exposure to PI, NNRTI and INSTI); hepatitis coinfection (AgHBs, anti-HBc, and HCV serologies); behavioral factors (alcohol consumption; yes/no; never-smoker/smoker/ex-smoker). Based on the observations, HIV transmission risk groups were analyzed as 3 categories: homosexual/bisexual, intravenous drug use (IVDU), and heterosexual/others. All variables associated with the outcome that had a P value lower than .20 in bivariate analysis were considered eligible to enter the multivariate model using multinomial regression. These multivariate models were built using a stepwise procedure with a P value at entry of .20 and a P value to stay of .10. As data on behavioral factors was not available for all patients, a subanalysis on patients with this available data was built using the same stepwise procedure. All data were analyzed using SPSS 20 Statistics (IBM, Madison, WI).
2.3. Ethics statement
All subjects provided written informed consent for the use of their medical records on NADIS. This electronic medical record was approved by the French Commission National Informatique et Liberté (Registration number: 2001/762876). This study was carried out in compliance with international guidelines for human research protection as per the Declaration of Helsinki and ICH-GCP.
3. Results
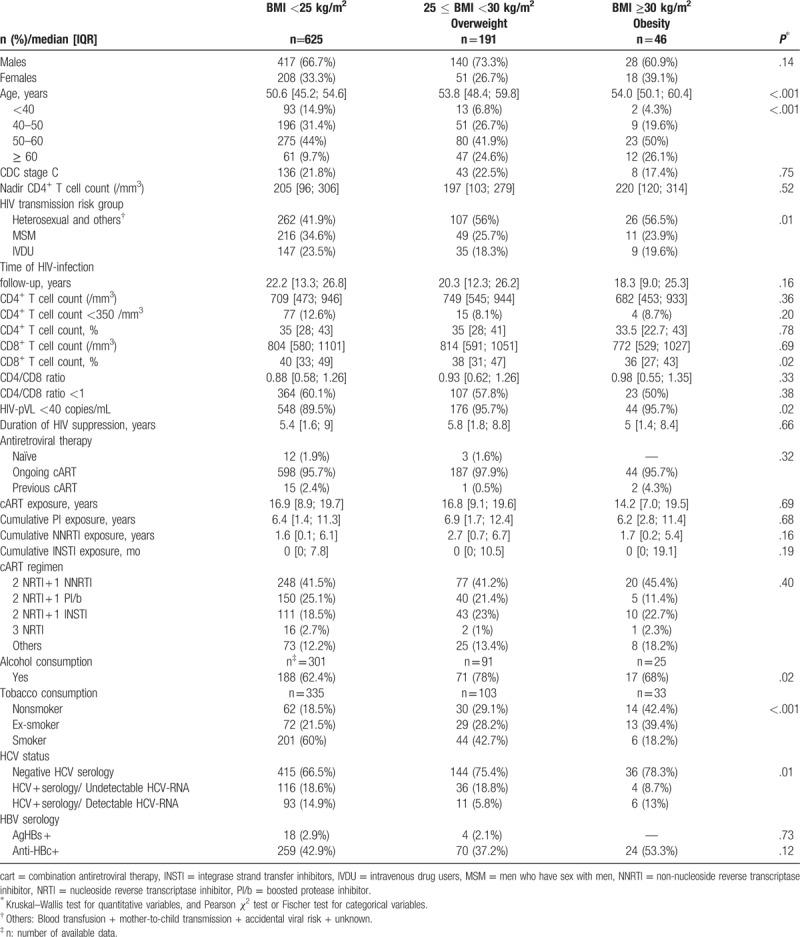
Eight-hundred eighty-four HIV-infected patients attended at least 1 medical visit during the study period, of whom 862 patients fulfilled selection criteria. Among them, 191 patients (22.2%) were overweight and 46 patients (5.3%) were obese. Patients’ characteristics by BMI are described in Table 1. Overall, 67.9% were males, with a median age 51.2 [46; 56] years and a median duration of HIV infection follow-up of 21.5 [12.3; 26.5] years. Gender differences for the prevalence of overweight and obesity were not significant, neither was the duration of HIV infection follow-up. Nevertheless, the prevalence of overweight and obesity increased with age. Among HIV-related variables, the proportion of patients contaminated heterosexually/others transmission risk group was significantly higher among patients with overweight and obesity (56% and 56.5%, respectively, versus 41.9% in patients <25 kg/m2; P=.01). Conversely, the duration of cART exposure, cART regimen, CD4+ or CD8+ T cell counts, and CD4/CD8 ratio were comparable across BMI groups, although patients with obesity had the lower percentage of CD8+ T cells. Furthermore, the proportion of patients with undetectable HIV plasma viral load was significantly higher in patients with overweight and obesity. Patient status regarding hepatitis C coinfection also differed across BMI groups, with the prevalence of negative HCV serology being significantly higher among patients with overweight and obesity, whereas the prevalence of chronic HCV infection (HCV+ serology with detectable HCV-RNA) was lower in patients with overweight. Data on alcohol and tobacco consumption were available in 417 (48%) and 471 (54.6%) patients, respectively, and both were available for 374 (43%) patients. The proportion of alcohol consumers was significantly higher among patients with overweight, whereas the proportions of never- and ex-smokers were significantly higher in patients with obesity.
Table 1.
Patients’ characteristics by BMI.
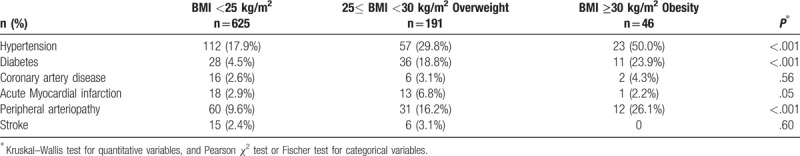
3.1. Prevalence of diabetes and cardiovascular comorbidities
The prevalence of diabetes and cardiovascular comorbidities by BMI are reported in Table 2. Three hundred nine patients (35.8%) presented at least 1 comorbidity, of whom 125 (52.7%) were overweight or obese. The distribution of comorbidities differed according to BMI. Indeed, the prevalence of hypertension, diabetes, and peripheral arteriopathy was significantly higher among overweight and patients with obesity, and the prevalence of acute myocardial infarction was significantly higher in patients with overweight.
Table 2.
Prevalence of diabetes and cardiovascular comorbidities according to BMI.
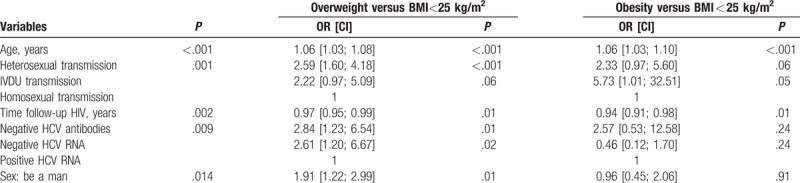
3.2. Multivariate analysis of factors associated with overweight and obesity
First, we used a multivariate model that considered the entire study cohort (Table 3), which revealed associations of overweight with negative HCV serology (OR: 2.84 [95% IC: 1.23; 6.54]), cleared HCV infection (OR: 2.61 [95% IC: 1.20; 6.67]) compared to active HCV infection, heterosexual/others transmission risk group (OR: 2.59 [95% IC: 1.60; 4.18] compared with men who have sex with men (MSM), male gender (OR: 1.91 [95% IC: 1.22; 2.99]), and age (OR: 1.06 [95% IC: 1.03; 1.08]). Compared with MSM, the IVDU transmission risk group was found to be associated with obesity (OR: 5.73 [95% IC: 1.01; 32.51]) but not overweight. Obesity was also associated with age (OR: 1.06 [95% IC: 1.03; 1.1]). Obesity and overweight were both negatively associated with the duration of HIV infection follow-up (OR: 0.94 [0.91; 0.98]) and 0.97 [0.95; 0.99] respectively).
Table 3.
Factors associated with overweight and obesity in HIV-infected patients; multivariate analysis.
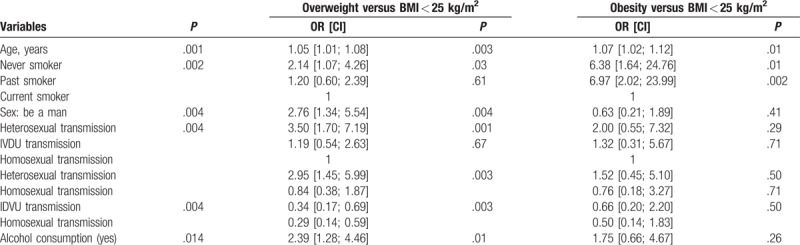
In a multivariate model considering only those patients for whom alcohol and smoking data were available (Table 4), overweight was associated with alcohol consumption (OR: 2.39 [95% IC: 1.28; 4.46], never-smoker status (OR: 2.14 [95% IC: 1.07; 4.26]). Obesity was found to be associated with ex-smoker status (OR: 6.97 [95% IC: 2.02; 23.99]) and nonsmoker status (6.38 [95% IC: 1.64; 24.76]). Heterosexual transmission risk group, being a man and age, remain associated as found in the general multivariated model.
Table 4.
Factors associated with overweight and obesity in HIV-infected patients with data tabacco and alcohol consumption; multivariate analysis.
4. Discussion
This cross-sectional study explored the risk factors associated with overweight and obesity in a large cohort of HIV-infected people who have received care for over 20 years with fairly successful HIV suppression. The data obtained showed that aging, gender, HIV transmission risk group, alcohol consumption, absence of active HCV coinfection and tobacco intoxication, but not cART regimen or CD4+ T cell count, are associated with overweight and/or obesity in this cohort of HIV-infected patients.
The advent of antiretroviral therapy has radically changed the course of body weight in HIV-infected patients. Indeed, weight loss and the concomitant wasting syndrome, which were observed in most untreated patients at the beginning of the epidemic, are observed in fewer than 10% of patients receiving cART in 2013.[11] In our study, only 7.5% of patients were underweight (BMI < 18.5 kg/m2), while obesity and overweight affected 27.5%, mirroring the progression of these conditions in HIV-infected patients.
Concern about overweight and obesity is growing worldwide. In a cross-sectional population-based survey performed between 2011 and 2013 and including 48,741 adults from several countries on different continents, the prevalence of overweight and obesity totaled 31.7% and 12.4% respectively.[12] In France, the trends in the general population were similar in 2008, with 30.6% of subjects with overweight and 13.1% with obesity,[13] and the prevalence of obesity increased steadily, reaching 15% in 2012.[14] The rising prevalence of overweight and obesity in HIV-infected people has been observed in many countries.[6,15,16] As in the general population, overweight and obesity are associated with a number of detrimental health conditions in HIV-infected patients, including cardiovascular diseases and diabetes.[16–20] This study confirms that the prevalence of diabetes and cardiovascular disease is high in HIV-infected patients, and that overweight and obesity increasing in this population add excess risk of these comorbidities. BMI distribution of patients starting cART is similar to that of the general population, but there is a significant risk of BMI gain during the first years after cART initiation.[15,21] Overweight or obesity was shown to affect half of patients initiating cART, and 1 in 5 patients appeared to move to a higher BMI category within 2 years of cART initiation.[15] This gain in BMI after cART initiation was associated with an increase in the subsequent risk of cardiovascular disease (CVD) and diabetes.[22] Our study found that 44.3% of HIV-infected patients with overweight/obesity had cardiovascular disease, including hypertension (33.7%), and 19.8% are diabetic. This prevalence is higher than previous observations in a younger cohort of HIV-infected patients,[20] suggesting a foreseeable age-related aggravation of this risk.
Multiple data have shown that patients receiving antiretroviral therapy have a higher BMI compared with naive ones,[11] and a significant gain in body weight has been observed shortly after cART initiation.[15,21] Nevertheless, a significant association between overweight/obesity and cART was not observed in our study, consistent with a previous meta-analysis on the HIV-infected population.[11] Therefore, risk factors for excessive weight gain other than cART should be monitored to avoid an over-risk of comorbidities in the HIV-infected population. Initial attempts to identify such risk factors for overweight and obesity in HIV infection found that Black African women and Hispanic people seem to be at a higher risk of obesity.[23,24] Unfortunately, ethnicity could not be documented in our study due to local regulations. In the general population, overweight and obesity are associated with aging, and observed more frequently over the age of 60.[12] Consistently, our study and others found that aging was significantly associated with overweight and obesity in HIV-infected patients.[6,15] Nevertheless, 17.6% of patients under 50 years old were also affected by overweight in our study. Previously, it was reported that obesity favors recovery of CD4+ T-cell counts in cART naive patients and those initiating cART.[8,25,26] Although no association between immune cell counts and obesity was found in our study, its cross-sectional design does not allow the impact of excessive weight on immune reconstitution over time to be excluded.
Among new risk factors for overweight and obesity found in this study, the absence of active HCV coinfection (either never coinfected or cleared coinfection) deserves particular interest. A lower BMI in HCV-co-infected subjects was also reported recently in a large study evaluating changes in body composition among HIV-infected patients.[24] Although the prevalence of HCV coinfection is high (15–30%) among HIV-infected patients,[27] and concerns a third of our cohort, the recent evolution of HCV-infection management with the advent of direct antiviral agents (DAA) allows a sustained viral response in more than 94% of HIV-HCV coinfected patients.[28–30] Since the conditions for the eradication of HCV-co-infection are now met in locations where DAA are available, it is predictable that the prevalence of overweight and obesity will rise in this population.
We found that several behavioral factors including transmission risk group and substance use (tobacco and alcohol) have a significant link with overweight and obesity. The data available on the role of transmission risk group on excessive weight is scant. A recent study comparing lifestyle and health behavior in MSM and heterosexual men found that MSM are more likely to perform intense physical training, which might limit overweight and obesity in this population compared with heterosexual men.[31] There is evidence that IVDU have an increased risk of low BMI in the general population,[32] and HIV-infected IVDU females have a lower BMI compared with their noninjected drug user counterparts.[33] Nevertheless, these studies did not consider other transmission risk groups and therefore, their results and ours cannot be compared. Regarding smoking, our observations in HIV-infected patients are consistent with patterns in the general population where smoking cessation was previously associated with both overweight and obesity, while light or moderate smoking was inversely associated with obesity.[12] In the same study, moderate alcohol intake was associated with both overweight and obesity. In our study, alcohol consumers were more likely to be overweight but not obese. However, as the amount of alcohol consumed was not available in our study, the impact of the consumption level remains elusive.
Our study has limitations. As mentioned above, the cross-sectional design of our study did not allow the impact of overweight and obesity on several biological and clinical variables, including immune reconstitution, to be evaluated. Moreover, data on exercise habits, diet, personal income, and education level were unavailable and could not be evaluated.
Altogether, the risk factors for excessive weight identified in this study of a long-lived cohort of HIV-infected patients reflect the impact of improvements in the management of HIV infection over the history of the epidemic. The availability of highly active antiretroviral drugs and DAA for hepatitis treatment, closer monitoring of comorbidities, and the implementation of educational programs for preventing substance abuse, including tobacco and alcohol, contribute to an extended lifespan and quality of life in HIV-infected patients. Nevertheless, the risk of obesity and excess weight also increased with age, HCV clearing, and smoking cessation.
With a longer lifespan, overweight in the HIV-infected population is increasing and associated with serious adverse medical consequences. Clinicians should be aware of these trends and consider introducing weight management programs as part of routine HIV care. As some risk behaviors appear to be associated with overweight and obesity, specific interventions targeting these factors have to be initiated, especially among smokers included in smoking cessation programs.
Acknowledgment
The authors thank the staff of the Research Department of the Immunohematology Unit of AP-HM Sainte Marguerite Hospital for helpful discussions and advise on this study.
Author contributions
Investigation: Sylvie Bregigeon, Olivia Zaegel-Faucher, Helene Laroche, Sebastien Galie, Perrine Geneau De Lamarlière, Matthieu Orticoni, Marie-Josèphe Soavi, Armelle Saout, Isabelle Poizot.
Methodology: Véronique Obry-Roguet, Carla Cano, Caroline Lions.
Writing – original draft: Véronique Obry-Roguet, Carla Cano, Isabelle Poizot.
Footnotes
Abbreviations: BMI = body mass index, cART = combined antiretroviral therapy, CVD = cardio vascular disease, DAA = direct antiviral agents, HBV = hepatitis B virus, HCV = hepatitis C virus, HIV = human immunodeficiency virus, IVDU = intravenous drug use, MSM = men who have sex with Men.
The authors have no conflicts of interest to disclose.
References
- [1].Campa A, Yang Z, Lai S, et al. HIV-related wasting in HIV-infected drug users in the era of highly active antiretroviral therapy. Clin Infect Dis 2005;41:1179–85. [DOI] [PubMed] [Google Scholar]
- [2].Data Collection on Adverse Events of Anti HIVdSG, Smith C, Sabin CA, et al. Factors associated with specific causes of death amongst HIV-positive individuals in the D:A:D study. AIDS 2010; 24:1537–1548. [DOI] [PubMed] [Google Scholar]
- [3].Bogers RP, Bemelmans WJ, Hoogenveen RT, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med 2007;167:1720–8. [DOI] [PubMed] [Google Scholar]
- [4].Sullivan PW, Morrato EH, Ghushchyan V, et al. Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S., 2000-2002. Diabetes Care 2005;28:1599–603. [DOI] [PubMed] [Google Scholar]
- [5].Tate T, Willig AL, Willig JH, et al. HIV infection and obesity: where did all the wasting go? Antivir Ther 2012;17:1281–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Castro Ade C, Silveira EA, Falco Mde O, et al. Overweight and abdominal obesity in adults living with HIV/AIDS. Rev Assoc Med Bras 19922016;62:353–60. [DOI] [PubMed] [Google Scholar]
- [7].Koethe JR, Jenkins CA, Lau B, et al. Rising obesity prevalence and weight gain among adults starting antiretroviral therapy in the United States and Canada. AIDS Res Hum Retroviruses 2016;32:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Crum-Cianflone NF, Roediger M, Eberly LE, et al. Obesity among HIV-infected persons: impact of weight on CD4 cell count. AIDS 2010;24:1069–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pugliese P, Cuzin L, Cabie A, et al. A large French prospective cohort of HIV-infected patients: the Nadis Cohort. HIV Med 2009;10:504–11. [DOI] [PubMed] [Google Scholar]
- [10].Pugliese P, Cuzin L, Enel P, et al. [NADIS 2000, development of an electronic medical record for patients infected by HIV, HBV and HCV]. Presse Med 2003;32:299–303. [PubMed] [Google Scholar]
- [11].Buchacz K, Baker RK, Palella FJ, et al. Disparities in prevalence of key chronic diseases by gender and race/ethnicity among antiretroviral-treated HIV-infected adults in the US. Antivir Ther 2013;18:65–75. [DOI] [PubMed] [Google Scholar]
- [12].Pengpid S, Peltzer K. Associations between behavioural risk factors and overweight and obesity among adults in population-based samples from 31 countries. Obes Res Clin Pract 2017;11:158–66. [DOI] [PubMed] [Google Scholar]
- [13].Charles MA, Eschwege E, Basdevant A. Monitoring the obesity epidemic in France: the Obepi surveys 1997-2006. Obesity (Silver Spring) 2008;16:2182–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].INSERM, HEALTH K, ROCHE. National epidemiological survey on overweight and obesity (French). 2012. [Google Scholar]
- [15].Crum-Cianflone N, Roediger MP, Eberly L, et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS One 2010;5:e10106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gomes A, Reyes EV, Garduno LS, et al. Incidence of diabetes mellitus and obesity and the overlap of comorbidities in HIV+ hispanics initiating antiretroviral therapy. PLoS One 2016;11:e0160797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bray GA. Complications of obesity. Ann Intern Med 1985;103:1052–62. [DOI] [PubMed] [Google Scholar]
- [18].Wilson PWF, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med 2002;162:1867–72. [DOI] [PubMed] [Google Scholar]
- [19].Eeg-Olofsson K, Cederholm J, Nilsson PM, et al. Risk of cardiovascular disease and mortality in overweight and obese patients with type 2 diabetes: an observational study in 13,087 patients. Diabetologia 2009;52:65–73. [DOI] [PubMed] [Google Scholar]
- [20].Crum-Cianflone N, Tejidor R, Medina S, et al. Obesity among patients with HIV: the latest epidemic. AIDS Patient Care STDS 2008;22:925–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Amorosa V, Synnestvedt M, Gross R, et al. A tale of 2 epidemics: the intersection between obesity and HIV infection in Philadelphia. J Acquir Immune Defic Syndr 2005;39:557–61. [PubMed] [Google Scholar]
- [22].Achhra AC, Mocroft A, Reiss P, et al. Short-term weight gain after antiretroviral therapy initiation and subsequent risk of cardiovascular disease and diabetes: the D:A:D study. HIV Med 2016;17:255–68. [DOI] [PubMed] [Google Scholar]
- [23].Ilozue C, Howe B, Shaw S, et al. Obesity in the HIV-infected population in Northeast England: a particular issue in Black-African women. Int J STD AIDS 2017;28:284–9. [DOI] [PubMed] [Google Scholar]
- [24].Erlandson KM, Zhang L, Lake JE, et al. Changes in weight and weight distribution across the lifespan among HIV-infected and -uninfected men and women. Medicine (Baltimore) 2016;95:e5399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Palermo B, Bosch RJ, Bennett K, et al. Body mass index and CD4+ T-lymphocyte recovery in HIV-infected men with viral suppression on antiretroviral therapy. HIV Clin Trials 2011;12:222–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Koethe JR, Jenkins CA, Lau B, et al. Higher time-updated body mass index: association with improved CD4+ cell recovery on HIV treatment. J Acquir Immune Defic Syndr 2016;73:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Alter MJ. Epidemiology of viral hepatitis and HIV coinfection. J Hepatol 2006;44:S6–9. [DOI] [PubMed] [Google Scholar]
- [28].Naggie S, Cooper C, Saag M, et al. Ledipasvir and sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med 2015;373:705–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Sulkowski MS, Eron JJ, Wyles D, et al. Ombitasvir, paritaprevir co-dosed with ritonavir, dasabuvir, and ribavirin for hepatitis C in patients co-infected with HIV-1: a randomized trial. JAMA 2015;313:1223–31. [DOI] [PubMed] [Google Scholar]
- [30].Wyles DL, Ruane PJ, Sulkowski MS, et al. Daclatasvir plus sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med 2015;373:714–25. [DOI] [PubMed] [Google Scholar]
- [31].Mor Z, Parfionov K, Davidovitch N, et al. Gym exercising patterns, lifestyle and high-risk sexual behaviour in men who have sex with men and in heterosexual men. BMJ Open 2014;4:e005205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Nazrul Islam SK, Hossain KJ, Ahmed A, et al. Nutritional status of drug addicts undergoing detoxification: prevalence of malnutrition and influence of illicit drugs and lifestyle. Br J Nutr 2002;88:507–13. [DOI] [PubMed] [Google Scholar]
- [33].Forrester JE, Woods MN, Knox TA, et al. Body composition and dietary intake in relation to drug abuse in a cohort of HIV-positive persons. J Acquir Immune Defic Syndr 2000;25:S43–8. [DOI] [PubMed] [Google Scholar]


